Lec: 3 Dr. Yasameen Alsaffar
The Adrenal Glands
The adrenals comprise several separate endocrine glands within a single anatomical structure. The adrenal medulla is an extension of the sympathetic nervous system which secretes catecholamines into capillaries.Most of the adrenal cortex is made up of cells which secrete cortisol and adrenal androgens, and form part of the hypothalamic–pituitary–adrenal (HPA) axis.
The small outer glomerulosa of the cortex secretes aldosterone under the control of the renin– angiotensin system. These functions are important in the integrated control of cardiovascular, metabolic and immune responses to stress.
Cushing’s syndrome
Cushing’s syndrome is caused by excessive activation of glucocorticoid receptors. It is most commonly iatrogenic, due to prolonged administration of synthetic glucocorticoids such as prednisolone. Endogenous Cushing’s syndrome is uncommon but is due to chronic over-production of cortisol by the adrenal glands, either as the result of an adrenal tumour or because of excessive production of ACTH by a pituitary tumour or ectopic ACTH production by other tumours.Causes:
1- ACTH-dependent – 80%• Pituitary adenoma secreting ACTH (Cushing’s disease) – 70%
• Ectopic ACTH syndrome (bronchial carcinoid, small-cell lung carcinoma, other neuro-endocrine tumour) – 10%
2- Non-ACTH-dependent – 20%
• Adrenal adenoma – 15%• Adrenal carcinoma – 5%
Hypercortisolism due to other causes (also referred to as pseudo-Cushing’s syndrome)
a- Alcohol excess (biochemical and clinical features)
b- Major depressive illness (biochemical features only, some clinical overlap)
c- Primary obesity (mild biochemical features, some clinical overlap)
d. Pregnancy or the use of oral contraceptive pills
Both Cushing’s disease and cortisol-secreting adrenal tumours are four times more common in women than men.
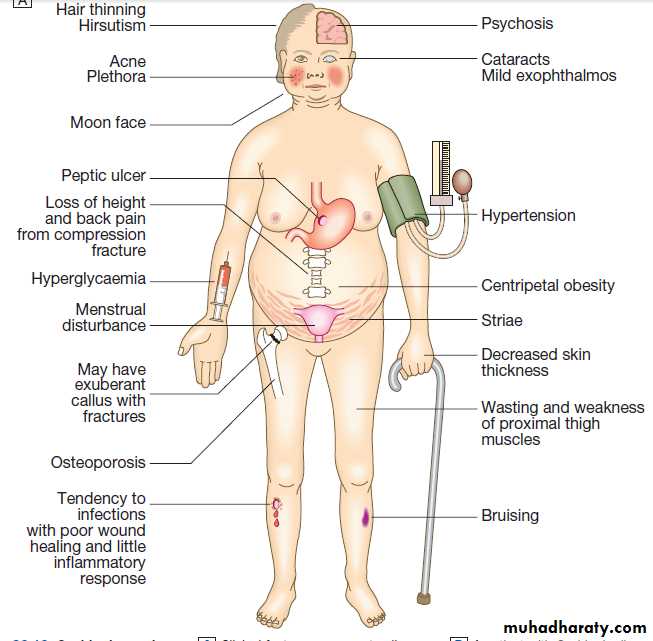
Clinical feature: as shown in figure below
Note 1: There are many diseases causes same clinical feature of Cushing syndrome such as obesity, alcoholism and depression so the features which favor Cushing’s syndrome in an obese patient are:1- Bruising
2- Myopathy3- Thin skin.
Note 2: Any clinical suspicion of cortisol excess is best resolved by further investigation.
Note 3: The high ACTH levels are associated with marked pigmentation because of binding to melanocortin1 receptors on melanocytes in the skin.
Note 4: When the tumour that is secreting ACTH is malignant, then the onset is usually rapid and may be associated with cachexia.
