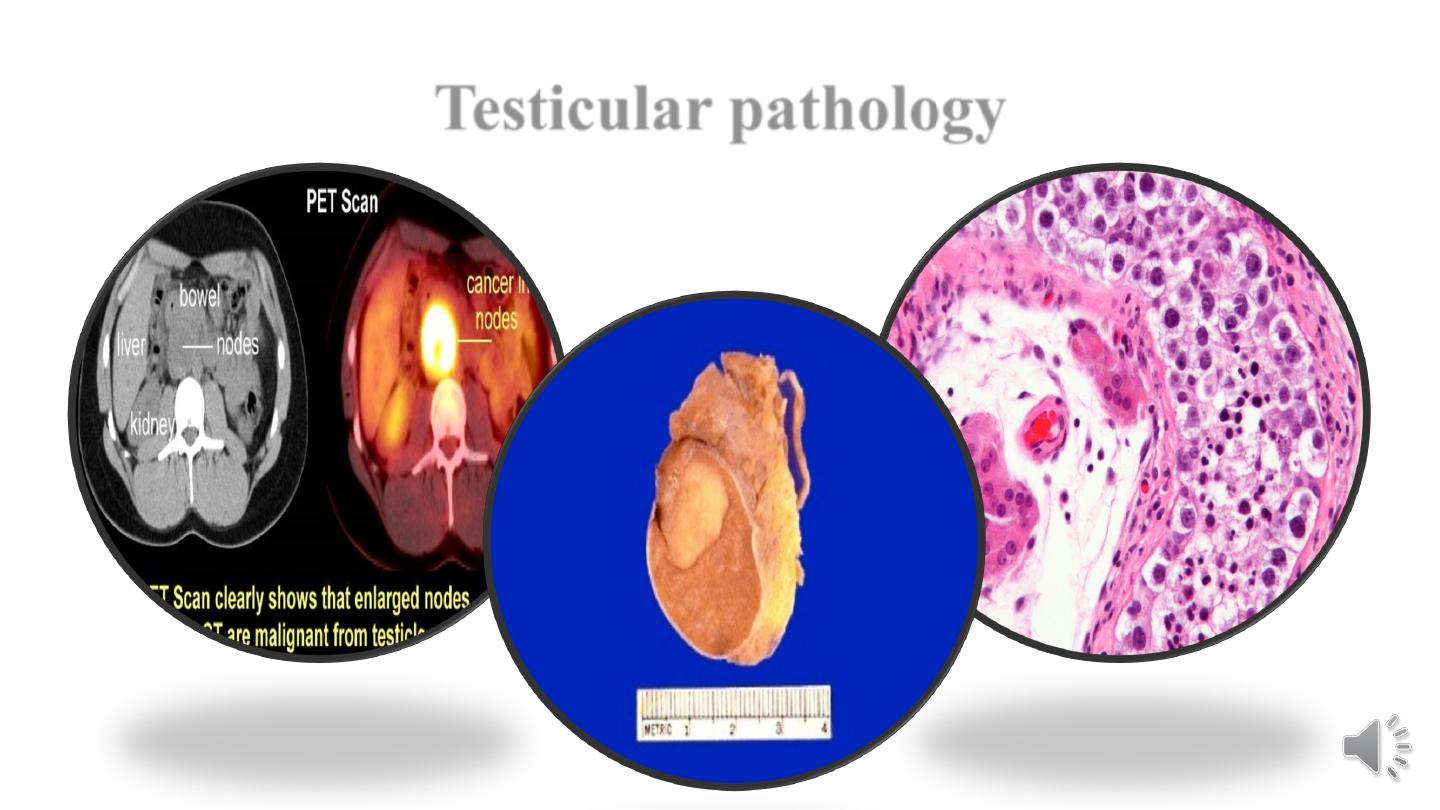
Testicular pathology
Male genital tract pathology
Lecture 1
Testicular pathology
Dr.Ahmed Raji
F.I.C.M.Path
College of Medicine - University of Babylon
22.6.2020

Testicular Atrophy
Atrophy is a regressive change that affects the testis.
Etiology
(1) Progressive atherosclerotic narrowing of the blood supply in old age.
(2) The end stage of an inflammatory orchitis.
(3) Cryptorchidism.
(4) Hypopituitarism.
(5) generalized malnutrition or cachexia.
(6) Irradiation.
(7) Prolonged administration of antiandrogens (treatment for advanced carcinoma of the prostate).
(8) A primary failure of genetic origin, such as in Klinefelter syndrome.
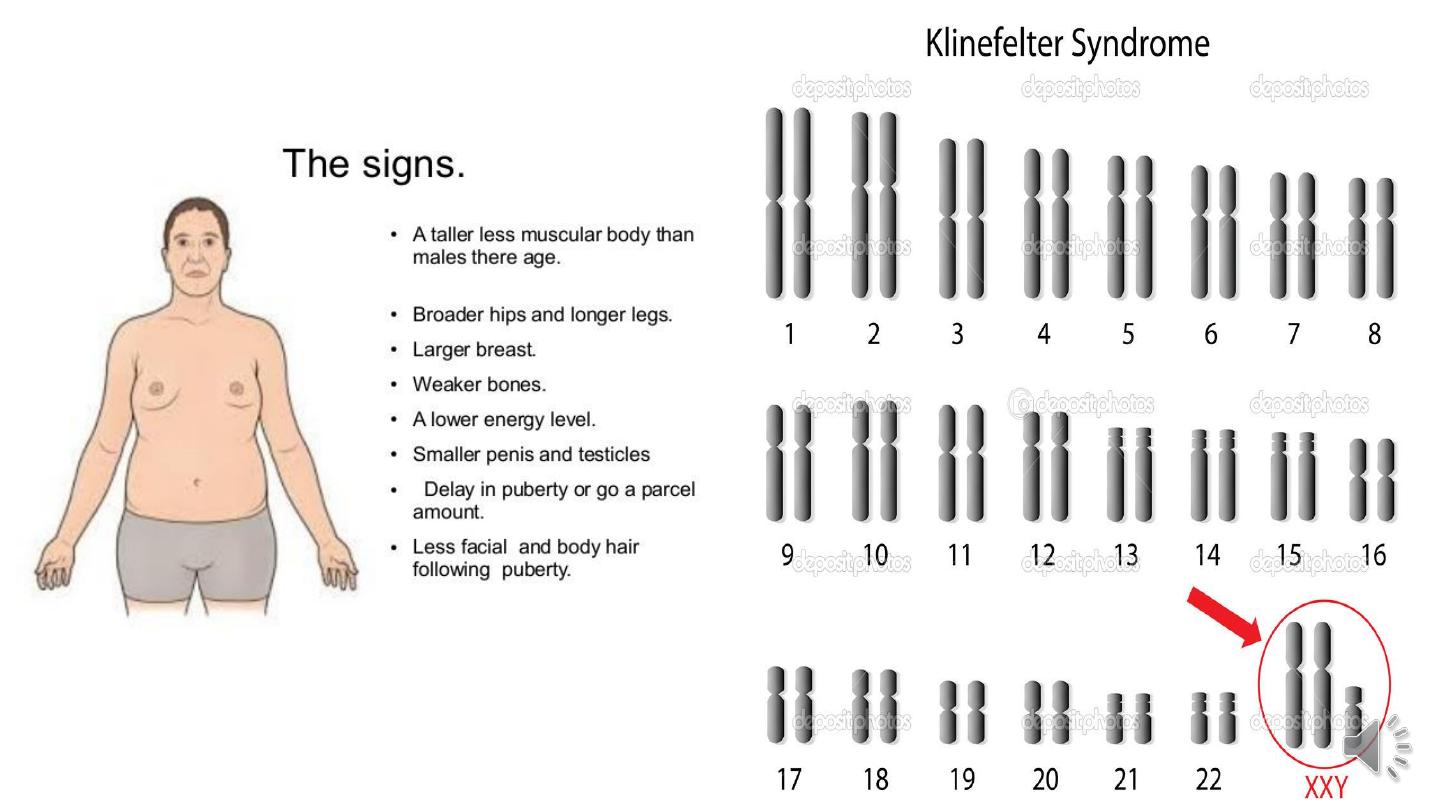
The clinical features:
The patients with testicular atrophy present with features of
hypogonadism:
Delayed puberty.
Loss of libido.
Lethargy with muscle weakness.
Decreased frequency of shaving.
Gynaecomastia.
Infertility.
Osteoporosis.
