Lec. 5
Dr. Mohammed Alhamdany
Tumours of the pancreas
Adenocarcinoma of the pancreas
Predisposing factors
The disease is associated with increasing age, smoking and chronic pancreatitis.
Between 5% and 10% of patients have a genetic predisposition; Men are
affected twice as often as women.
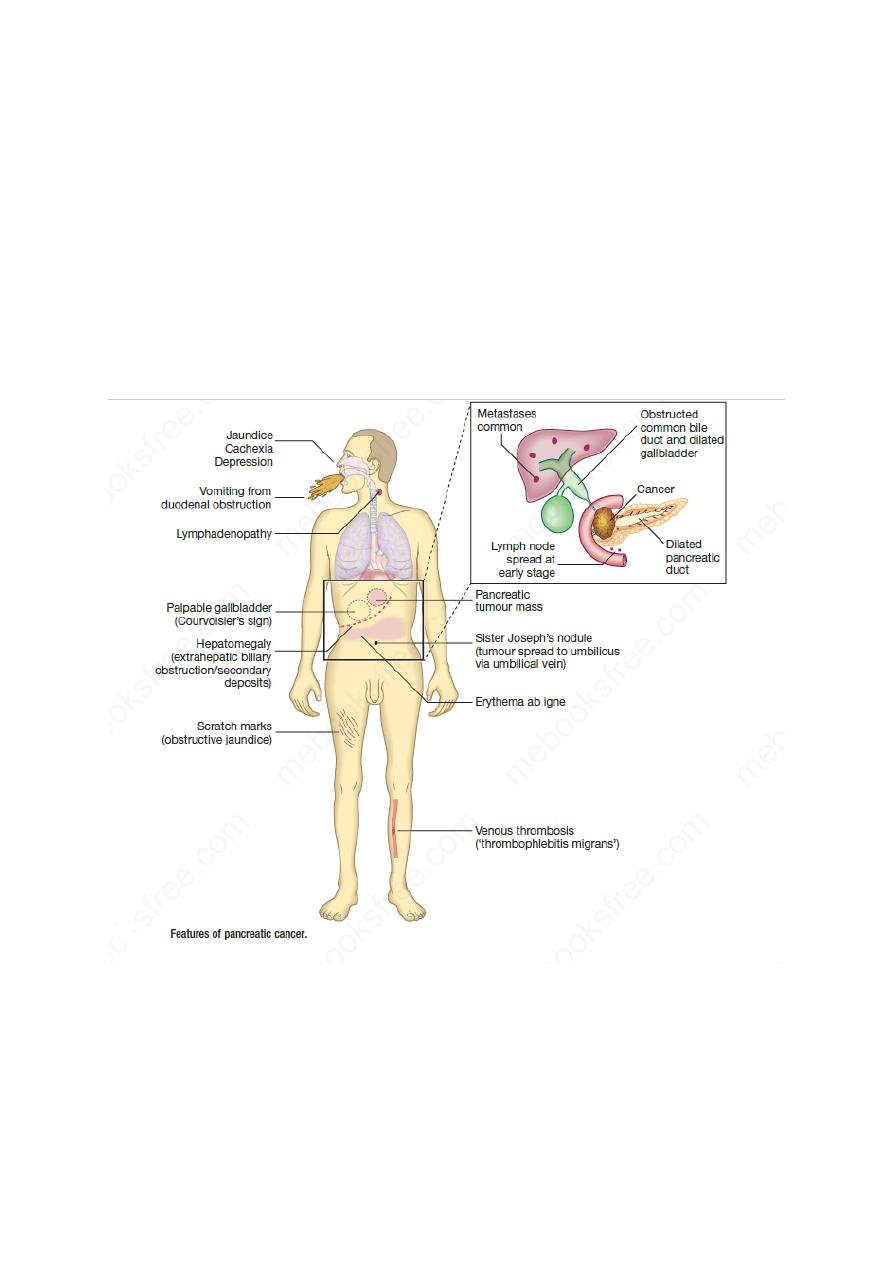
Clinical feature:
Route of transmission
These tumours involve local structures and metastasise to regional lymph nodes
at an early stage.
