Fifth stage
ENTLec-2
د.سعد
4/10/2015
Inflammatory conditions of the nasal cavity (Rhinitis)Rhinitis is inflammation of the nasal cavity which may be caused by a variety of factors;
(1) VIRAL RHINITIS or CORYZA ( common cold );Is probably the commonest viral infection in man. The virus is transmitted by means of airborne droplet , the most common virus involved is rhinovirus and corona virus , but the infection occur only when the individual's resistance is lowered or when the concentration and virulence of the viral infection is high. It is most common in winter and affect all age group especially children and young adult.
CLINICAL FEATURE;
The course of the disease may be described in 4 stages ;
Prodromal or ischaemic stage; This last for few hours, and represents the stage of local invasion and general nasal ischaemia. The patient feels hot, dry or tickling spot at the site of invasion with patent nasal airway.
Early reaction or irritation ; The infection which at first localized , spread to the adjacent mucus membrane. This process may take few hours or days. The patient feels sorethroat , sneezing, watery discharge and obstruction. The mucus membrane is red and swollen. General symptoms of mild toxaemia and fever now appear.
3) Stage of venous stasis and secondary infection; After the 2nd day , the colour of the mucosa become dusky , with a bluish tinge, the discharge thickens, diminishes and become mucopurulent. The obstruction and toxaemia are at their maximum.
4) Resolution; The symptoms and signs gradually diminish, and after 5-10 days recovery takes place.
TREATMENT;
Isolation of the patient.
Bed rest.
3. Decongestant drops ( ephedrine and xylometazolin ) to promote drainage and to prevent occlusion of the sinus, as well as for the relief of discomfort.
4. Steam inhalation with menthol or tincture of benzoin, given few minutes after the decongestant drops, this may be soothing and apply heat directly to the mucus membrane.
Analgesic.
Antihistamine.
Antibiotics should only be used if complications develop such as, acute otitis media, sinusitis, tonsillitis, bronchitis or pneumonia.
(2) ALLERGIC RHINITIS:
Definition ; Is an IgE-mediated hypersensitivity of the nasal mucus membrane characterized by sneezing, itching, watery nasal discharge and nasal obstruction.
Aetiology; Allergic rhinitis, asthma and eczema are the clinical expression of atopic diseases which are due to genetically inherited tendency to develop an exaggerated IgE response to extrinsic allergens. Therefore, the patient may present early in life with infantile eczema and progress to allergic rhinitis and asthma.
Allergens are either present in the air (inhalants), or less often, in the food (ingested). Inhalants, seasonal or perineal, are the most common group of allergens.
Seasonal allergic rhinitis, which occur in spring and autumn are caused by pollens and fungi spores.
Perineal allergic rhinitis, are due to inhaled allergens independent of the season e.g. house dust mite which is found in high concentration in bedrooms, as it feeds on skin scales (see the fig. below). Other examples are the epithelial debris from the domestic cat and dogs.
Foods like fish, strawberry, nuts, eggs, milk and flour are examples of ingested allergens. There are also occupational allergens e.g. to flour in bakers, to hair and epithelial scales in hairdressers, wood dust in carpenters, washing powders in soup powder manufacturers.
