Vermiform appendix
ا د ﻣﮭﻧد اﻟﺷﻼه
Understanding applied anatomy , micro anatomy
and pathophysiology
Describe the clinical features, investigations and
principles of management of diseases of Appendix
including appendicitis and its complications.
Learning objectives

The vermiform appendix is importance in surgery due to its
propensity for inflammation, which results in the clinical syndrome
known as ‘acute appendicitis’.
The vermiform appendix is a blind muscular tube with mucosal,
submucosal, muscular and serosal layers.
Acute appendicitis is the most common cause of an ‘acute abdomen’ in
young adults.
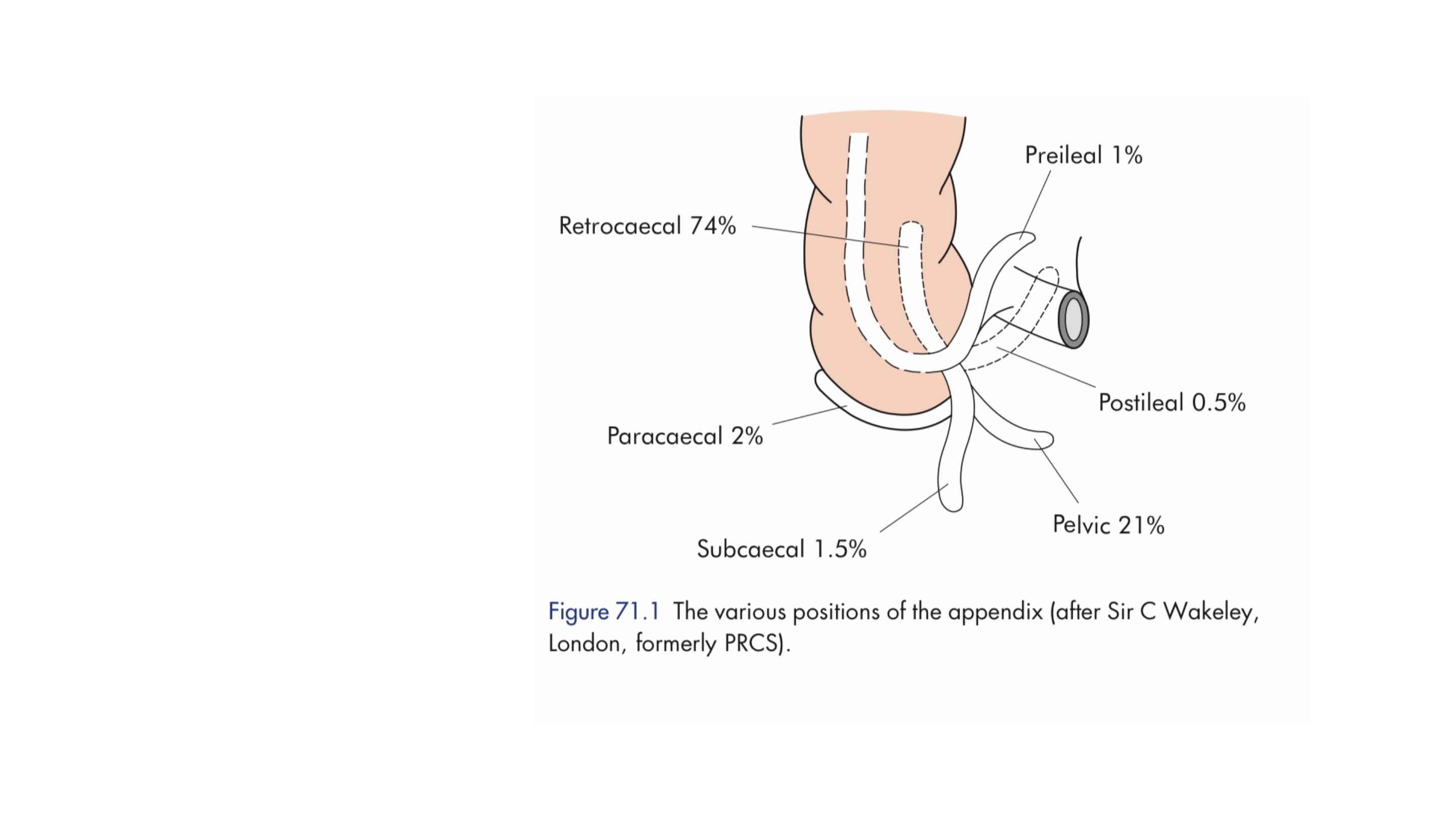
Applied anatomy
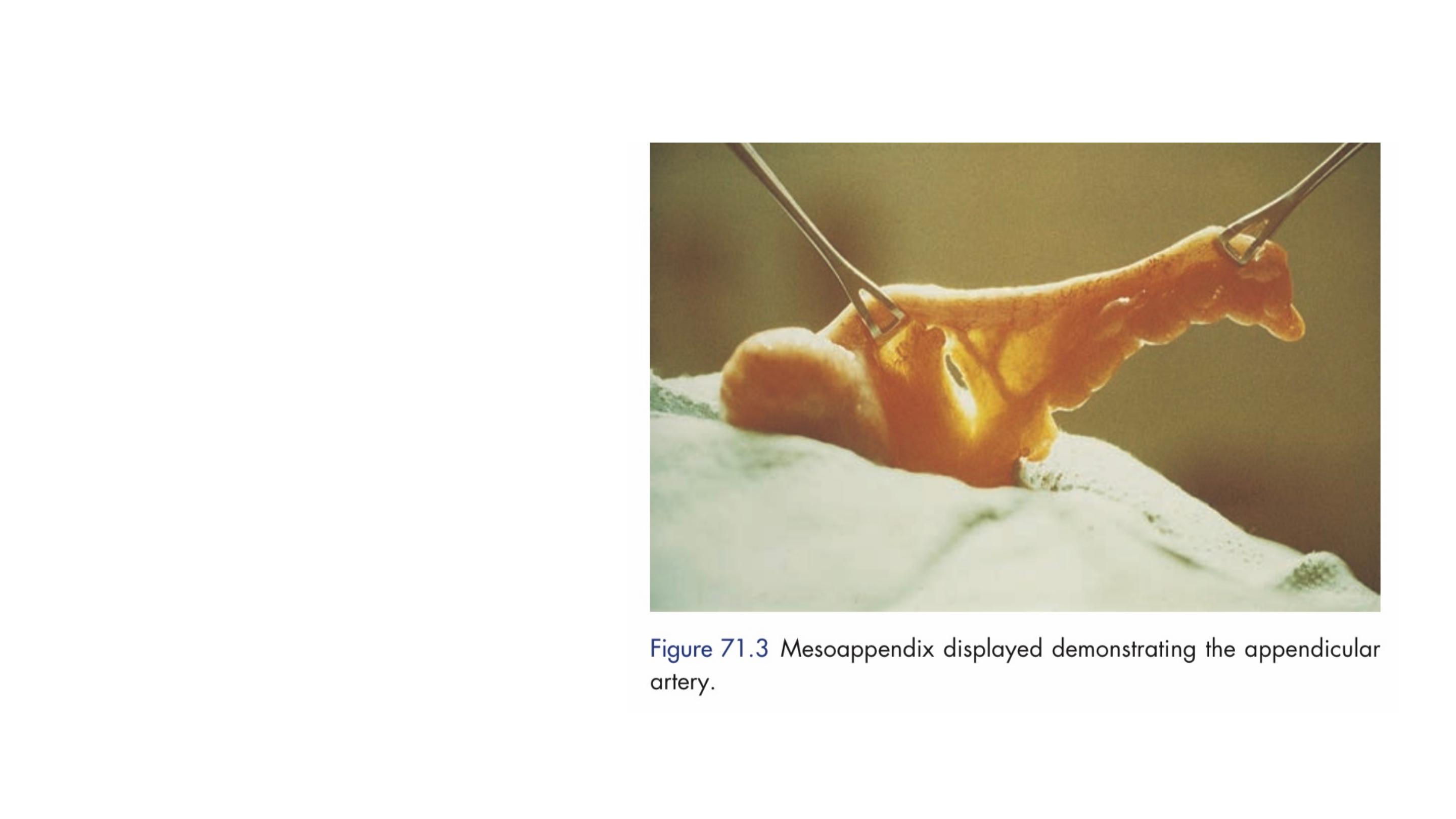
The position of the base of the
appendix is constant. It is found
at the confluence of the three
taeniae coli, an anatomical fact
