1
Lec: 2
Dr. Mohammed Alhamdany
Diseases of the small intestine
Disorders causing malabsorption
Coeliac disease
Coeliac disease is an inflammatory disorder of the small bowel occurring in
genetically susceptible individuals, which results from intolerance to wheat
gluten and similar proteins found in rye, barley and, to a lesser extent, oats. It
can result in malabsorption and responds to a gluten-free diet.
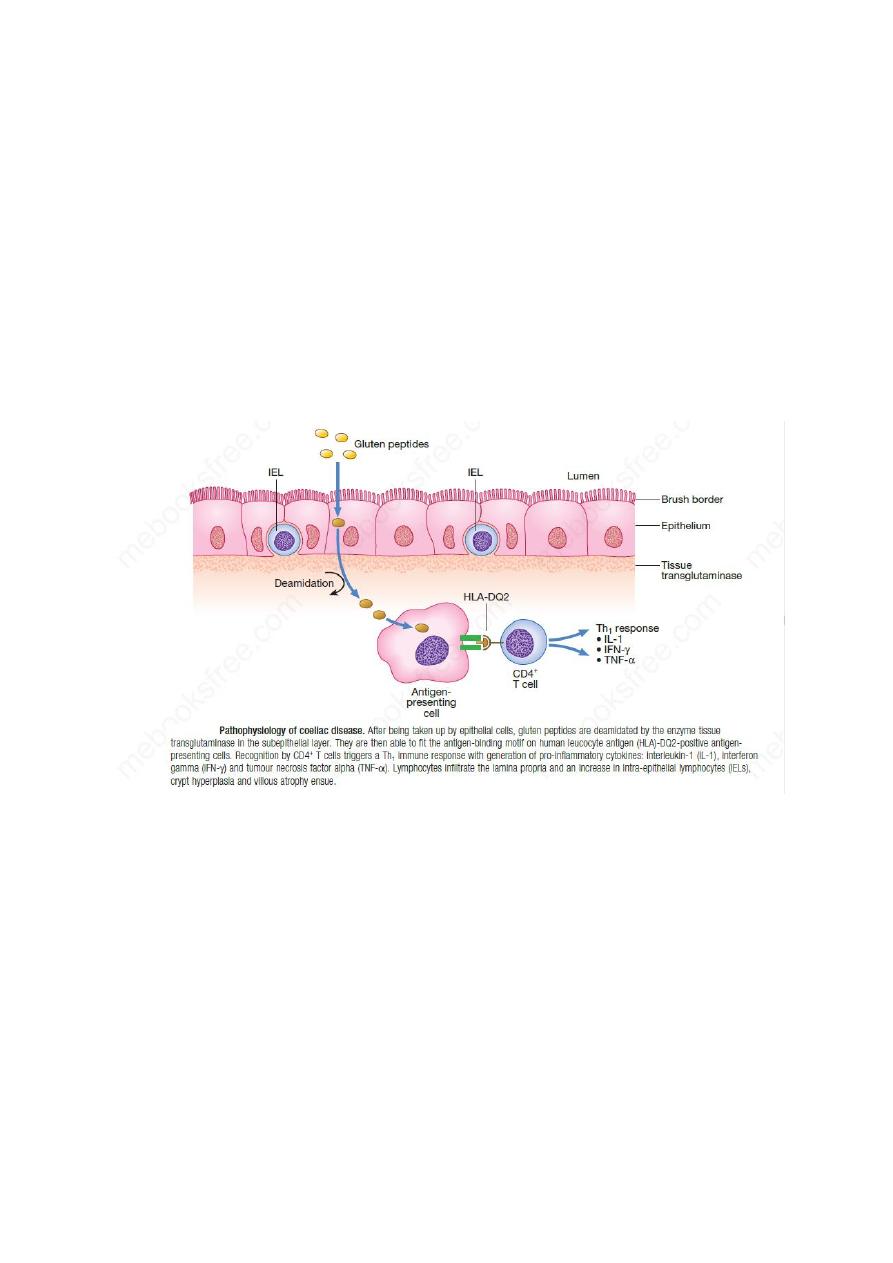
Pathophysiology
The precise mechanism of mucosal damage is unclear but immunological
responses to gluten play a key role. There is a strong genetic component. There
is a strong association with human leukocyte antigen (HLA)-DQ2/DQ8.
Dysbiosis of the intestinal microbiota has been identified.