1
Investigations
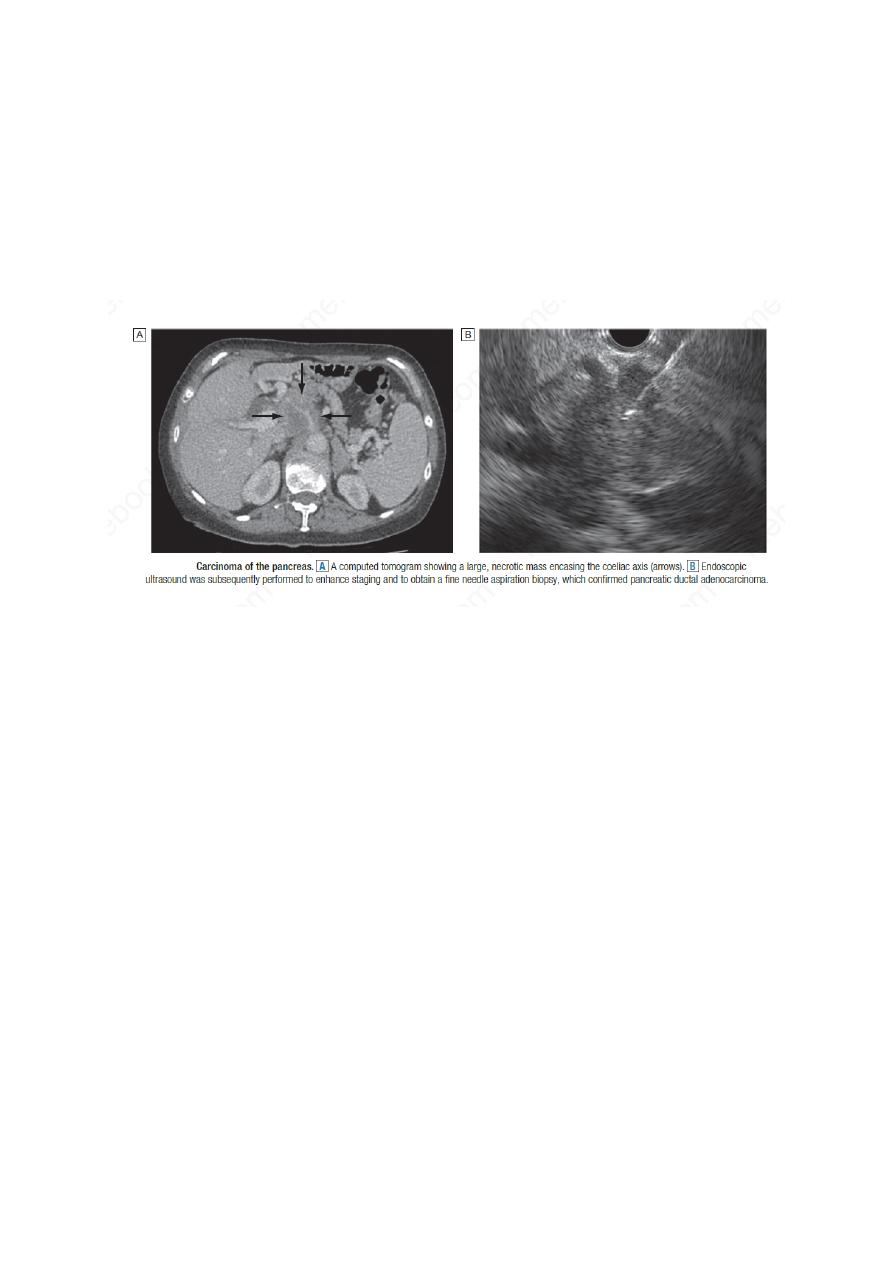
The diagnosis is usually made by ultrasound and contrast enhanced CT.
