
د مهند الشاله
Lecture 1
The Anus and Anal canal
Describe applied anatomy and histology of the anal canal
Describe the clinical features, investigations and principles of
management of common anorectal diseases
Learning objectives
Surgical anatomy
The anal canal commences at the
level where the rectum passes
downwards and backwards for
around 4 cm through the pelvic
diaphragm and ends at the anal
verge.
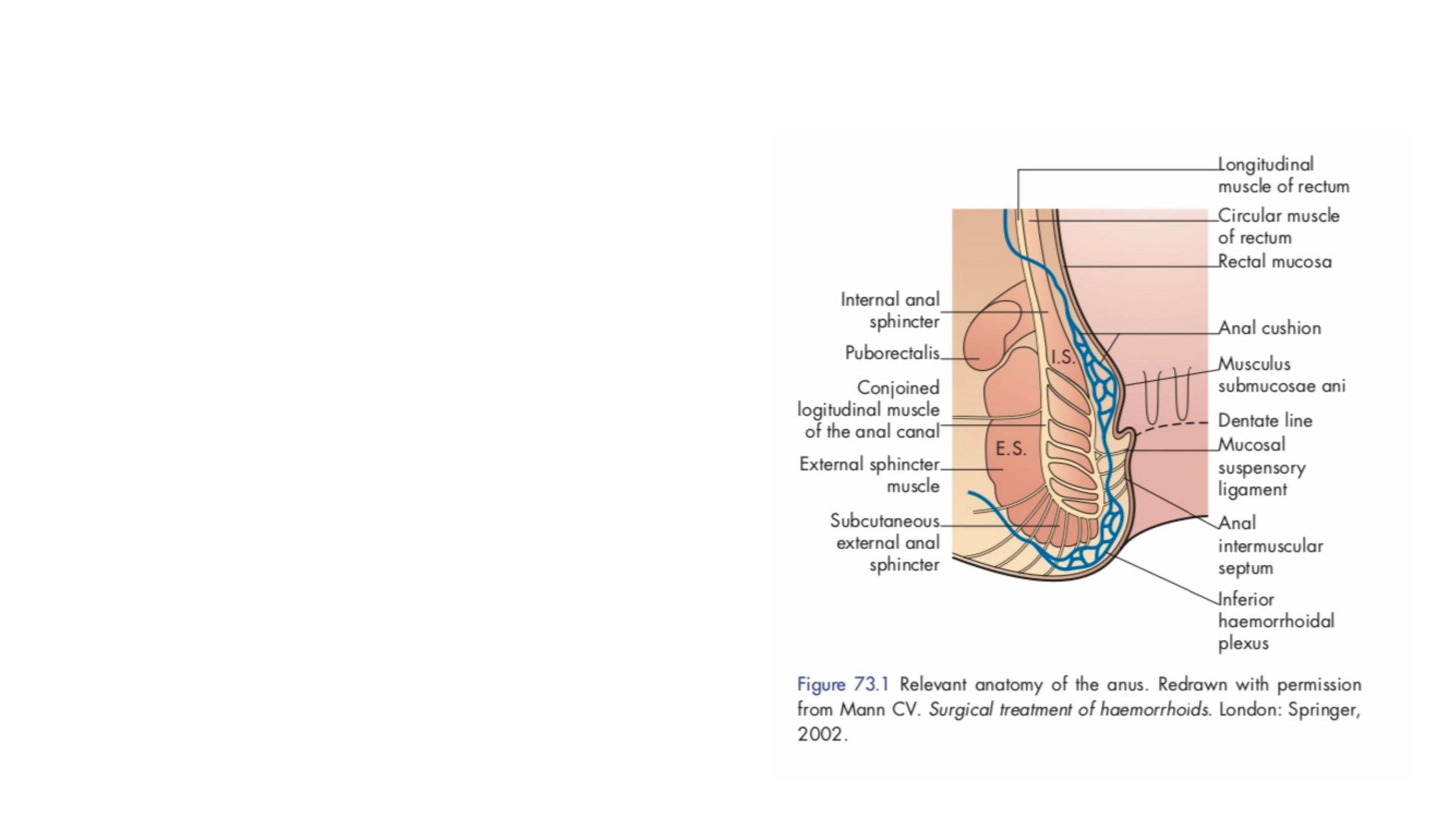
The internal sphincter is a condensation
of the circular muscle of the bowel wall.
