
Urinary tract pathology
Lecture 1
Renal and urothelial carcinoma
Dr.Ahmed Raji
F.I.C.M.Path
College of Medicine - University of Babylon
6.7.2020

Renal carcinoma

Renal cell carcinomas represent about 3% of all newly diagnosed visceral cancers
in the United States and account for 85% of renal cancers in adults.
There are approximately 30,000 new cases per year and 12,000 deaths from the
disease.
The tumors occur most often in older individuals, usually in the sixth and seventh
decades of life, and show a 2: 1 male preponderance.
These
tumors
arise
from
tubular
epithelium
and
are
therefore
renal
adenocarcinomas.

Risk factors:
1. Tobacco is the most significant risk factor.
2. Obesity (particularly in women).
3. Hypertension.
4. Unopposed estrogen therapy.
5. Asbestos.
6. Petroleum products, and heavy metals.
7. Chronic renal failure and acquired cystic disease.
8. Tuberous sclerosis.
9. Familial.

Classification of renal cell carcinoma:
The classification of renal cell carcinoma is based on correlative cytogenetic, genetic, and histologic
studies.
The major types of tumor are as follows:
1.
Clear cell carcinoma.
This is the most common type, accounting for 70% to 80% of
renal cell cancers. The tumors are made up of cells with clear or granular cytoplasm and are
nonpapillary. In most cases (95%) are sporadic.
2.
Papillary carcinoma
accounts for 10% to 15% of renal cancers. It is characterized by a
papillary growth pattern and also occurs in both familial and sporadic forms.
3.
Chromophobe renal carcinoma
represents 5% of renal cell cancers and is composed of
cells with prominent cell membranes and pale eosinophilic cytoplasm, usually with a halo around the
nucleus.
4.
Collecting duct carcinoma
represents approximately 1% or less of renal epithelial
neoplasms. They arise from collecting duct cells in the medulla.
Clinical Features
The three classic diagnostic features of renal cell carcinoma are:
1. Costovertebral pain.
2. Palpable mass.
3. Hematuria.
But these are seen in only 10% of cases.
The most reliable of the three is
hematuria
, it is
usually intermittent and may be microscopic.
The tumor may remain silent until it attains a
large size. At this time it is often associated with
generalized constitutional symptoms, such as
fever (fever of unknown origin, FUO)
, malaise,
weakness, and weight loss.
So the tumor may have reached a diameter of
more than 10 cm when it is first discovered.
Currently, an increasing number of tumors are
being discovered in the
asymptomatic state
by
incidental radiologic studies (e.g., computed
tomographic
scan
or
magnetic
resonance
imaging)
usually
performed
for
non-renal
indications.
Etiology of fever of unknown origin (FUO)
Renal cell carcinomas produce a number of paraneoplastic syndromes due to
abnormal hormone production, including
polycythemia
, and
Hypercalcemia
.

One of the common characteristics of this tumor is its tendency to metastasize widely before giving rise to any
local symptoms or signs.
In 25% of new patients with renal cell carcinoma, there is radiologic evidence of metastases
at the time of
presentation
.
The most common locations of metastasis are the
lungs
(more than 50%) and
bones
(33%).
The average 5-year survival rate of persons with renal cell carcinoma is about 45% and as high as 70% in
the absence of distant metastases.

