كلية الطب
جامعة بابل
Lec3
Hepatology
Chronic HBV and HCV
Dr.Hassan aljumaily

•
Chronic hepatitis B virus infection:
Hepatitis B is one of the most common causes of chronic liver
disease and hepatocellular carcinoma worldwide. Hepatitis B may
cause an acute viral hepatitis however, acute infection is often
asymptomatic, particularly when acquired at birth. Many
individuals with chronic hepatitis B are also asymptomatic .
The risk of progression to chronic liver disease depends on the
source and timing of infection .
Full recovery occurs in 90–95% of adults following acute
HBV infection. The remaining 5–10% develop a chronic
hepatitis B infection that usually continues for life, although
later recovery occasionally occurs.
Infection passing from mother to child at birth leads to
chronic infection in the child in 90% of cases and recovery is
rare. Chronic infection is also common in immunodeficient
individuals, such as those with Down’s syndrome or human
immunodeficiency virus (HIV) infection.
Combined HBV and
HDV infection causes more aggressive disease

Source of hepatitis B infection and risk of chronic
infection
Horizontal transmission (10%)
• Injection drug use
• Infected unscreened blood products
• Tattoos/acupuncture needles
• Sexual (homosexual and heterosexual)
• Close living quarters/playground play as a toddler
(may
contribute to high rate of horizontal transmission
in Africa)
Vertical transmission (90%)
• HBsAg-positive mother

Clinical presentation:
■Incubation period of acute infection is 1 to 4 months
■Symptomatic acute hepatitis (e.g., abdominal pain, low-grade
fever, nausea, jaundice) occurs in 30% of adults, but in only 10%
of children younger than 4 years of age
■Clinical symptoms usually normalize after 1 to 3 months
■Many are chronic inactive carriers with normal liver
chemistries, presence of anti-HBe, and minimal serum HBV DNA.
Inactive carriers remain at risk for HCC. This phase of the
disease is also known as immune tolerance.
■Reactivation of HBV replication (presence of anti-HBe, high
serum HBV DNA, intermittently elevated ALT) can occur in the
setting of immunosuppression (i.e., chemotherapy)
■Extrahepatic manifestations (in 10% to 20% of chronic HBV)
include polyarteritis nodosa, membranous or
membranoproliferative glomerulonephritis, and mixed cryoglobu

INVESTIGATION
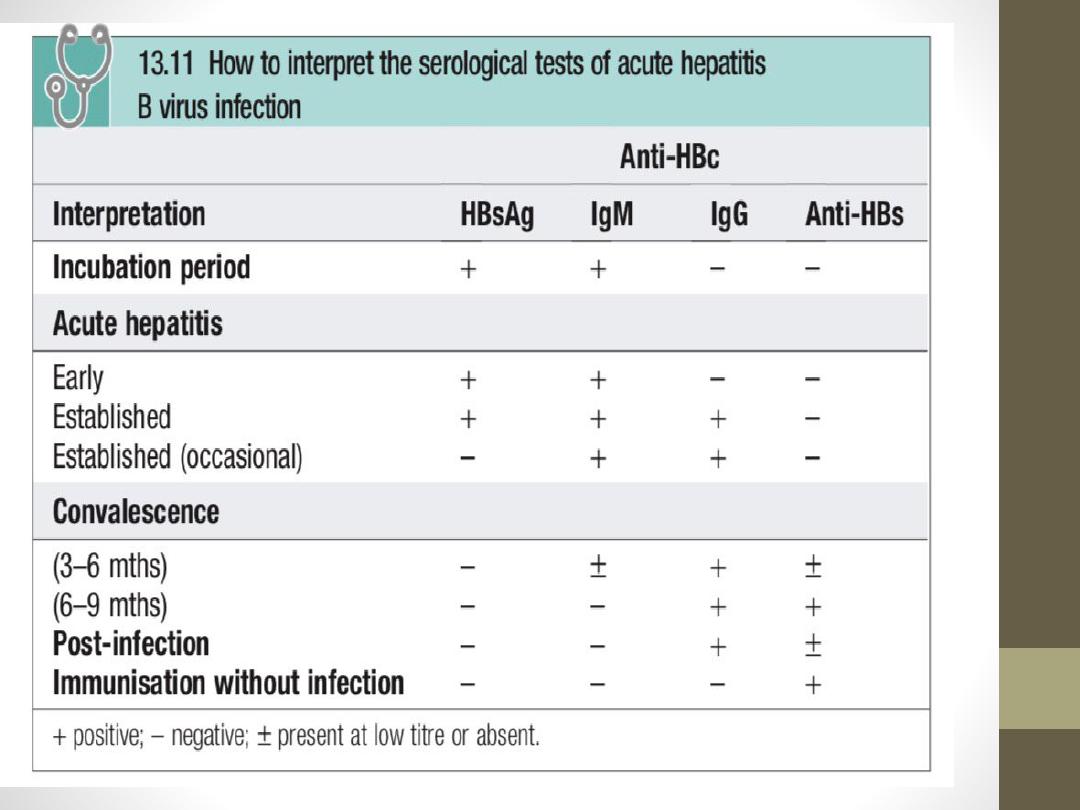
Serology: In acute infection HBsAg is a reliable marker of HBV
infection . Antibody to HBsAg (anti-HBs) appears after about
3–6 mths and persists for many years or even permanently.
Anti-HBs implies either a previous infection, in which case anti-
HBc (see below) is usually also present; or previous
vaccination, when anti-HBc is not present.
The hepatitis B core antigen (HBcAg) is not found in the blood
but antibody to it (anti-HBc) appears early in the illness. Anti-
HBc is initially of IgM type, with IgG antibody appearing later.
The hepatitis B e antigen (HBeAg) is an indicator of active viral
replication. It appears only transiently at the outset of the
illness and is followed by the production of antibody (anti-
HBe). Chronic HBV infection (see below) is marked by the
persistence of HBsAg and anti-HBc (IgG) in the blood. Usually,
HBeAg or anti-HBe is also present. Interpretation of serological
tests is shown in Box

