
37 year old woman –ve PMHx
4 days abdominal pain fever and jaundice.
PE: BP120/70, HR 80 per min, jaundice, no SOB
painful epigastric palpation
no signs of CLD
no signs of neurological distress
no encephalopathy.

bilirubin 7.58 mg/dl,
direct bilirubin 5.97 mg/dl
(ALT) AST↑,
, PT 24
RBS114 mg /dl
US of the liver was suggestive of hepatitis. The patient
was admitted for clinical observation because of the
high risk of liver failure and the need to study possible
liver disease. Fluid resuscitation was started, and
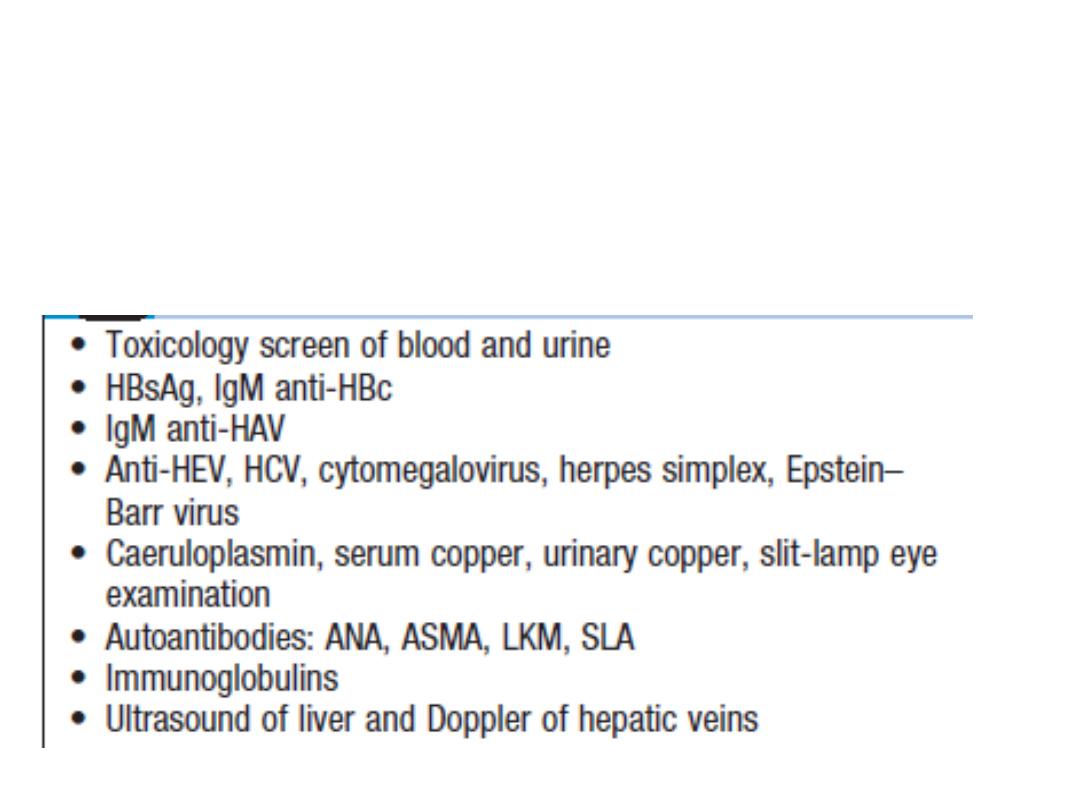
studies of liver disease began with a viral profile (HBsAg,
HVC, Total HVA, IgM Hep E, IgG, M Varicella zoster), an
immunological profile (ANA- ASMA), and levels of
ceruloplasmin and copper
.

NO Hxhistory of alcoholism and no Hx ingestion of
toxic substances,
. During the
first three days
in the hospital, the
patient remained hemodynamically stable without
signs of hepatic encephalopathy, but with worsening
of liver function. Tests for
HBsAg
were frankly
positive.