Fit patients with small, localised tumours should undergo staging to define
operability. EUS (endoscopic U/S) or laparoscopy with laparoscopic ultrasound
will define tumour size, involvement of blood vessels and metastatic spread.
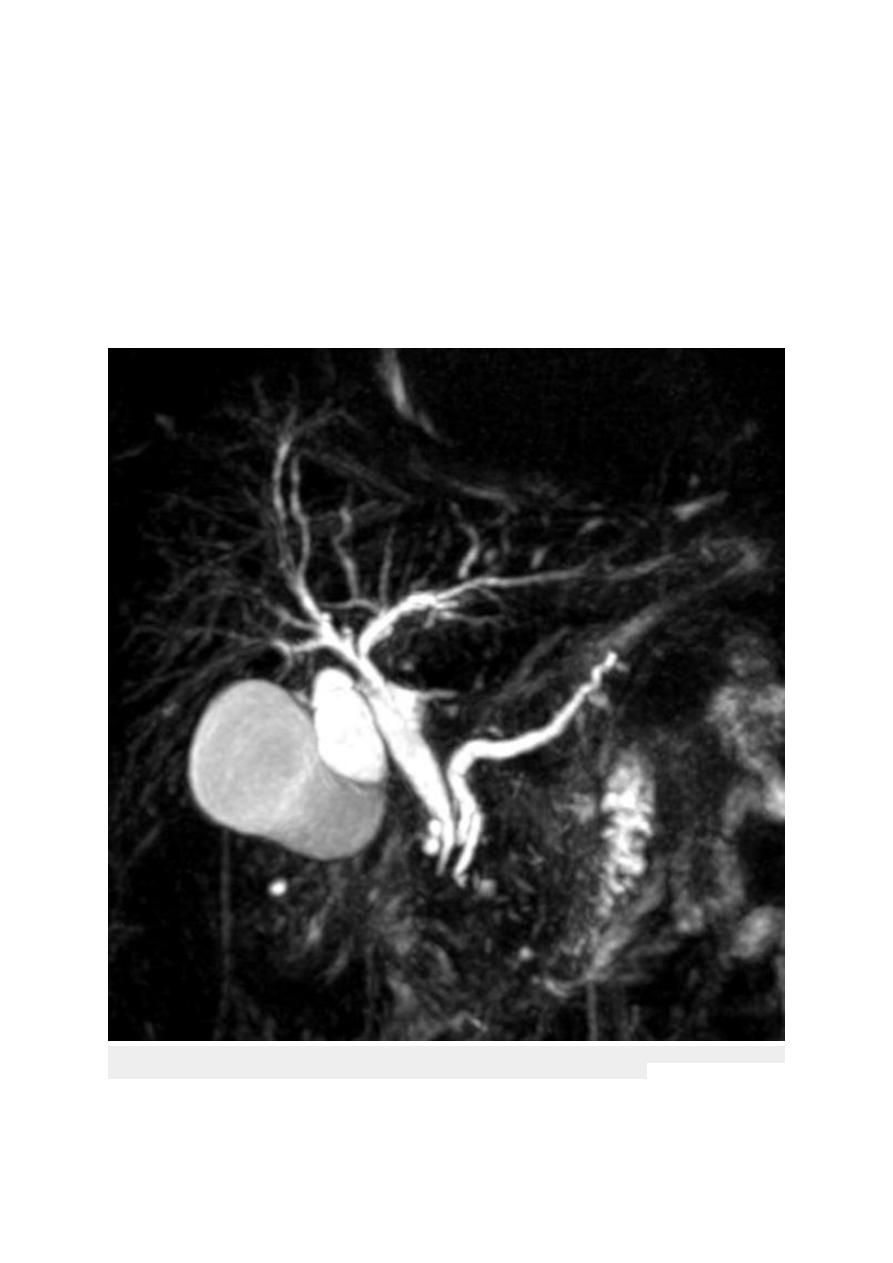
MRCP and ERCP are sensitive methods of diagnosing pancreatic cancer and are
valuable when the diagnosis is in doubt, although differentiation between cancer
and localised chronic pancreatitis can be difficult.