often used to find the appendix
during an operation for acute
appendicitis.
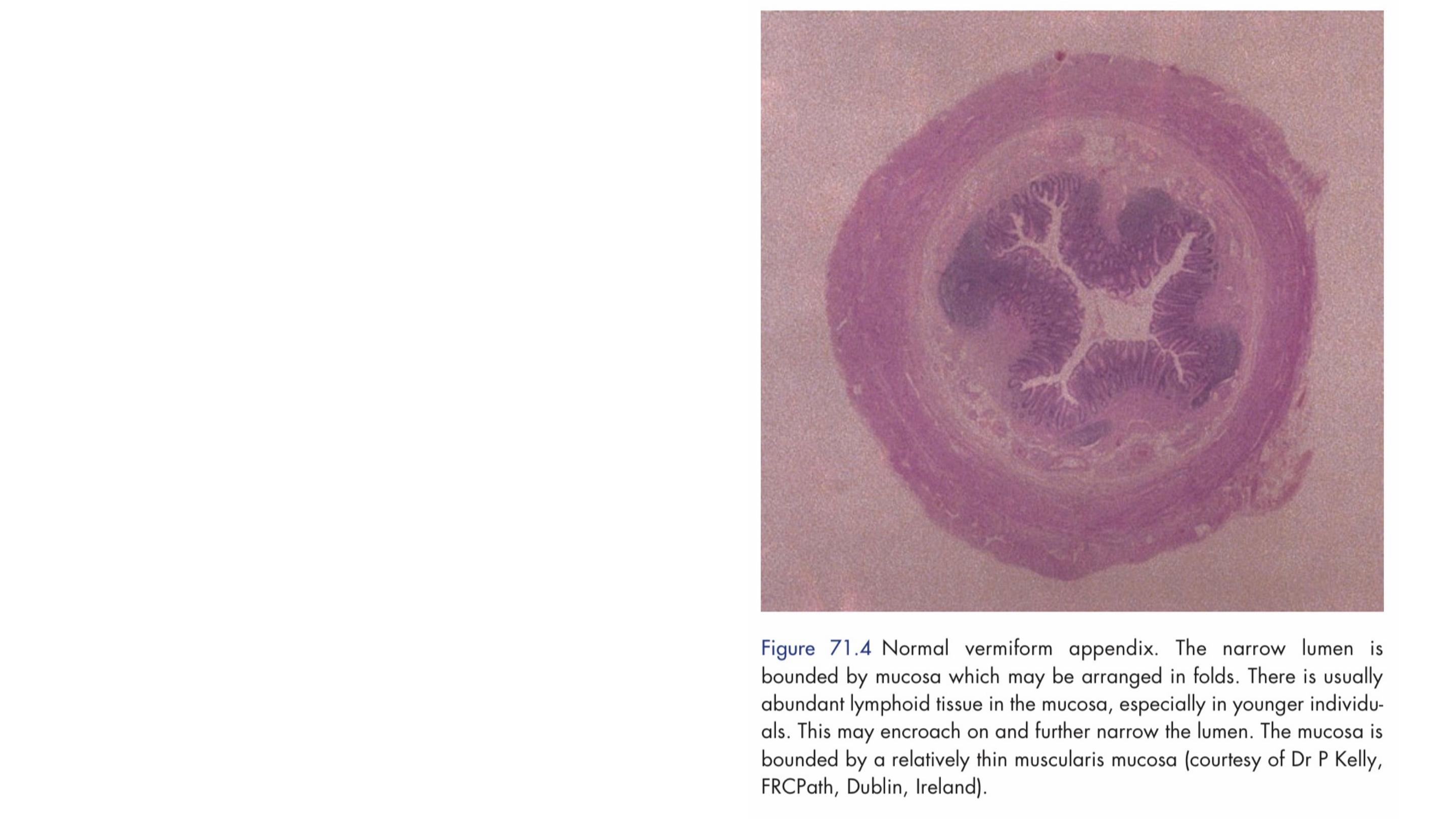
Histologically the submucosa of
the appendix is rich in lymphoid
follicles. In the base of the
appendicular crypts argentaffin
(Kulschitsky) cells, the source of
carcinoid tumours, are present.
It’s lined by columnar cell intestinal
mucosa of colonic type.
Microscopic anatomy