Pathophysiology;
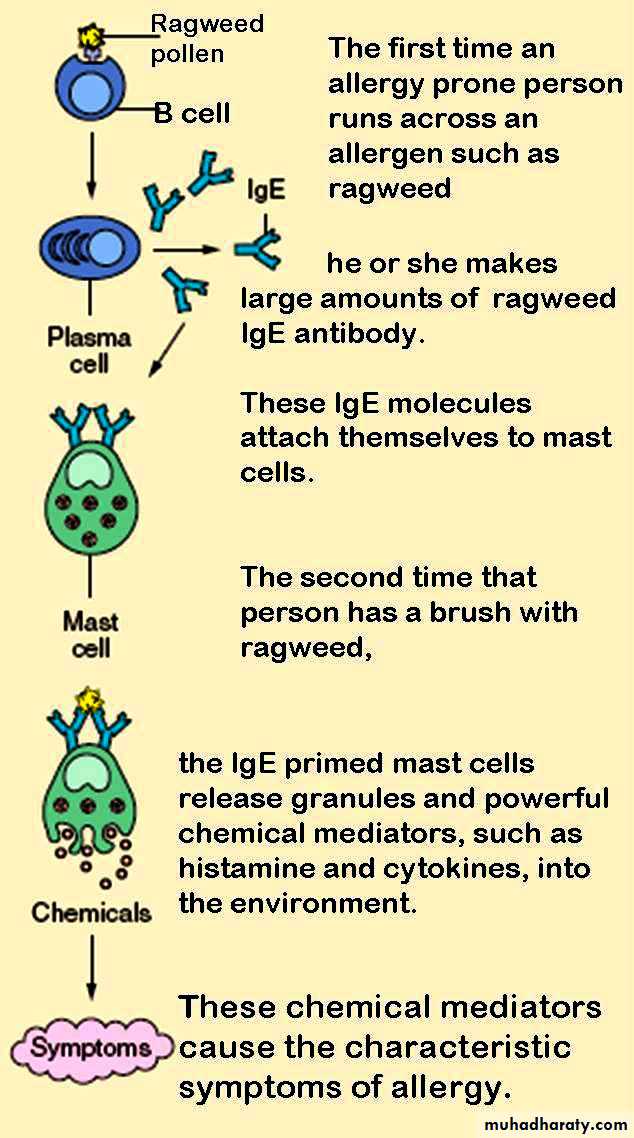
Initial presentation of an allergen to the immune system usually produce no symptom but prepare the host to respond to the future exposure.
In subsequent attack with the allergens, the antigen interact with the antibody on the mast cell surface leading to mast cell degranulation and secretion of histamine and other mediators of anaphylaxis .
DIAGNOSIS:
HISTORY: We have to ask the patient about the following;Symptoms; sneezing, nasal itching, profuse watery nasal discharge and obstruction .
When it occur? ( seasonal or perineal ) and what initiate its attack?( predisposing factors).
Previous history of infantile eczema, tendency to wheezy bronchitis and family history of allergy.
EXAMINATION:
Typical physical eye findings ( injected conjunctiva with watery discharge and eyelid puffiness).
Anterior rhinoscopy may be normal or we may find oedematous bluish-gray mucosa covered with watery mucus. The inferior turbinate may be swollen with polypoidal appearance.
INVESTIGATION:
Skin prick test ; are used to determine the presence of IgE antibody directed against specific allergen, by using solution containing various allergens.
Nasal cytology ; A characteristic of nasal secretion is the large number of eosinophils, especially just after an acute attack.
Increase serum IgE level.
TREATMENT:
Avoidance of specific allergens; e.g. use of air conditioning and filters .
Pharmacotherapy;
Antihistamine; are useful for relief of itching, sneezing and watery rhinorrhoea but are less effective for nasal congestion.
They are of 2 types ;
1st generation antihistamine; this has the side effect of sedation and anticholinergic effect , e.g. diphenhydramine and chlorpheniramine.
2nd generation antihistamine; which does not cross the blood-brain barrier and therefore non-sedating in most patient (e.g. Fexofenadine and Loratidine). They may produce cardiac arrhythmias and may have serious interaction with antifungals erythromycin.
Steroids ; (Anti- inflammatory)
Topical steroid therapy: (drops or sprays)used for prevention and control of allergic rhinitis e.g. beclomethasone spray . In seasonal rhinitis they are best used before onset of season.Local dryness and bleeding occasionally occur .
Systemic steroids : oral prednisolone, in short course (20 mg./ day for 5 days) or long acting intramuscular steroid which may give dramatic symptomatic relief but have more precaution for use .
Topical anticholinergic agent ; (nasal ipratropium bromide) is only effective against watery rhinorrhoea .
Mast-cell stabilizing agent: ( nasal disodium chromoglycate) is less effective than steroid sprays .They are the treatment of first choice in young children(safe and non toxic). They are used also for prophylaxis.
Immunotherapy;(specific hyposensitisation).