Metastatic renal cell carcinoma to femure

Metastatic renal cell carcinoma to hand bones
Morphology.
Gross
Renal cell carcinomas may arise in any portion of the kidney, but more commonly affects
the poles.
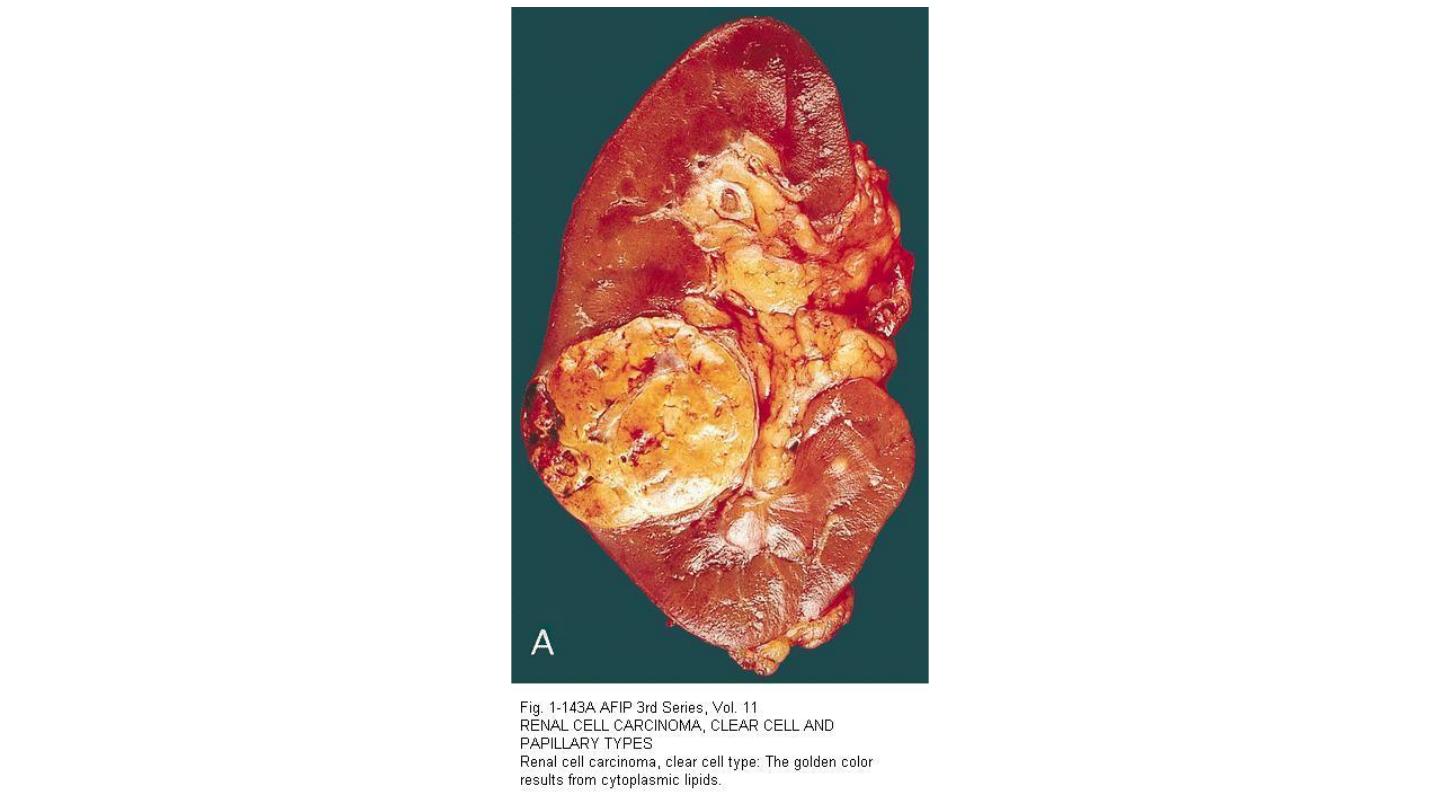
Clear cell carcinomas:
Solitary unilateral lesions.
Spherical masses.
Variable sizes.
Bright yellow-gray-white tissue.
Large areas of ischemic, gray-white necrosis, and foci of hemorrhagic discoloration.
The margins are usually sharply defined and confined within the renal capsule.
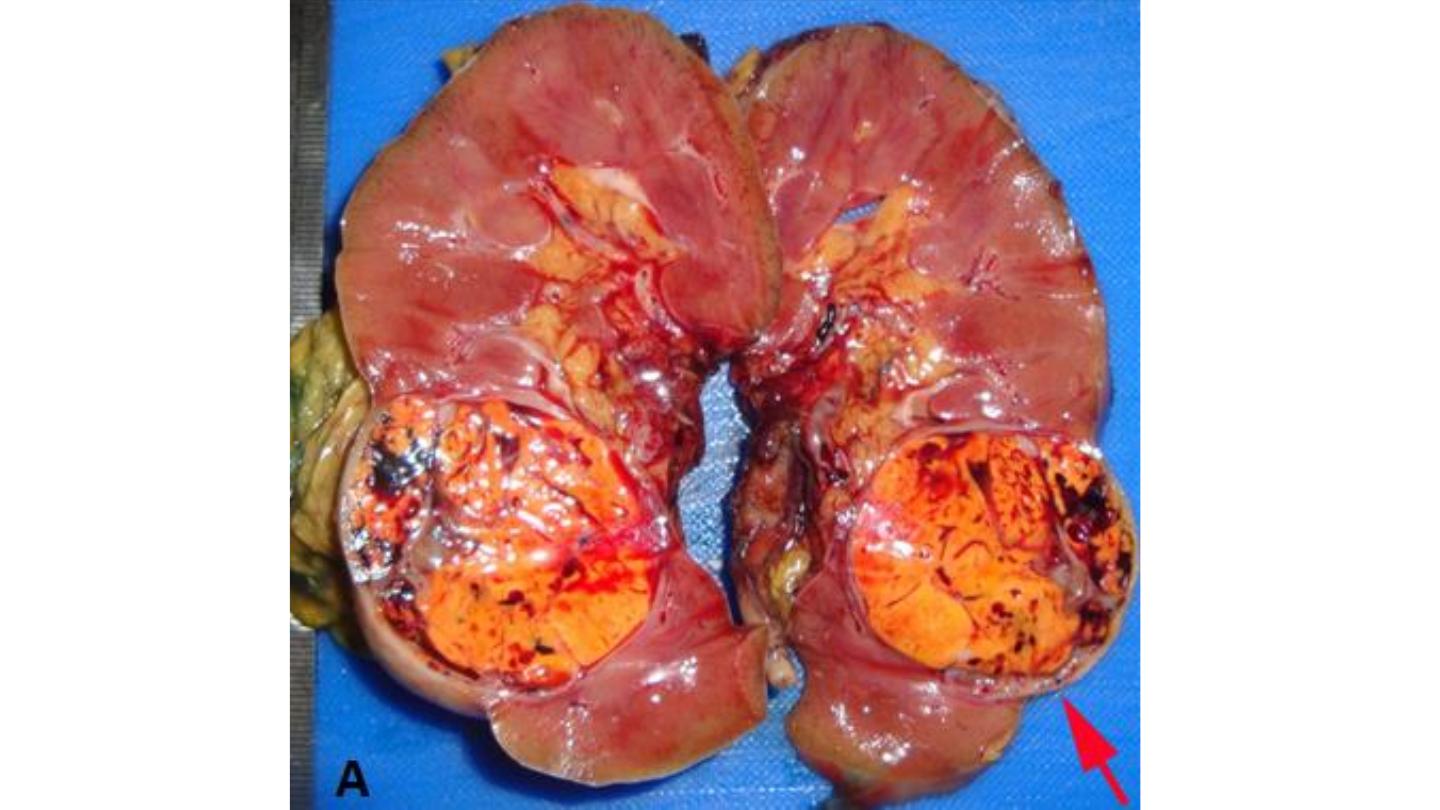
Papillary renal cell carcinoma