Clinical features
Coeliac disease can present at any age. In infancy, it occurs after weaning on to
cereals and typically presents with diarrhoea, malabsorption and failure to
thrive. In older children, it may present with non-specific features, such as
delayed growth. In adults, the disease usually presents during the third or fourth
decade and females are affected twice as often as males. The presentation is
highly variable, depending on the severity and extent of small bowel
involvement. Some have florid malabsorption, while others develop non-
specific symptoms, such as tiredness, weight loss, folate deficiency or iron
deficiency anaemia. Other presentations include oral ulceration, dyspepsia and
bloating. Unrecognised coeliac disease is associated with mild under-nutrition
and osteoporosis.

2
Disease associations of coeliac disease
1. Type 1 diabetes mellitus
2. Thyroid disease
3. Primary biliary cirrhosis
4. Sjögren’s syndrome
5. Immunoglobulin A deficiency
6. Pernicious anaemia
7. Neurological complications
8. Dermatitis herpetiformis
9. Enteropathy-associated T-cell lymphoma
10. Small bowel carcinoma
11. Squamous carcinoma of oesophagus
12. Ulcerative jejunitis
13. Pancreatic insufficiency
14. Microscopic colitis
15. Splenic atrophy
Investigations
Duodenal biopsy
Endoscopic small bowel biopsy is the gold standard. Endoscopic appearances
should not preclude biopsy, as the mucosa usually looks normal. As the
histological changes can be patchy, an adequate number of biopsies – currently,
more than four biopsies from the second part of the duodenum plus one from
the duodenal bulb – should be retrieved. The histological features are Subtotal
villous atrophy in coeliac disease,there is blunting of villi , crypt hyperplasia
and inflammatory infiltration of the lamina propria
Important causes of subtotal villous atrophy
1. Coeliac disease
2. Tropical sprue
3. Dermatitis herpetiformis
4. Lymphoma
5. HIV-related enteropathy
6. Giardiasis
7. Hypogammaglobulinaemia
8. Radiation
9. Whipple’s disease
10. Zollinger–Ellison syndrome
Antibodies
Good screen test but are not a diagnostic substitute for small bowel biopsy at
present. Tissue transglutaminase (tTG) is now recognised as the autoantigen for

3
anti-endomysial antibodies. If the antibody screen is positive, adult patients
should remain on a gluten-containing diet until duodenal biopsies are taken.
High-titre serology in children can be diagnostic without the need for
endoscopy and biopsy. Antibody titres usually become negative with successful
treatment.
1- Anti-endomysial antibodies of the IgA class are detectable by
immunofluorescence in most untreated cases. They are sensitive (85–95%) and
specific (approximately 99%) for the diagnosis, except in very young infants.
IgG antibodies, however, must be analysed in patients with coexisting IgA
deficiency.
2- The tTG assay has become the serological test of choice in many countries,
as it is easier to perform, is semi-quantitative, has more than 95% sensitivity
and specificity, and is more accurate in patients with IgA deficiency.
Haematology and biochemistry
A full blood count may show microcytic or macrocytic anaemia from iron or
folate deficiency and features of hyposplenism (target cells, spherocytes and
Howell–Jolly bodies). Biochemical tests may reveal reduced concentrations of
calcium, magnesium, total protein, albumin or vitamin D.
Other investigations Measurement of bone density should be considered to look
for evidence of osteoporosis, especially in older patients and post-menopausal
women.
Management
The aims are to
1- Correct existing deficiencies of micronutrients, such as iron, folate, calcium
and/or vitamin D
2- To achieve mucosal healing through a life-long gluten-free diet. This requires
the exclusion of wheat, rye, barley and initially oats, although oats may be re-
introduced safely in most patients after 6–12 months.
Follow up through
1- Assessment of symptoms, weight and nutritional status
2- Measurement of tTG or anti-endomysial antibodies
3- No need for re-biopsy
Indication of re-biopsy only in non-responders symptomatically or
biochemically (Ab sustain +ve)
Not responders may be due:
1- Poor compliance
2- Other associated diseases such as pancreatic insufficiency or microscopic
colitis
3- complications of disease like ulcerative jejunitis or enteropathy-associated T-
cell lymphoma.
4- Small numbers of non-responders coeliac disease whom may need
glucocorticoids or immunosuppressive drugs.