The pathophysiologic process leading to acute appendicitis was initially
described by Dr. Reginald Fitz in 1886, where appendicitis was described as
a process that began with appendiceal luminal obstruction that led to
secondary bacterial infection, ischemia, necrosis, and perforation.
Causes result in lumen obstruction :
1. Hypertrophied lymphoid tissue
2. Fecalith
3. Foreign body
4. Parasite
5. Tumor (carcinoid)

Natural history of acute appendicitis
Once obstruction occurs, Oedema and mucosal ulceration
develop with bacterial translocation to the submucosa.
Resolution may occur at this point either spontaneously or
in response to antibiotic therapy.
If the condition progresses, further distension of the
appendix may cause venous obstruction and ischaemia of
the appendix wall.
Finally, ischaemic necrosis of the appendix wall produces
gangrenous appendicitis, with free bacterial contamination
of the peritoneal cavity.
Alternatively, the greater omentum and loops of
small bowel become adherent to the inflamed
appendix, walling off the spread of peritoneal
contamination, and resulting in a phlegmonous
mass or paracaecal abscess.
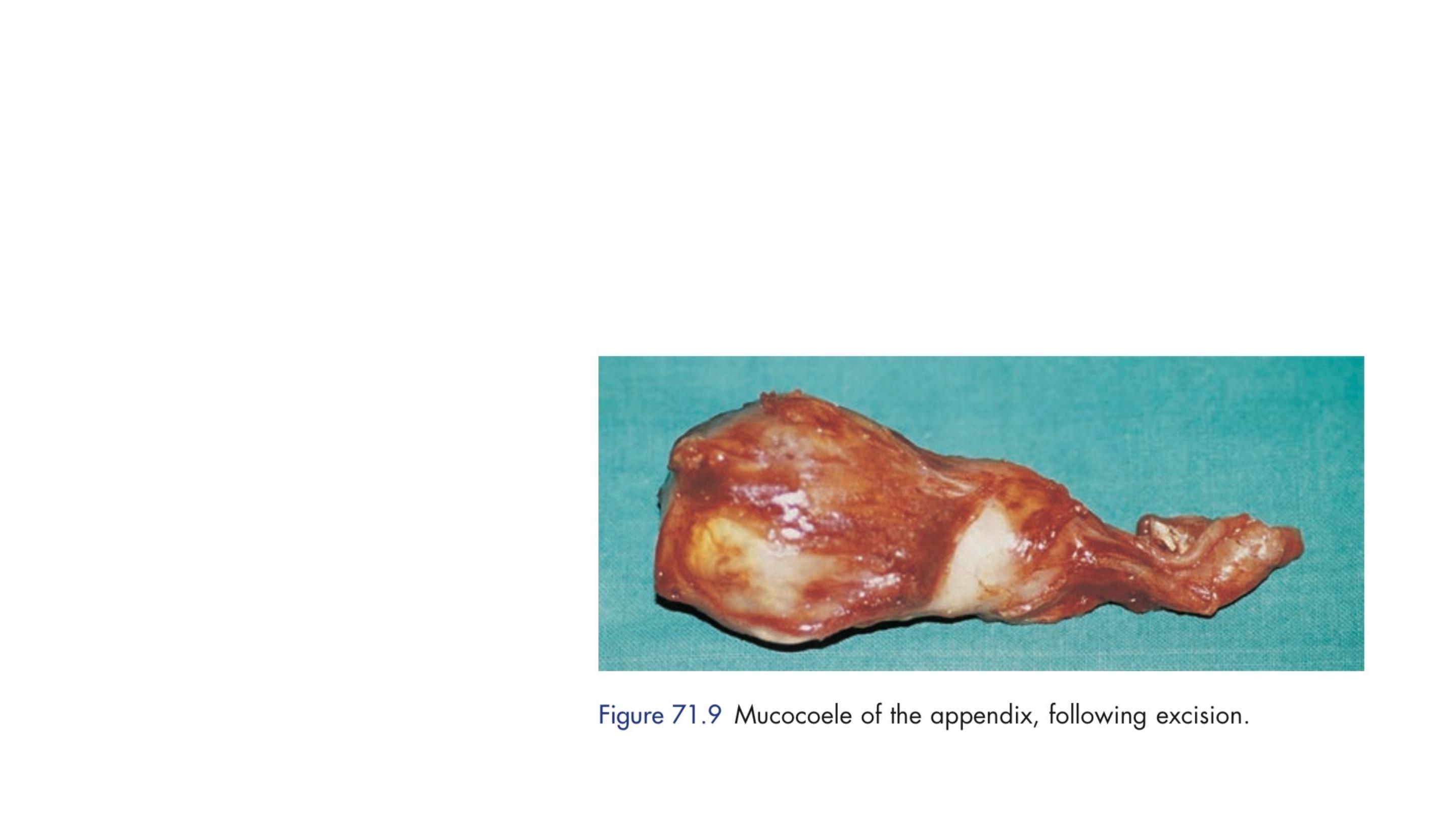
Rarely, appendiceal inflammation resolves,
leaving a distended mucus-filled organ termed a
‘mucocoele’ of the appendix.