The external sphincter is a composite
striated muscle. Its lower fibres encircle
the anal canal and they can be subdivided
into deep, superficial and subcutaneous
portions.
The dentate line represents the site
of fusion of the proctodaeum and
post- allantoic gut.
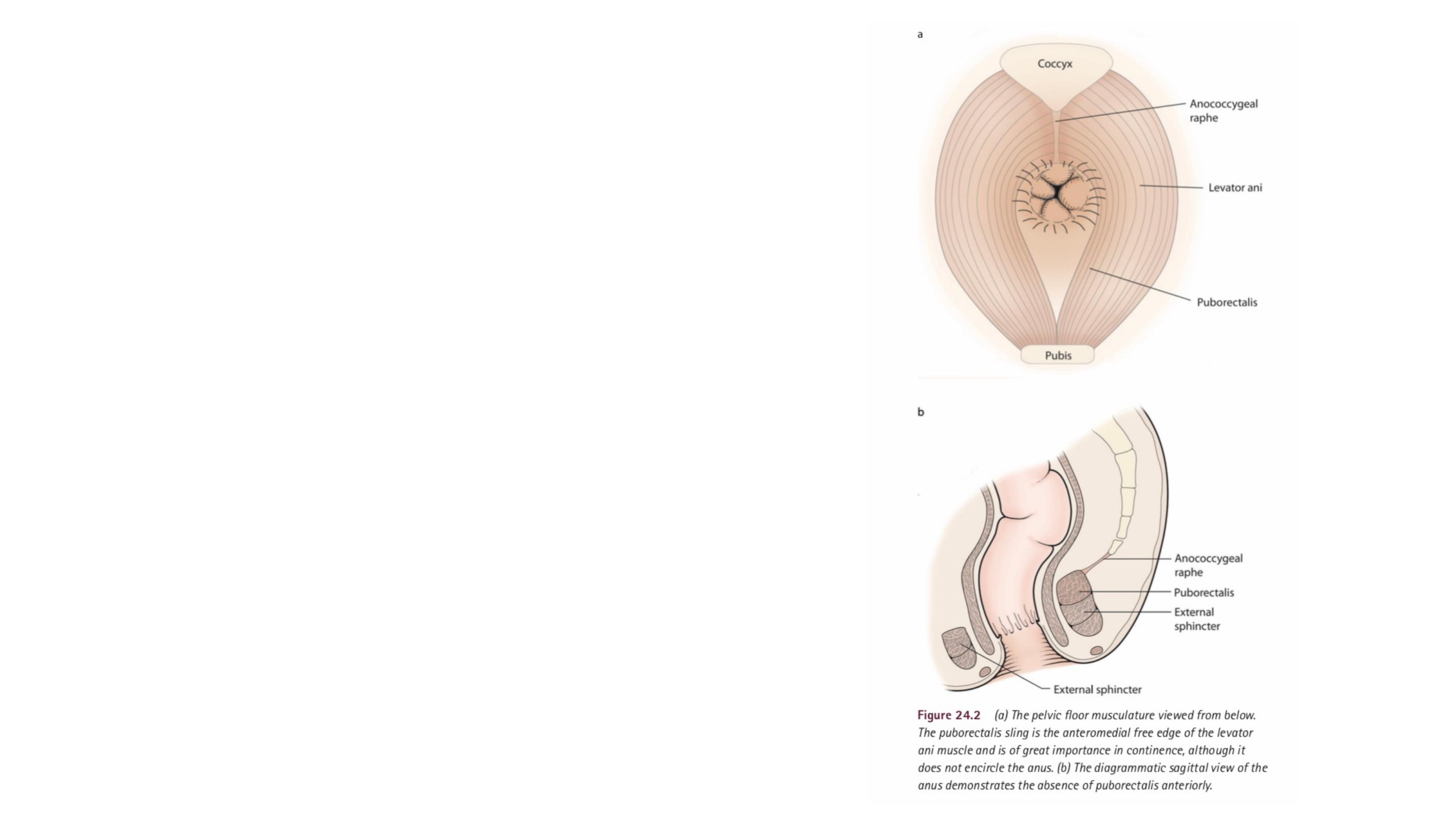
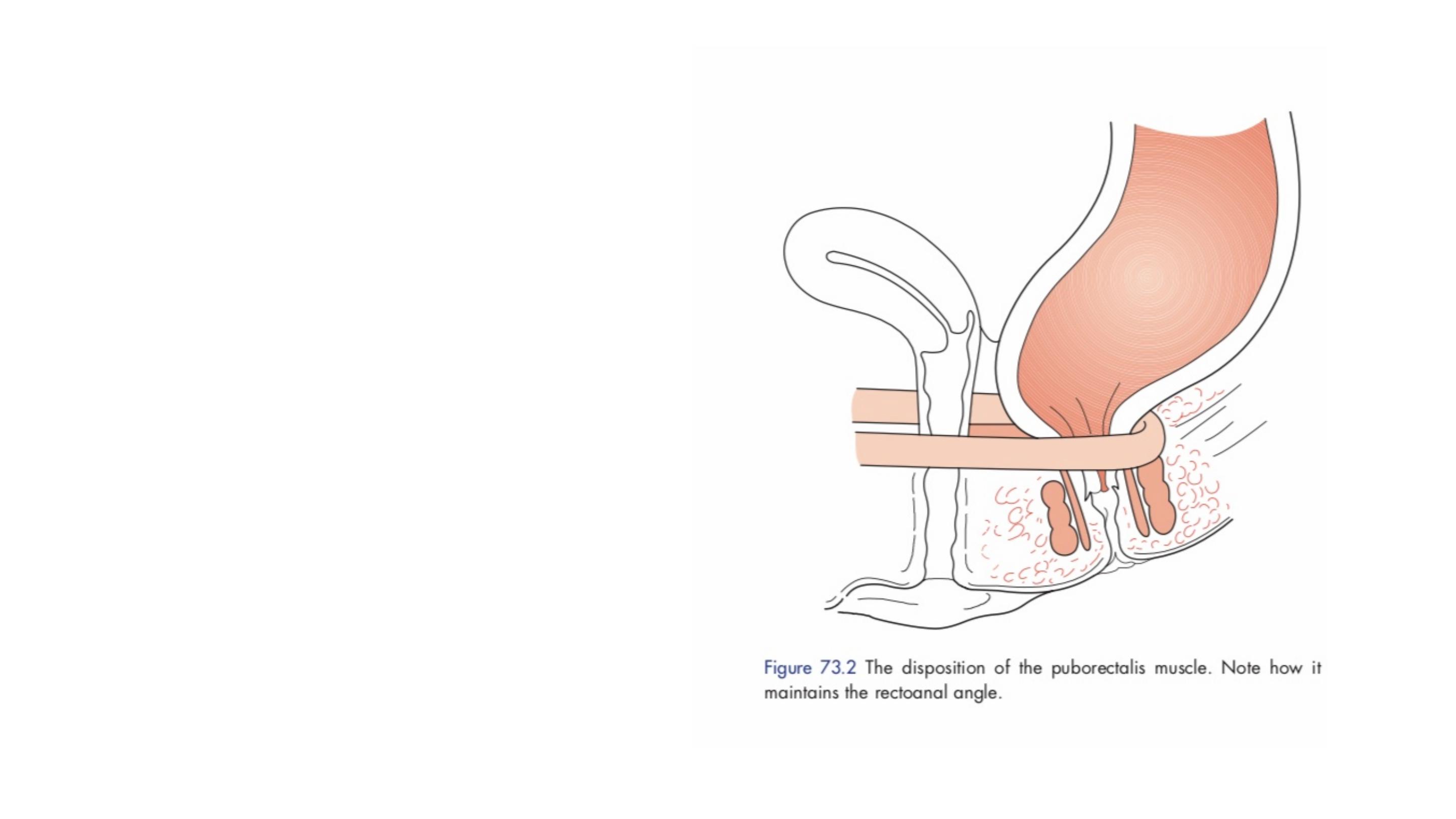
Superiorly, the external sphincter
blends with the puborectalis portion
of the levator ani muscle of the
pelvic floor.
The puborectalis muscle sling does
not encircle the anus and is
deficient anteriorly.