Management
Surgical resection is the only method of effecting cure, and 5-year survival in
patients undergoing a complete resection is around 12%. Clinical trials have
demonstrated improved survival (21–29%) with adjuvant chemotherapy using
gemcitabine.
Unfortunately, only 10–15% of tumours are resectable for cure, since most are
locally advanced at the time of diagnosis. For the great majority of patients,
treatment is palliative.
Palliative treatment
Pain relief can be achieved using analgesics but, in some patients, coeliac
plexus neurolysis may be required.
Jaundice can be relieved by choledochojejunostomy in fit patients, whereas
percutaneous or endoscopic stenting is preferable in the elderly and those with
very advanced disease.
Prognosis
Overall survival is only 3–5%, with a median survival of 6–10 months for those
with locally advanced disease and 3–5 months if metastases are present.
Ampullary or periampullary adenocarcinomas:
Are rare neoplasms that arise from the ampulla of Vater or adjacent duodenum.
They are often polypoid and may ulcerate; they frequently infiltrate the
duodenum but behave less aggressively than pancreatic adenocarcinoma.
2
presented with pain, anaemia, vomiting and weight loss. Jaundice may be
intermittent or persistent.
The diagnosis is made by duodenal endoscopy and biopsy of the tumour but
staging by CT/MRI and EUS is essential. Imaging may show a ‘double duct
sign’ with stricturing of both the common bile duct and pancreatic duct at the
ampulla and upstream dilatation of the ducts. EUS is the most sensitive method
of assessing and staging ampullary or periampullary tumours.
Curative surgical treatment can be undertaken by pancreaticoduodenectomy and
the 5-year survival may be as high as 50%. If resection is impossible, palliative
surgical bypass or stenting may be necessary.
Abrupt loss of bile signal at the distal portions of the common bile duct & pancreatic ducts with mild
dilatation of their proximal portions (giving rise for the characteristic double duct sign)
3

Carcinoma of the gallbladder
This is an uncommon tumour, occurring more often in females and usually in
those over the age of 70 years.
Risk factors
1- Gallstones are present in 70–80% of cases and are thought to be important in
the aetiology of the tumour.
2- Individuals with a calcified gallbladder (‘porcelain gallbladder) are at high
risk of malignant change. (Calcium may be secreted into the lumen of the
hydropic gallbladder, causing ‘limey’ bile, and if calcium salts are precipitated
in the gallbladder wall, the radiological appearance of ‘porcelain’ gallbladder
results)
3- Gallbladder polyps over 1 cm in size are associated with increased risk of
malignancy; preventative cholecystectomy should be considered in such
patients.
4- Chronic infection with Salmonella, especially in areas where typhoid is
endemic, is also a risk factor.
diagnosis:
It may manifest as repeated attacks of biliary pain and, later, persistent jaundice
and weight loss.
A gallbladder mass may be palpable in the right hypochondrium.
LFTs show cholestasis, and porcelain gallbladder may be found on X-ray. The
tumour can be diagnosed by ultrasonography and staged by CT.
Treatment
surgical excision
but local extension of the tumour beyond the wall of the gallbladder into the
liver, lymph nodes and surrounding tissues is invariable and palliative
management is usually all that can be offered.
Prognosis:
Survival is generally short, death typically occurring within 1 year in patients
presenting with symptoms.