Typically, two clinical syndromes of acute appendicitis can be
discerned, acute catarrhal (non-obstructive) appendicitis and acute
obstructive appendicitis, the latter characterised by a more acute
course.
Risk factors for perforation of the appendix
■ Extremes of age
■ Immunosuppression
■ Diabetes mellitus
■ Faecolith obstruction
■ Pelvic appendix
■ Previous abdominal surgery

Symptoms of appendicitis
■ Periumbilical colic
■
Pain shifting to the right iliac fossa
■
Anorexia
■ Nausea

Clinical signs in appendicitis
■ Pyrexia
■ Localised tenderness in the right iliac fossa
■ Muscle guarding
■ Rebound tenderness
■ Pointing sign
■ Rovsing’s sign
■ Psoas sign
■
Obturator sign
■
Cutaneous hyperaesthesia

Retrocaecal
Rigidity is often absent, and even application of deep pressure may
fail to elicit tenderness
However, deep tenderness is often present in the loin, and rigidity of
the quadratus lumborum may be in evidence.
Psoas spasm, due to the inflamed appendix being in contact with
that muscle, may be sufficient to cause flexion of the hip joint.
Hyperextension of the hip joint may induce abdominal pain when the
degree of psoas spasm is insufficient to cause flexion of the hip.
Special features, according to position of the appendix