Can be multifocal and bilateral.
Hemorrhagic and cystic.
Microscopical
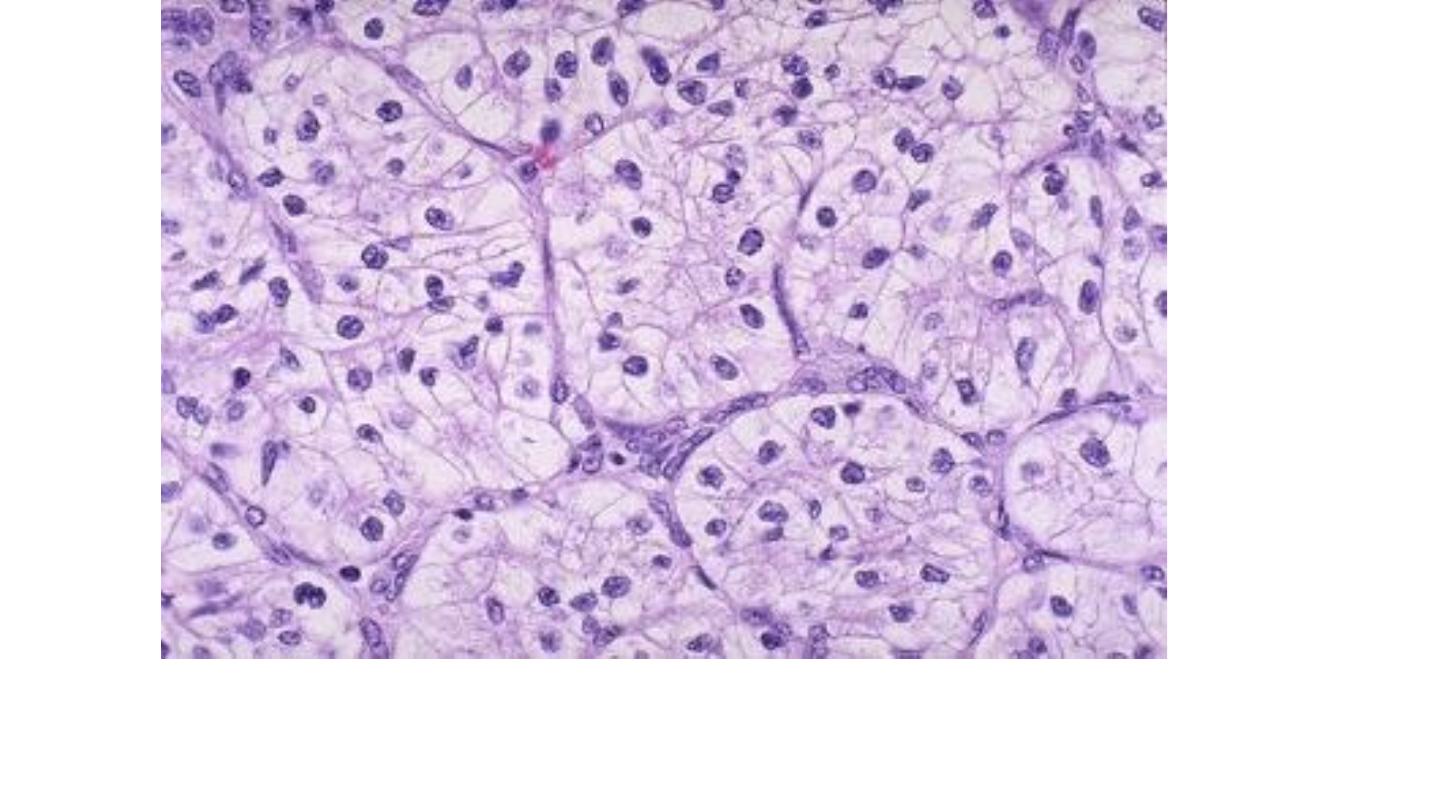
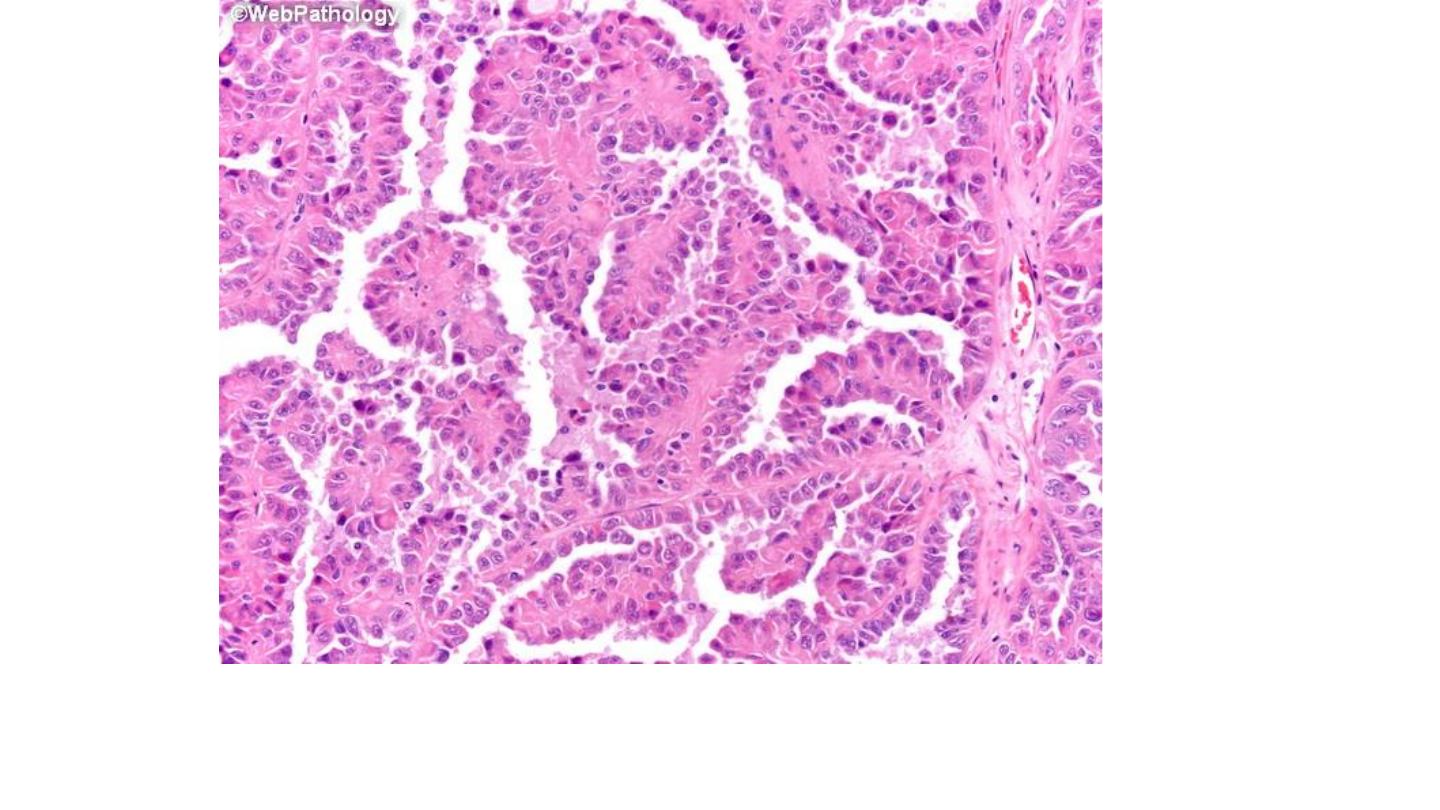
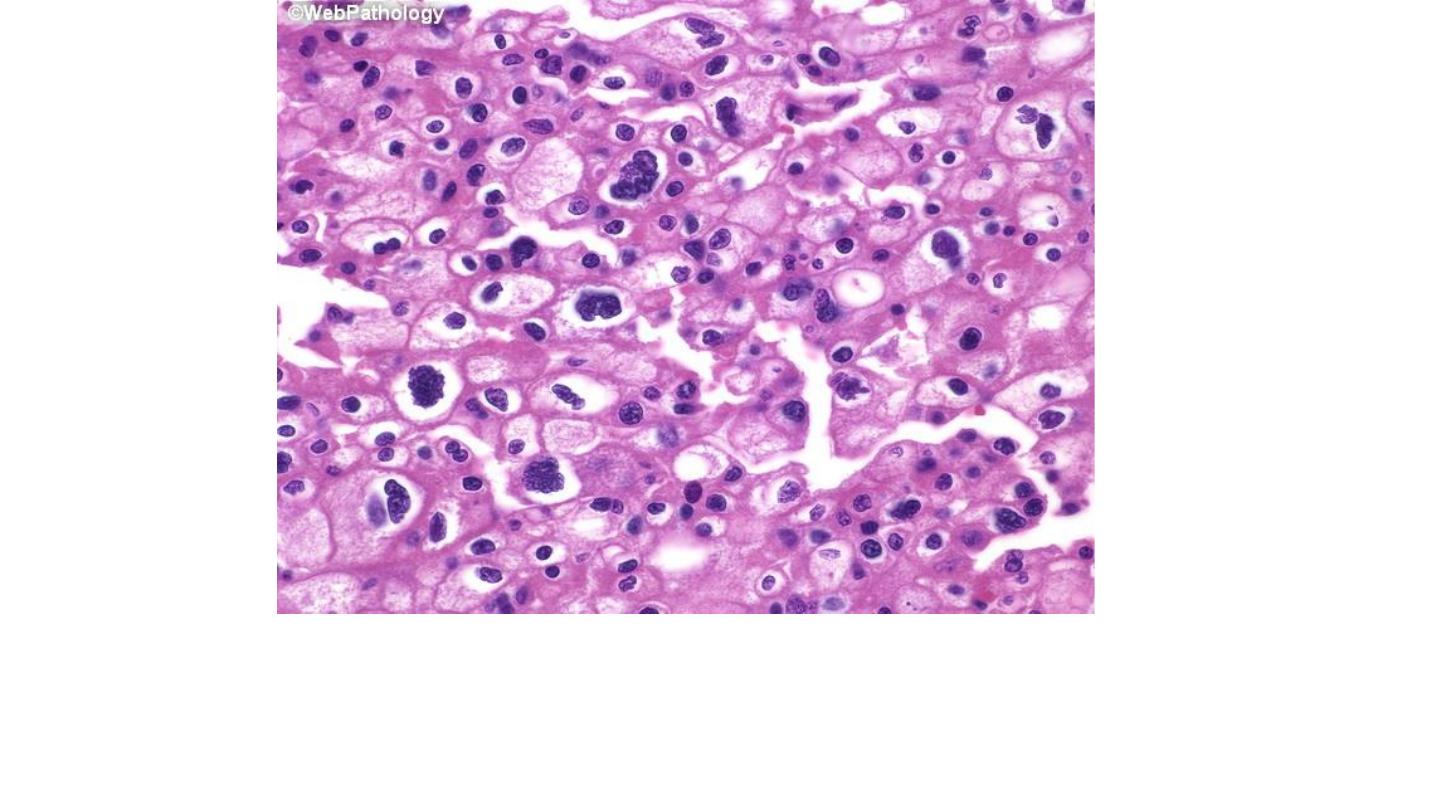
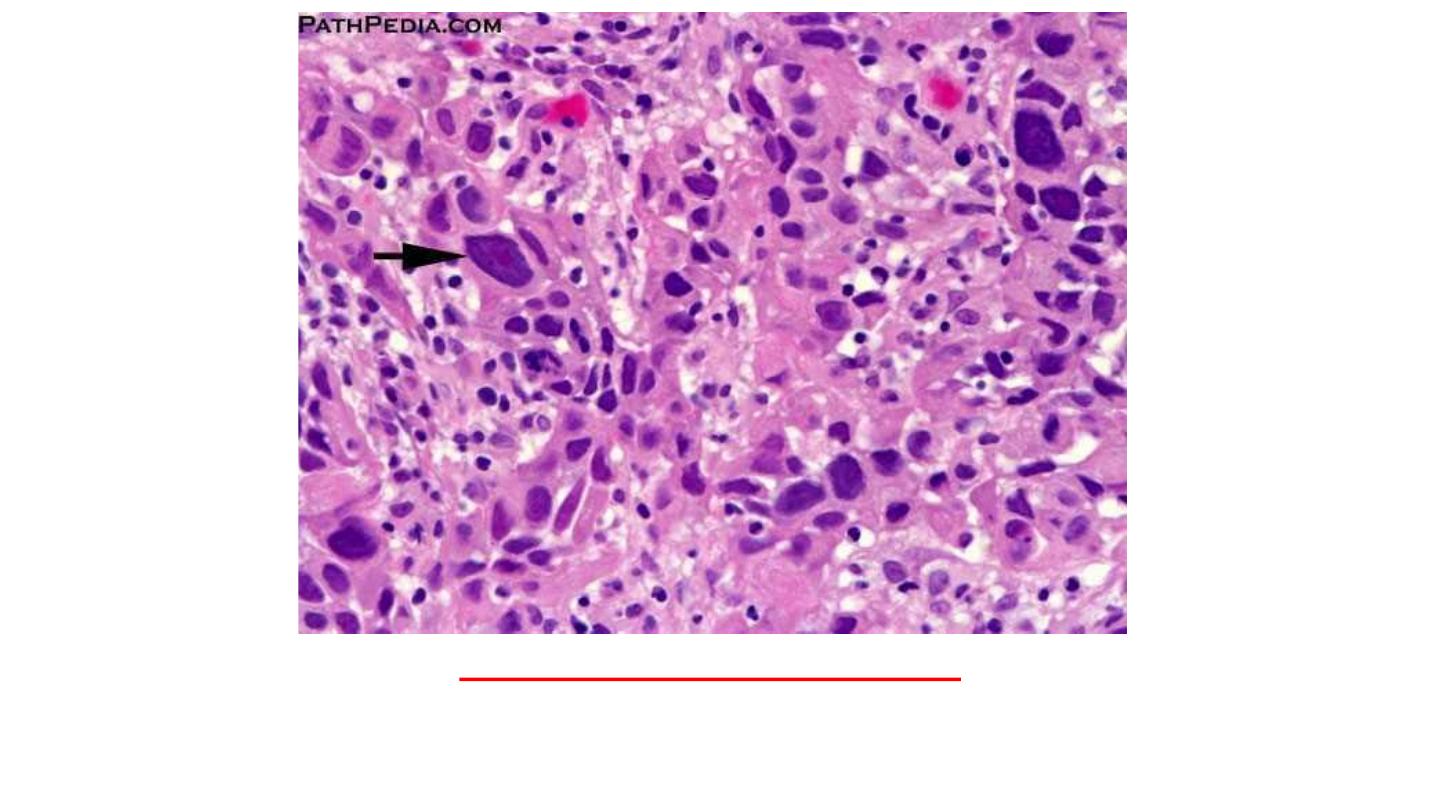
Clear cell carcinoma
1. The growth pattern varies from solid to trabecular (cordlike) or tubular
(resembling tubules).
2. The tumor cells have a rounded or polygonal shape and abundant clear or
granular cytoplasm, which contains glycogen and lipids.
3. The tumors have delicate branching vasculature and may show cystic as well
as solid areas.