The anal glands lie partly in the submucosal plane and partly between the
sphincters in the intersphincteric plane; infection in these glands is thought to
be the main cause of peri- anal sepsis and fistulae. The orifices of the glands
open just above the anal valves and this is therefore the commonest site of
the internal opening for a fistula.

Vascular plexi lie beneath the mucosa of the anal canal.
The main arterial inflow is from the terminal branches of the superior
rectal artery, which classically divides into a left lateral, a right
anterolateral and a right posterolateral branch; they anastomose with
branches of the inferior rectal artery. Three small swellings, or anal
cushions, are associated with the underlying vascular plexi.
Blood supply to the anal canal is via superior, middle and inferior rectal vessels
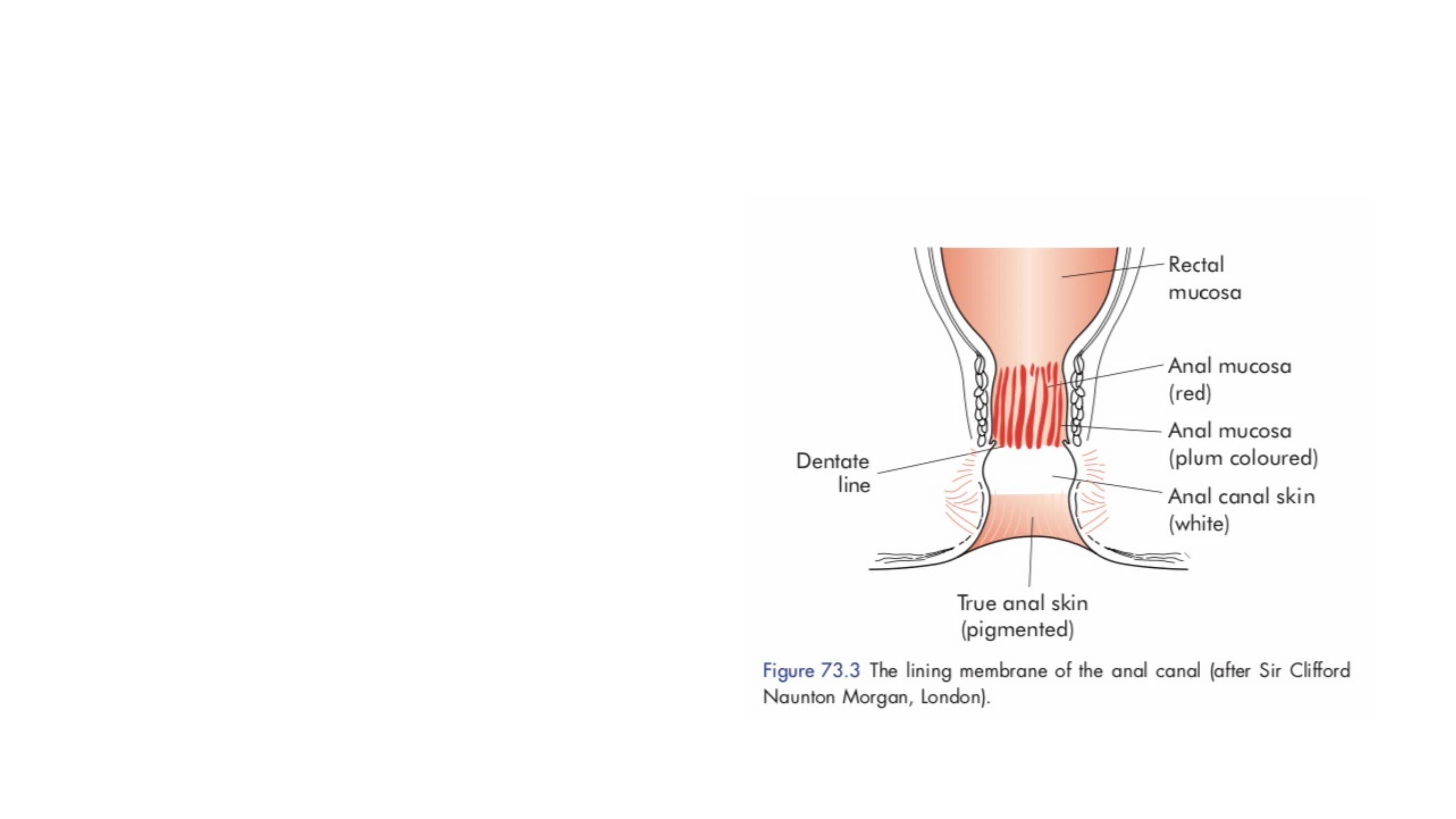
The epithelium of anal canal
The lining of the anal canal above
the dentate line is similar to the
columnar epithelium of the colon
and rectum, except that there is a
junctional zone extending for about
1 cm above the dentate line.
Below this line it is modified skin,
or anoderm, consisting of
squamous epithelium.

This change in the mucosa is important, as malignant lesions
arising in the distal anal canal are more likely to be squamous cell
carcinomas than adenocarcinomas.
The dentate line also marks the watershed for lymphatic drainage.
The upper anal canal drains to the inferior mesenteric nodes and
the lower anal canal to the inguinal nodes.
The dentate line is also the division between somatic and visceral
sensation. Distal pathology in the anal canal may thus be
extremely painful.
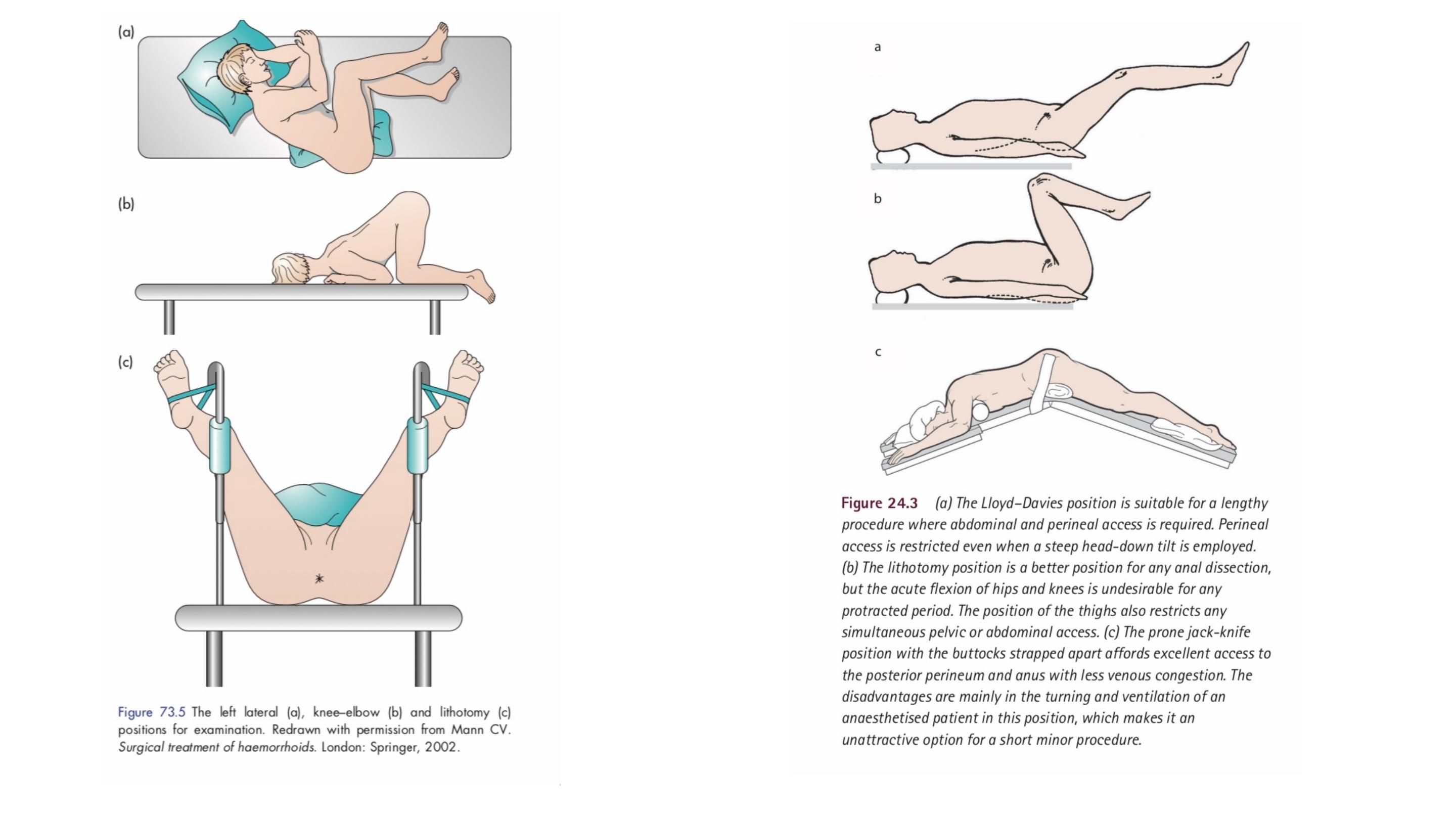