Pelvic
Occasionally, early diarrhoea results from an inflamed appendix being in contact with
the rectum.
When the appendix lies entirely within the pelvis, there is usually complete absence of
abdominal rigidity, and often tenderness over McBurney’s point is also lacking.
In some instances, deep tenderness can be made out just above and to the right of
the symphysis pubis.
In either event, a rectal examination reveals tenderness in the rectovesical pouch or the
pouch of Douglas, especially on the right side.
Spasm of the psoas and obturator internus muscles may be present when the
appendix is in this position.
An inflamed appendix in contact with the bladder may cause frequency of micturition.
This is more common in children.
Postileal
It presents the greatest difficulty in diagnosis because the pain may not shift,
diarrhoea is a feature and marked retching may occur.
Tenderness, if any, is ill defined, although it may be present immediately to
the right of the umbilicus.
Differential diagnosis
Acute gastroenteritis
Mesenteric lymphadenitis
Meckel’s diverticulitis
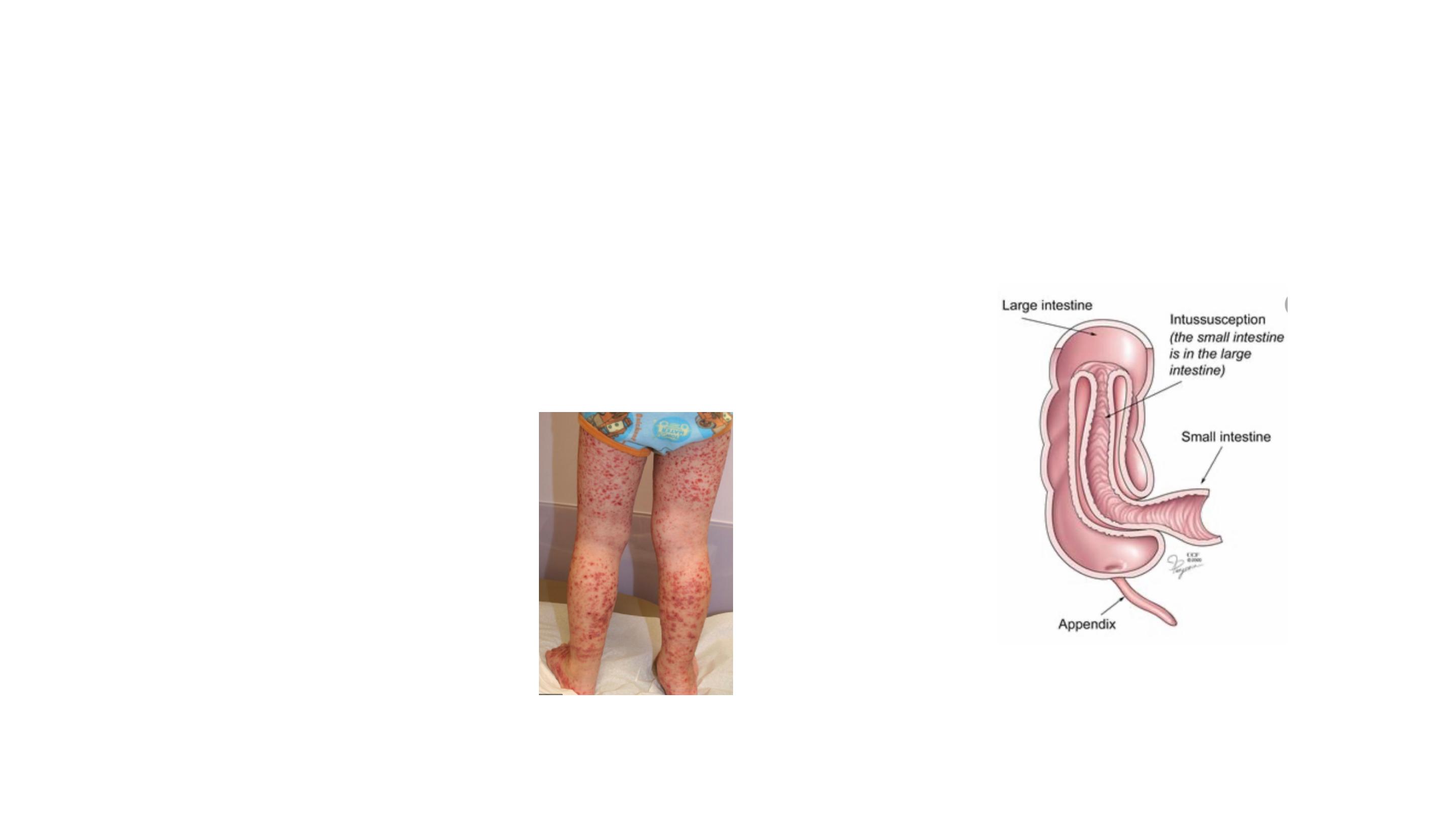
Intussusception
Henoch–Schönlein purpura
Lobar pneumonia and pleurisy

Regional enteritis
Ureteric colic
Right-sided acute pyelonephritis
Perforated peptic ulcer
Differential Diagnosis in Adult
Torsion of testis
Pancreatitis
Rectus sheath haematoma

Pelvic inflammatory disease (PID)
Mittelschmerz
Endometriosis
Pyelonephritis
Differential Diagnosis in adult female
Torsion or haemorrhage of an ovarian cyst
Ectopic pregnancy.

Diverticulitis
Intestinal obstruction
Colonic carcinoma
Differential Diagnosis in elderly
Torsion appendix epiploicae
Mesenteric infarction
Leaking aortic aneurysm