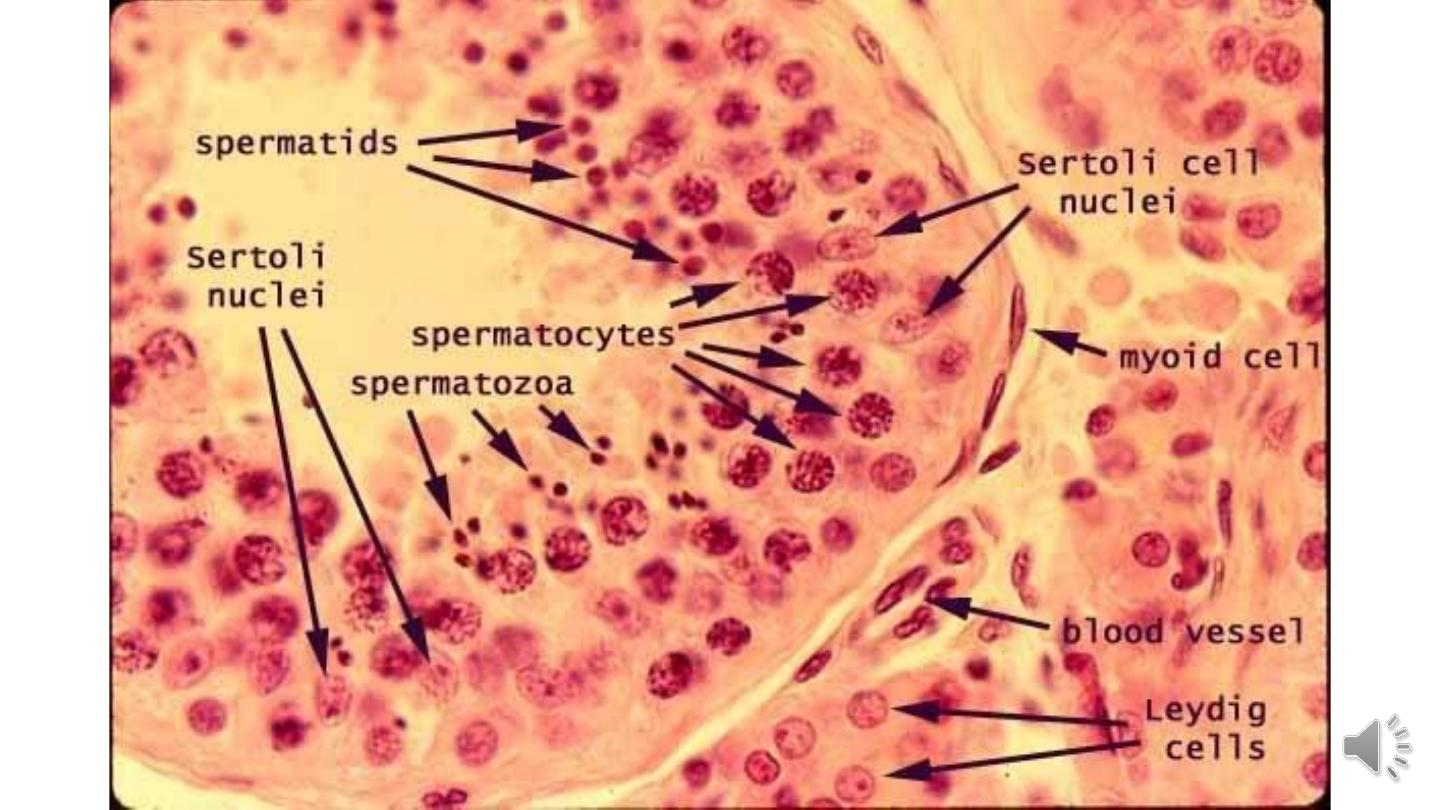
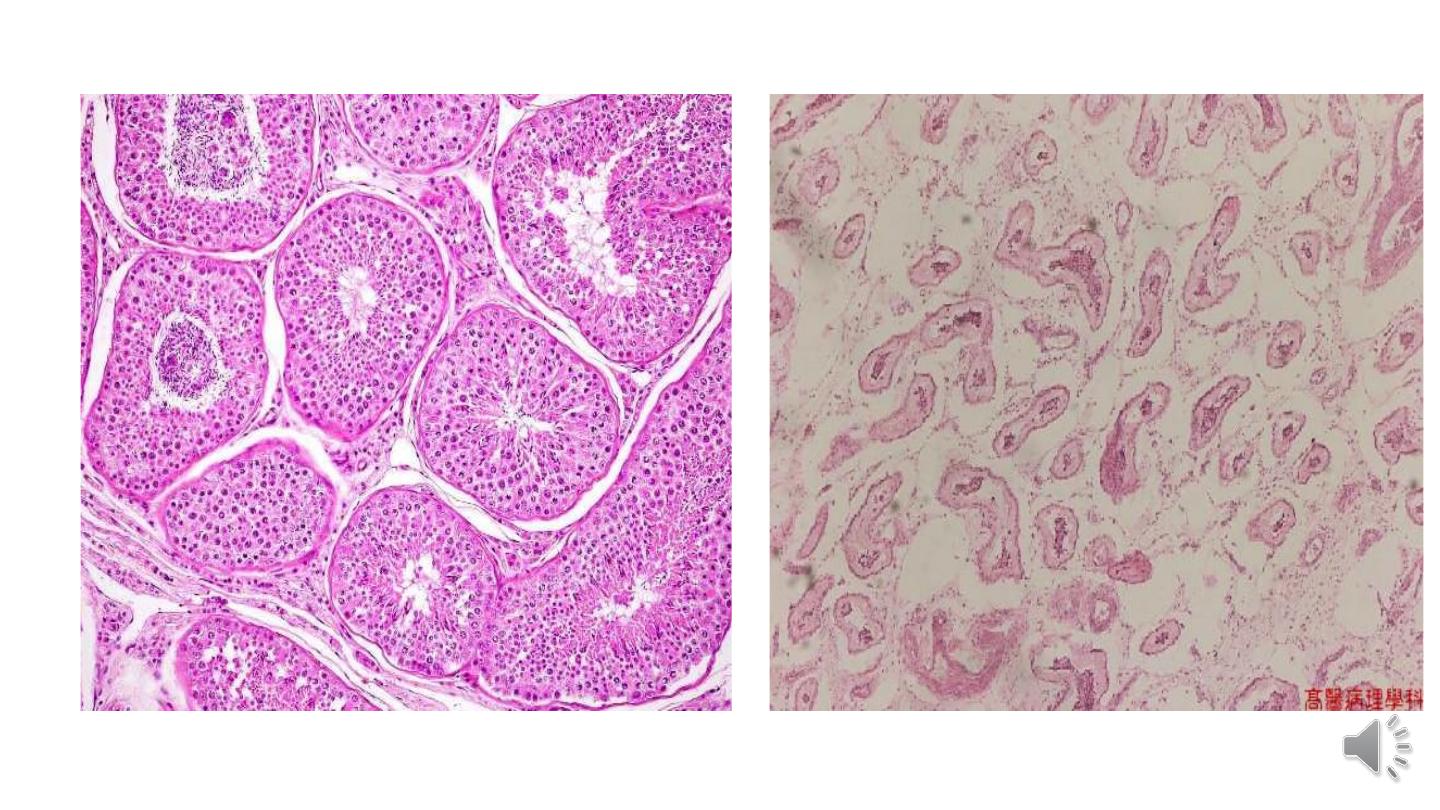
Morphology.
Grossly
Testis is small in size and is firm in consistency as a result of fibrotic changes.
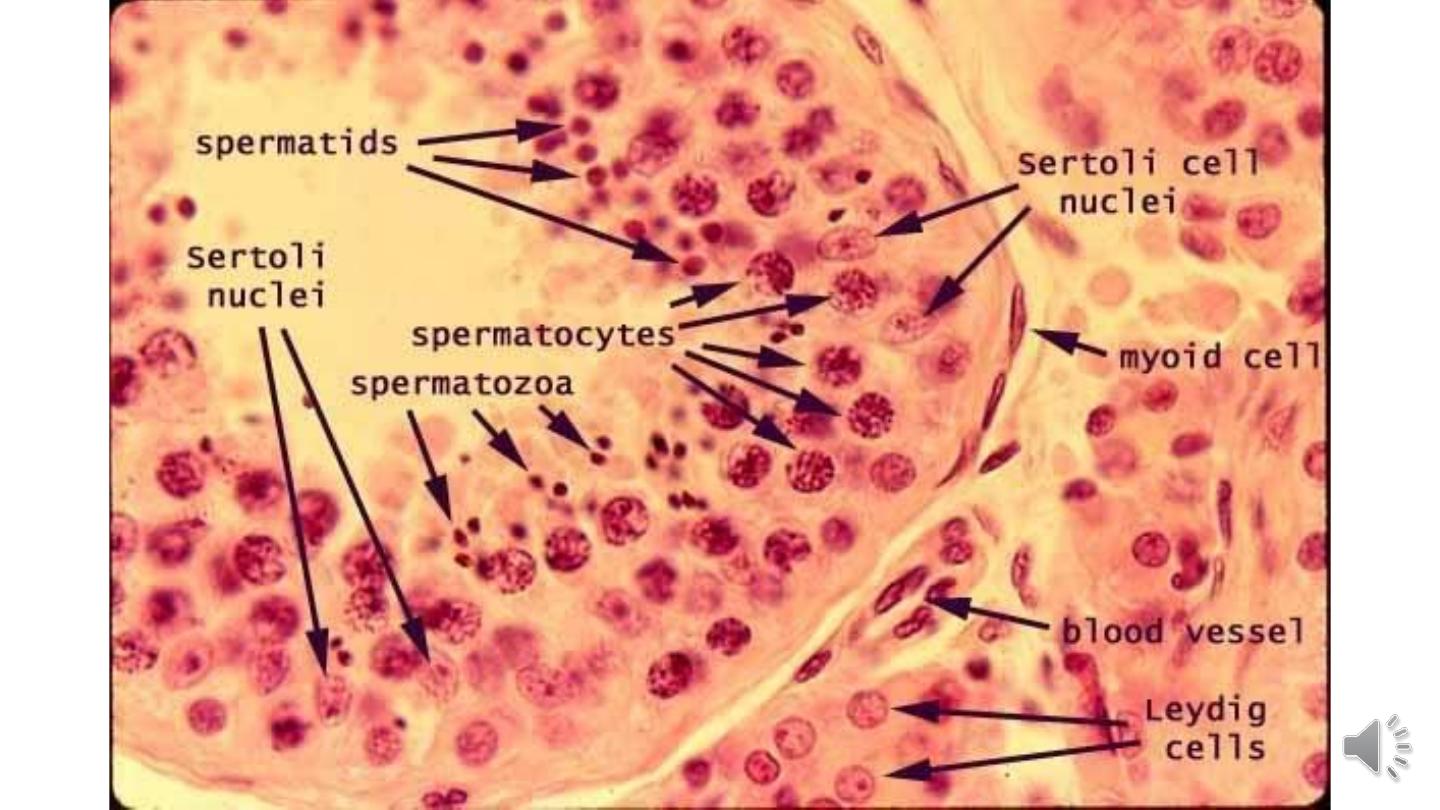
Microscopically
1- Arrest in the development of germ cells.
2- Marked hyalinization and thickening of the basement membrane of the spermatic
tubules.
3- Some tubules appear as dense cords of hyaline connective tissue outlined by prominent
basement membranes.
4- There is concomitant increase in interstitial stroma and Leydig cells are prominent.
Testicular Tumors
Testicular neoplasms are divided into two major categories:
1- Germ cell tumors.
2- Sex cord–stromal tumors.
Approximately 95% of testicular tumors arise from germ cells.
Most germ cell tumors are aggressive cancers capable of rapid, wide
dissemination, although with current therapy most can be cured.
Sex cord–stromal tumors, in contrast, are generally benign.
Pathologic Classification of Common Testicular Tumors
1. Germ Cell Tumors
Seminomatous tumors
Classical seminoma
Spermatocytic seminoma
Non-seminomatous tumors
Embryonal carcinoma,
Yolk sac (endodermal sinus) tumor
Choriocarcinoma
Teratoma
2. Sex Cord-Stromal Tumors
Leydig cell tumor
Sertoli cell tumor
Etiology.
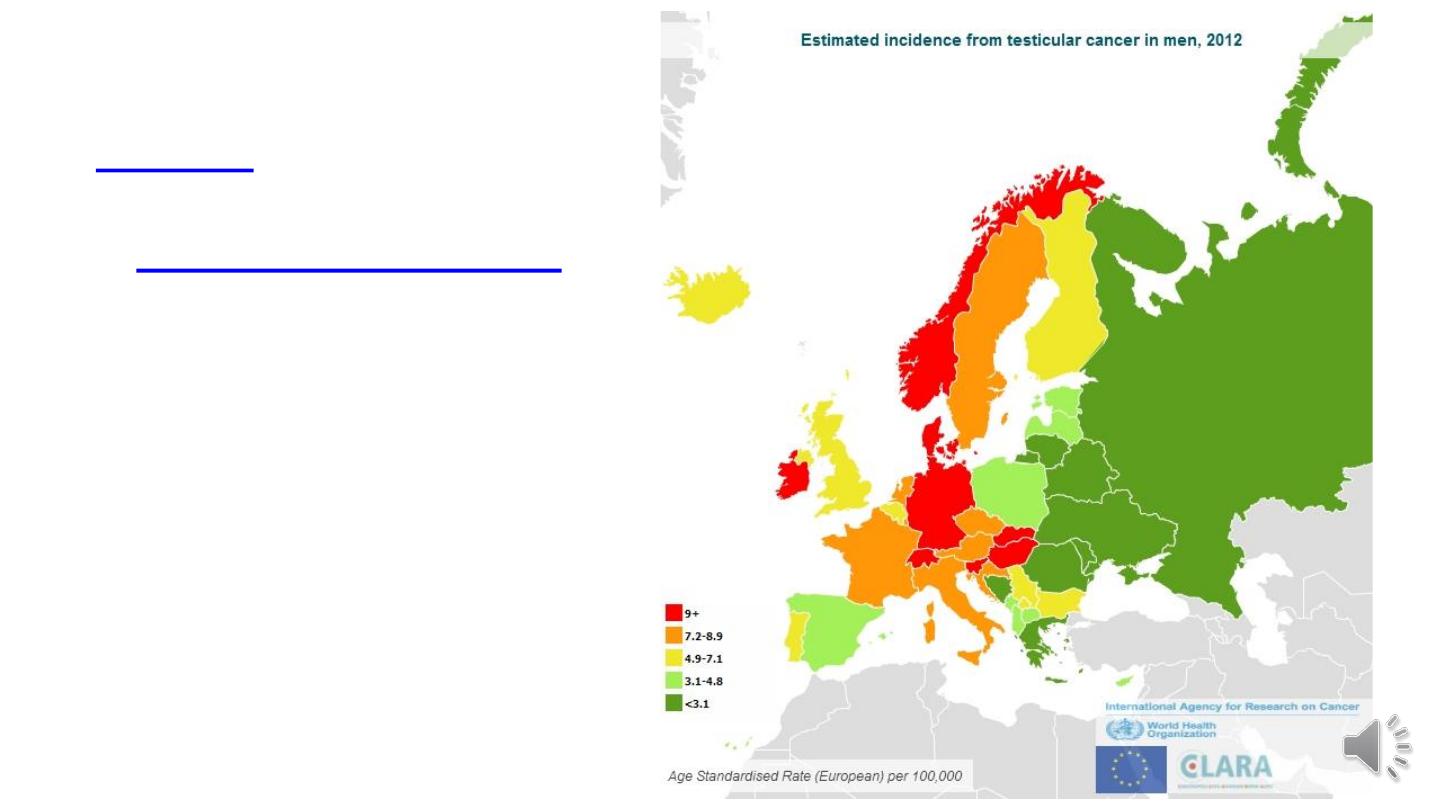
1. Environmental factors:
the incidence of testicular
germ
cell
tumors
in
Finland
is
about
two
times
lower
than
in
Sweden.