EXAMINATION OF THE ANUS
Careful clinical examination will be diagnostic in the vast majority of
patients complaining of anal symptoms, but it requires a relaxed patient
who is informed of what the examination will entail, a private environment, a
chaperone (for the security of both parties) and good light.
A rectal examination is essential for any patient with anorectal and/or
bowel symptoms – ‘If you don’t put your finger in, you might put your
foot in it’
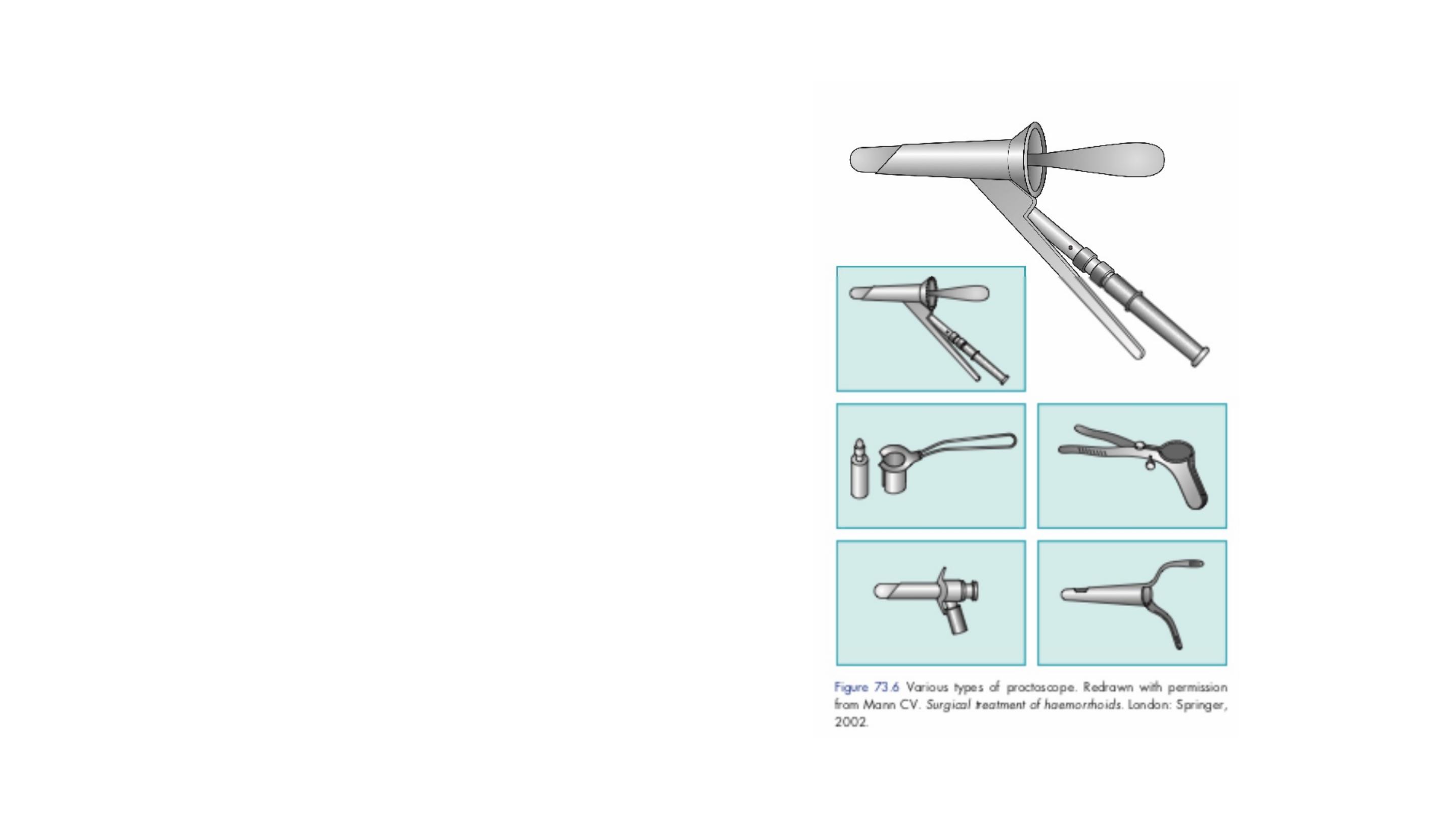
A proctosigmoidoscopy is essential in any
patient with bowel symptoms, and particularly
if there is rectal bleeding
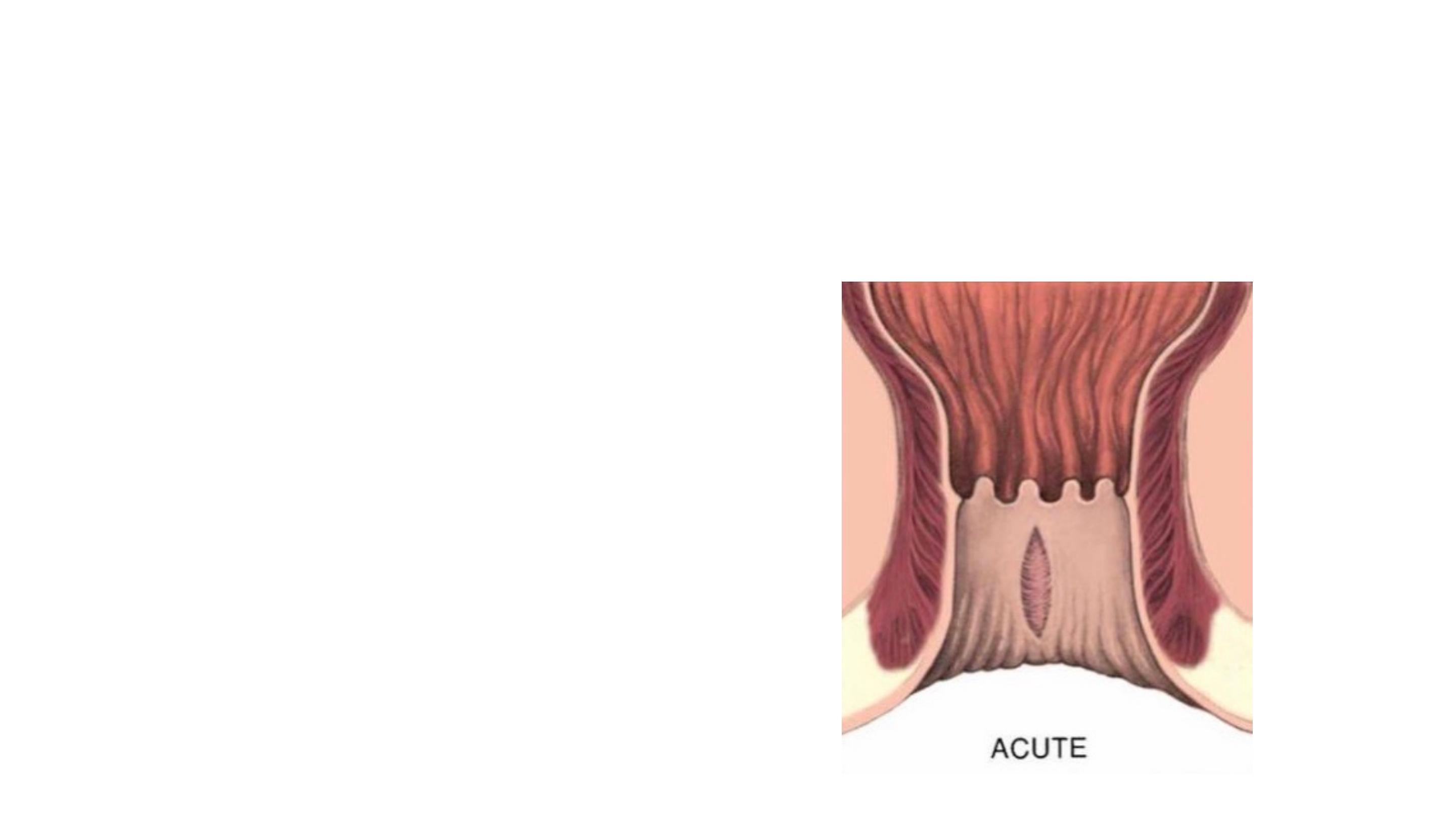
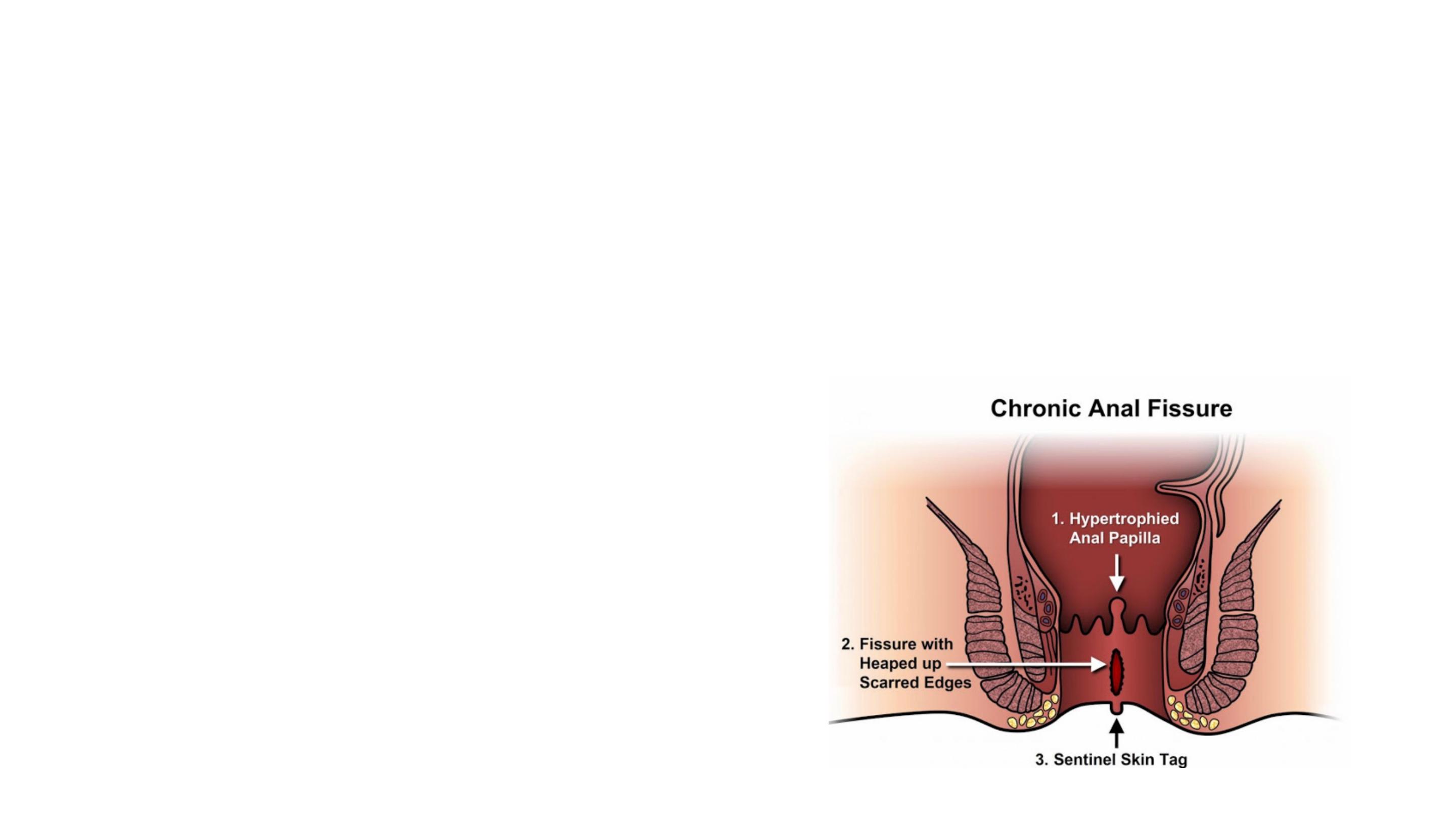
ANAL FISSURE
An anal fissure is a longitudinal split in the anoderm of the distal
anal canal which extends from the anal verge proximally towards,
but not beyond, the dentate line.
Symptoms
:
•
Pain on defaecation
•
Bright-red bleeding
•
Mucous discharge
•
Constipation