4. Most tumors are well differentiated, but some show marked nuclear atypia
with formation of bizarre nuclei and giant cells.
Clear cell carcinoma
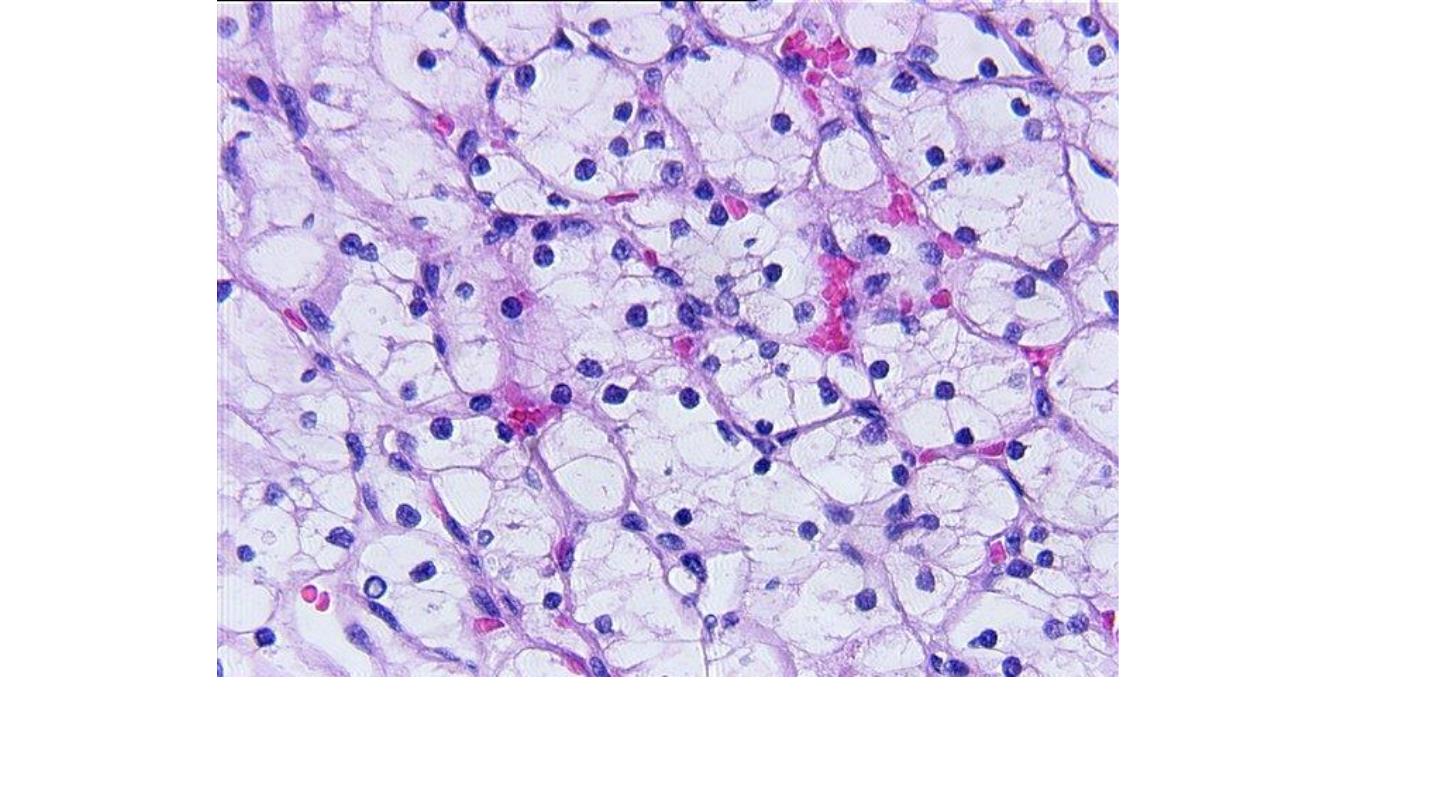
Clear cell carcinoma
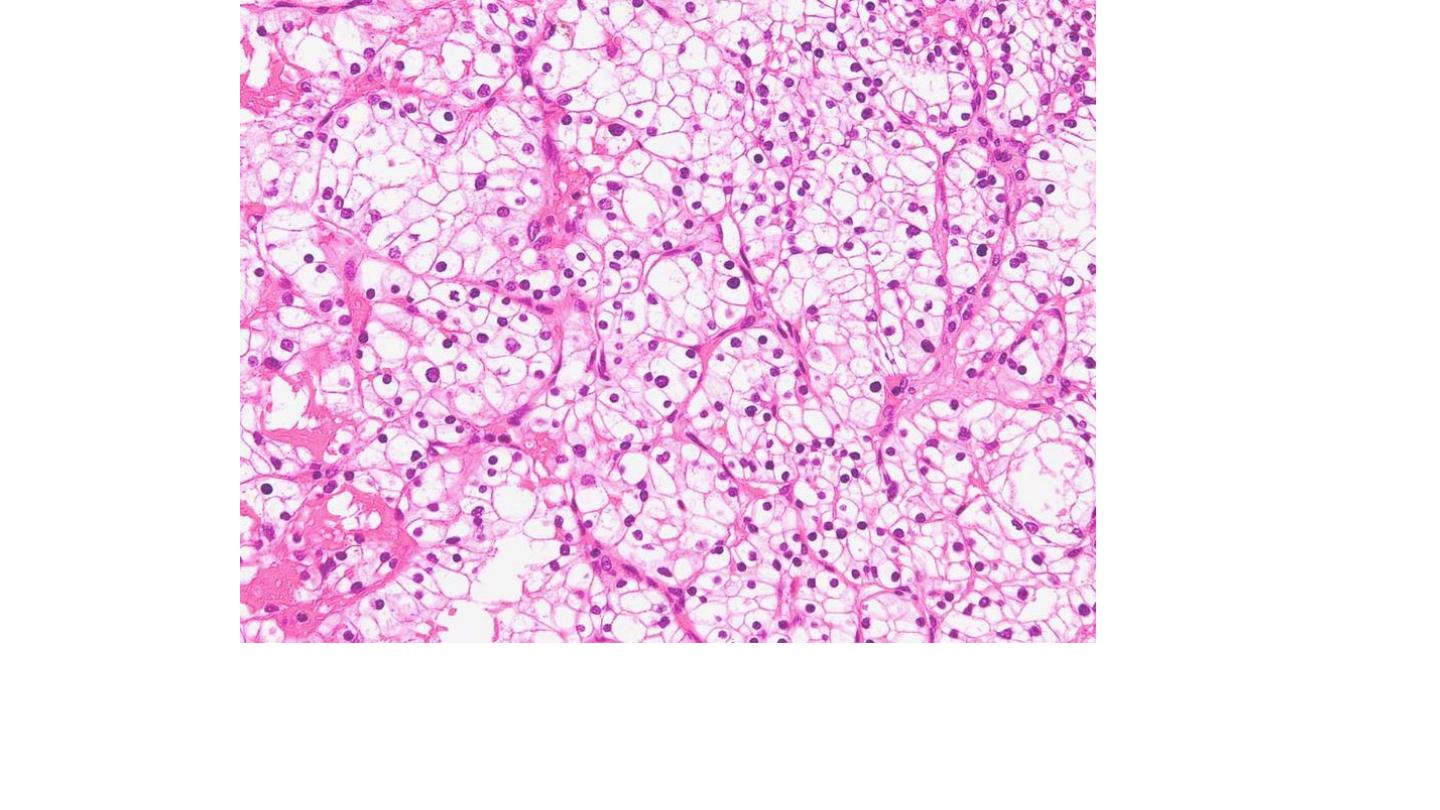
Clear cell carcinoma
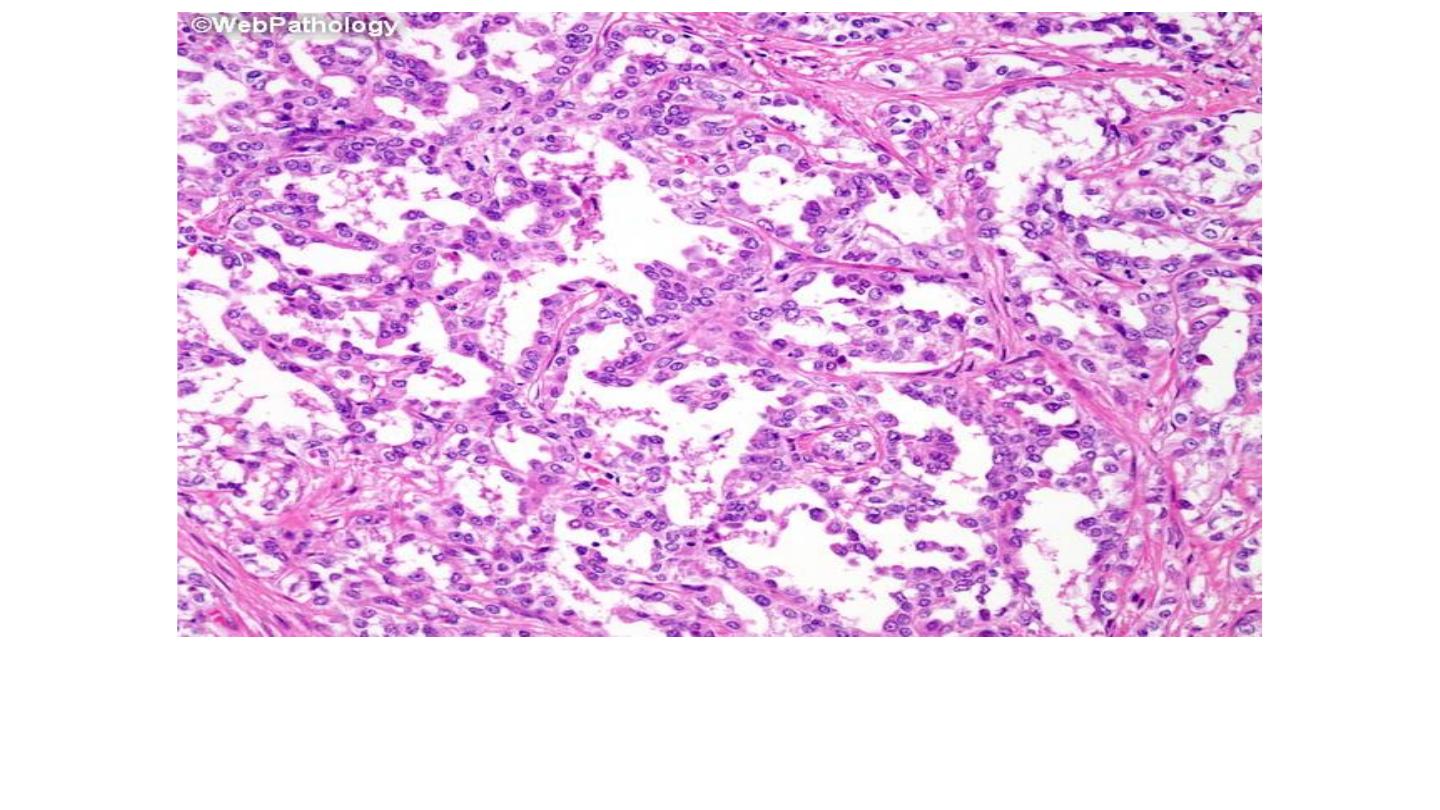
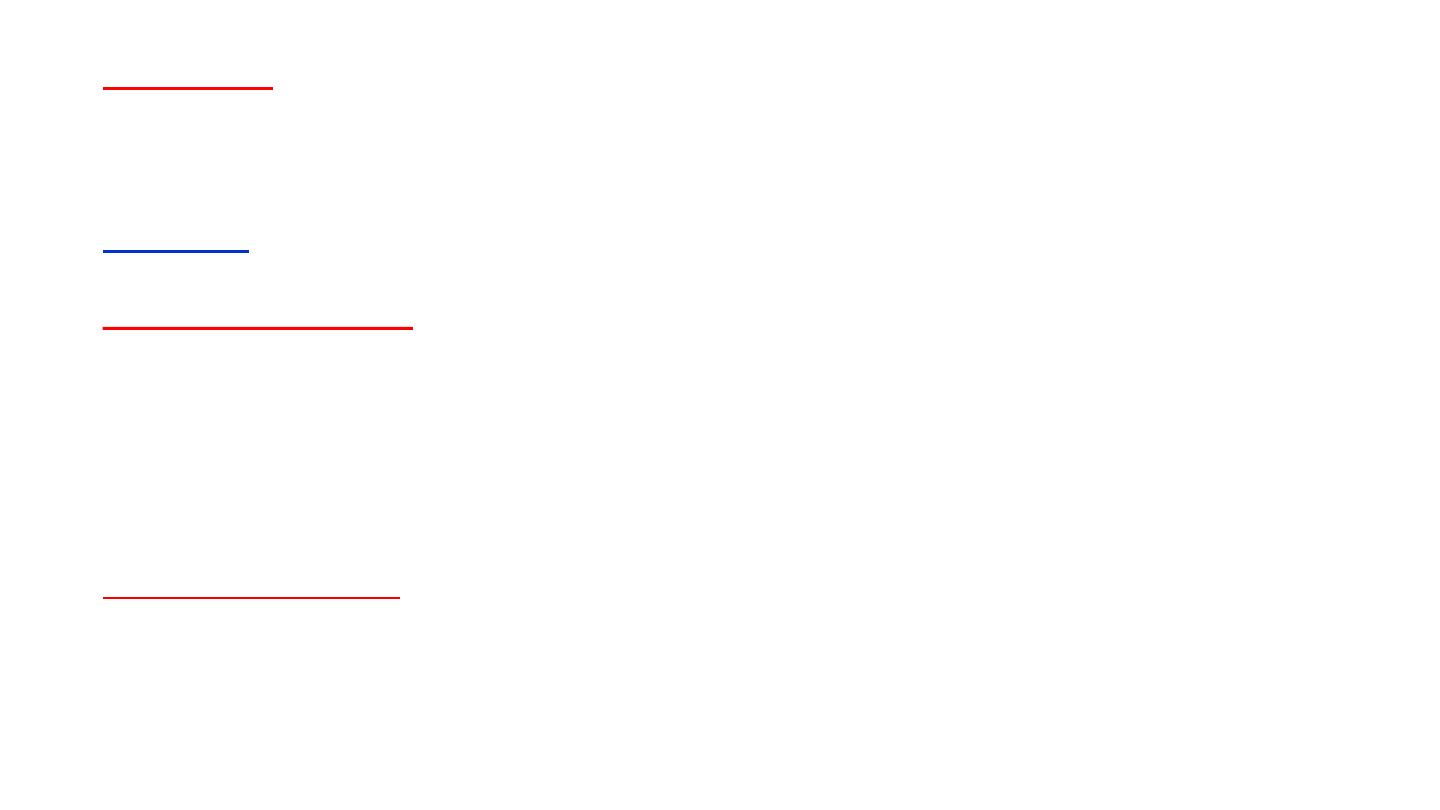
Papillary carcinoma
1. Composed of cuboidal or low columnar cells arranged in papillary
formations.
2. Interstitial foam cells are common in the papillary cores.
3. Psammoma bodies may be present.
4. The stroma is usually scanty but highly vascularized.