2. Testicular dysgenesis syndrome (TDS): testicular germ cell tumors are associated
with a spectrum of disorders known as
testicular dysgenesis syndrome (TDS).
This
syndrome includes cryptorchidism, hypospadias, and poor sperm quality.
3. Klinefelter syndrome: is associated with an increased risk (50 times greater than
normal) for the development of mediastinal germ cell tumors, but these patients do not
develop testicular tumors.
4. Family predisposition.
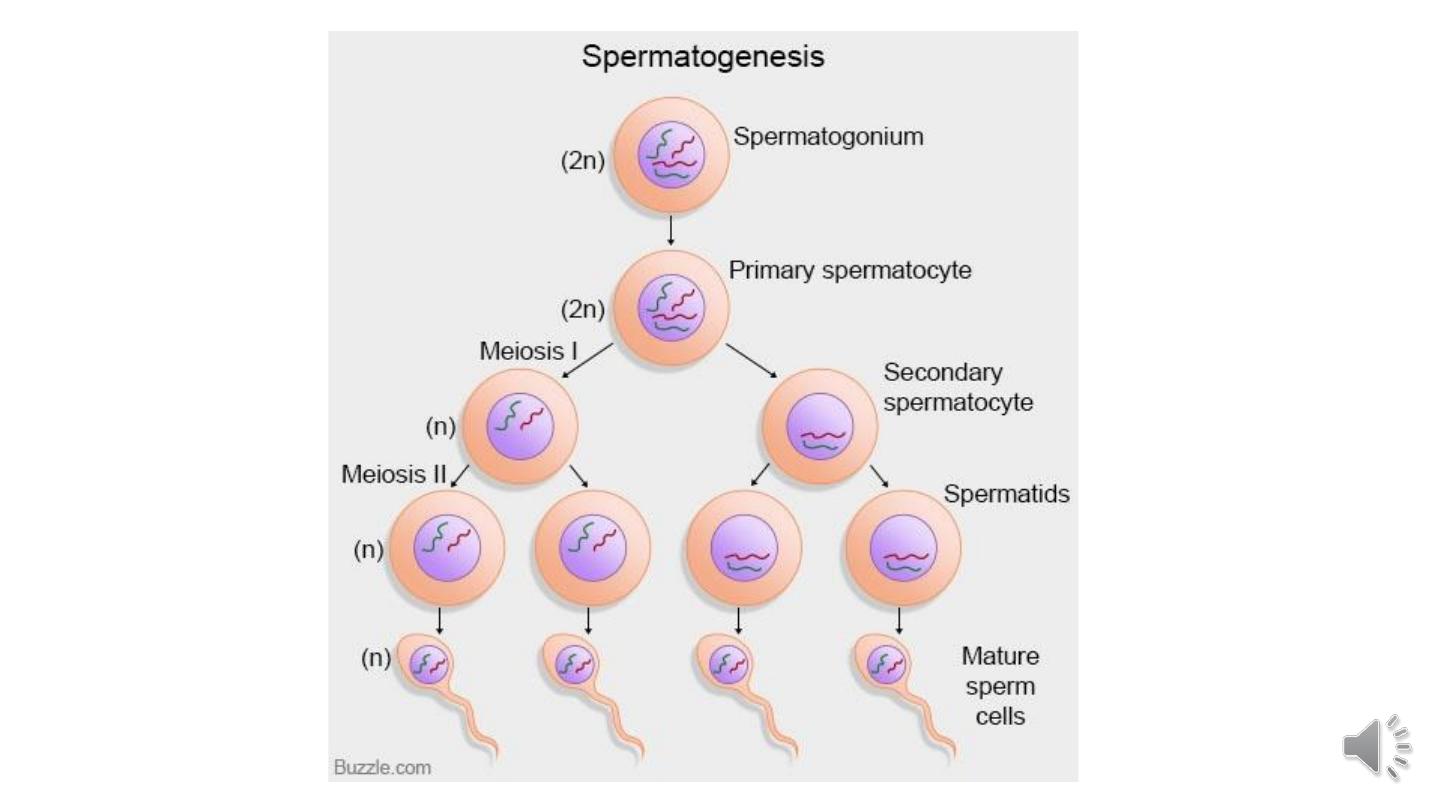
Germ cells tumors
Germ cell tumors are subdivided into seminomas and non-seminomas (teratoma, embryonal
carcinoma, choriocarcinoma, yolk sac tumor).
Clinical features of germ
cell testicular tumors.
1- Painless enlargement of
the testis is a characteristic
feature of germ cell
neoplasms,
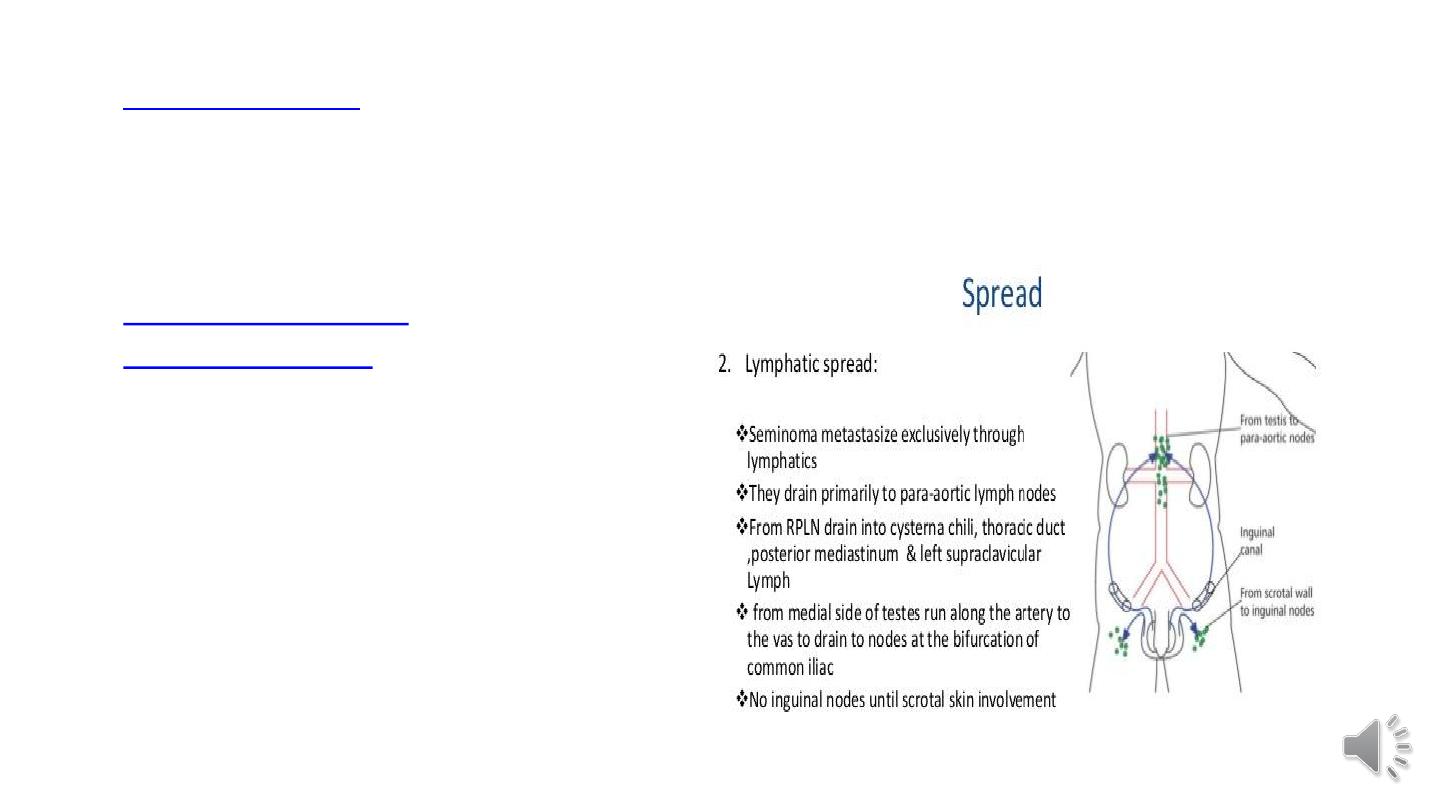
2- Retroperitoneal and
para-aortic nodes
enlargements. Subsequent
spread may occur to
mediastinal and
supraclavicular nodes.

3- Hematogenous spread is primarily to
the lungs, but liver, brain, and bones may
also be involved.
