1
Breast Pathology
Fourth Stage /Lec.no.3
Dr. Rawaa Ghalib
Breast carcinoma
Breast carcinoma is the most common malignant tumor and the leading
cause of death in women, more than 1,000,000cases occurring
worldwide.
The incidence is high in North America and northern Europe,
intermediate in southern European and Latin American countries, and low
in most Asian and African countries (but rising rapidly in recent years in
these countries).
75% of women with breast cancer are older than 50, and approximately
50% of the cases are affect the upper outer quadrant of the breast.
Risk factors
1-Age :: The incidence rises throughout a woman's lifetime, peaking at
the age of 75–80 years and then declining slightly thereafter. Breast
cancer is very rare in all groups before the age of 25.
2-Age at Menarche::Women who reach menarche when younger than 11
years of age have a 20% increased risk compared with women who are
more than 14 years of age at menarche. Late menopause also increases
risk.
3-Age at First Live Birth::Women who experience a first full-term
pregnancy at ages younger than 20 years have half the risk of nulliparous
women or women over the age of 35 at their first birth.
4-First-Degree Relatives with Breast Cancer ::The risk of breast cancer
increases with the number of affected first-degree relatives (mother,
sister, or daughter), especially if the cancer occurred at a young age.
5-Atypical Hyperplasia:: A history of prior breast biopsies, especially if
revealing atypical hyperplasia, increases the risk of invasive carcinoma.

2
6-Race/Ethnicity::
Non-Hispanic white women have the highest rates of
breast cancer. The risk of developing an invasive carcinoma within the
next 20 years at age 50 is 1 in 15 for this group, 1 in 20 for African
Americans, social factors such as decreased access to health care and
lower use of mammography may well contribute to these differences, but
biologic differences also play an important role.
7-Estrogen Exposure::Postmenopausal hormone replacement therapy
increases the risk of breast cancer 1.2- 1.7 fold, and adding progesterone
increases the risk further.
Oral contraceptives have not been shown strongly to affect breast cancer
risk but do decrease the risk of endometrial and ovarian carcinomas.
Reducing endogenous estrogens by oophorectomy decreases the risk of
developing breast cancer by up to 75%. Drugs that block estrogenic
effects (e.g., tamoxifen) or block the formation of estrogen (e.g.,
aromatase inhibitors) also decrease the risk of breast cancer.
8-Radiation Exposure ::Radiation to the chest due to cancer therapy,
atomic bomb exposure, or nuclear accidents, results in a higher rate of
breast cancer. The risk is greatest with exposure at young ages and with
high radiation doses.
9-Carcinoma of the Contralateral Breast or Endometrium
Approximately 1% of women with breast cancer develop a second
contralateral breast carcinoma per year.
10-Geographic Influence :: Breast cancer incidence rates in the United
States and Europe are four to seven times higher than those in other
countries. The risk of breast cancer increases in immigrants to the United
States with each generation. Reproductive history (number and timing of
pregnancies), breastfeeding, diet, obesity, physical activity, and
environmental factors all probably play a role.
11-Breastfeeding::The longer women breastfeed, the greater the
reduction in risk, lactation suppresses ovulation and may trigger terminal
differentiation of luminal cells, the lower incidence of breast cancer in
3
developing countries largely can be explained by the more frequent and
longer nursing of infants.
Breast cancer pathogenesis
The major risk factors for the development of breast cancer are hormonal
and genetic therefore breast carcinomas can be divided into:
Sporadic cases, probably related to hormonal exposure.
Hereditary cases, associated with germline mutations.
Hereditary Breast Cancer
The inheritance of a susceptibility gene or genes is the primary cause of
approximately 12% of breast cancers.
The probability of a hereditary etiology increases in the cases of:
1-Multiple affected first-degree relatives.
2-Individuals are affected before menopause and/or have multiple
cancers.
3-There are family members with other specific cancers.
4-Mutations in BRCA1 and BRCA2 account for the majority of cancers
attributable to hereditary causes.
5-Mutations in BRCA1 located on chromosome 17q21also markedly
increase the risk of developing ovarian carcinoma, which occurs in as
many as 20-40% of carriers.
The finding of a positive test for the mutation can lead to an distressing
decision on the part of the affected individual, the main choices being
close follow-up and prophylactic mastectomy.
6-BRCA2 located on chromosome 13q12.3confers a smaller risk for
ovarian carcinoma (10- 20%) but is associated more frequently with male
breast cancer.