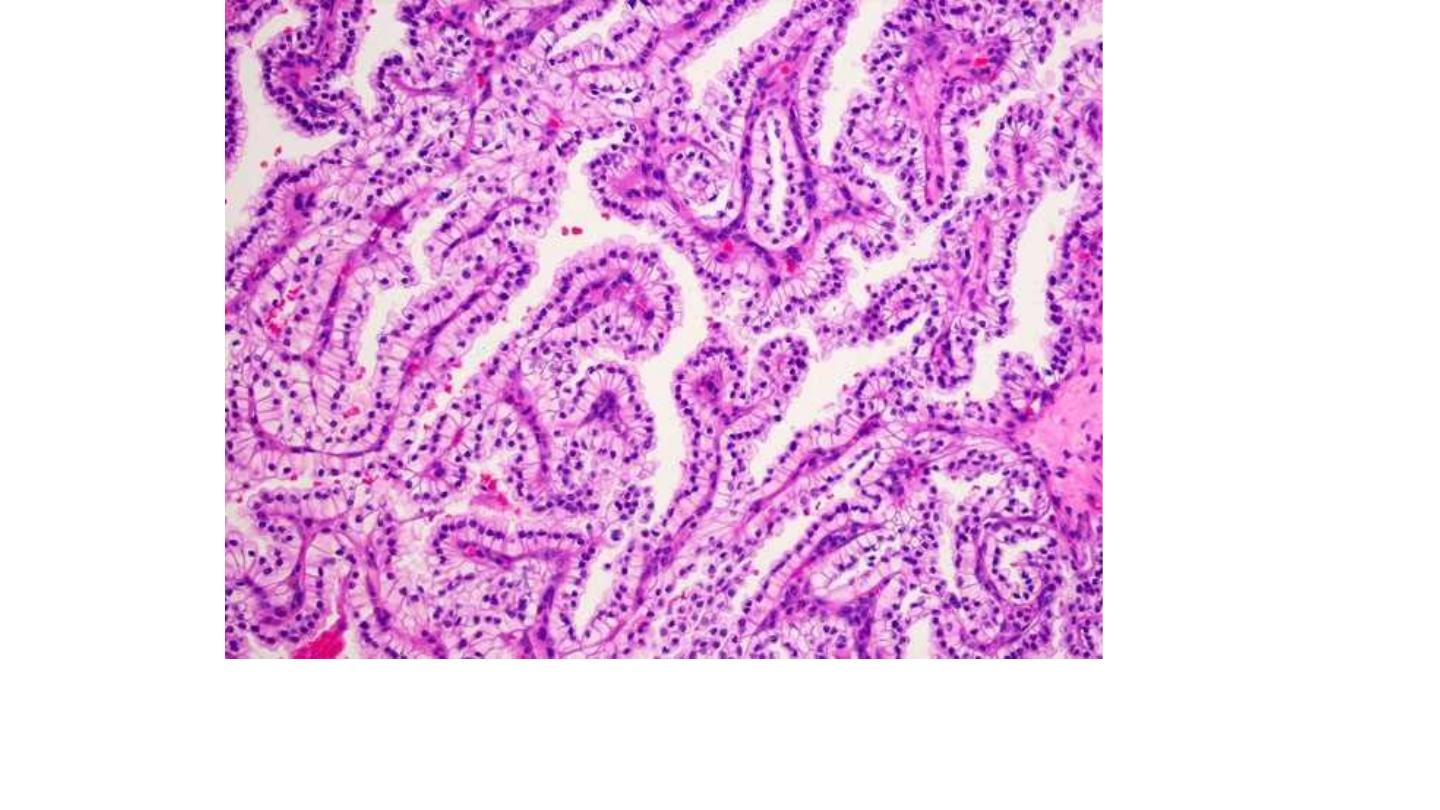
Papillary carcinoma
Papillary carcinoma
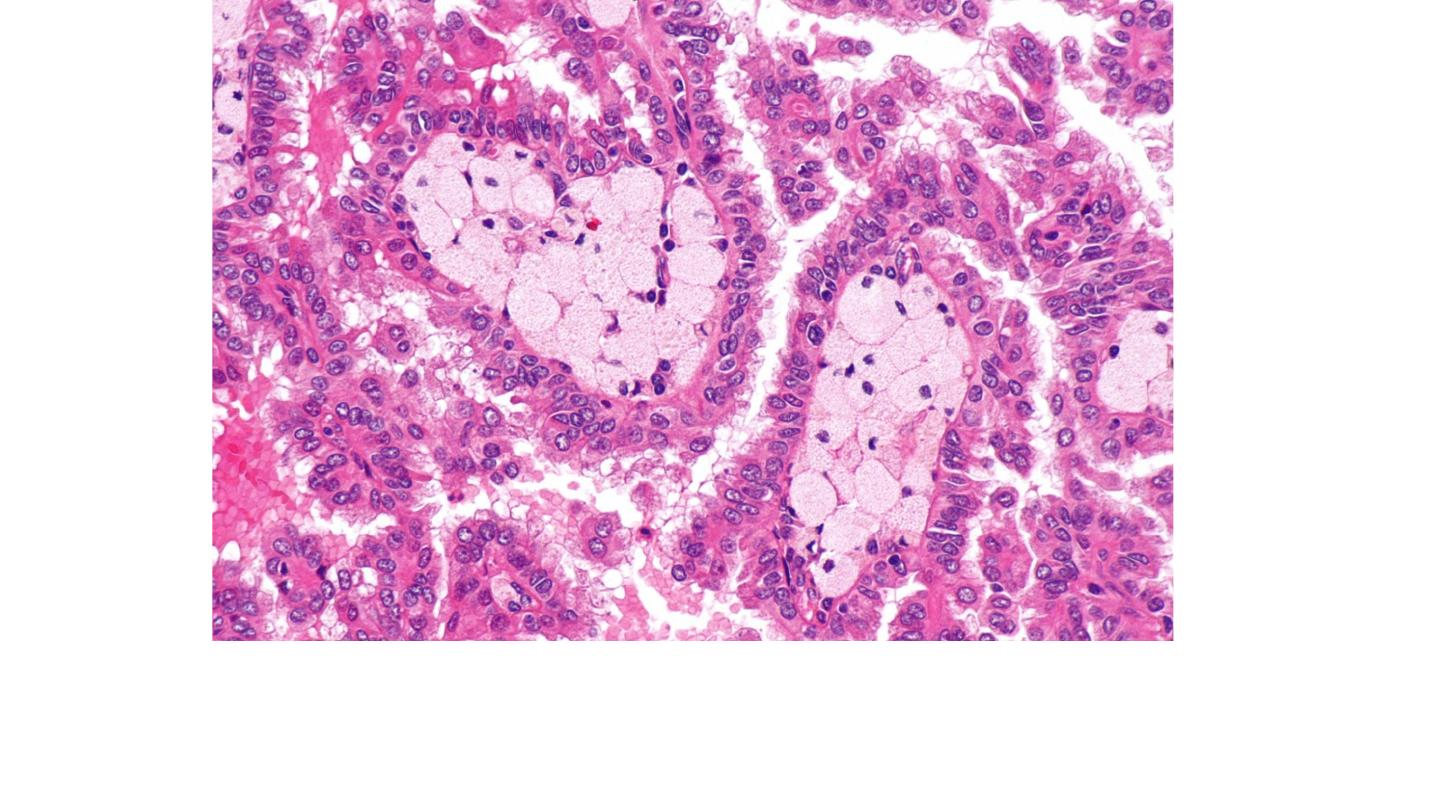
Papillary carcinoma
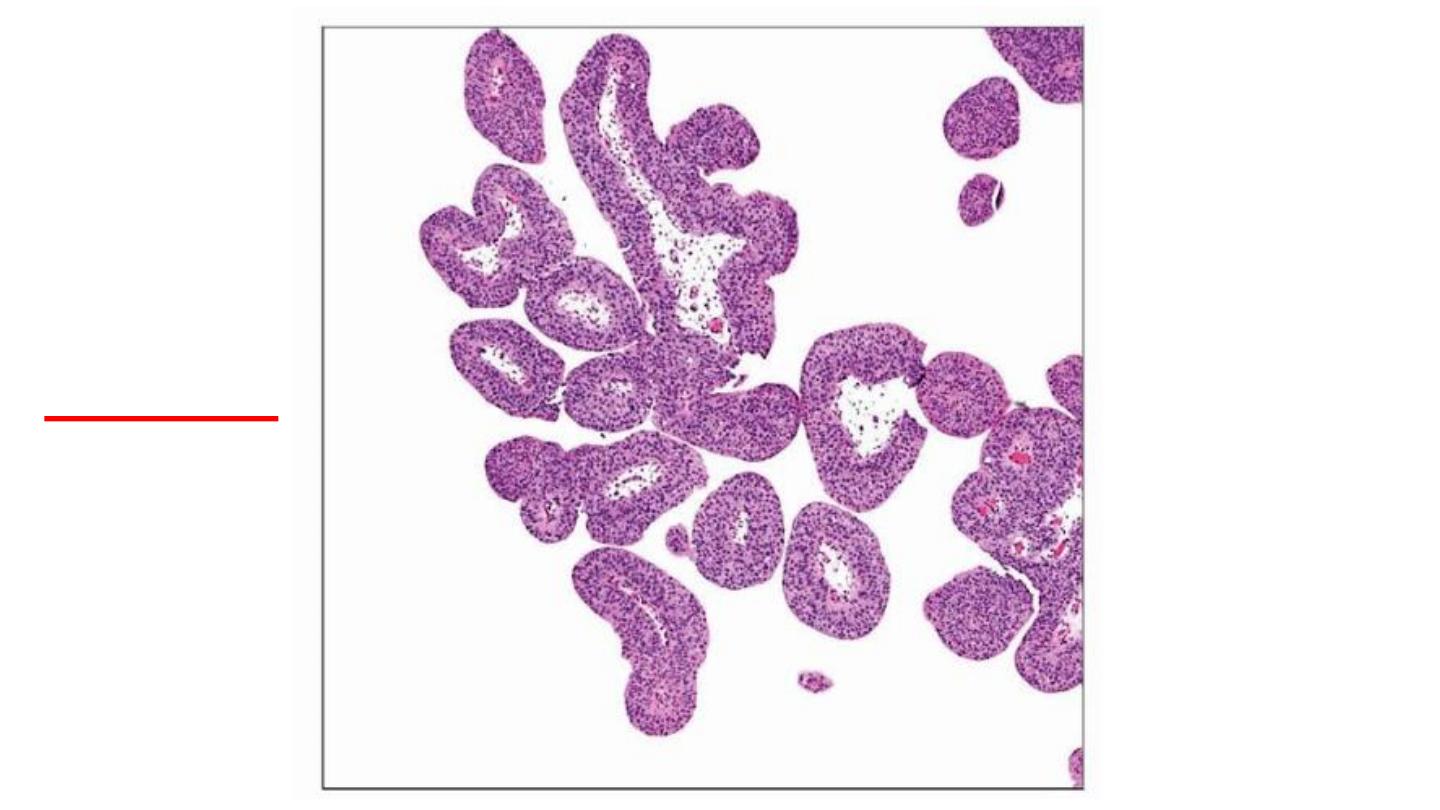
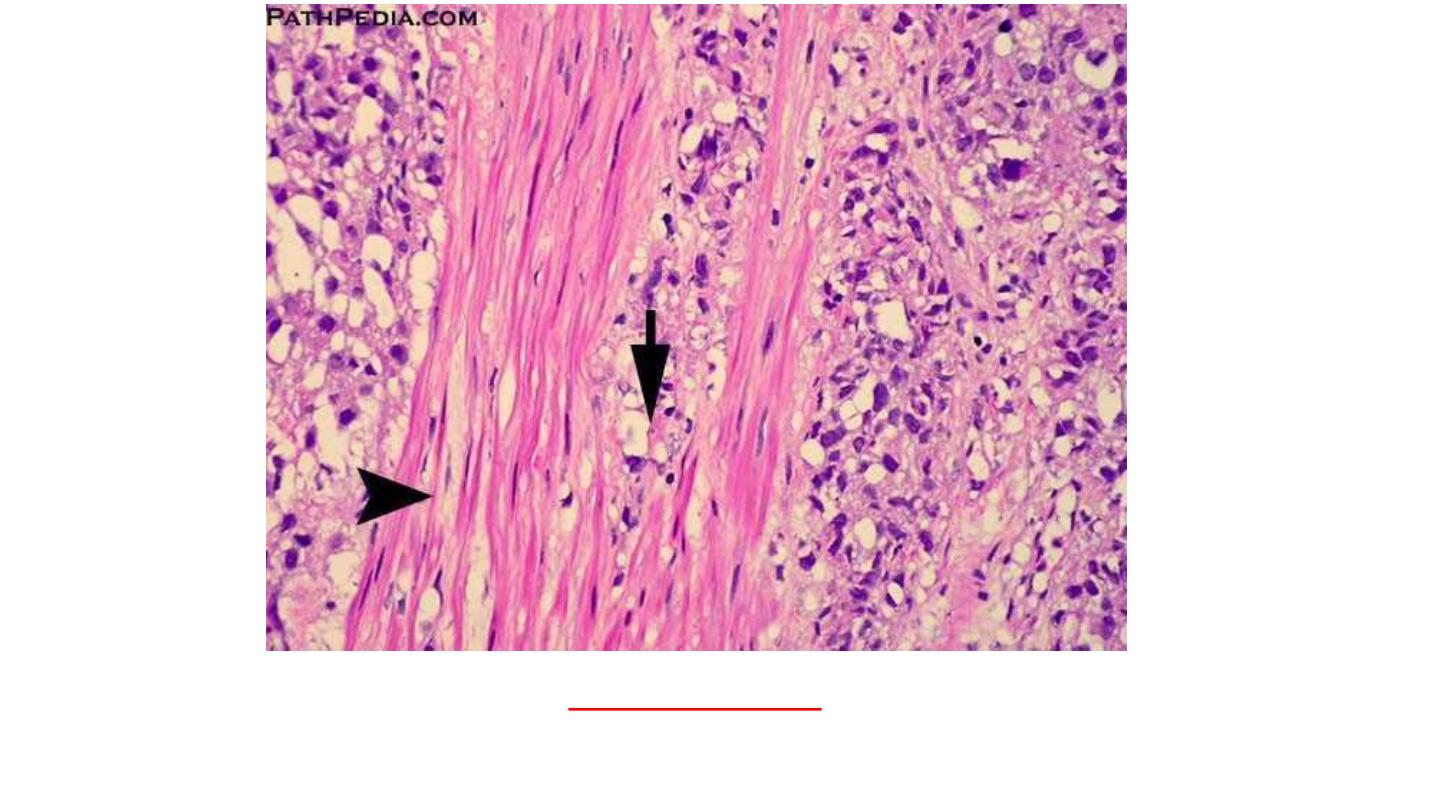
Chromophobe renal carcinoma
1. Pale eosinophilic cells.
2. A perinuclear halo.
Collecting duct carcinoma
Irregular channels lined by highly atypical epithelium with a
hobnail pattern
.
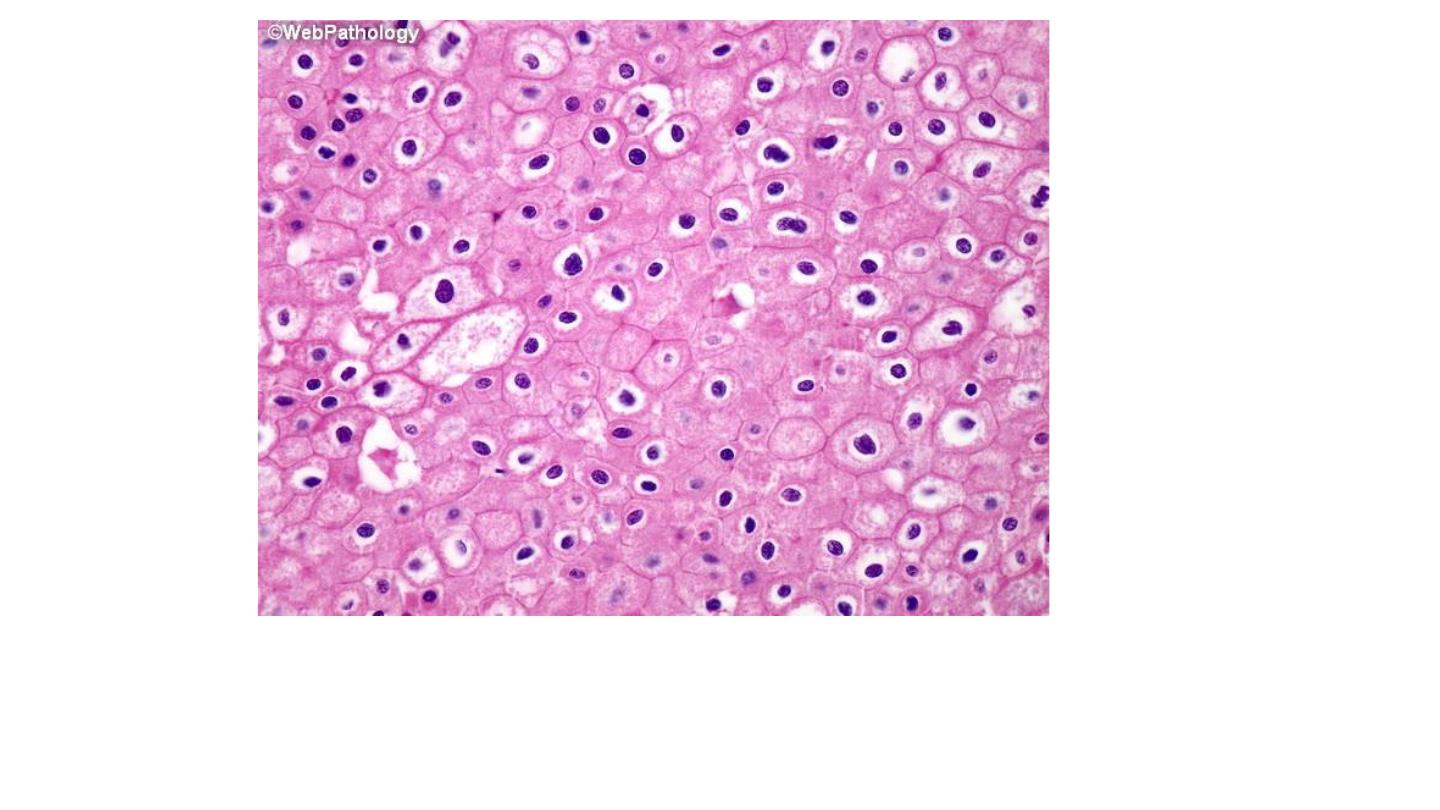
Chromophobe renal carcinoma
Chromophobe renal carcinoma
Collecting duct renal carcinoma
Urinary bladder neoplasms