4

Cholangiocarcinoma
Risk factors
The cause is unknown but can associated with:
1. gallstones,
2. primary and secondary sclerosing cholangitis
3. Caroli’s disease
4. choledochal cysts
5. chronic liver fluke infection
5
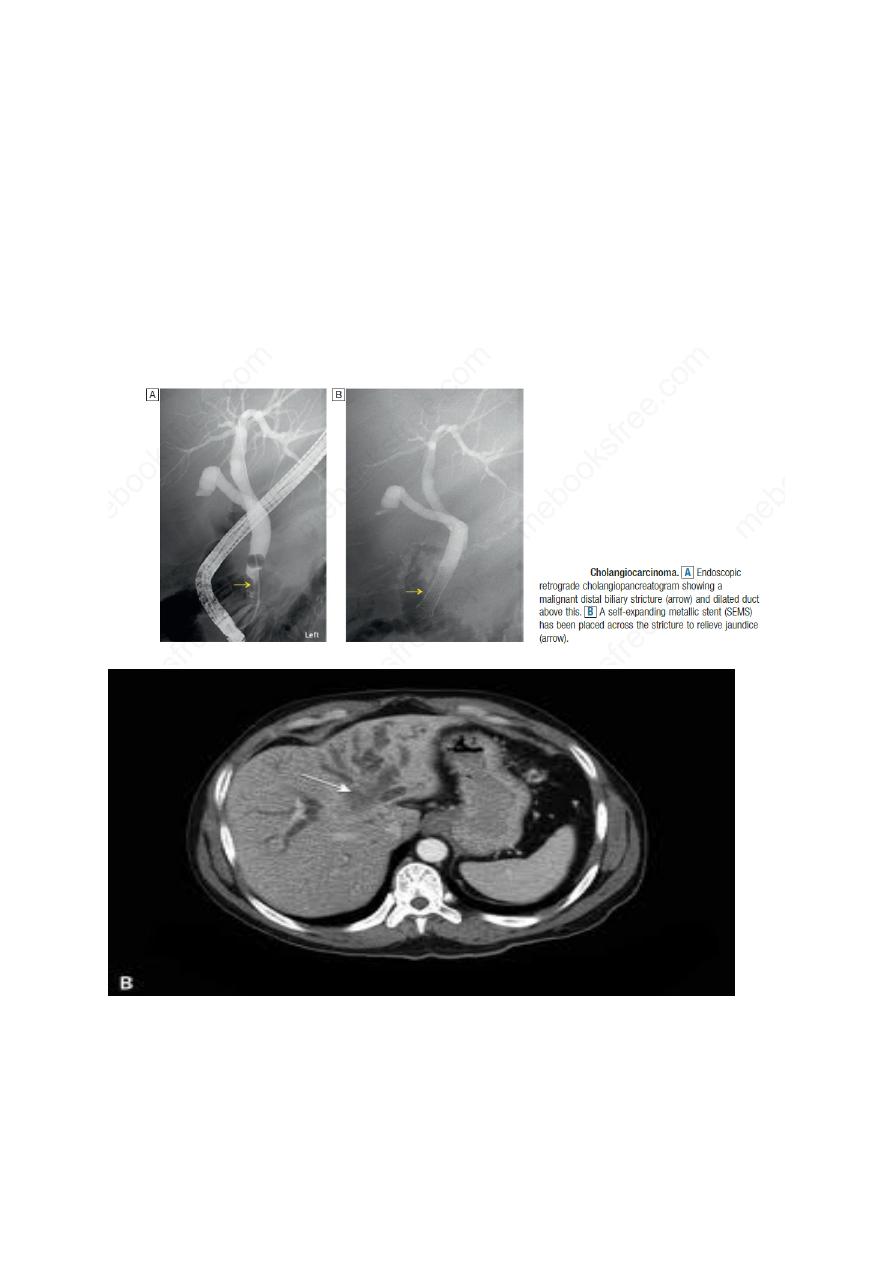
Tumours typically invade the lymphatics and adjacent vessels, with a
predilection for spread within perineural sheaths. The presentation is usually
with obstructive jaundice. About 50% of patients also have upper abdominal
pain and weight loss. The diagnosis is made using a combination of CT and
MRI, but can be difficult to confirm in patients with sclerosing cholangitis.
Serum levels of the tumour marker CA19-9 are elevated in up to 80% of cases,
although this may occur in biliary obstruction of any cause.
ERCP may result in positive biliary cytology.
Endoscopic ultrasound–fine needle aspiration (EUS-FNA) of bile duct masses is
sometimes possible.