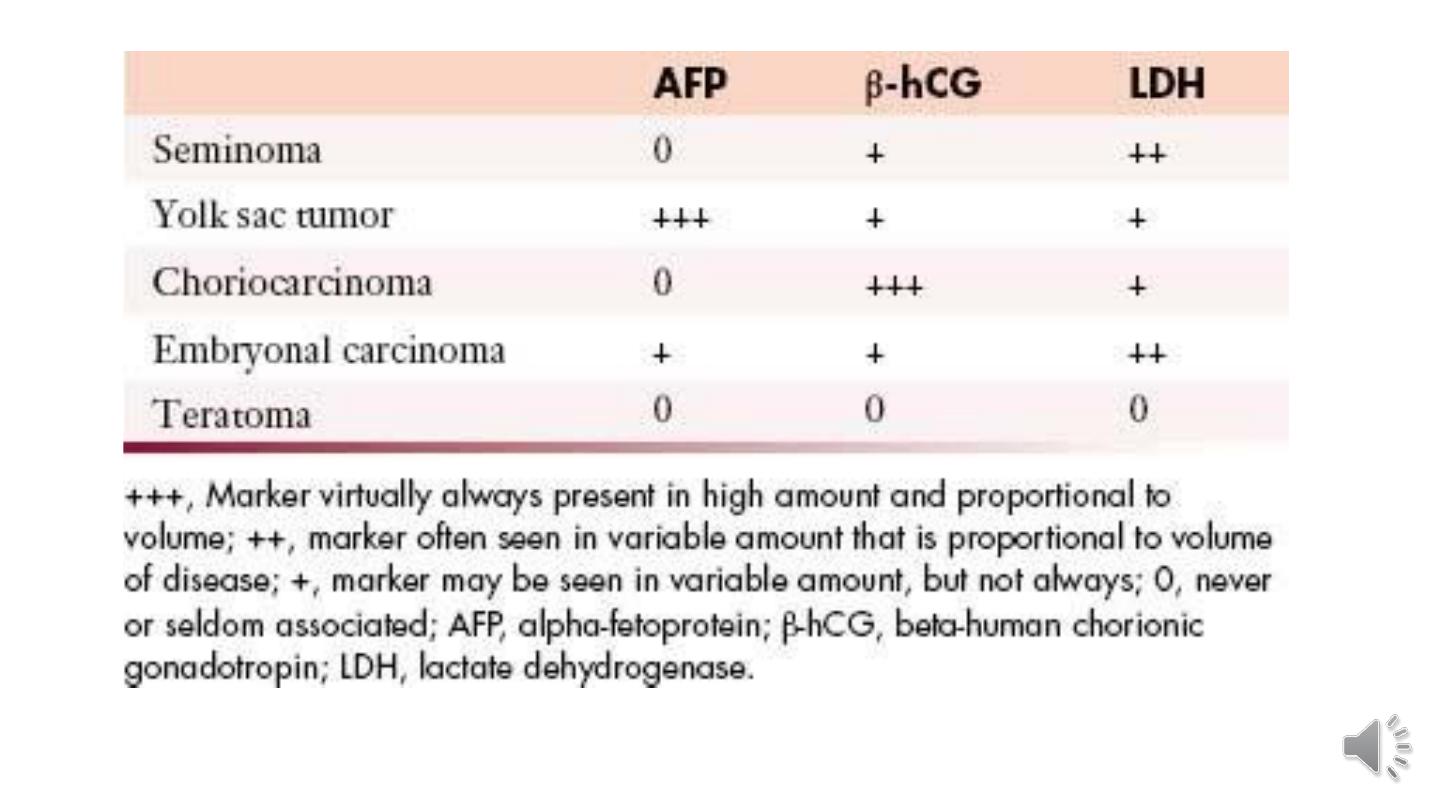
4- Germ cell tumors of the test is often
secrete polypeptide hormones and certain
enzymes that can be detected in blood by
sensitive assays, such biologic markers
include HCG, and AFP, which are valuable
in the diagnosis and management of
testicular cancer.

Seminoma
Seminomas are the most common type of germ cell tumor, making up about 50% of these tumors. The
peak incidence is the third decade and they almost never occur in infants. An identical tumor arises in the
ovary, where it is called dysgerminoma.
Morphology.
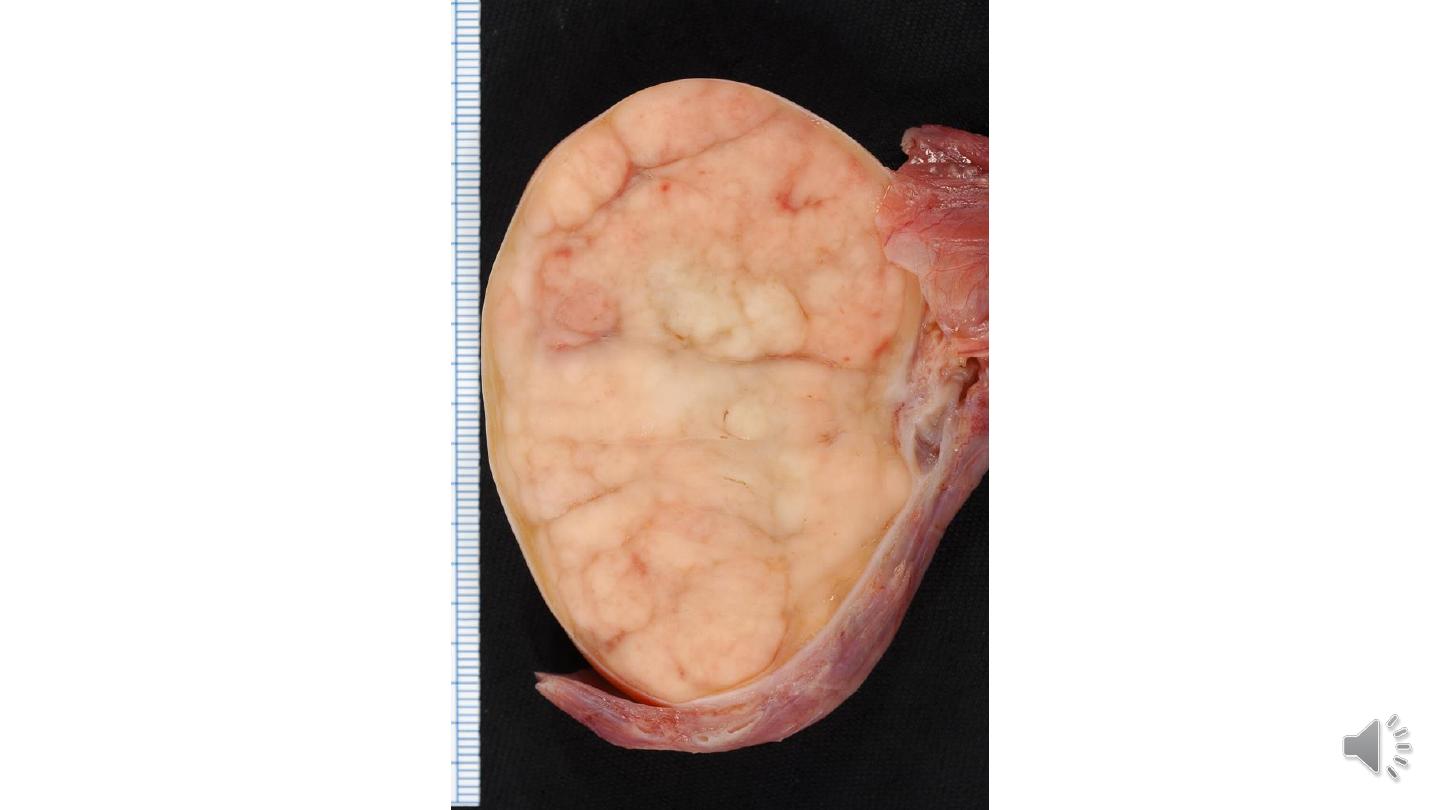
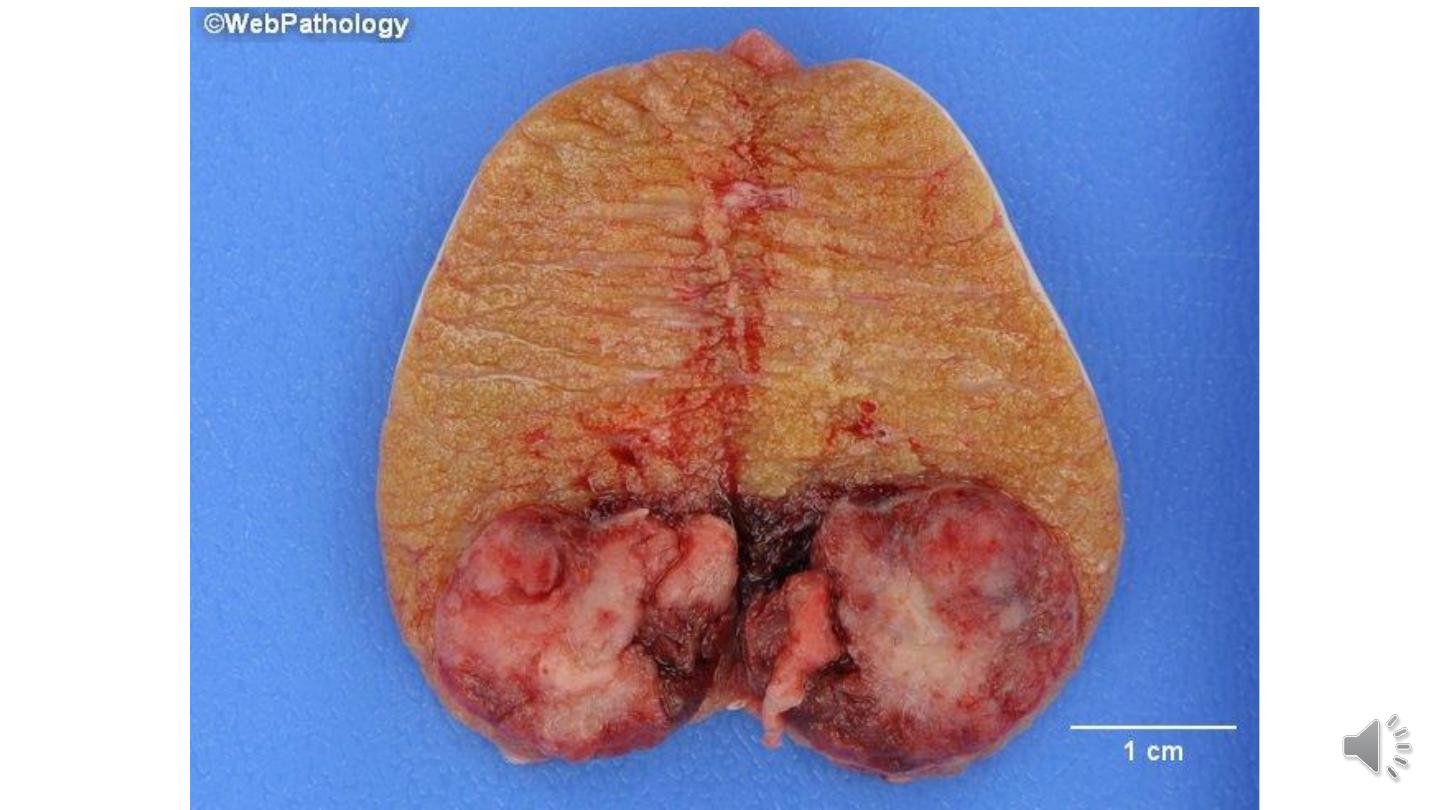
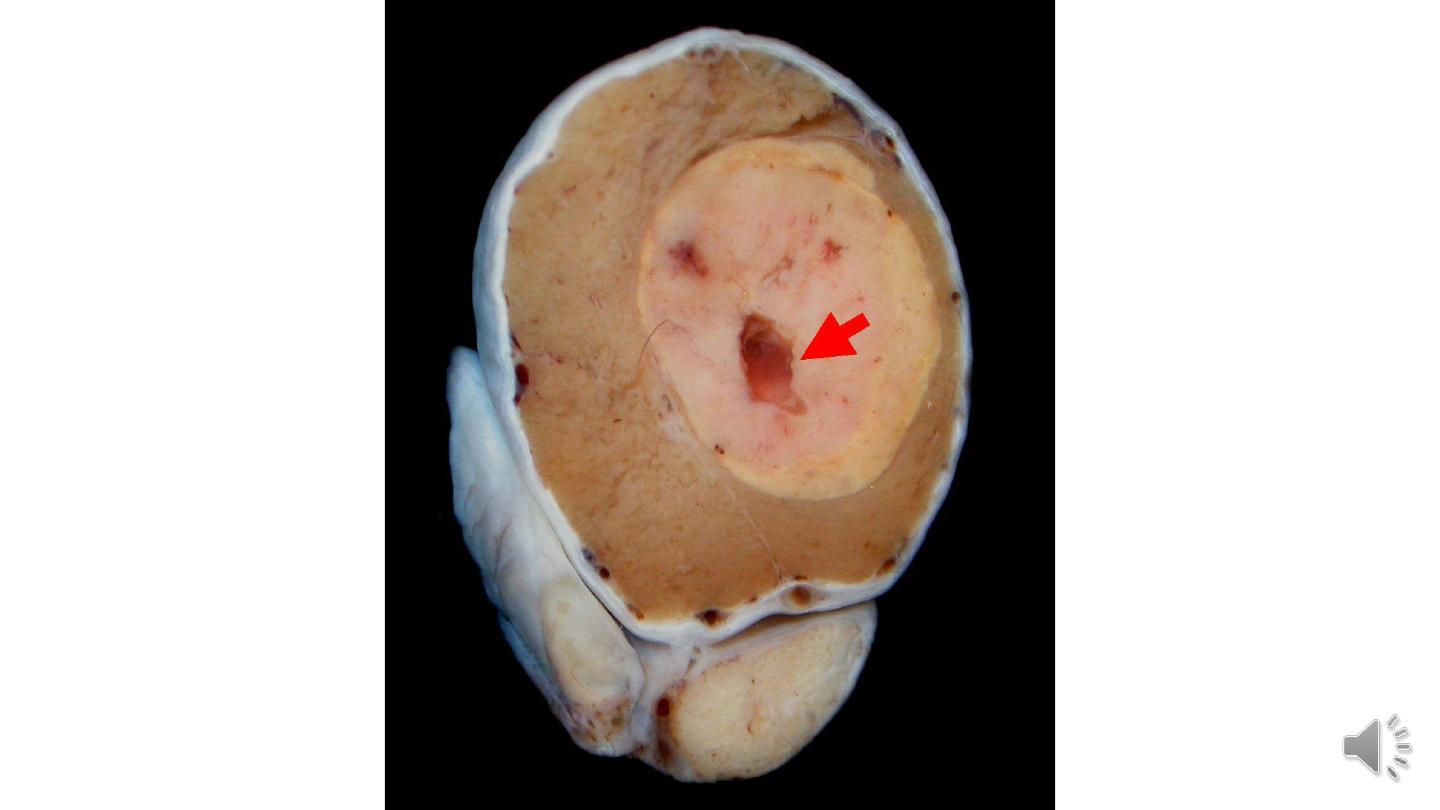
Grossly
1- Bulky masses.