Preoperative investigations in appendicitis
■ Routine
Full blood count
Urinalysis
■ Selective
Pregnancy test
Urea and electrolytes
Supine abdominal radiograph
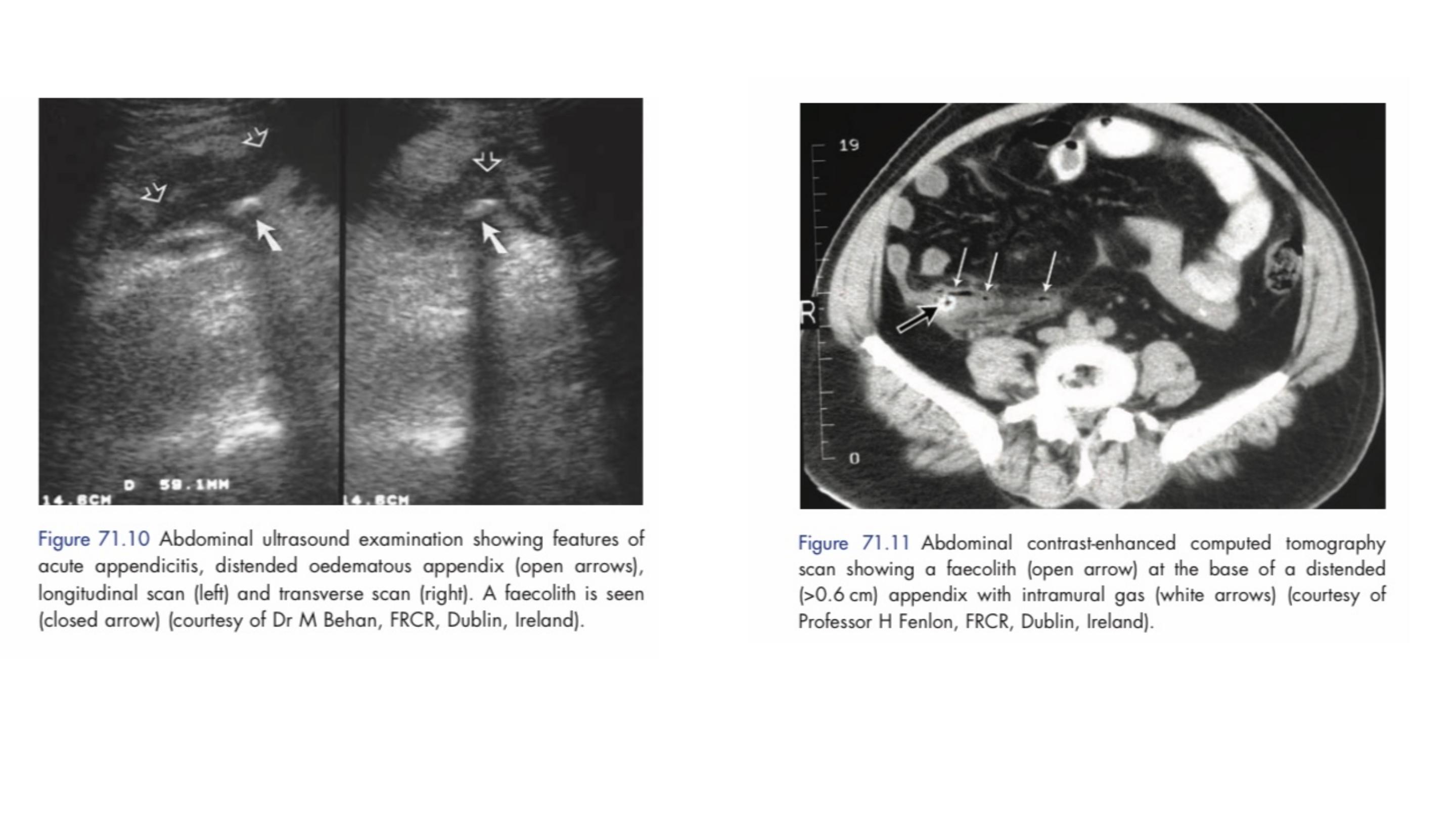
Ultrasound of the abdomen/pelvis
Contrast-enhanced abdomen and pelvic computed tomography scan