4
7-p53 is the most commonly mutated gene in sporadic breast cancers.
Sporadic Breast Cancer
The major risk factors for sporadic breast cancer are related to hormone
exposure and these are: gender, age at menarche and menopause,
reproductive history, breastfeeding, and exogenous estrogens.
Hormones increase the risk of carcinoma by the following
mechanisms:
1 - Hormonal exposure increases the number of breast epithelial cells by
stimulating breast growth during puberty, menstrual cycles, and
pregnancy.
2 - Exposure also drives cycles of proliferation that place cells at risk for
DNA damage.
3-Once premalignant or malignant cells are present, hormones can
stimulate their growth, as well as the growth of normal epithelial and
stromal cells that may aid and assist tumor development.
Diagnosis of breast carcinoma
1- History
2-Examination
3-Investigation:
A-Radiological (mammography, ultrasound)
B-Lab
1- FNA.
2-True cut biopsy.
3-Incisional biopsy.
4-Excisinal biopsy.
5-Immunohistochemistry
6-Gencs
5
Classification of Breast Carcinoma
Greater than 95% of breast malignancies are adenocarcinomas, which
are divided into
1 - CARCINOMA IN SITU
Ductal carcinoma in situ
Lobular carcinoma in situ
2 - INVASIVE CARCINOMA
No-special-type carcinoma (ductal)
Lobular carcinoma
Tubular/cribriform carcinoma
Mucinous (colloid) carcinoma
Medullary carcinoma
Papillary carcinoma
Metaplastic carcinoma
Ductal Carcinoma in Situ (DCIS)
DCIS consists of a malignant population of cells limited to ducts and
lobules by the basement membrane. The myoepithelial cells are
preserved.
Most are detected as a result of calcifications; less commonly, as a
mammographic density or a vaguely palpable mass. Rarely, DCIS
produces a nipple discharge or is detected as an incidental finding upon
biopsy for another lesion.
Morphology:: Many morphologic variants of DCIS exist, such as
comedocarcinoma , solid ,cribriform ,papillary,micropapillary.
Some
cases of DCIS have a single growth pattern, but the majority show a
mixture of patterns .
Comedocarcinoma is characterized by the presence of solid sheets of
pleomorphic cells with “high-grade” hyperchromatic nuclei and
lacking
connective tissue support. Necrosis is always present and constitutes an
6
important diagnostic sign, whether in the form of a large central focus or
of individual tumor cells. Coarse calcification often supervenes in these
necrotic areas.
Noncomedo DCIS consists of a monomorphic population of cells with
nuclear grades ranging from low to high. Several morphologic variants
can be seen. In cribriform DCIS, intraepithelial spaces are evenly
distributed and regular in shape (cookie cutter–like).
All women with DCIS were treated with mastectomy, usually followed
by radiation.If untreated, women with small, low-grade DCIS develop
invasive cancer at a rate of about 1% per year.
Lobular Carcinoma in Situ (LCIS)
LCIS is always an incidental biopsy finding, since it is not associated
with calcifications nor produce mammographic densities. LCIS is more
common in young women, with 80-90% of cases occurring before
menopause.
It is multicentric in approximately 70% of cases and bilateral
in approximately 30–40%.
LCIS consist of dyscohesive cells with oval or round nuclei and small
nucleoli, the cells lack the cell adhesion protein E-cadherin, resulting in
the cells appearing rounded without attachment to adjacent cells .
Women with LCIS develop invasive carcinomas at a frequency similar to
that of women with untreated DCIS, treatment choices include bilateral
prophylactic mastectomy, or, close clinical follow-up and mammographic
screening.
Invasive (Infiltrating) Carcinoma
Clinically
Invasive carcinoma almost always presents as a palpable mass that may
be fixed to the chest wall or cause dimpling of the skin.
Palpable tumors
are associated with axillary lymph node metastases in over 50% of
patients, retraction of the nipple may develop. Lymphatics may become
so involved as to block the local area of skin drainage and cause
7
lymphedema and thickening of the skin. In such cases, tethering of the
skin to the breast by Cooper ligaments mimics the appearance of an
orange peel, an appearance referred to as peau d'orange.
The term inflammatory carcinoma is reserved for tumors that present
with a swollen, erythematous breast, this gross appearance is caused by
extensive invasion and obstruction of dermal lymphatics by tumor cells.