2- Homogeneous, gray-white, lobulated cut surface, usually devoid of hemorrhage or necrosis.
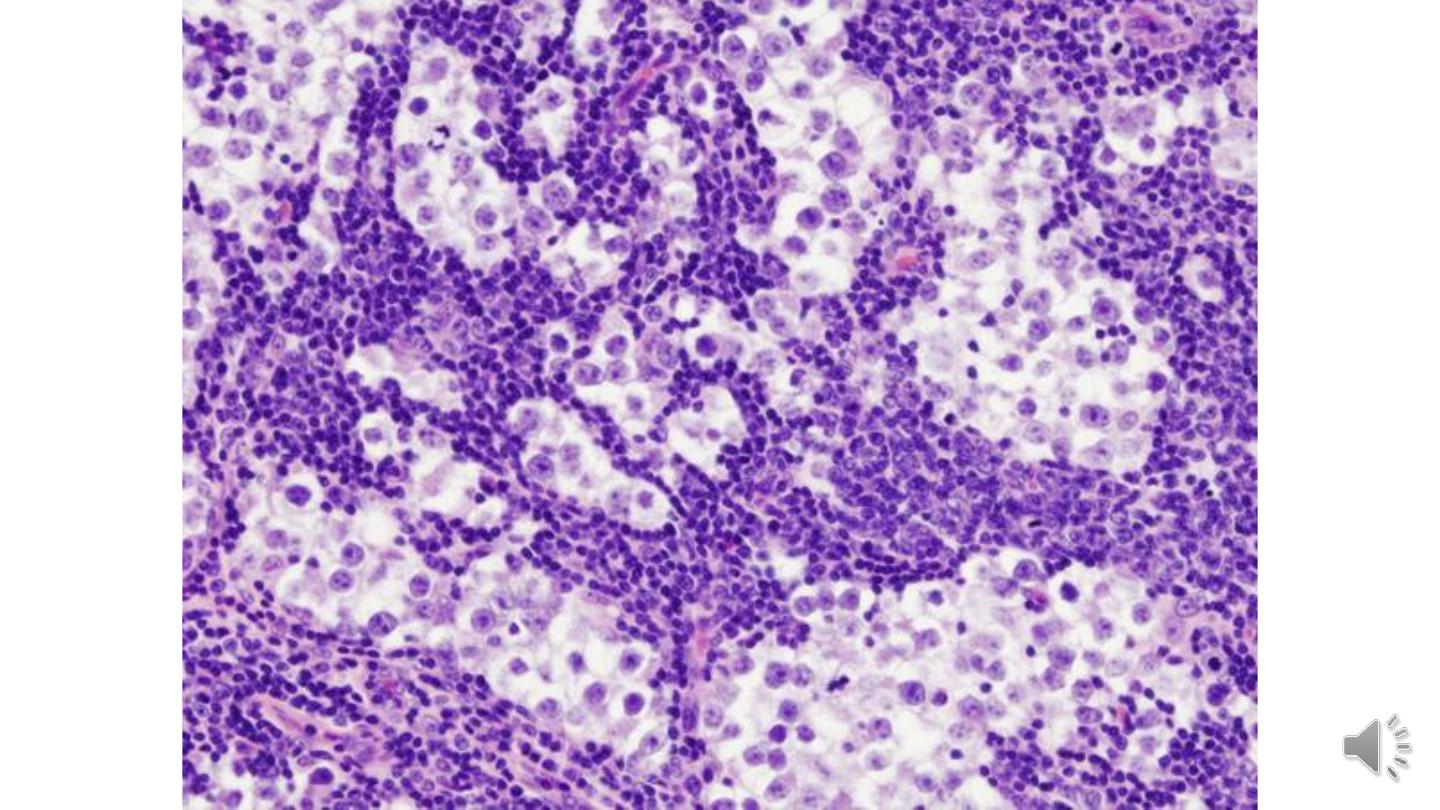
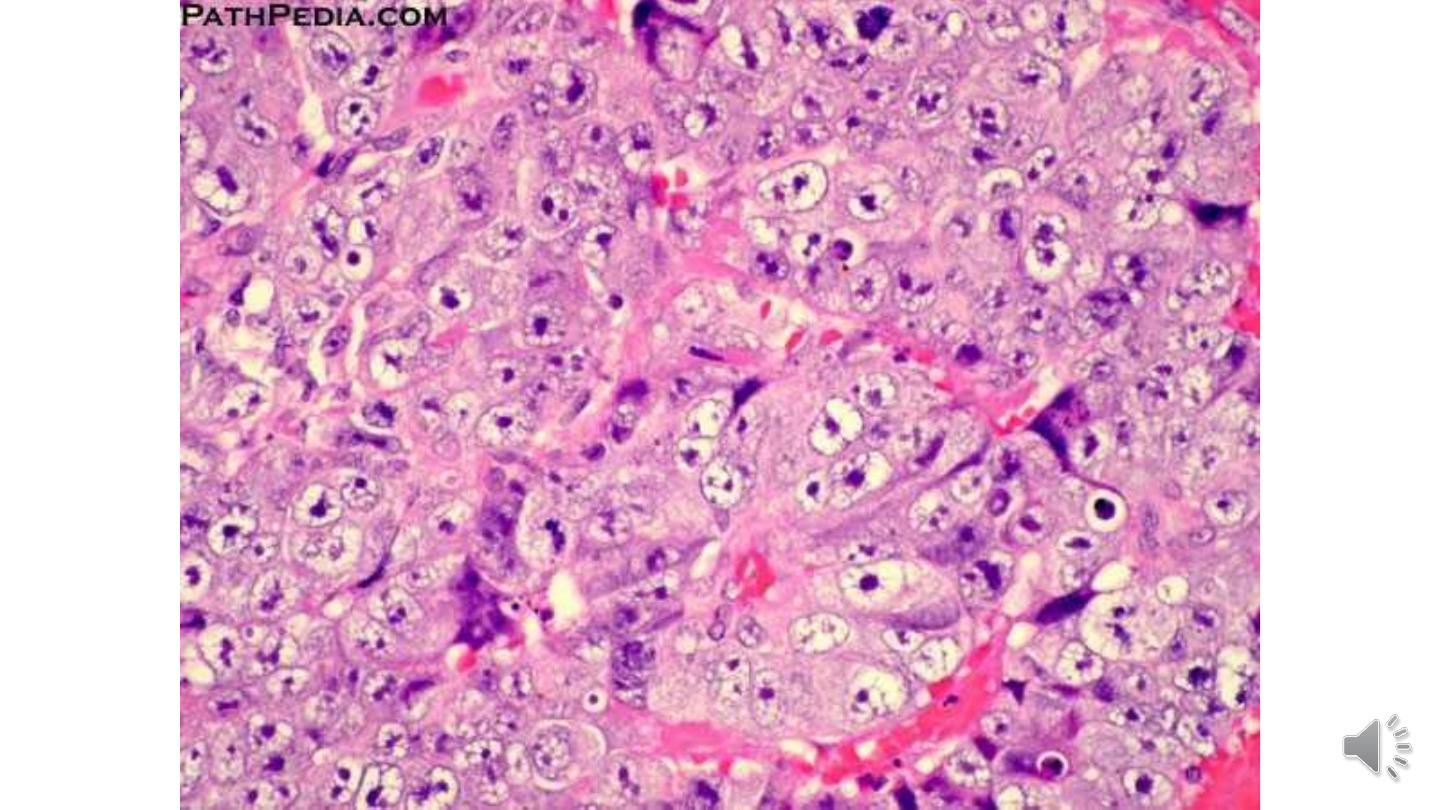
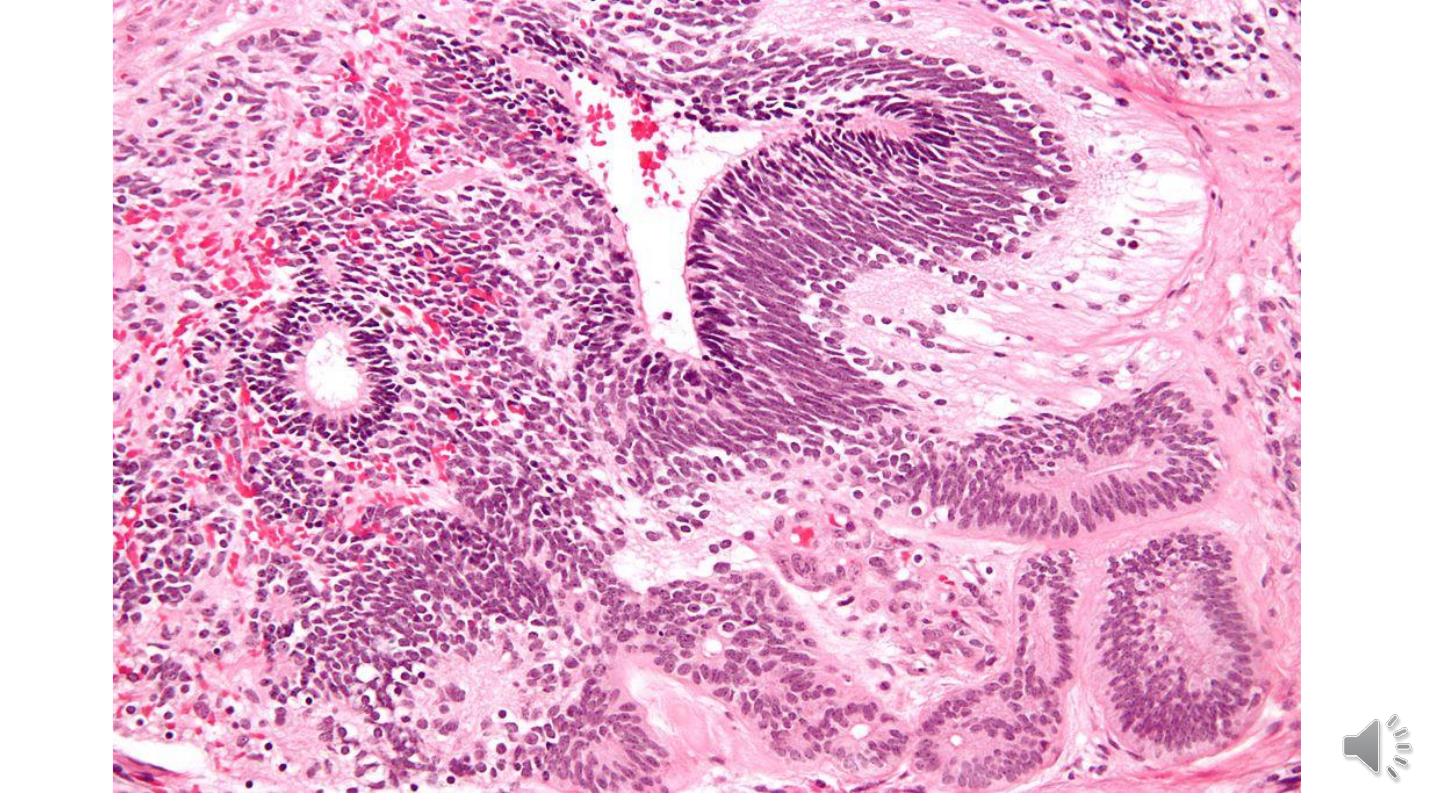
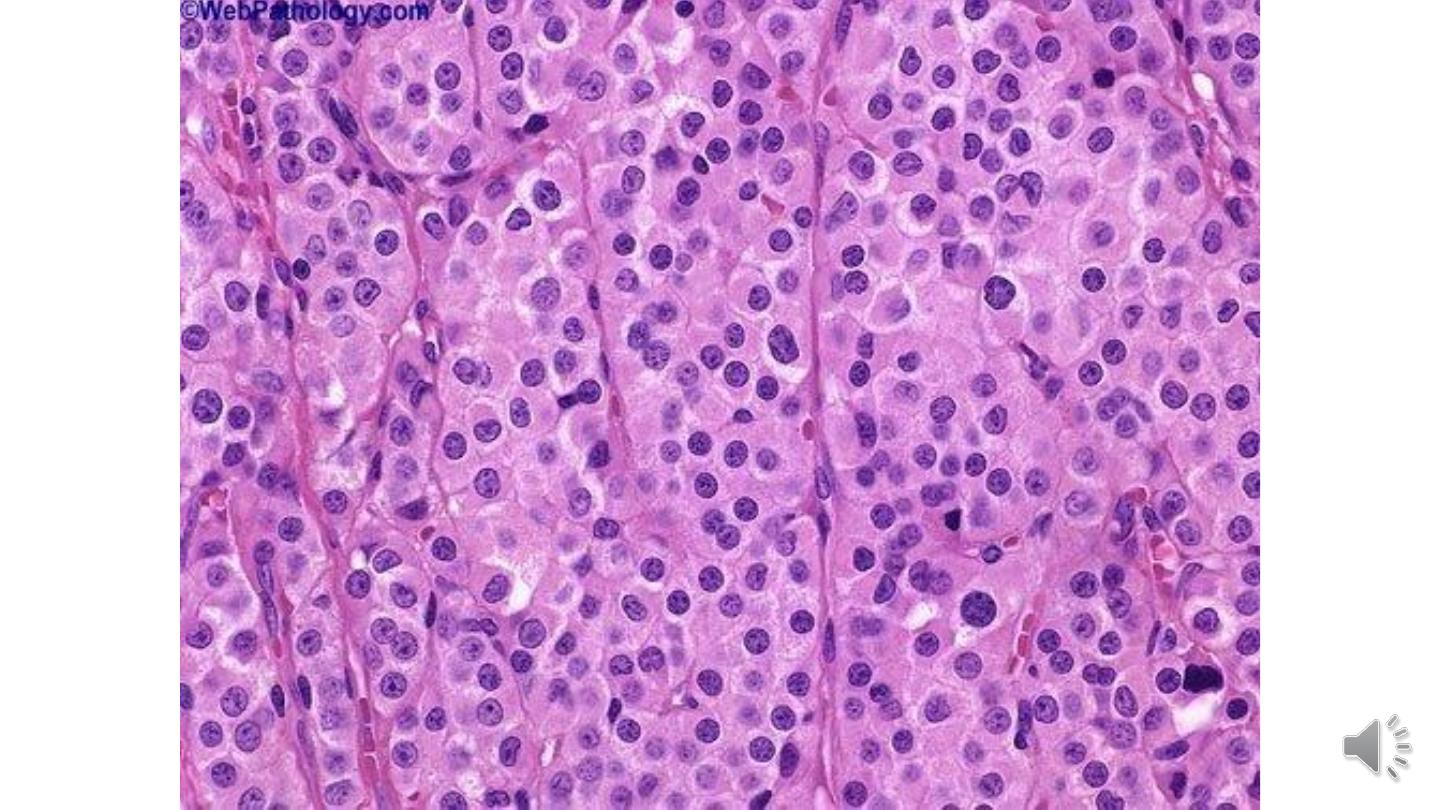
Microscopically
1- Sheets of uniform cells divided into poorly demarcated lobules by delicate septa of fibrous tissue
containing a moderate amount of lymphocytes.
2- Seminoma cell is large and round to polyhedral and has a distinct cell membrane, a clear or watery-
appearing cytoplasm; and a large, central nucleus with one or two prominent nucleoli.