Bladder cancer accounts for approximately 7% of cancers and 3% of
cancer mortality in the United States.
About 95% of bladder tumors are of epithelial origin, the remainder
being mesenchymal tumors.
Most epithelial tumors are composed of urothelial (transitional cell) type
and are thus called urothelial or transitional tumors, but squamous and
glandular carcinomas also occur.
Urothelial Tumors
Urothelial tumors represent about 90% of all bladder tumors and range
from small benign lesions that may never recur to aggressive cancers
associated with a high risk of death.

Classification of Tumors of the Urinary Bladder
1- Urothelial (transitional) tumors
Papilloma
Exophytic papilloma
Inverted papilloma
Papillary urothelial neoplasms of low malignant potential
Low grade and high grade papillary urothelial cancers
Carcinoma in situ (CIS, or flat non-invasive urothelial carcinoma)
2- Adenocarcinoma
3- Mixed carcinoma
4- Small-cell carcinoma
5- Sarcomas
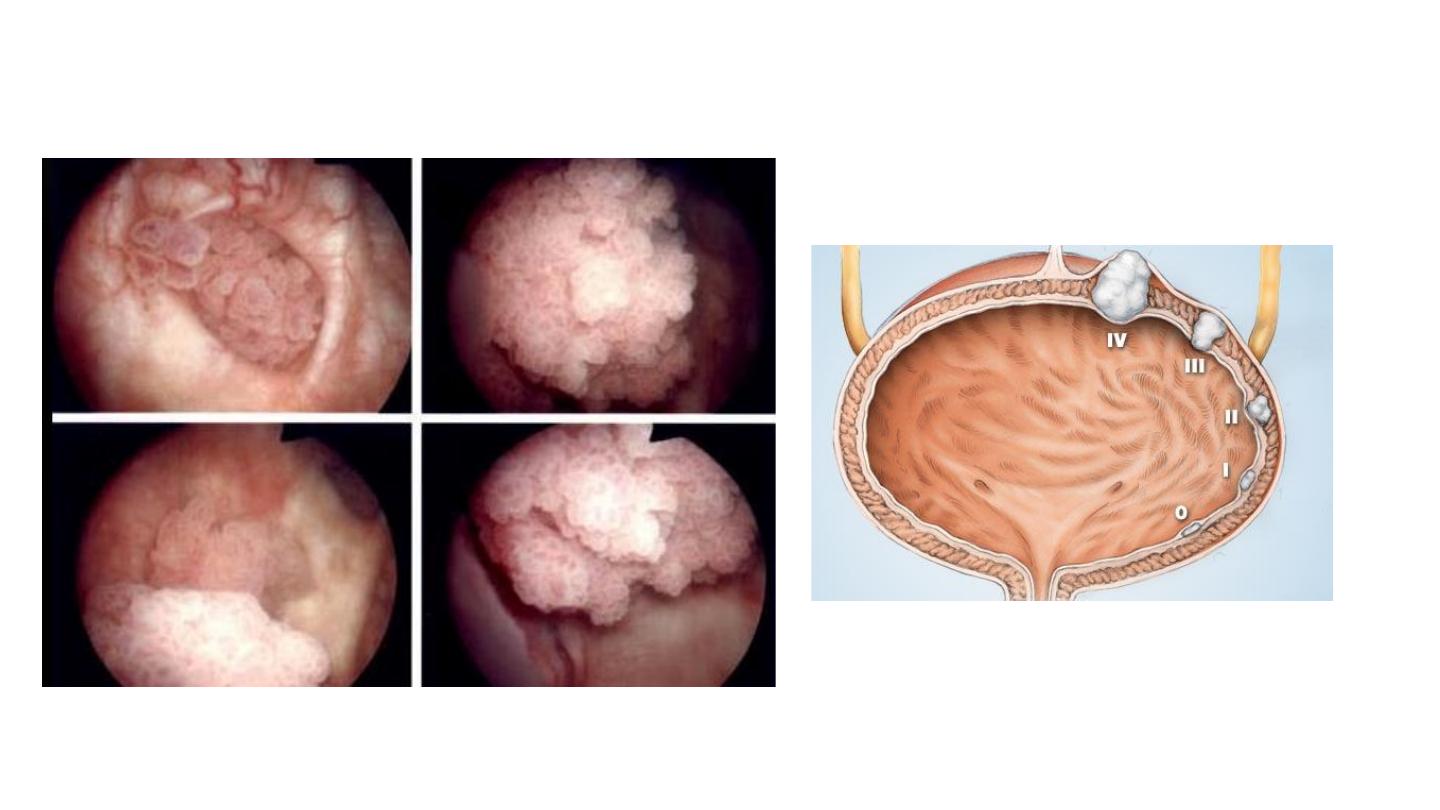
Clinical course of bladder cancer.
Bladder tumors classically produce
painless hematuria
. This is their dominant
and sometimes only clinical manifestation.
Frequency, urgency, and dysuria occasionally accompany the hematuria.
When the ureteral orifice is involved, pyelonephritis or hydronephrosis may
follow.
About 60% of neoplasms, when first discovered, are single, and 70% are
localized to the bladder.