The diagnosis of acute appendicitis is essentially clinical;
however, a decision to operate based on clinical suspicion
alone can lead to the removal of a normal appendix in 15–
30 per cent of cases.
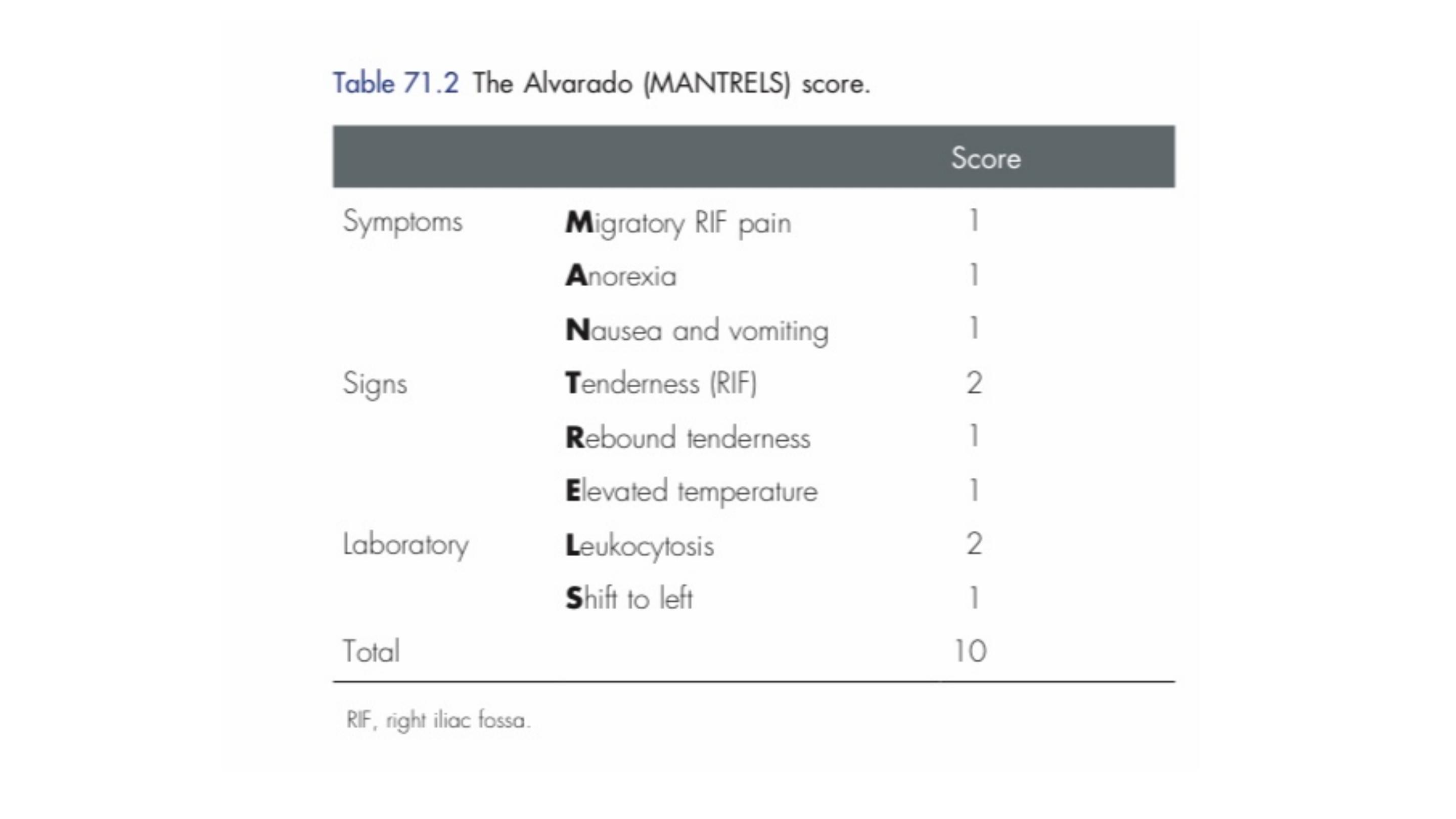

A score of 7 or more is strongly predictive of acute
appendicitis.
In patients with an equivocal score (5–6), abdominal
ultrasound or contrast-enhanced CT examination further
reduces the rate of negative appendicectomy.
What are the traditional treatment for acute
appendicitis ?
There is an emerging body of literature to support a
trial of conservative management in patients with
uncomplicated (absence of appendicolith, perforation or
abscess) appendicitis.

Treatment is bowel rest and intravenous antibiotics, usually
metranidazole and third-generation cephalosporin.
The available data indicate successful outcomes in 80–90 per cent of
patients, however there is an approximately 15 per cent recurrence
rate within one year.
This approach should be considered in patients with high operative
risk (multiple comorbidities).
Conservative management
Recommendation is to use laparoscopy and LA in patients with
suspected appendicitis unless laparoscopy itself is contraindicated or
not feasible. Especially young female, obese, and employed patients
seem to benefit from LA.

Thank you for your attention