Anal fissure typically located in the Posterior midline of anus.
~10% of women have anterior midline lesions—weakest muscular
support
Classically, acute anal fissures arise from the trauma caused by the
strained evacuation of a hard stool or, less commonly, from the
repeated passage of diarrhoea.
Chronicity may result from repeated
trauma, anal hypertonicity and vascular
insufficiency, either secondary to
increased sphincter tone or because
the posterior commissure is less well
perfused than the remainder of the anal
circumference.

Treatment of an anal fissure
■
Conservative initially, consisting of stool-bulking agents and
softeners, and chemical agents in the form of ointments designed
to relax the anal sphincter and improve blood flow
■
Conservative management should result in the healing of almost
all acute and the majority of chronic fissures.

Such agents include glyceryl trinitrate (GTN) 0.2 per cent applied four times per
day to the anal margin (although this may cause headaches) and diltiazem 2 per
cent applied twice daily.
■ Surgery if above fails, consisting of lateral internal sphincterotomy or
anal advancement flap

Hemorrhoids are cushions of submucosal tissue containing venules,
arterioles, and smooth muscle fibers that are located in the anal canal.
Three hemorrhoidal cushions are found in the left lateral, right anterior,
and right posterior positions.
Cushions are thought to function as part of the continence mechanism
and aid in complete closure of the anal canal at rest. Because
hemorrhoids are a normal part of anorectal anatomy, treatment is only
indicated if they become symptomatic.
Haemorrhoids (Greek: haima, blood; rhoos, flowing; synonym:
piles, Latin: pila, a ball)

External haemorrhoids relate to venous channels of the inferior
haemorrhoidal plexus and located distal to the dentate line and are
covered with anoderm.
Because the anoderm is richly innervated, thrombosis of an external
hemorrhoid may cause significant pain.
Internal hemorrhoids are located proximal to the dentate line and
covered by insensate anorectal mucosa.
Combined internal and external hemorrhoids straddle the dentate
line and have characteristics of both internal and external
hemorrhoids.

Causes of hemorrhoid
Engorged anal cushions and vessels from increased pelvic/
abdominal pressures:
•
Constipation/straining
•
Pregnancy
•
Ascites/abdominal tumors
•
Portal hypertension

Symptoms of haemorrhoids:
•
Bright-red, painless bleeding
•
Mucous discharge
•
Prolapse
•
Pain only on prolapse
Internal hemorrhoids may prolapse or bleed, but rarely become painful
unless they develop thrombosis and necrosis (usually related to severe
prolapse, incarceration, and/or strangulation).

■ First degree – bleed only, no prolapse
■ Second degree – prolapse, but reduce spontaneously
■ Third degree – prolapse and have to be manually reduced
■ Fourth degree – permanently prolapsed
Internal hemorrhoid are graded according to the extent of
prolapse into four degree:

Complications of haemorrhoids
■ Strangulation and thrombosis
■ Ulceration
■ Gangrene
■ Portal pyaemia
■ Fibrosis
Management
Exclusion of other causes of rectal bleeding, especially colorectal
malignancy, is the first priority.
Important measures include attempts at normalising bowel and defaecatory
habits: only evacuating when the natural desire to do so arises, adopting a
defaecatory position to minimise straining, and the addition of stool soften-
ers and bulking agents to ease the defaecatory act.
Various creams can be inserted into the rectum from a collapsible tube fitted
with a nozzle, at night and before defaecation. Suppositories are also useful.
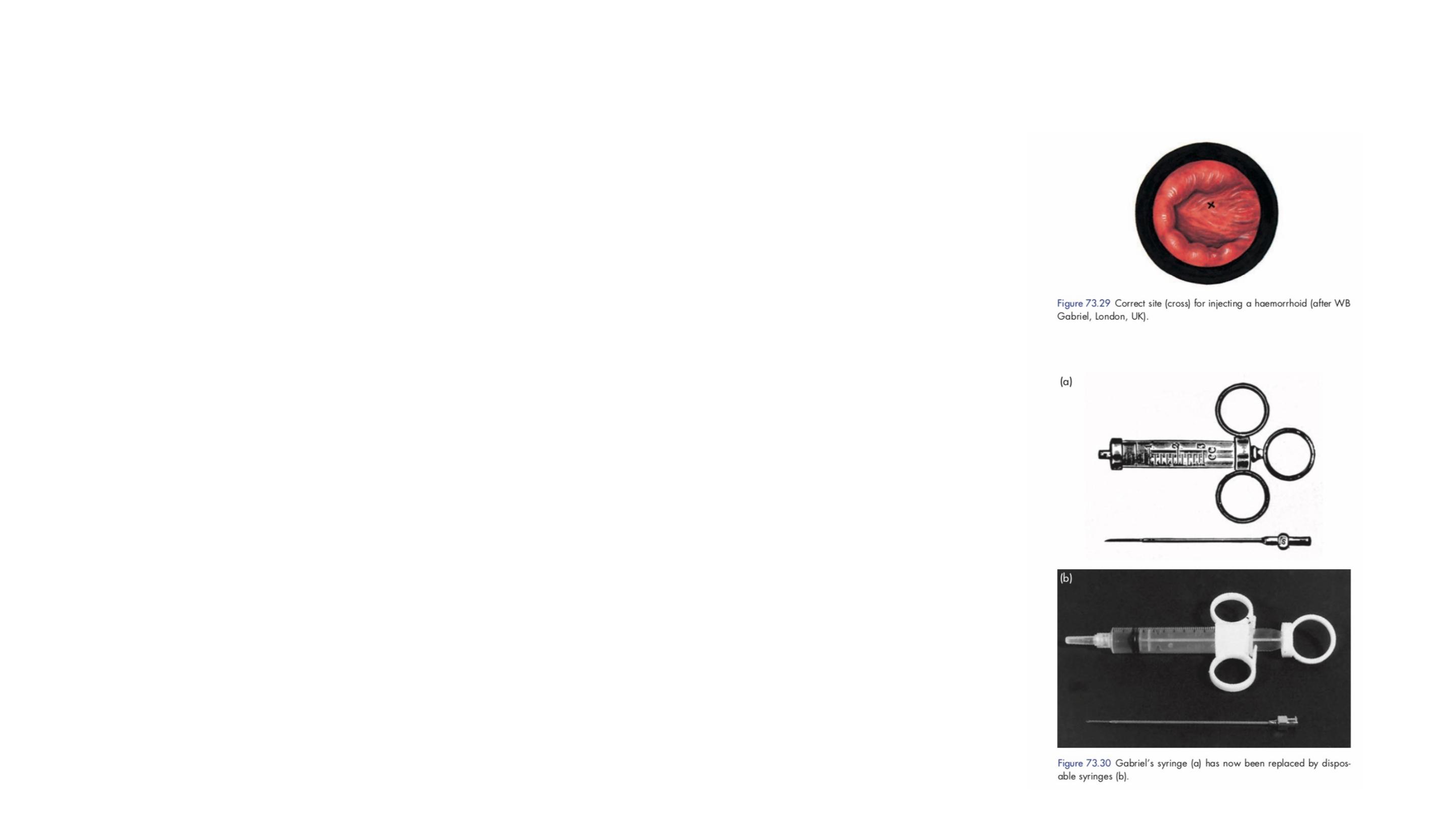
Sclerotherapy
A submucosal injection of 5 per cent phenol
in almond oil causes both thrombosis of the
feeding vessels and fibrosis, which tethers
the lax mucosa, thus reducing prolapse.
Infrared photocoagulation
With infrared photocoagulation (IRPC) an infrared radiation
source is applied immediately proximal to the upper
margin of the haemorrhoid.
The aim is to create fibrosis, cause obliteration of
the vascular channels and hitch up the anorectal