Grading of Urothelial Papillary (Transitional Cell) Tumors
Urothelial papilloma
Urothelial neoplasm of low malignant potential
Papillary urothelial carcinoma, low grade
Papillary urothelial carcinoma, high grade
Carcinoma in situ

Pathogenesis.
Several factors have been implicated in the causation of urothelial carcinoma. Some of the more
important contributors include the following:
•
Cigarette smoking
•
Industrial exposure , the cancers appear 15 to 40 years after the first exposure.
•
Schistosoma haematobium infections in endemic areas .
•
Long-term use of analgesics is implicated.
•
Heavy long-term exposure to cyclophosphamide, an immunosuppressive agent.
•
exposure of the bladder to irradiation, administered for other pelvic malignancies.
Morphology.
Gross
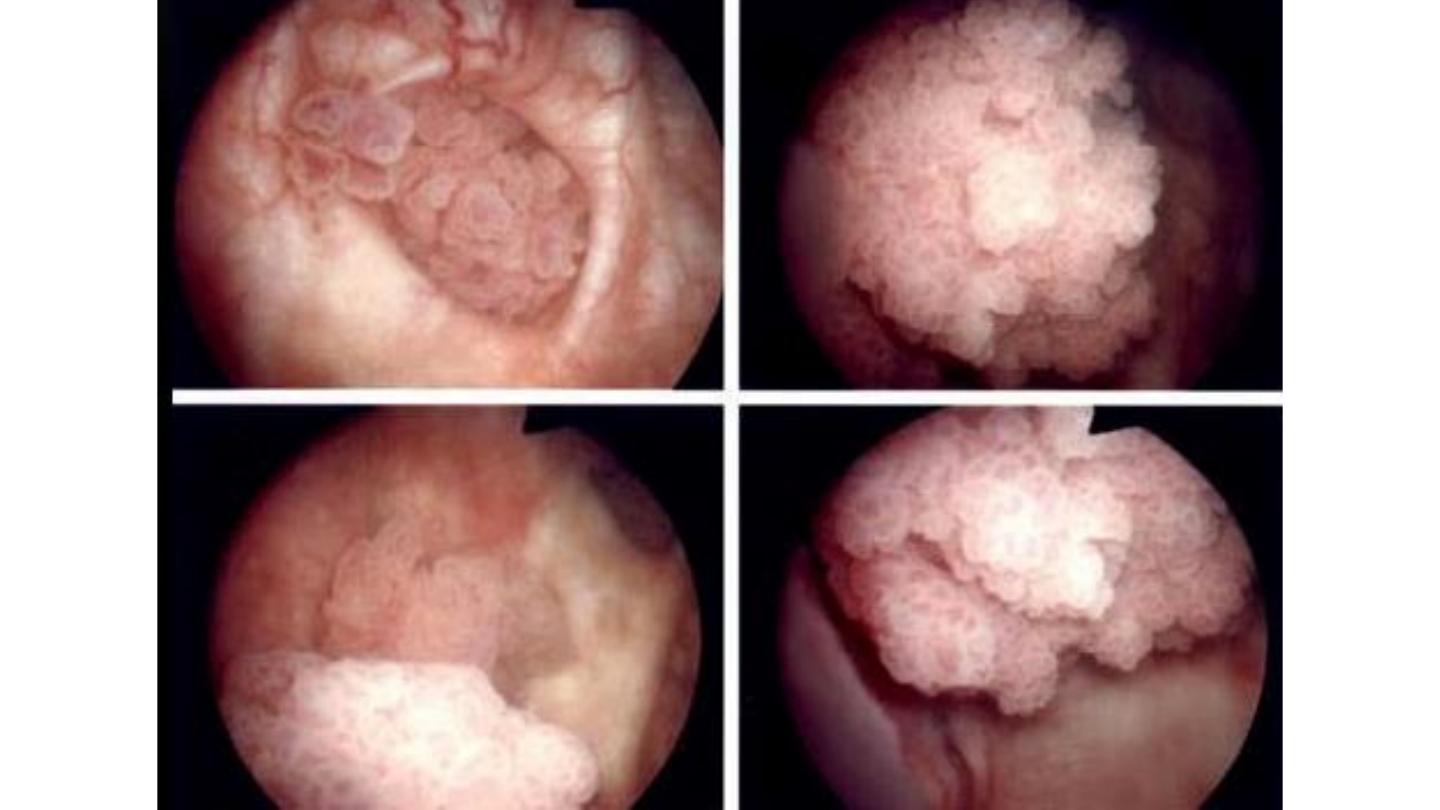
Range from purely papillary to nodular or flat lesion.
Papillary lesions appear as red, elevated projection varying in size
from less than 1 cm in diameter to large masses up to 5 cm in
diameter .