Embryonal Carcinoma
Embryonal carcinomas occur mostly in the 20- to 30-year age group. These tumors are more
aggressive than seminomas.
Morphology.
Grossly
1- The tumor is smaller than seminoma and usually does not replace the entire testis.
2-On cut surfaces the mass is often variegated, poorly demarcated, and punctuated by foci of
hemorrhage or necrosis.
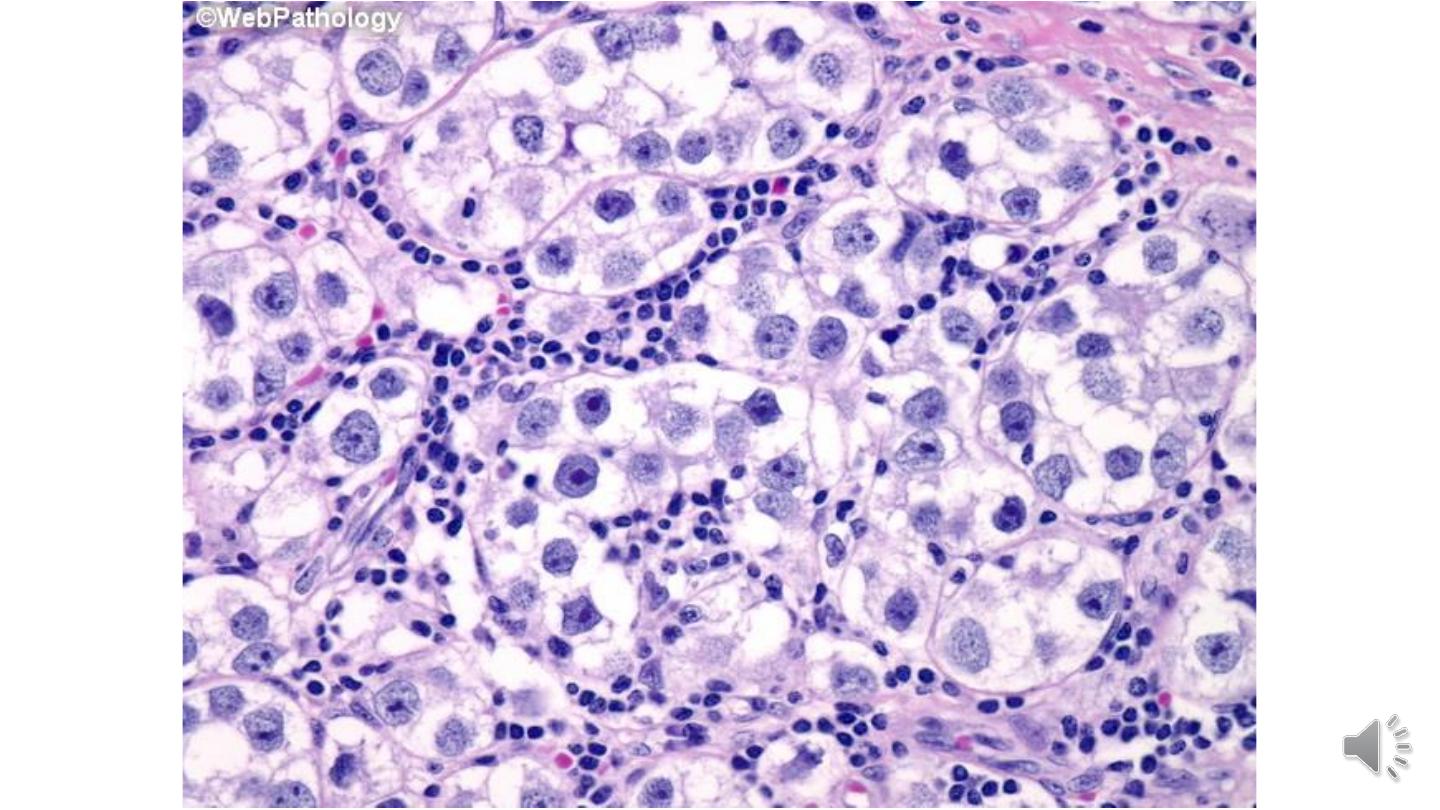
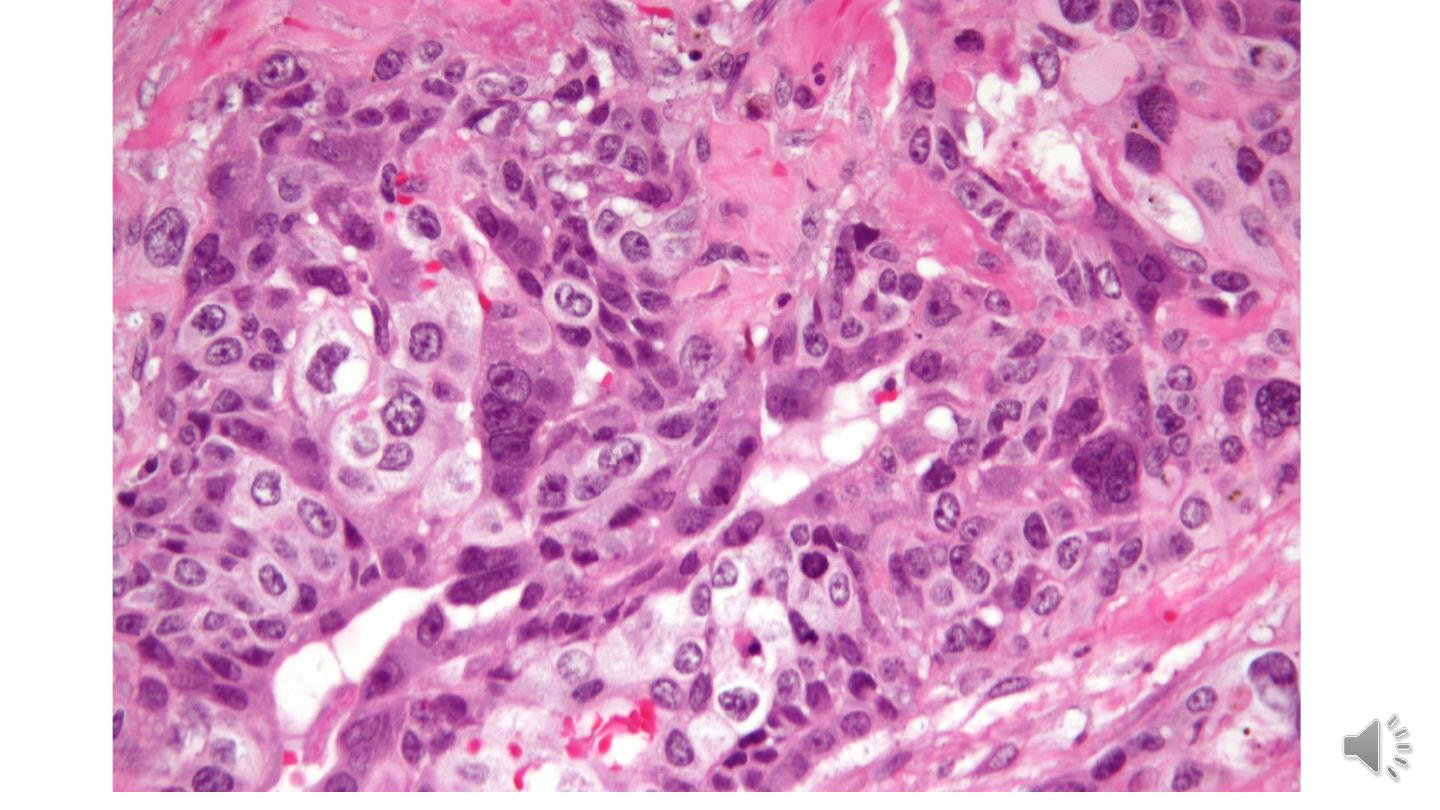
Microscopically
1- The cells grow in alveolar or tubular patterns, sometimes with papillary convolutions
2- More undifferentiated lesions may display sheets of cells.