mucosa.
In those with first- or second-degree piles whose symptoms are not
improved by conservative measures,
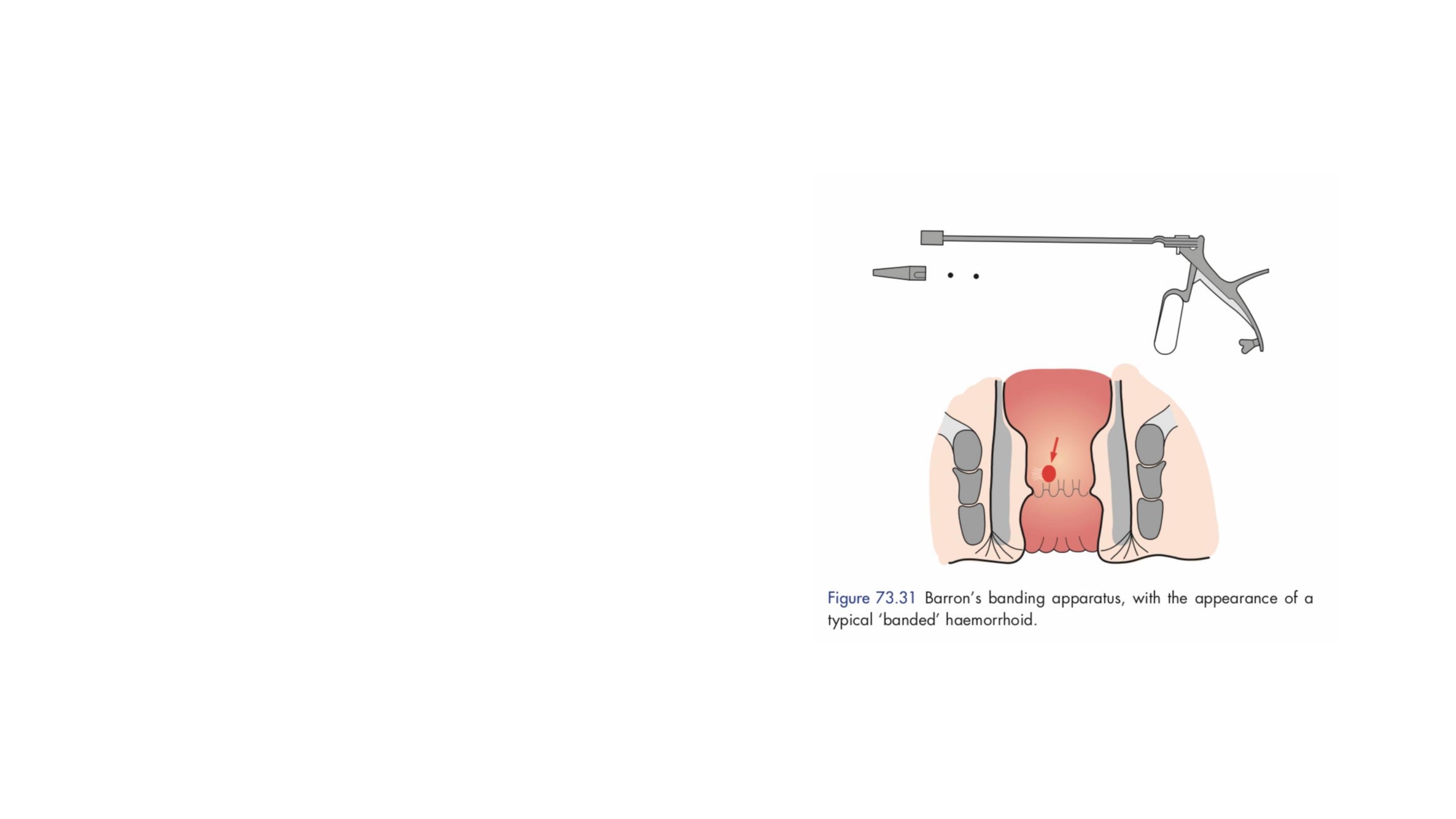
Banding
For more bulky piles, banding has been
shown to be efficacious, but it is
associated with more discomfort.
The Barron’s bander is a commonly
available device used to slip tight elastic
bands onto the base of the pedicle of each
haemorrhoid.
The bands cause ischaemic necrosis of the
piles, which slough off within 10 days; this
may be associated with bleeding, about
which the patient must be warned.

Operation management
The indications for haemorrhoidectomy include:
Third- and fourth-degree haemorrhoids
Second-degree haemorrhoids that have not been cured by
non-operative treatments
Fibrosed haemorrhoids
Interoexternal haemorrhoids when the external
haemorrhoid is well defined.
Surgical treatment of haemorrhoids
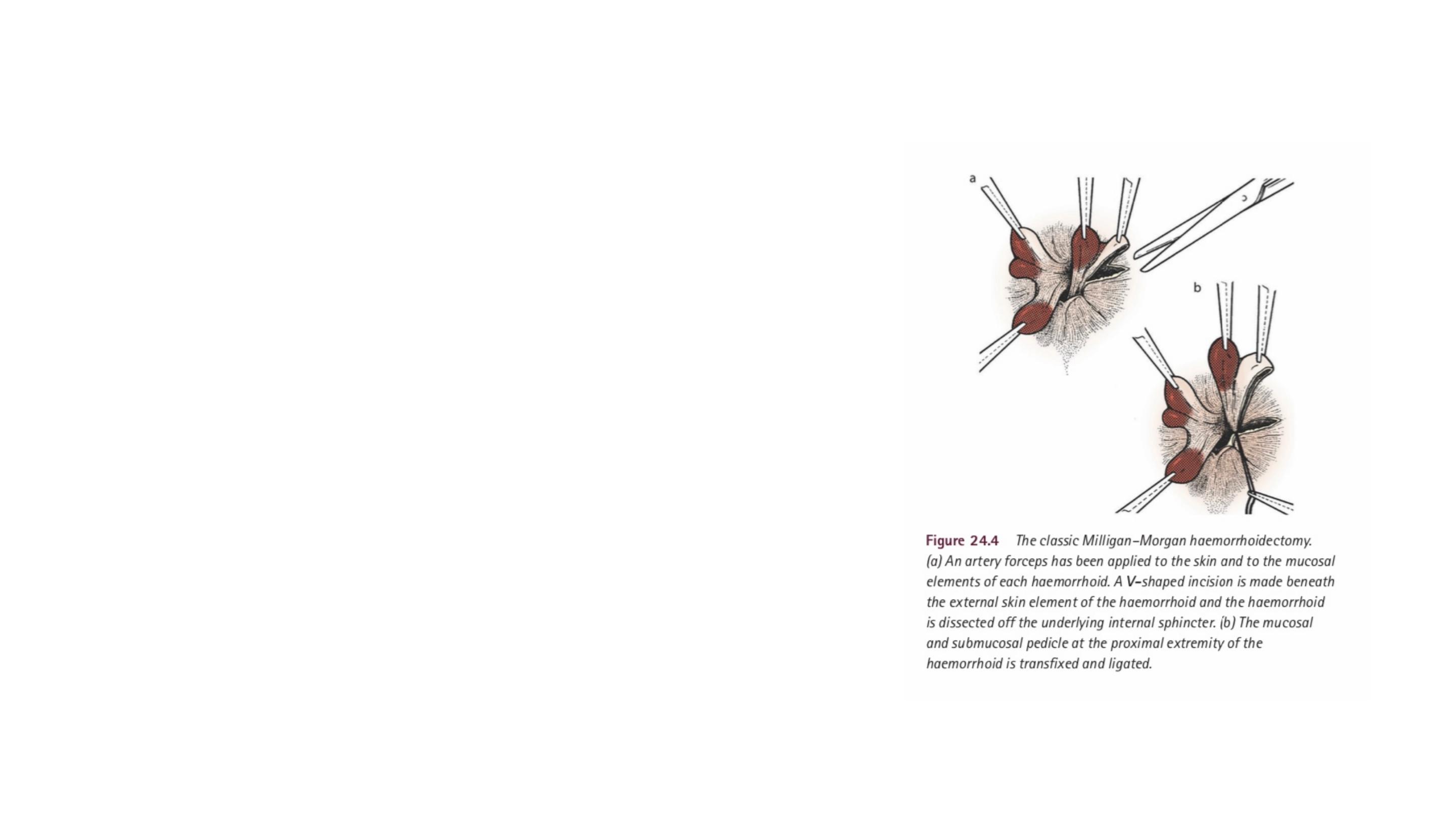
MILLIGAN–MORGAN HAEMORRHOIDECTOMY
In this classical operation involves resection of
hemorrhoidal tissue.
Adequate bridges of skin and mucosa must be left
intact between the excisions to prevent anal
stenosis developing during healing.