Viral load:
HBV-DNA can be measured by PCR in the blood. Viral loads are
usually >105 copies/mL in the presence of active viral replication,
as indicated by the presence of e antigen. In contrast, in those
with low viral replication, HBsAg- and anti-HBe-positive, viral
loads are usually <105 copies/mL. High viral loads are also found
in e antigen-negative chronic hepatitis, which occurs in the Far
East and is due to a mutation.

Management
Acute hepatitis B:
Treatment is supportive, with monitoring for
acute liver failure, which occurs in < 1% of
cases.
Chronic hepatitis B:
1- This develops in 5–10% of acute cases and
is lifelong. No drug is consistently able to
render patients HBsAg-negative.

2- Lamivudine and tenofovir are both effective, but viral
mutations causing resistance commonly develop. Tenofovir
also has anti-HIV efficacy, so monotherapy should be avoided
in HIV co-infected patients to prevent HIV antiviral drug
resistance. Interferon alfa is most effective in patients with low
viral load and high transami- nases, in whom it acts by
augmenting a native immune response.
3-Interferon is contraindicated in the presence of cirrhosis, as it
may precipitate liver failure. Longer-acting pegylated
interferons, which can be given once weekly, have been
evaluated in both HBeAg- positive and HBeAg-negative chronic
hepatitis.
The use of post-liver transplant prophylaxis with lamivudine
and hepatitis B immunoglobulins has reduced the re-infection
rate to 10% and increased 5-yr survival to 80%, making
transplantation an acceptable treatment option.
•
PREVENTION
1.
Individuals are most infectious when markers of continuing viral
replication, such as HBeAg, and high levels of HBV-DNA are present in
the blood. The virus is about ten times more infectious than hepatitis C,
which in turn is about ten times more infectious than HIV.
2.
A recombinant hepatitis B vaccine containing HBsAg is available
(Engerix) and is capable of producing active immunisation in 95% of
normal individuals. The vaccine should be offered to those at special risk
of infection who are not already immune, as evidenced by anti-HBs in the
blood .
The vaccine is
in
effective in those already infected by HBV.
3.
Infection can also be prevented or minimised by the intramuscular
injection of hyperimmune serum globulin prepared from blood containing
anti-HBs.
This should be given within 24 hours, or
•
at most a week of exposure to infected blood in circumstances likely to
cause infection (e.g. needle stick injury, contamination of cuts or mucous
membranes).
Vaccine can be given together with hyperimmune
globulin(active–passive immunization) .
Neonates born to hepatitis B-infected mothers should be immunised at birth
and given immunoglobulin. Hepatitis B serology should then be checked at
12 months of age

At-risk groups meriting hepatitis B vaccination
•
Parenteral drug users
•
Men who have sex with men
•
Close contacts of infected individuals
•
Newborn of infected mothers
•
Regular sexual partners
•
Patients on chronic haemodialysis
•
Patients with chronic liver disease
•
Medical, nursing and laboratory personnel