3- The neoplastic cells are large and anaplastic, and have hyperchromatic to vesicular nuclei with
prominent nucleoli, the cell borders are usually indistinct, and there is considerable variation in cell
and nuclear size and shape.

Yolk Sac Tumor
Also known as endodermal sinus tumor.
It is the most common testicular tumor in infants and children up to 3 years of age. In this age group it has a
very good prognosis.
In adults the pure form of this tumor is rare; instead, yolk sac elements frequently occur in combination with
embryonal carcinoma.
Morphology.
Grossly
1- The tumor is non encapsulated,
2- On cross-section it presents a homogeneous, yellow-white, mucinous appearance.
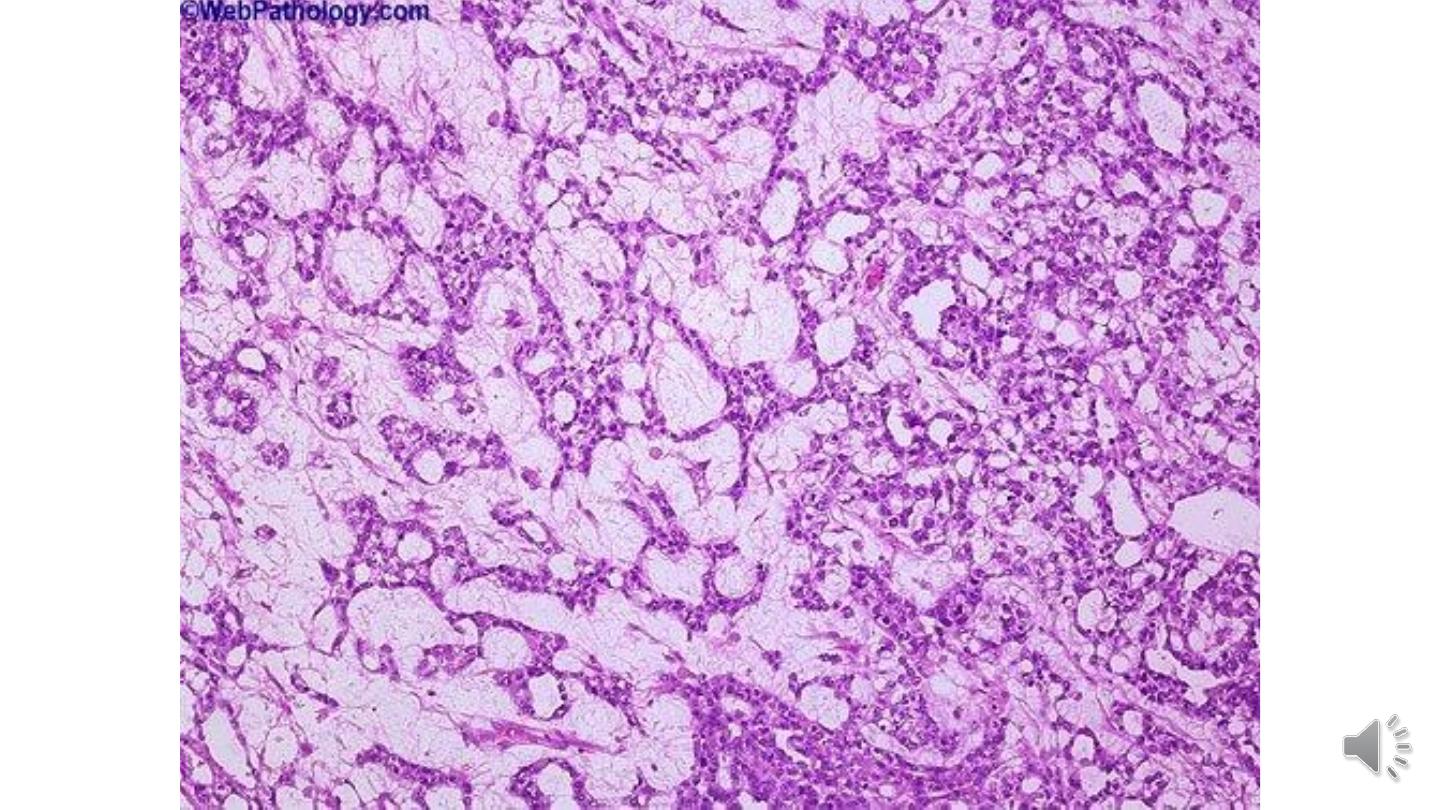
Microscopically
1- A lacelike (reticular) network of medium-sized cuboidal or flattened cells.
2- Papillary structures, solid cords of cells
3- In approximately 50% of tumors, structures resembling endodermal sinuses (Schiller-Duval bodies) may be
seen; these consist of a core with a central capillary and a visceral and parietal layer of cells resembling
primitive glomeruli.


Choriocarcinoma
Choriocarcinoma is a highly malignant form of testicular tumor. In its “pure” form choriocarcinoma is rare,
constituting less than 1% of all germ cell tumors.
Morphology.
Grossly
1- Often they cause no testicular enlargement and are detected only as a small palpable nodule.
2- Typically, these tumors are small, rarely larger than 5 cm in diameter.
3- Hemorrhage and necrosis are extremely common.
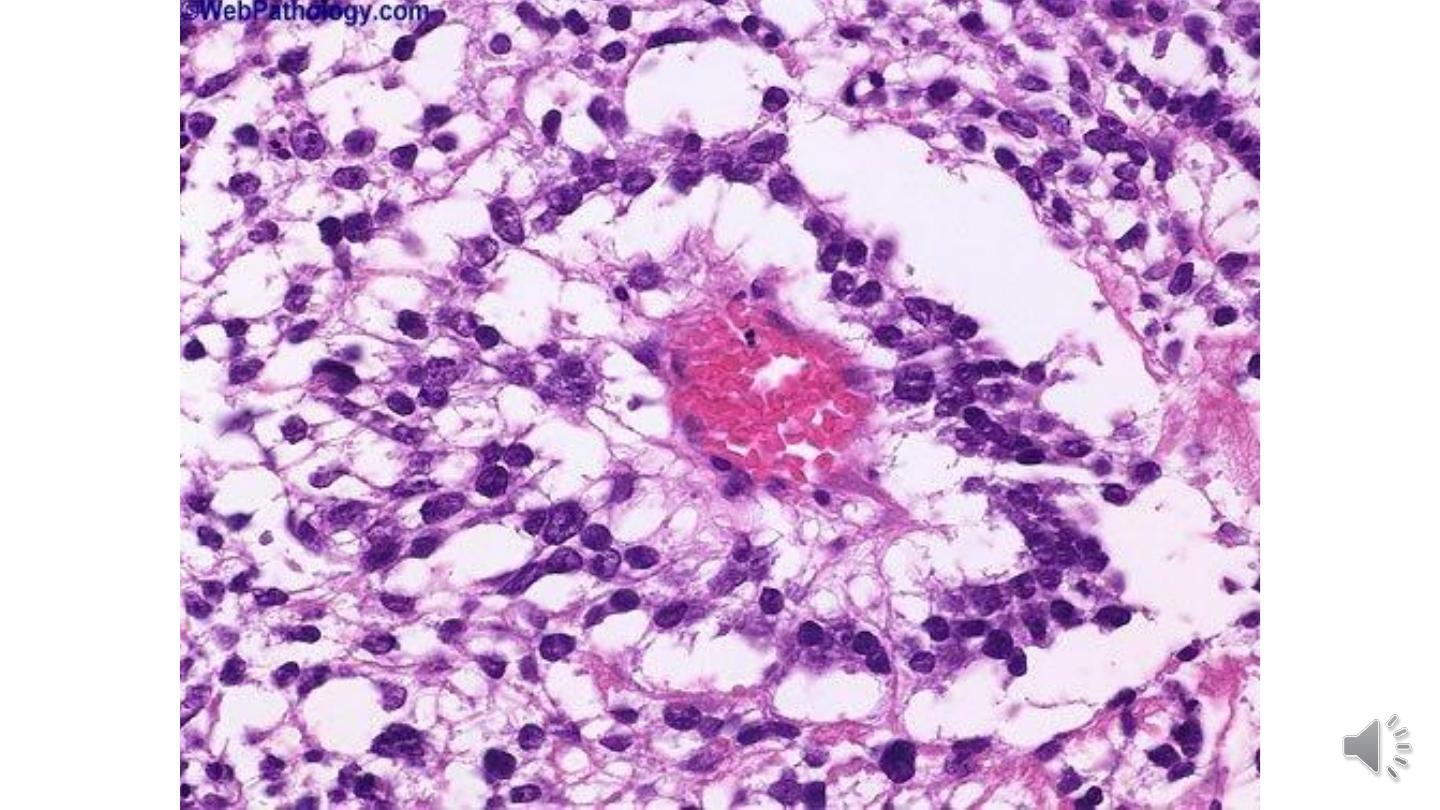
Microscopically
The tumors contain two cell types:
The syncytiotrophoblastic cells are large and have many hyperchromatic nuclei and an abundant eosinophilic
vacuolated cytoplasm.