4
Complications
1- Enteropathy associated T-cell lymphoma.
2- Small bowel carcinoma.
3- squamous carcinoma of the oesophagus
4- Ulcerative jejuno-ileitis.
5- Osteoporosis and osteomalacia
Dermatitis herpetiformis
Notes
1- This is crops of intensely itchy blisters over the elbows, knees, back and
buttocks
2- Almost all patients have partial villous atrophy on duodenal biopsy
3- granular or linear IgA deposition at the dermo-epidermal junction on skin
biopsy.
4- 10% of coeliac patients have evidence of dermatitis herpetiformis,
5- treatment with gluten-free diet + dapsone
Tropical sprue
Tropical sprue is defined as chronic, progressive malabsorption in a patient in or
from the tropics
Clinical features
There is diarrhoea, abdominal distension, anorexia, fatigue and weight loss.
When the disorder becomes chronic, the features of megaloblastic anaemia
(vitamin B12 and folic acid malabsorption) and other deficiencies, including
ankle oedema, glossitis and stomatitis, are common. Remissions and relapses
may occur.
Management
Tetracycline (250 mg 4 times daily for 28 days) is the treatment of choice and
brings about long-term remission or cure. In most patients, pharmacological
doses of folic acid (5 mg daily) improve symptoms and jejunal morphology.

5
Small bowel bacterial overgrowth (‘blind loop syndrome’)
The normal duodenum and jejunum contain fewer than 10
4
/mL organisms,
which are usually derived from saliva. The count of coliform organisms never
exceeds 10
3
/mL. In bacterial overgrowth, there may be 10
8
–1010/mL
organisms, most of which are normally found only in the colon.
Causes of small bowel bacterial overgrowth
1- Hypo- or achlorhydria like Pernicious anaemia, partial gastrectomy, and
long-term proton pump inhibitor therapy.
2- Impaired intestinal motility such as systemic sclerosis, diabetic autonomic
neuropathy.
3- Structural abnormalities such as gastric surgery (blind loop after Billroth II
operation), jejunal diverticulosis, enterocolic fistulae or strictures (Crohn’s
disease the most commonly cause), extensive small bowel resection
4- Impaired immune function like Hypogammaglobulinaemia
Management
The underlying cause of small bowel bacterial overgrowth should be addressed,
where possible. A course of broad-spectrum antibiotic for 2 weeks is the first-
line treatment, Examples include tetracycline (250 mg 4 times daily),
metronidazole (400 mg 3 times daily), amoxicillin (250 mg 3 times daily) or
ciprofloxacin (250 mg twice daily).
If not respond extend treatment for prolong course for 4 weeks, and continuous
rotating courses of antibiotics are necessary.
Intramuscular vitamin B12 supplementation may be needed in chronic cases, as
the bacteria utilize vitamin B12.
Whipple’s disease
note
1- This rare condition is characterised by infiltration of small intestinal mucosa
by ‘foamy’ macrophages, which stain positive with periodic acid–Schiff (PAS)
reagent.
2- Whipple’s disease is caused by infection with the Gram-positive bacillus
Tropheryma whipplei, which becomes resident within macrophages in the
bowel mucosa.
3- Middle-aged Caucasian men are most frequently affected and presentation
depends on the pattern of organ involvement.
4- Low-grade fever is common and most patients have joint symptoms to some
degree, often as the first manifestation.
5- CNS involvement is the most serious consequence.
6- Organ involve include: Gastrointestinal, Musculoskeletal, Cardiac,
Neurological, Pulmonary, Haematological, systemic (Fever)
7- Diagnosis is made by the characteristic features on small bowel biopsy, with
characterisation of the bacillus by polymerase chain reaction (PCR).
6
8- Whipple’s disease is often fatal if untreated but responds well, at least
initially, to intravenous ceftriaxone (2 g daily for 2 weeks), followed by oral co-
trimoxazole for at least 1 year.