Paget disease of the nipple
Paget disease is the name given to a crusted lesion of the nipple caused by
breast carcinoma,
its
a rare manifestation of breast cancer and account 1-
4% of cases. It is accompanied in nearly all instances by an underlying
DCIS of breast carcinoma, with or without associated stromal invasion.
Clinically a unilateral erythematous eruption with a scale crust. Pruritus
is common, and the lesion may be mistaken for eczema.
Microscopically large clear cells with atypical nuclei are seen within the
epidermis, usually concentrated along the basal layer,the cells can be
isolated or in clusters, and sometimes they form small glandular
structures.
A palpable mass is present in 50- 60% of women with Paget disease, the
carcinomas are usually poorly differentiated, ER negative, and
overexpress HER2/neu.
Rarely, breast cancer presents as an axillary nodal metastasis or distant
metastasis before cancer is detected in the breast.
Invasive
Ductal Carcinoma, No Special Type (NST)
Invasive carcinomas of no special type include the majority of
carcinomas (70 - 80%).
8
Morphology.
Grossly
Most tumors are firm to hard and have an irregular border, when cut they
typically produce a resistant gritty sensation, and shows a yellowish-gray
cut surface,with trabeculae radiating through the surrounding parenchyma
into the fat.
Microscopically
Well-differentiated carcinomas show prominent tubule formation, small
round nuclei, and rare mitotic figures with a surrounding desmoplastic
response.
Moderately differentiated carcinomas may have tubules, but solid
clusters or single infiltrating cells are also present. These tumors have a
greater degree of nuclear pleomorphism and contain mitotic figures.
Poorly differentiated carcinomas often invade as nests or solid sheets of
cells with enlarged irregular nuclei. A high proliferation rate and areas of
tumor necrosis are common.
Invasive Lobular Carcinoma
Invasive lobular carcinomas usually present as a palpable mass or a
mammographic density with irregular borders.
Lobular carcinomas have been reported to have a greater incidence of
bilaterality.
The actual fraction of women who develop invasive carcinomas in the
contralateral breast is only 5-10%.
Morphology
Microscopically
The histologic hallmark is the presence of dyscohesive infiltrating tumor
cells, often arranged in single file or in loose clusters or sheets, tubule
formation is absent. Signet-ring cells containing an intracytoplasmic
mucin droplet are common. Desmoplasia may be minimal or absent.
9
Lobular carcinomas have a different pattern of metastasis than other
breast cancers. Metastasis tends to occur to the peritoneum and
retroperitoneum, the leptomeninges (carcinoma meningitis), the
gastrointestinal tract, and the ovaries and uterus.
Immunohistochemistry
Estrogen and progesterone receptors (ER, PR).
These are nuclear hormone receptors, and represent an important
predictor of response to hormonal therapy, 80 % of carcinomas that are
ER and PR positive respond to hormonal manipulation, whereas only
about 40% of those with either ER or PR alone respond. ER-positive
cancers are less likely to respond to chemotherapy. Conversely, cancers
that fail to express either ER or PR have a less than 10% likelihood of
responding to hormonal therapy but are more likely to respond to
chemotherapy .
HER2/neu.
HER2/neu is a transmembrane receptor, its overexpression is associated
with poorer survival, but its main importance is as a predictor of response
to certain drugs like (Herceptin).
Genetic study:
Recently developed techniques that examine the DNA, RNA, and
proteins of carcinomas have provided new molecular classifications of
breast cancers.
Gene expression profiling has identified four major patterns of gene
expression in the ductal carcinoma group: luminal A, luminal B, basal-
like, and HER2 positive.
These molecular classes correlate with prognosis and response to therapy,
and thus have taken on clinical importance.
1-Luminal A (40- 55% of NST cancers): This is the largest group and
consists of cancers that are ER positive and HER2/neu negative. The
majority are well- or moderately differentiated, and most occur in
10
postmenopausal women, these cancers are generally slow growing and
respond well to hormonal treatments.