6
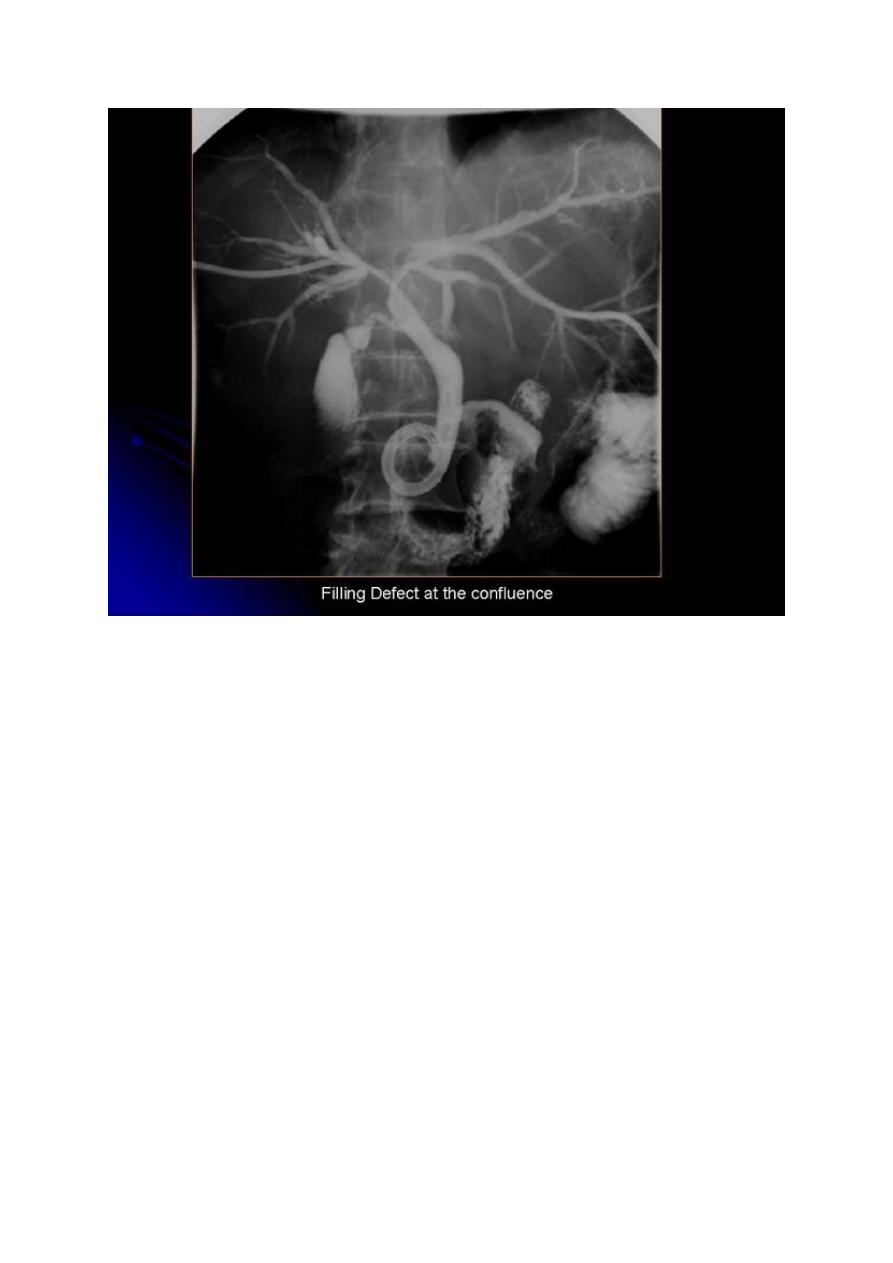
Klatskin tumor is a term that was traditionally given to a hilar
cholangiocarcinoma, occurring at the bifurcation of the common hepatic duct.
Treatment
Surgery involves excision of the extrahepatic biliary tree with or without a liver
resection and a Roux loop reconstruction. However, most patients (inoperable)
are treated by stent insertion across the malignant biliary stricture, using
endoscopic or percutaneous transhepatic techniques.
With best wishes
7
