Haemorrhagic fevers
Dr. Ameer kadhim Hussein.
M.B.Ch.B. FICMS (Community Medicine).
Haemorrhagic fevers
Viral haemorrhagic fever is a term which usually
applied to disease caused by :
Arenaviridae
(eg. Lassa fever).
Bunyaviridae (eg. Crimean-Congo haemorrhagic
fever).
Filoviridae
(eg. Ebola)
Flaviviridae
(eg. yellow fever).
Crimean-Congo haemorrhagic fever
• Crimean-Congo haemorrhagic fever (CCHF) is a widespread
disease caused by a tick-borne virus (Nairovirus) of the
Bunyaviridae family.
• The CCHF virus causes severe viral haemorrhagic fever
outbreaks, with a case fatality rate of 10–40%.
• CCHF is endemic in Africa, the Balkans, the Middle East and
some Asian countries.
• The hosts of the CCHF virus include a wide range of wild and
domestic animals such as cattle, sheep and goats.
Crimean-Congo haemorrhagic fever
• Animals become infected by the bite of infected ticks and the
virus remains in their bloodstream for about one week after
infection, allowing the tick-animal-tick cycle to continue when
another tick bites. Although a number of tick genera are capable
of becoming infected with CCHF virus, ticks of the genus
Hyalomma are the principal vector.
Transmission
• The CCHF virus is transmitted to people either by tick bites or
through contact with infected animal blood or tissues during and
immediately after slaughter.
• The majority of cases have occurred in people involved in the
livestock industry, such as agricultural workers, slaughterhouse
workers and veterinarians.
• Human-to-human transmission can occur resulting from close
contact with the blood, secretions, organs or other bodily fluids
of infected persons.
• Hospital-acquired infections can also occur due to improper
sterilization of medical equipment, reuse of needles and
contamination of medical supplies.
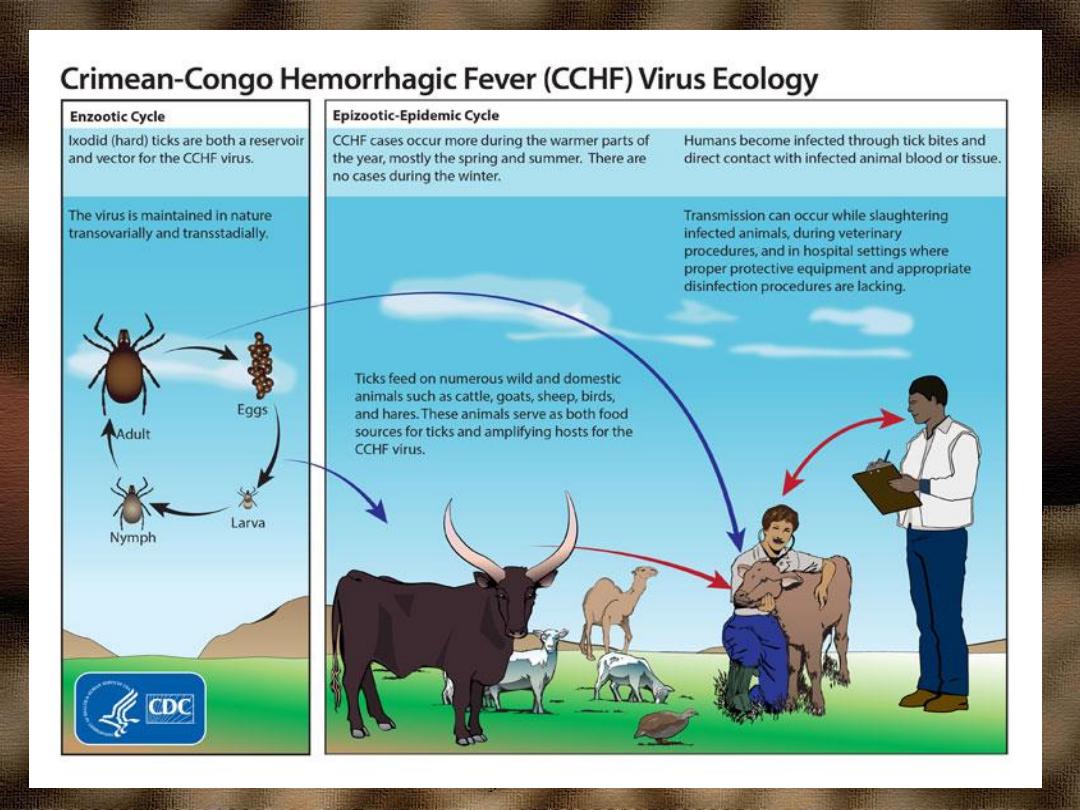