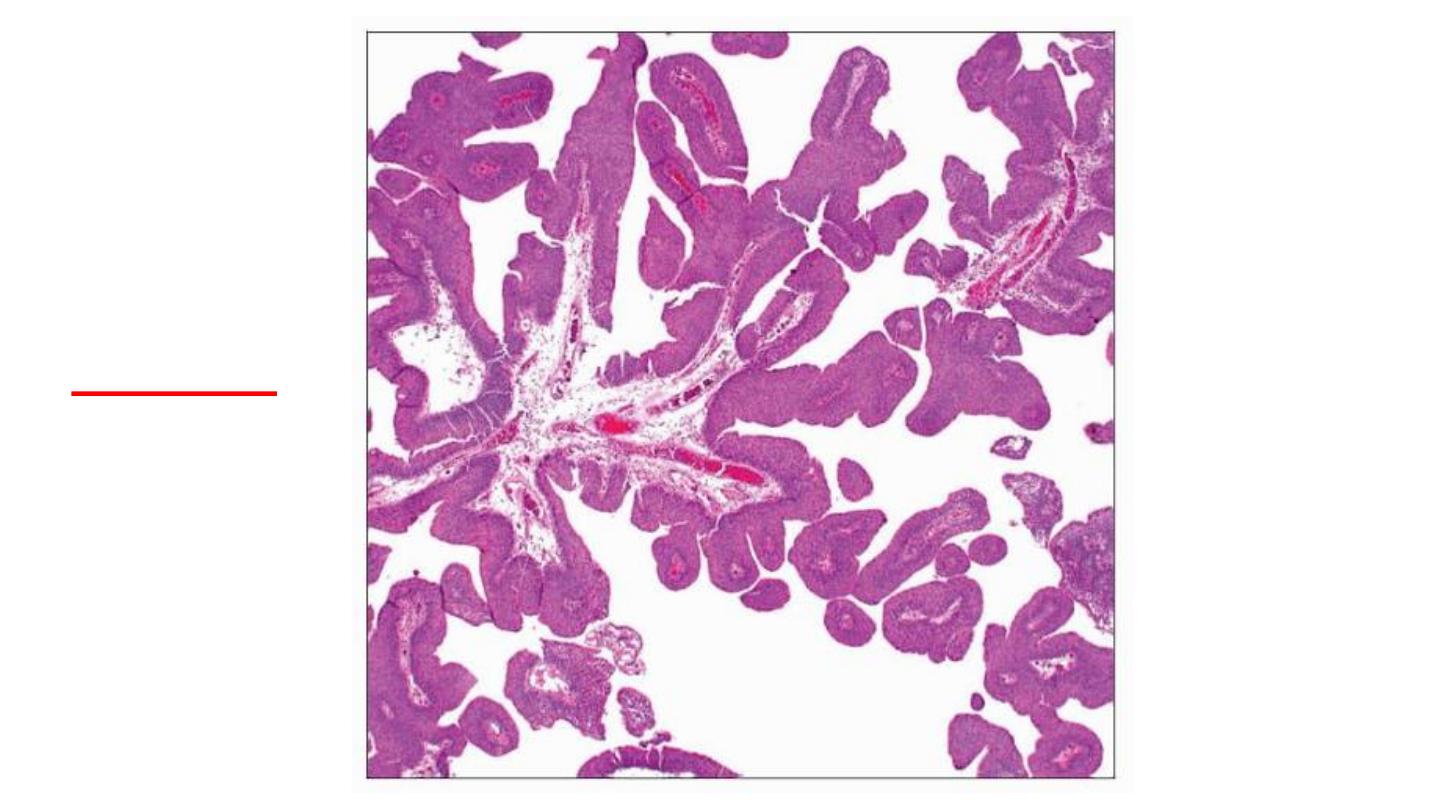
Papillary urothelial carcinoma

Microscopical
Range from benign papilloma to highly aggressive anaplastic cancers.
Papillomas
represent 1% or less of bladder tumors, and are usually seen in younger patients.
Two types :
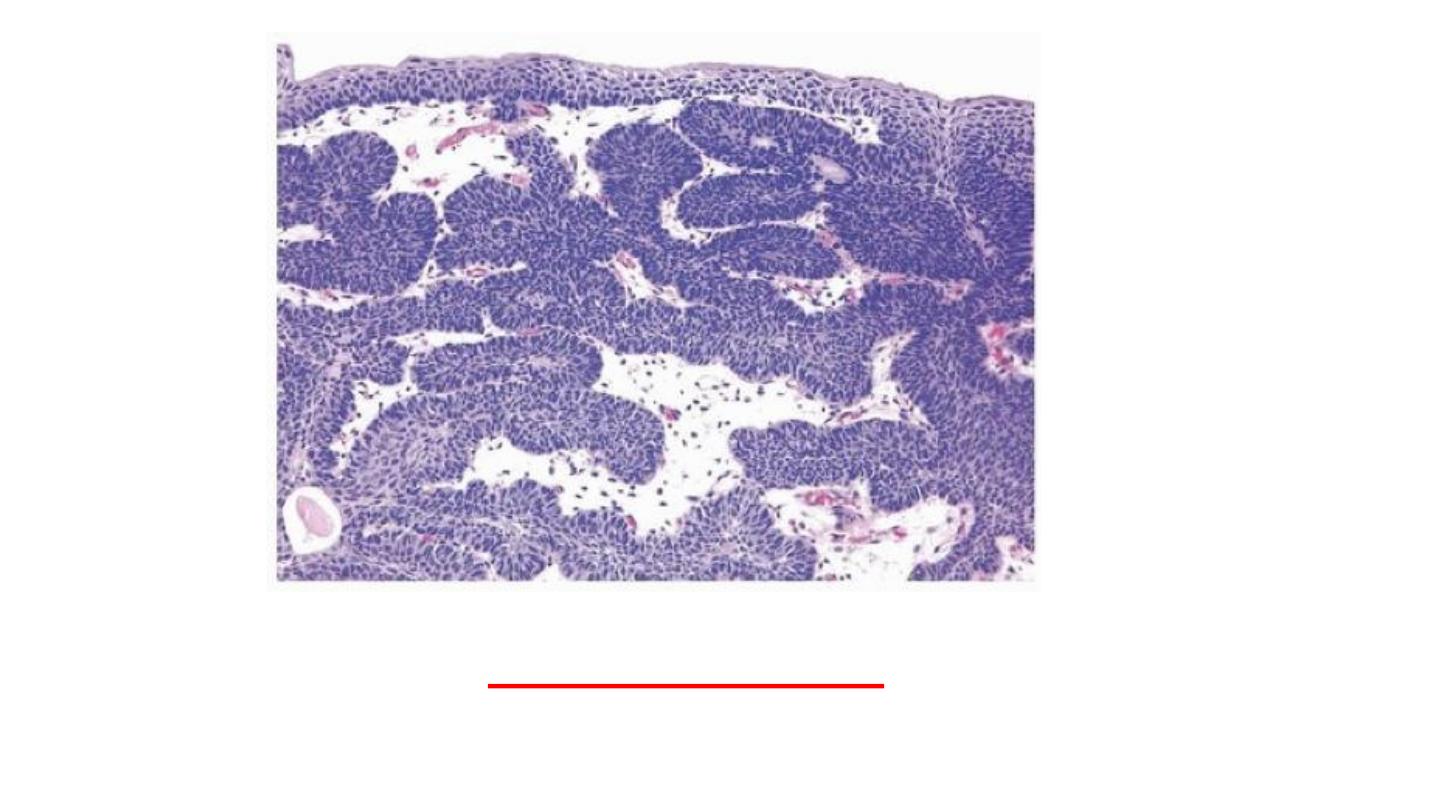
1- Exophytic papillomas
.
The tumors typically arise as single small, delicate, structure, superficially attached to the
mucosa by a stalk.
The individual finger-like papillae have a central core of loose fibrovascular tissue covered by
epithelium that is histologically identical to normal urothelium.
Recurrences and progression rarely occur, yet patients still need long-term follow-up.
2- Inverted papillomas.
Are benign lesions, consist of cords of cytologically bland urothelium that extend down into
the lamina propria and cured by excision.
Papilloma
Inverted Papilloma
Papillary urothelial neoplasms of low malignant potential (PUNLMPs).
They differ from papilloma, by being have
thicker urothelium
or
diffuse nuclear
enlargement
than papilloma.
At cystoscopy, PUNLMPs tend to be larger than papillomas and may be
indistinguishable from low- and high-grade papillary cancers.
PUNLMPs may recur with the same morphology, are not associated with invasion,
and only rarely recur as higher grade tumors associated with invasion and
progression.
PUNLMP
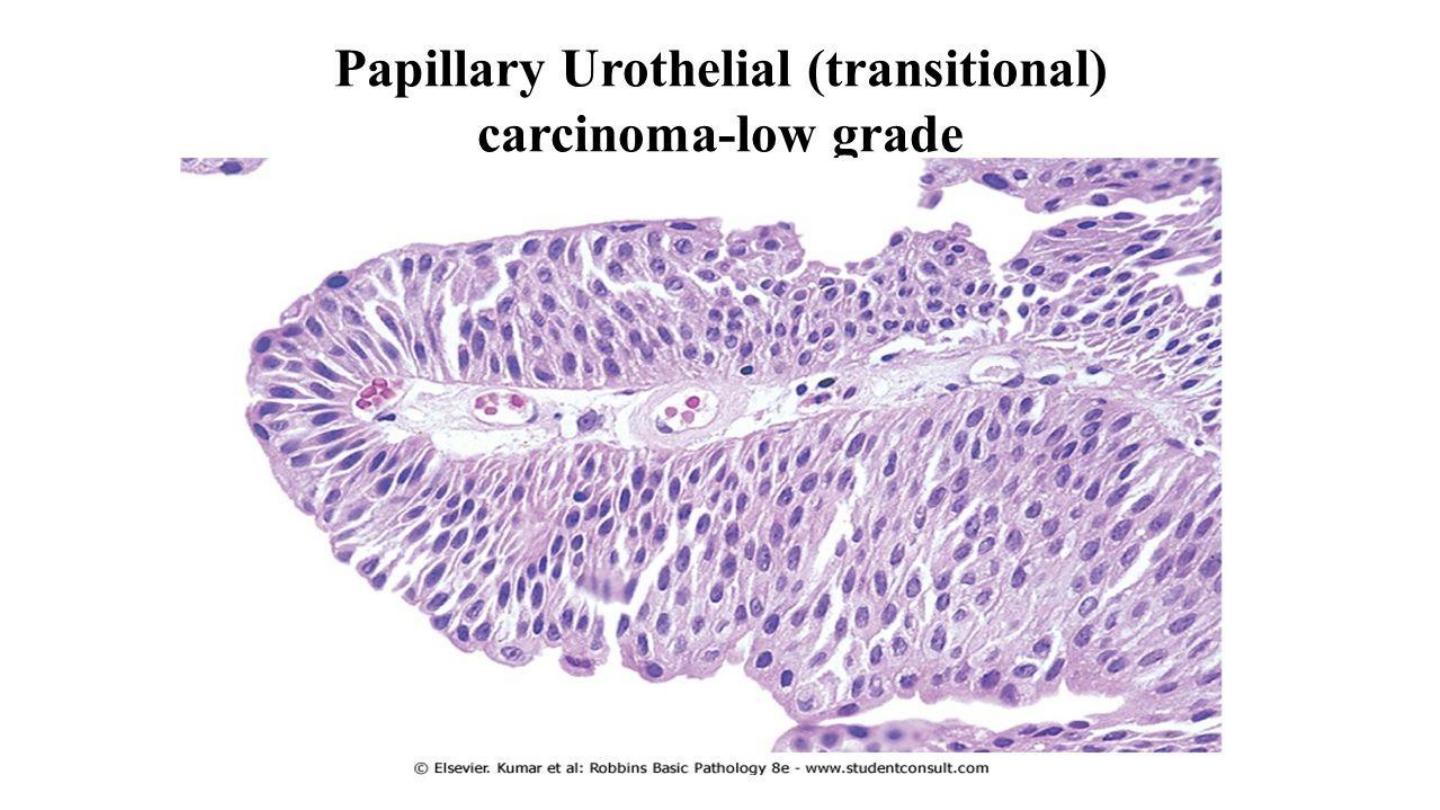
Low-grade papillary urothelial carcinomas
are characterized by an orderly appearance both
architecturally and cytologically
.
The cells are
evenly spaced
(i.e., maintain polarity) and
cohesive
.
Nuclear atypia
consisting of scattered hyperchromatic nuclei, infrequent mitotic
figures, and
mild variation in nuclear size and shape
.
Low-grade cancers can recur and, though infrequent, can invade. Only rarely do
these tumors pose a threat to the patient's life.
High-grade papillary urothelial cancers
Contain cells that may be
dyscohesive
with
large hyperchromatic nuclei
. Some of
the tumor cells show
frank anaplasia
.
Mitotic figures, are frequent. Architecturally, there is
disarray and loss of polarity
.
These tumors have a much higher incidence of invasion into the muscular layer, and
a significant metastatic potential.
High grade urothelial carcinoma
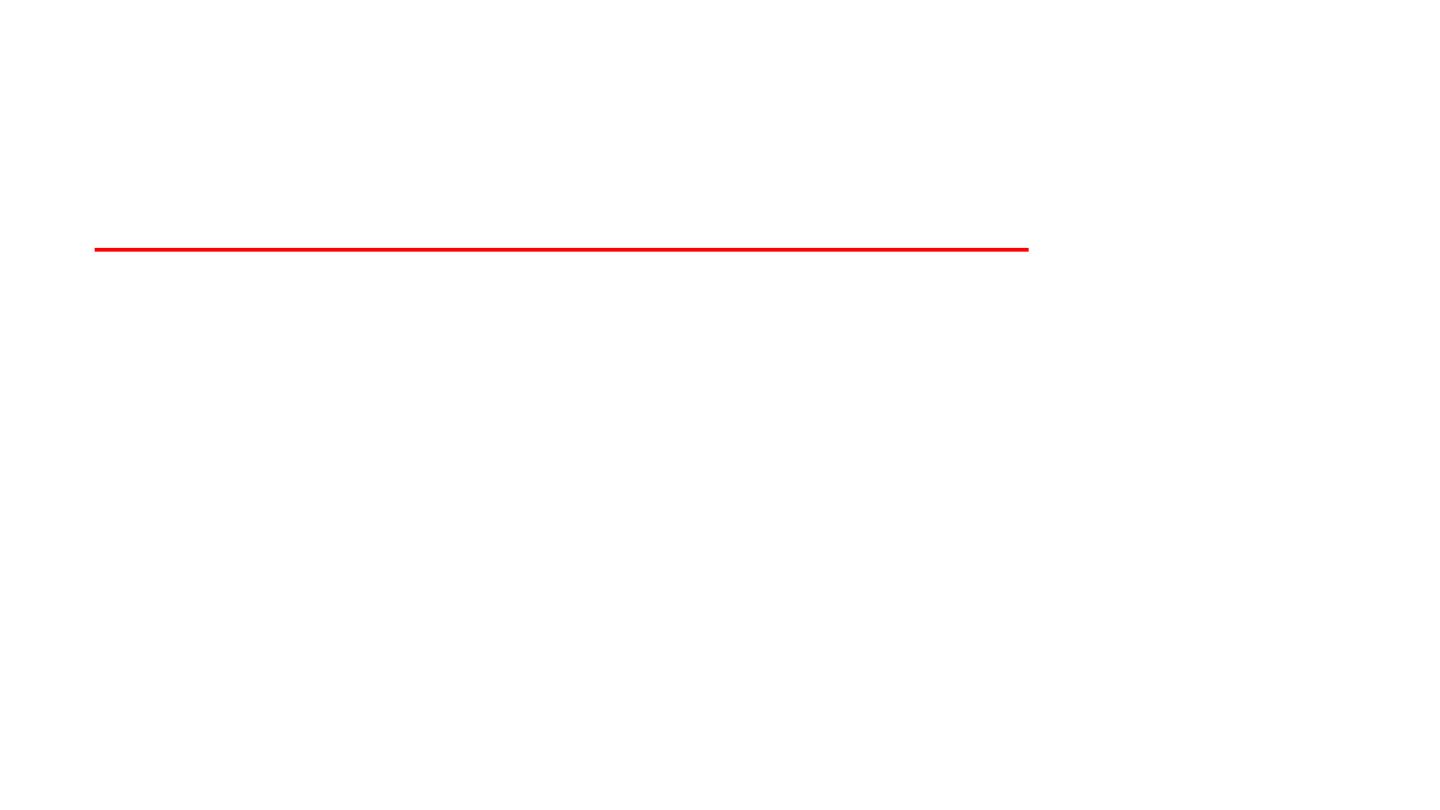
Carcinoma in situ (CIS or flat urothelial carcinoma)
is defined by the presence of cytologically malignant cells within a flat
urothelium. If untreated, 50% to 75% of CIS cases progress to muscle-
invasive cancer.
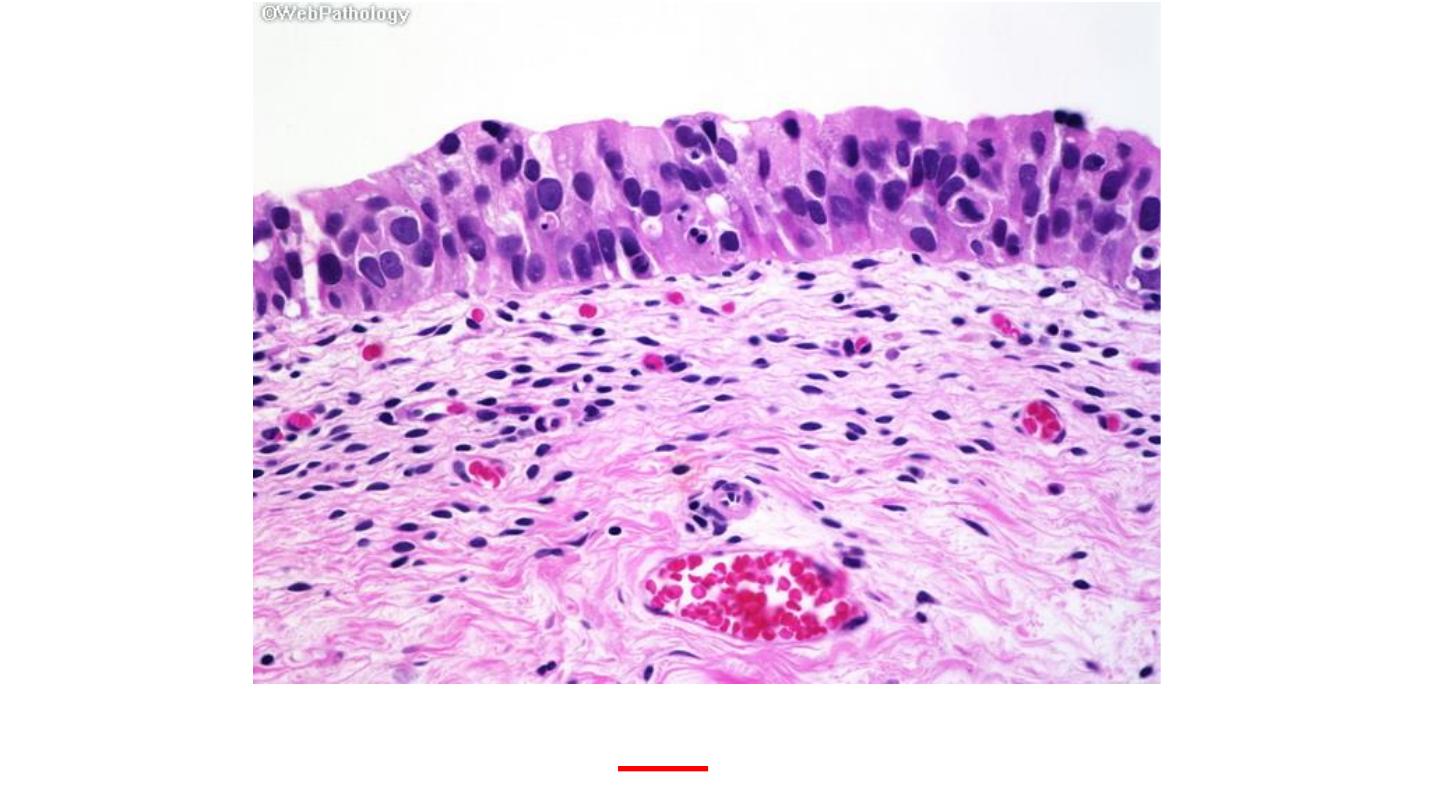
CIS
CIS

Although invasion into the lamina propria worsens the prognosis,
the major decrease in survival is associated with
invasion of the
muscularis propria
(detrusor muscle).
Once muscularis propria invasion occurs, there is a 30% 5-year
mortality rate.
MUSCLE INVASION

In most analyses, less than
10% of low-grade cancers
invade, but
as many as 80% of high-grade
urothelial carcinomas
are invasive.
About
40%
of these deeply invasive tumors metastasize to regional lymph nodes. Hematogenous
dissemination, principally to the liver, lungs, and bone marrow, may result.
The extent of spread (staging) at the time of initial diagnosis
is the most important factor in
determining the outlook for a patient.

Thank You
Thank You