2-Luminal B
3-Basal-like
4-HER2 positive
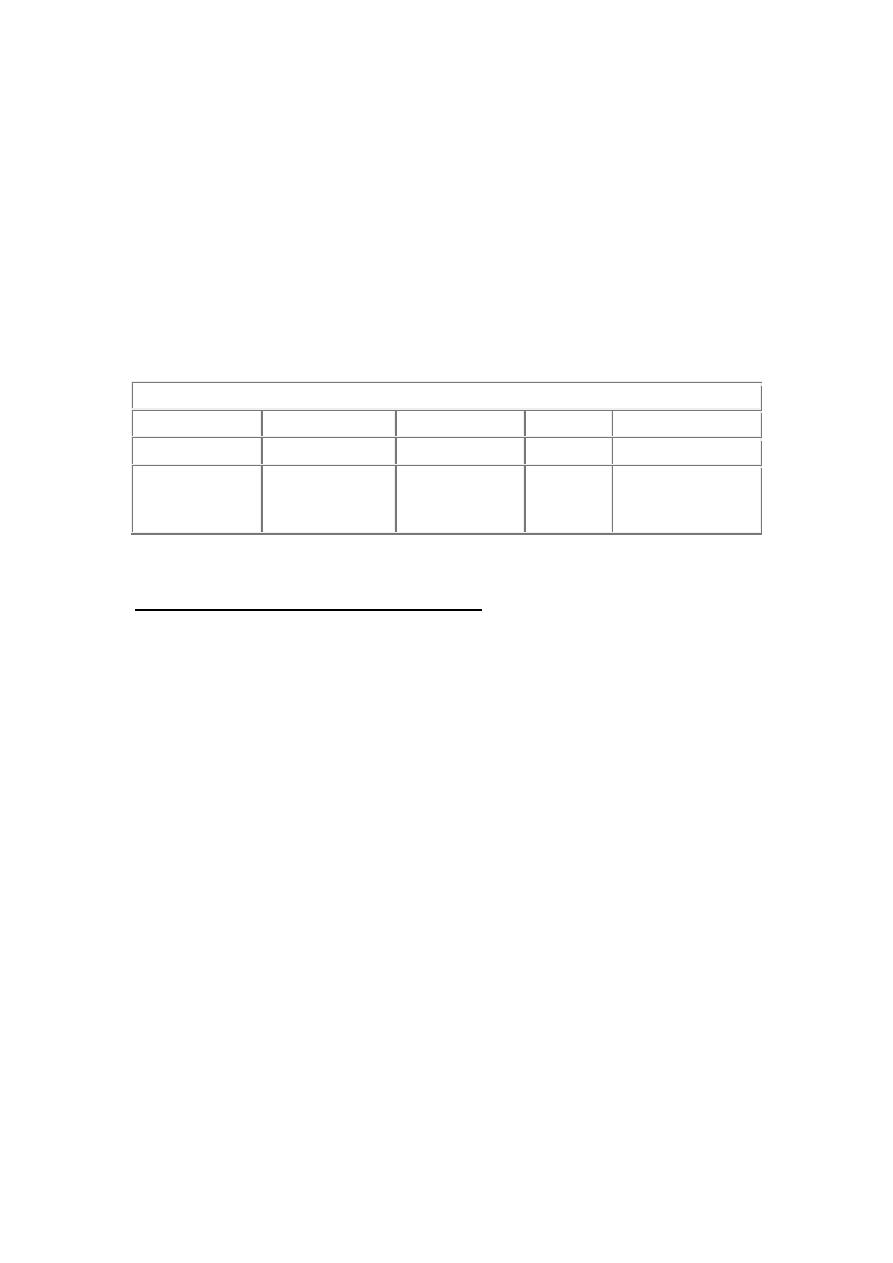
Use of immunohistochemistry as surrogate marker for the molecular
subtypes of breast cancer
MOLECULAR SUBTYPE
Immunoprofile Luminal A
Luminal B
HER2/neu Basal-like
ER, PR
ER and/or PR+
ER and/or PR+ ER–, PR– ER–, PR–
HER2 and
others
HER2–
Low Ki-67
(<14%)
HER2+ or
HER2–
Ki-67 =14%
HER2+
HER2–
CK5/6 and/or
EGFR+
Prognostic and Predictive Factors
The outcome for women with breast cancer varies widely. Many women
have a normal life expectancy, whereas others have only a 10% chance of
being alive in 5 years.
The major prognostic factors are as follows:
1. Invasive carcinoma versus in situ disease.
2. Distant metastases.
3. Lymph node metastases
4. Tumor size.
5. Locally advanced disease.
6. Inflammatory carcinoma.
Minor Prognostic and Predictive Factors
• Histologic subtype.
• Histologic grade.
• Estrogen and progesterone receptors.

11
• HER2/neu.
• Lymphovascular invasion.
• Proliferative rate.
• DNA content.
• Response to neoadjuvant therapy.