Investigations
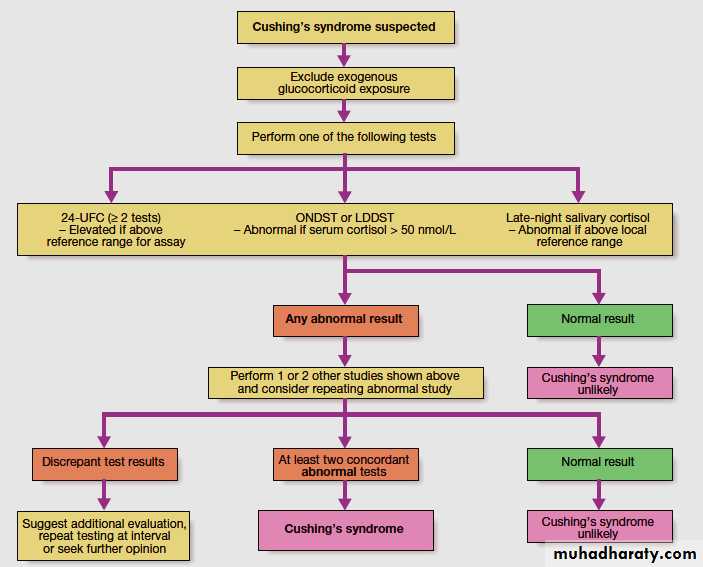
The large number of tests available for Cushing’s syndrome reflects the fact that each one has limited specificity and sensitivity in isolation. Accordingly, several tests are usually combined to establish the diagnosis.Testing for Cushing’s syndrome should be avoided under conditions of stress, such as an acute illness, because this activates the HPA axis, causing potentially spurious results. The diagnosis of Cushing’s is a two-step process:
1. To establish whether the patient has Cushing’s syndrome.
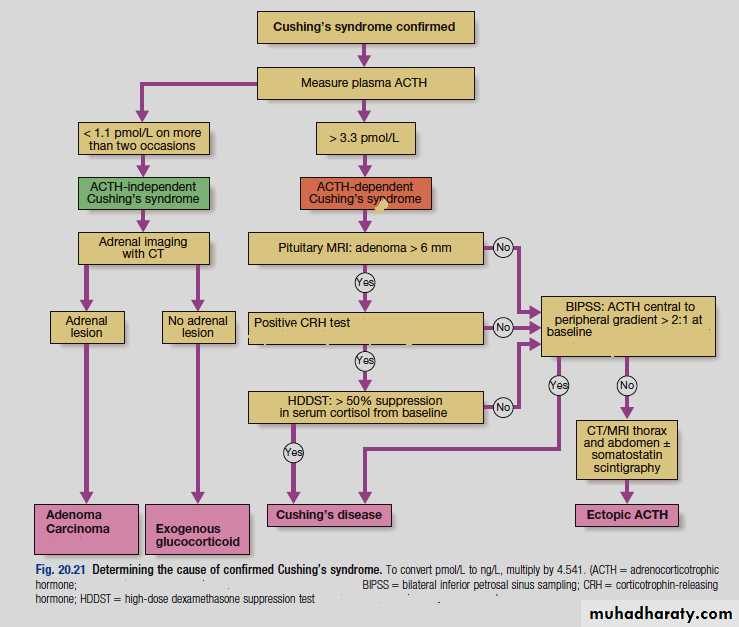
2. To define its cause:
Some additional tests are useful in all cases of Cushing’s syndrome, including plasma electrolytes, glucose, glycosylated haemoglobin and bone mineral density measurement.
Establishing the presence of Cushing’s syndrome
Cushing’s syndrome is confirmed by using two of three main tests:1. Failure to suppress serum cortisol with low doses of oral dexamethasone.
2. Loss of the normal circadian rhythm of cortisol, with inappropriately elevated late-night serum or salivary cortisol
3. Increased 24-hour urine free cortisol.
Dexamethasone is used for suppression testing because it does not cross-react in radioimmunoassays for cortisol. An overnight dexamethasone suppression test (ONDST) involves administration of 1 mg dexamethasone at 2300 hrs and measuring serum cortisol at 0900 hrs the following day. In a low-dose dexamethasone suppression test (LDDST), serum cortisol is measured following administration of 0.5 mg dexamethasone 4 times daily for 48 hours.
Use of multiple salivary cortisol samples over weeks or months can be of use in diagnosis, but an elevated salivary cortisol alone should not be taken as proof of diagnosis. In iatrogenic Cushing’s syndrome, cortisol levels are low unless the patient is taking a corticosteroid (such as prednisolone) that cross-reacts in immunoassays with cortisol.
Management
Untreated severe Cushing’s syndrome has 50% 5-year mortality. Most patients are treated surgically, but medical therapy may be given in severe cases for a few weeks prior to operation to improve the clinical state. A number of drugs are used to inhibit corticosteroid biosynthesis, including metyrapone and ketoconazole. The dose of these agents is best titrated against serum cortisol levels or 24-hour urine free cortisol.
Cushing’s disease
Trans-sphenoidal surgery carried out by an experienced surgeon with selective removal of the adenoma is the treatment of choice, with approximately 70% of patients going into immediate remission.Laparoscopic bilateral adrenalectomy performed by an expert surgeon effectively cures ACTH-dependent Cushing’s syndrome, but in patients with pituitary dependent Cushing’s syndrome, this can result in Nelson’s syndrome, with an invasive pituitary macroadenoma and very high ACTH levels causing pigmentation. The risk of Nelson’s syndrome may be reduced by pituitary irradiation.