Hepatitis C
•
This is caused by an RNA flavivirus.
Acute symptomatic
infection with hepatitis C is rare
. Most individuals are
unaware of when they became infected and are only
identified when they develop chronic liver disease.
80% of
individuals exposed to the virus become chronically infected
and late spontaneous viral clearance is rare
.(unlike HBV).
•
Hepatitis C infection is usually identified in asymptomatic
individuals screened because they have risk factors for
infection or have incidentally been found to have abnormal
liver blood tests. Although most individuals remain
asymptomatic until progression to cirrhosis occurs, fatigue
can complicate chronic infection and is unrelated to the
degree of liver damage.
Risk factors
:
•
Intravenous drug misuse (95% ).
•
Unscreened blood products
•
Vertical transmission (3% risk).
•
Needlestick injury (3% risk).
•
Iatrogenic parenteral transmission (i.e. contaminated
vaccination needles).
•
Sharing toothbrushes

PRESENATION
•
Symptoms often first develop as clinical findings of extra
hepatic manifestations of HCV and most commonly
involve the joints, muscle, and skin. The most commonly
occurring extra hepatic manifestations :
•
Arthralgias ,Paresthesia , Myalgia , sensory neuropathy.
•
Sicca syndrome necrotizing vasculitis,
Cryoglobulinemia.
•
Lymphoma , Idiopathic thrombocytopenic purpura.
•
porphyria cutanea tarda ,Pruritus, Lichen planus.
•
Membranoproliferative glomerulonephritis.
•
.
Risk factors for manifestations of extra hepatic chronic
hepatitis C infection include advanced age, female sex,
and liver fibrosis
Investigations
1-
Serology and virology
•
The HCV protein contains several antigens that give rise to
antibodies in an infected person and these are used in diagnosis.
It may take 6–12 weeks for antibodies to appear in the blood
following acute infection. In these cases, hepatitis C RNA can be
identified in the blood as early as 2–4 weeks after infection.
•
Active infection is confirmed by the presence of serum
hepatitis C RNA in anyone who is antibody-positive. Anti-HCV
antibodies persist in serum even after viral clearance, whether
spontaneous or post-treatment.
2-
Molecular analysis
•
There are
6
common viral genotypes, the distribution of which
varies worldwide. Genotype has
no
effect on progression of
liver disease , but does affect response to treatment. Genotype 1
less easy to eradicate than genotypes 2 and 3 with traditional
pegylated interferon alfa/ ribavirin-based treatments.
3- Liver function tests
•
LFTs may be normal or show fluctuating serum
transaminases between 50 and 200 U/L. Jaundice is rare and
only usually appears in end-stage cirrhosis.
4-
Liver histology
•
Serum transaminase levels in hepatitis C are a poor
predictor of the degree of liver fibrosis and so a liver biopsy
is often required to stage the degree of liver damage
. The
degree of inflammation and fibrosis can be scored
histologically. The most common scoring system used in
hepatitis C is the Metavir system, which scores fibrosis
from 1 to 4, the latter equating to cirrhosis.

Management
Antiviral therapy for chronic hepatitis C should be determined on a
case-by-case basis. However, treatment is widely recommended for
patients with elevated serum alanine aminotransferase (ALT) levels
who meet the following criteria :
•
Age greater than 18 years.
•
Positive HCV antibody and serum HCV RNA test results.
•
Compensated liver disease (eg, no hepatic encephalopathy or
ascites).
•
Acceptable hematologic and biochemical indices (hemoglobin at
least 13 g/dL for men and 12 g/dL for women; neutrophil count
>1500/mm 3, serum creatinine < 1.5 mg/dL).
•
Willingness to be treated and to adhere to treatment requirements.
•
No contraindications for treatment.
Extra hepatic manifestations

•
N.B A further criterion is liver biopsy findings consistent
with a diagnosis of chronic hepatitis. However, a
pretreatment liver biopsy is not mandatory. It may be
helpful in certain situations, such as in patients with normal
transaminase levels, particularly those with a history of
alcohol dependence, in whom little correlation may exist
between liver enzyme levels and histologic findings.
•
Progression from chronic hepatitis to cirrhosis occurs over
20–40 years. Risk factors for progression include:
1-male gender.
2-immunosuppression (such as co-infection with HIV).
3- prothrombotic states and heavy alcohol misuse.

The aim of treatment is to eradicate infection. Until
recently, the treatment of choice was dual therapy with
pegylated interferon- alfa given weekly SC, together
with oral ribavirin, a synthetic nucle- otide analogue.
The length of treatment and efficacy depend on viral
genotype. The main side-effect of ribavirin is
haemolytic anaemia. Side-effects of interferon are
significant and include flu-like symp- toms, irritability
and depression. Recently, triple therapy with the
addition of protease inhibitors (e.g. telaprevir) has
increased the rate of sustained virological response
(defined as loss of virus from serum 6 mths after
completing therapy). Liver transplantation should be
considered when complications of cirrhosis occur.
Unfor- tunately, hepatitis C almost always recurs in
the transplanted liver.