Ixodid (hard) ticks, especially those of the genus,
Hyalomma, are both a reservoir and a vector for the
CCHF virus

Incubation period
The length of the incubation period depends on
the mode of acquisition of the virus. Following
infection by a tick bite, the incubation period is
usually
one to three days
, with a maximum of
nine days. The incubation period following
contact with infected blood or tissues is usually
five to six days
, with a documented maximum of
13 days
Signs and symptoms
Onset of symptoms is sudden, with fever,
myalgia, dizziness, neck pain and stiffness,
backache, headache, sore eyes and photophobia.
There may be nausea, vomiting, diarrhoea,
abdominal pain and sore throat early on,
followed by sharp mood swings and confusion.
After two to four days, the agitation may be
replaced by sleepiness, depression and lassitude,
and the abdominal pain may localize to the upper
right quadrant, with detectable hepatomegaly.
Signs and symptoms
Other clinical signs include tachycardia,
lymphadenopathy and a petechial rash on
internal mucosal surfaces, such as in the mouth
and throat, and on the skin. The petechiae may
give way to larger rashes called ecchymoses, and
other haemorrhagic phenomena. There is usually
evidence of hepatitis, and severely ill patients
may experience rapid kidney deterioration,
sudden liver failure or pulmonary failure after
the fifth day of illness.
Signs and symptoms
The mortality rate from CCHF is approximately
30%, with death occurring in the second week of
illness.
In patients who recover, improvement generally
begins on the ninth or tenth day after the onset of
illness.
Diagnosis
CCHF virus infection can be diagnosed by
several different laboratory tests:
enzyme-linked immunosorbent assay (ELISA).
antigen detection.
serum neutralization.
reverse transcriptase polymerase chain
reaction (RT-PCR) assay.
virus isolation by cell culture.
Treatment
General supportive care with treatment of
symptoms is the main approach to managing
CCHF in people.
The antiviral drug ribavirin has been used to treat
CCHF infection with apparent benefit. Both oral
and intravenous formulations seem to be
effective.

Prevention
Controlling CCHF in animals and ticks
• It is difficult to prevent or control CCHF
infection in animals and ticks as the tick-animal-
tick cycle usually goes unnoticed and the
infection in domestic animals is usually not
apparent. Furthermore, the tick vectors are
numerous and widespread, so tick control with
acaricides (chemicals intended to kill ticks) is
only a realistic option for well-managed
livestock production facilities.
• There are no vaccines available for use in
animals.
Reducing the risk of infection in people
• Although an inactivated, mouse brain-derived
vaccine against CCHF has been developed and
used on a small scale in eastern Europe, there is
currently no safe and effective vaccine widely
available for human use.
• In the absence of a vaccine, the only way to
reduce infection in people is by raising
awareness of the risk factors and educating
people about the measures they can take to
reduce exposure to the virus.

Public health advice should focus on several
aspects
Reducing the risk of tick-to-human transmission
wear protective clothing (long sleeves, long trousers).
wear light coloured clothing to allow easy detection of
ticks on the clothes.
use approved acaricides (chemicals intended to kill
ticks) on clothing.
use approved repellent on the skin and clothing.
regularly examine clothing and skin for ticks; if found,
remove them safely.
seek to eliminate or control tick infestations on animals
avoid areas where ticks are abundant and seasons when
they are most active.
Reducing the risk of animal-to-human transmission
wear gloves and other protective clothing while
handling animals or their tissues in endemic areas,
notably during slaughtering and butchering procedures
in slaughterhouses or at home.
quarantine animals before they enter slaughterhouses or
routinely treat animals with pesticides two weeks prior
to slaughter.
Reducing the risk of human-to-human transmission
in the community
avoid close physical contact with CCHF-infected
people
wear gloves and protective equipment when taking care
of ill people
wash hands regularly after caring for or visiting ill
people.
Controlling infection in health-care settings
Health-care workers caring for patients with suspected or
confirmed CCHF, or handling specimens from them, should
implement standard infection control precautions. These include
basic hand hygiene, use of personal protective equipment, safe
injection practices and safe burial practices.
Samples taken from people with suspected CCHF should be
handled by trained staff working in suitably equipped
laboratories.