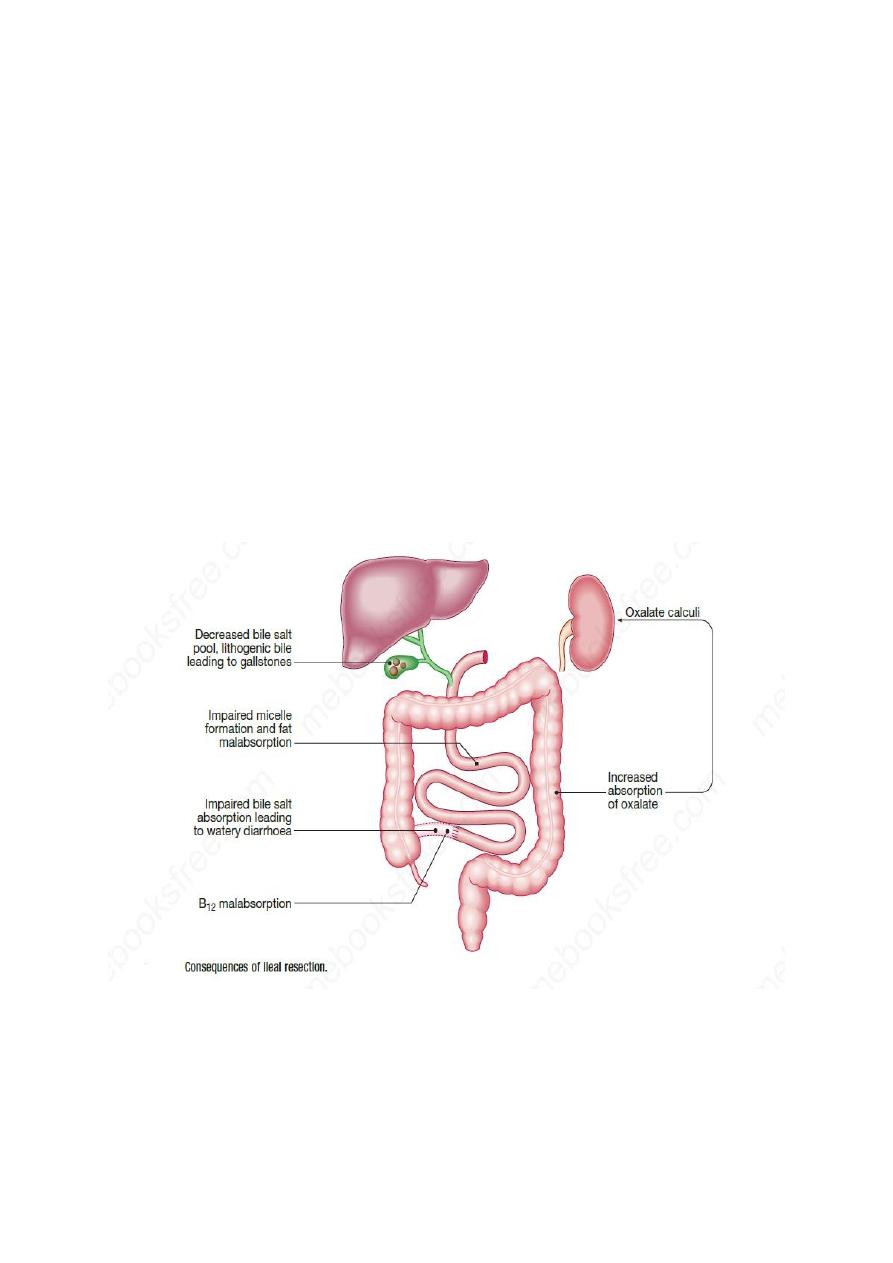
Bile acid diarrhea
Notes
1-Causes include: idiopathically, complication of small bowel resection, post
cholecystectomy, in association with other conditions such as microscopic
colitis, chronic pancreatitis, coeliac disease, small intestinal bacterial
overgrowth and diabetes mellitus.
2- Mechanism of diarrhea: unabsorbed bile salts pass into the colon, stimulating
water and electrolyte secretion and causing diarrhoea.
3- If hepatic synthesis of new bile acids cannot keep pace with faecal losses, fat
malabsorption occurs. Another consequence is the formation of lithogenic bile,
leading to gallstones.
Q: Why such patient develop renal calculi?
4- Treatment: Diarrhoea usually responds well to bile acid sequestrants, such as
colestyramine or colesevelam, which bind bile salts in the intestinal lumen.
Aluminium hydroxide can be used as an alternative.
Chronic complications of intestinal irradiation
•
Proctocolitis
•
Bleeding from telangiectasia
•
Small bowel strictures
•
Fistulae: rectovaginal, colovesical, enterocolic
•
Adhesions

7
•
Malabsorption: bacterial overgrowth, bile acid diarrhea
With best wishes