Closed Submucosal Hemorrhoidectomy.
The Parks or Ferguson hemorrhoidectomy involves resection of
hemorrhoidal tissue and closure of the wounds with absorbable
suture.
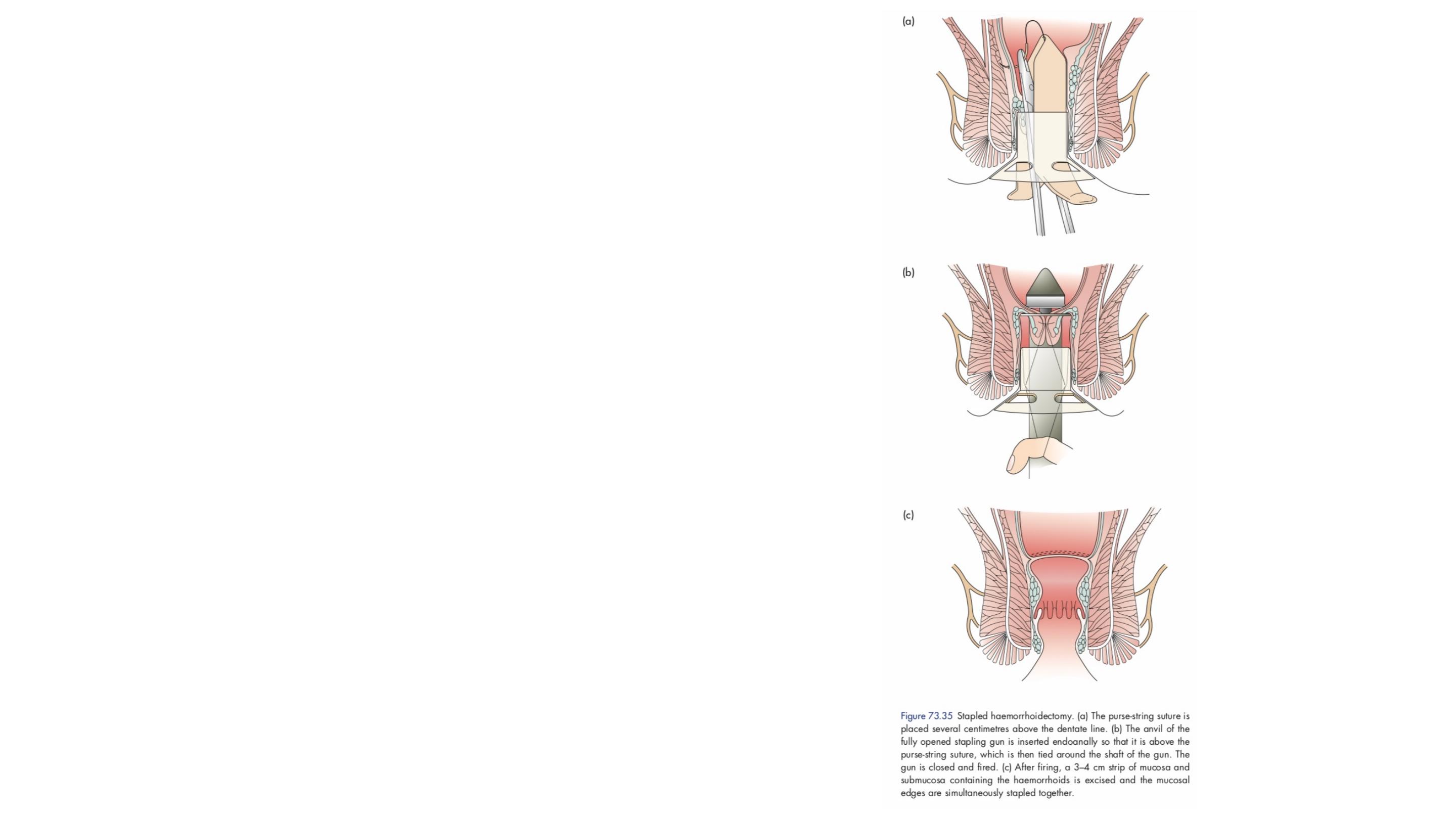
Procedure for prolapse and hemorrhoids
(PPH) removes a short circumferential segment
of rectal mucosa proximal to the dentate line
using a circular stapler.
This effectively ligates the venules feeding the
hemorrhoidal plexus and fixes redundant mucosa
higher in the anal canal.

Transanal haemorrhoidal dearterialisation
In this procedure, a Doppler probe is used to identify the artery or arteries
feeding the hemorrhoidal plexus. These vessels are then ligated.

Complications of haemorrhoidectomy
Early
•
Pain
•
Acute retention of urine
•
Reactionary haemorrhage
Late
•
Secondary haemorrhage
•
Anal stricture
•
Anal fissure
•
Incontinence

Thank you