This depend on repeated administration of specific allergens, based on allergen test e.g. skin prick test , but should only be offered in centers where full resuscitation facilities are available [done by injecting under the skin a solution of salt water (saline) that contains a very small amount of the allergen(s)]. It should be carried out before the pollen season and continued for several years. The body "get used to" the allergen, which can result in fewer or less severe symptoms. The precise mechanism responsible is still unknown.The principles of good treatment is avoidances of allergens whenever possible + anti-inflammatory treatment ( primarily topical steroid ) + mediator blocking agents( anti histamine).
The principles of good treatment is avoidances of allergens whenever possible + anti-inflammatory treatment ( primarily topical steroid ) + mediator blocking agents( anti histamine).
(3) NON-ALLERGIC RHINITIS: (Intrinsic or vasomotor rhinitis)
Definition; is non –infective, non-allergic condition suspected to be due to autonomic imbalance within the nasal cavity.
Symptoms ; Identical to those of allergic rhinitis.
Pathogenesis ;There is neurovascular disorder of the blood vessels of the nasal mucosa, affecting the parasympathetic system particularly ( overactive parasympathetic system) . Allergens to specific antibody can not be demonstrated (i.e. IgE- mediated mechanism do not play a role). The symptoms are provoked by non-specific exogenous factors (e.g. cold air, humidity change ,fatigue, stress, cigarette smoking, air conditioning and central heating).
Diagnosis: Typical history (episodic watery rhinorrhoea and nasal obstruction due to inferior turbinate hypertrophy) + negative allergen test + no elevated IgE in the secretion.
Treatment:
Avoidance of irritant (e.g. cigarette smoke).Topical nasal steroids.
When there is copious watery discharge, the addition of nasal anticholenergic (nasal ipratropium bromide) is usually recommended.
Surgery ;
Correction of associated septal deviation and turbinate hypertrophy.
Vidian neurectomy : disruption of parasympathetic fibers to the nasal mucosa.
(4) ATROPHIC RHINITIS:
Is a chronic nasal disease characterized by progressive atrophy of the mucosa and underlying bone of turbinates and the presence of viscid secretion which rapidly dries and form crusts which emit a characteristic foul odour called ozaena (a stench). There is an abnormal patency of nasal passages. (The ciliated columnar epithelium either metaplases to cuboidal or stratified squamous epithelium ).Aetiology:
Is still unknown but it can be divided into;Primary (idiopathic) atrophic rhinitis : this may be due to infection with Klibsiella ozaenae or some other bacteria, endocrine imbalance( because it is more common in female at puberty ), heredity and poor nutrition. Recently it is considered as autonomic disease.
Secondary atrophic rhinitis: may be due to :
Extensive nasal surgery.
Occupational exposure to glass, wood, asbestos …etc.
Irradiation.
Clinical picture:
Symptoms: nasal obstruction ,epistaxis and anosmia.
Signs:
(1) The presence of nasal fetor, not appreciated by the patient who anosmic.
(2) Green yellow and black crust lining the nasal cavity and there detachment reveals a bleeding and ulcerated mucosa.
(3) Wide nasal cavity.
Differential diagnosis: Nasal fetor may occur in :
Tumors of the nose and sinuses.
Purulent rhinitis and sinusitis especially of dental origin.
Rhinolith and foreign body(unilateral nasal obstruction and foul- smelling secretion).
Treatment:
Medical ;
Nasal irrigation with alkaline solution.
Regular nasal cleansing and removal of crusts, followed by ..;
Nasal drops composed of 25% glucose in glycerin which inhibit proteolytic organs.
Rifampicin 600MG orally once daily for 6 months.
Surgical:
Closure of one or both nostrils by plastic surgery.
(5) RHINITIS MEDICAMENTOSA:
This condition is the result of over-medication with local nasal decongestant (e.g. oxymetazoline, phenylephrine, and xylometazoline nasal sprays). The libral use of sprays initially brings releif to the patient with enlarged inferior turbinates. Unfortunately, when the effect wears off a rebound phenomenon occurs with reflex vasodilatation from ischaemia causing turbinate hypertrophy.If the decongestant treatment is repeated , a chronic nasal obstruction unresponsive to decongestant results.Treatment: Is immediate cessation of the decongestant with replacement by nasal or systemic steroids. If this is not successful then inferior turbinectomy may be required.