The cytotrophoblstic cells are more regular and tend to be polygonal, with distinct borders and clear cytoplasm; and
have a single, fairly uniform nucleus, they grow in cords or masses


Teratoma
Teratoma may occur at any age from infancy to adult life.
Pure forms of teratoma are common in infants and children.
In adults, pure teratomas are rare, constituting 2% to 3% of germ cell tumors. However, the frequency of teratomas
mixed with other germ cell tumors is approximately 45%.
In the child, differentiated mature teratomas usually follow a benign course.
In the postpubertal male all teratomas are regarded as malignant, capable of metastatic behavior whether the elements
are mature or immature.
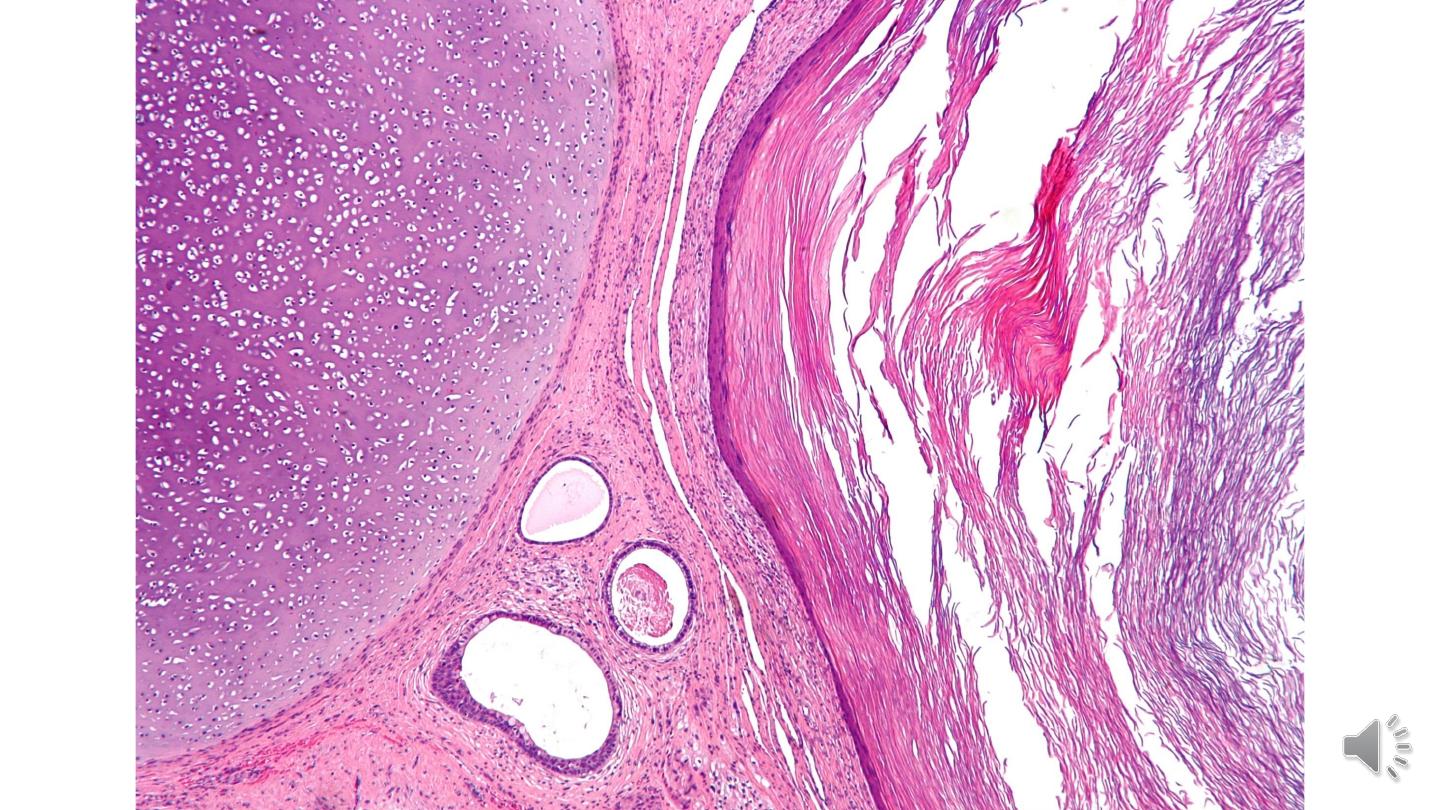
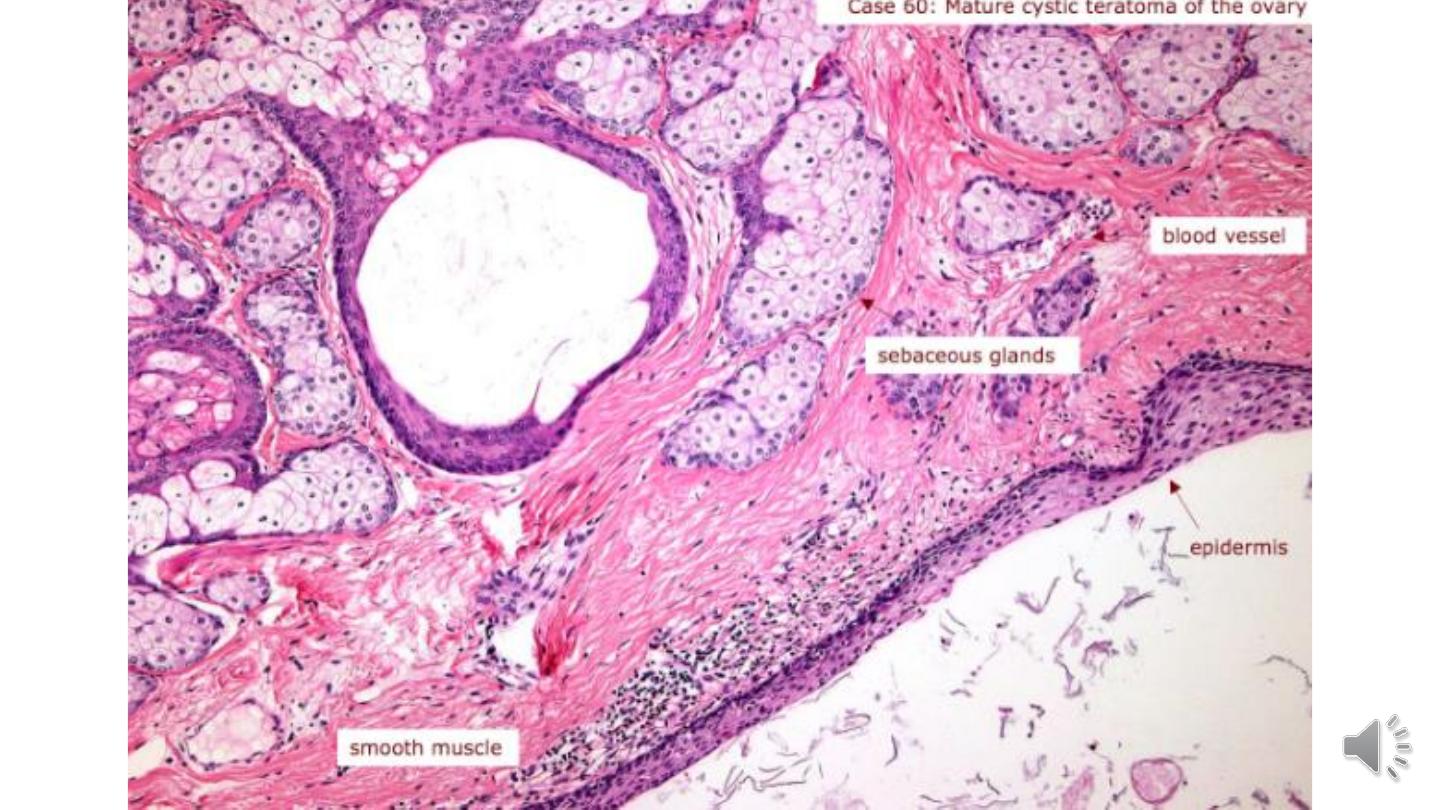
Morphology.
Grossly
1- Usually large, ranging from 5 to 10 cm in diameter.
2- The appearance is heterogeneous with solid, sometimes cartilaginous, and cystic areas.
3-Hemorrhage and necrosis usually indicate admixture with embryonal carcinoma, choriocarcinoma, or both.


Microscopically
1- Teratomas are composed of a heterogeneous collection of neural tissue, muscle
bundles, islands of cartilage, clusters of squamous epithelium, thyroid gland,
bronchial or bronchiolar epithelium, and intestinal wall or brain substance, all
embedded in a fibrous or myxoid stroma.
2- Elements may be mature (resembling various adult tissues) or immature (sharing
histologic features with fetal or embryonal tissue).
3- Rarely, a malignant non–germ cell tumors may arise in teratoma. This phenomenon
is referred to as “teratoma with malignant transformation,” where there is
malignancy in derivatives of one or more germ cell layers. Thus, there may be a focus
of squamous cell carcinoma, adenocarcinoma, or sarcoma.
Prognosis of testicular germ cell tumors
Prognosis of testicular germ cell tumors depend
largely on clinical stage and on the histologic
type.
Seminoma, which is extremely radiosensitive and
tends to remain localized for long periods, has the
best prognosis.
Pure choriocarcinoma has a poor prognosis.
Sex Cord-Stromal Tumors
The two most important members of this group—Leydig cell tumors and Sertoli cell
tumors.
Leydig Cell Tumors
They may arise at any age, although most cases occur between 20 and 60 years of age.
The most common presenting feature is testicular swelling. Tumors of Leydig cells
may secrete androgens and in some cases both androgens and estrogens, and even
corticosteroids. In some patients gynecomastia may be the first symptom in children,
Most are benign.
Approximately 10% of the tumors in adults are invasive and produce metastases.

Morphology.
Grossly
1-These neoplasms form circumscribed nodules, usually less than 5 cm
in diameter.
2-They have a distinctive golden brown, homogeneous cut surface.
Histologically
1- Neoplastic Leydig cells usually are large and round or polygonal
2- Neoplastic cells have an abundant granular eosinophilic cytoplasm
with a round central nucleus.
3-The cytoplasm frequently contains lipid granules, vacuoles, or
lipofuscin pigment.


Thank You
Thank You