. Treatment began with 0.5 mg doses of entecavir daily
On the
fourth day
the patient suffered overall deterioration to
grade II hepatic encephalopathy.
Management
metronidazole, lactulose (to counter
encephalopathy) and N-acetylcysteine to manage liver disease
was begun. Arterial blood gases :metabolic acidosis due to liver
failure, treated medically with bicarbonate of soda. The patient
was moved to the intensive care unit for progression to hepatic
encephalopathy grade III and hemodynamic deterioration
requiring vasopressor support. She did not respond favorably

5th day
she developed grade IV hepatic
encephalopathy. Orotracheal intubation became
necessary to protect respiration.
A CT scan :normal.
The fundi of her eyes were without papilledema, but
she was given a bolus of mannitol because of the
possibility of intracranial hypertension. There was no
clinical improvement. She developed supraventricular
tachycardia and hemodynamic collapse requiring
electrical and pharmacological cardioversion

.
She had also developed upper gastrointestinal
bleeding for which infusion of omeprazole was
initiated. She was transfused with 15 cc/kg of
plasma plus vitamin K. The patient progressed to
cardiac arrest. She was unresponsive to advanced
maneuvers and died 5 days after admission to the
institution and nine days after onset of symptoms.
The cause of death was determined to be
fulminant liver failure secondary to hepatitis B

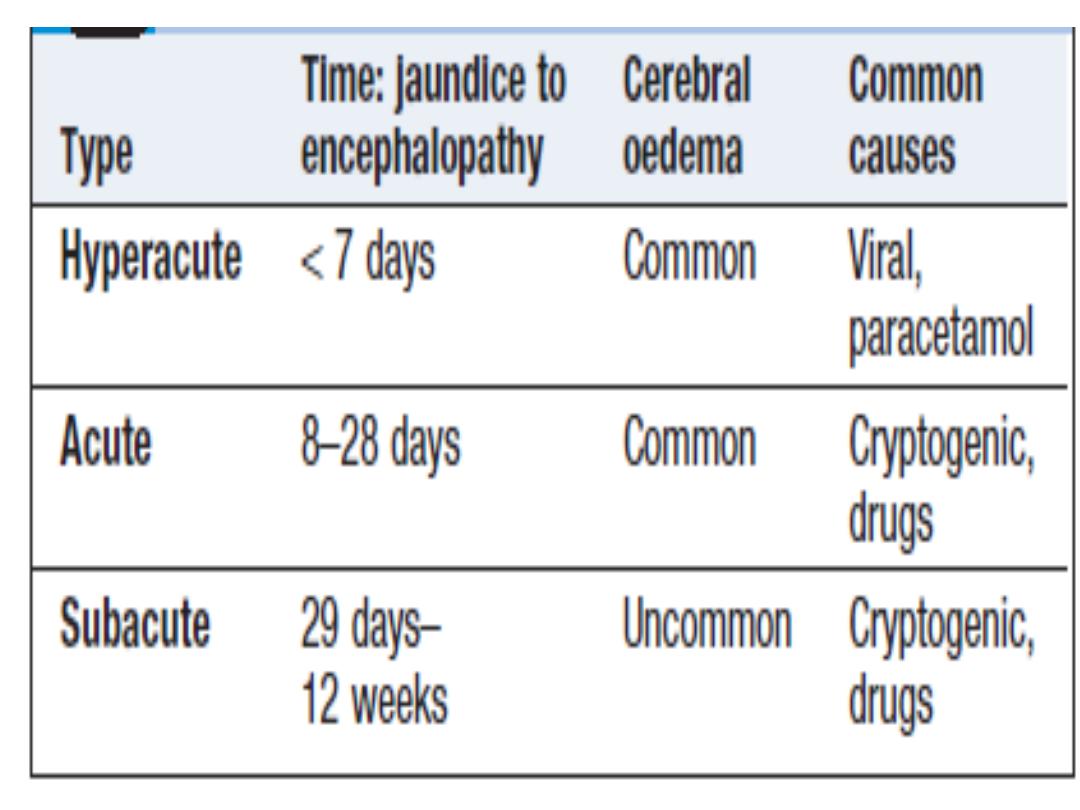
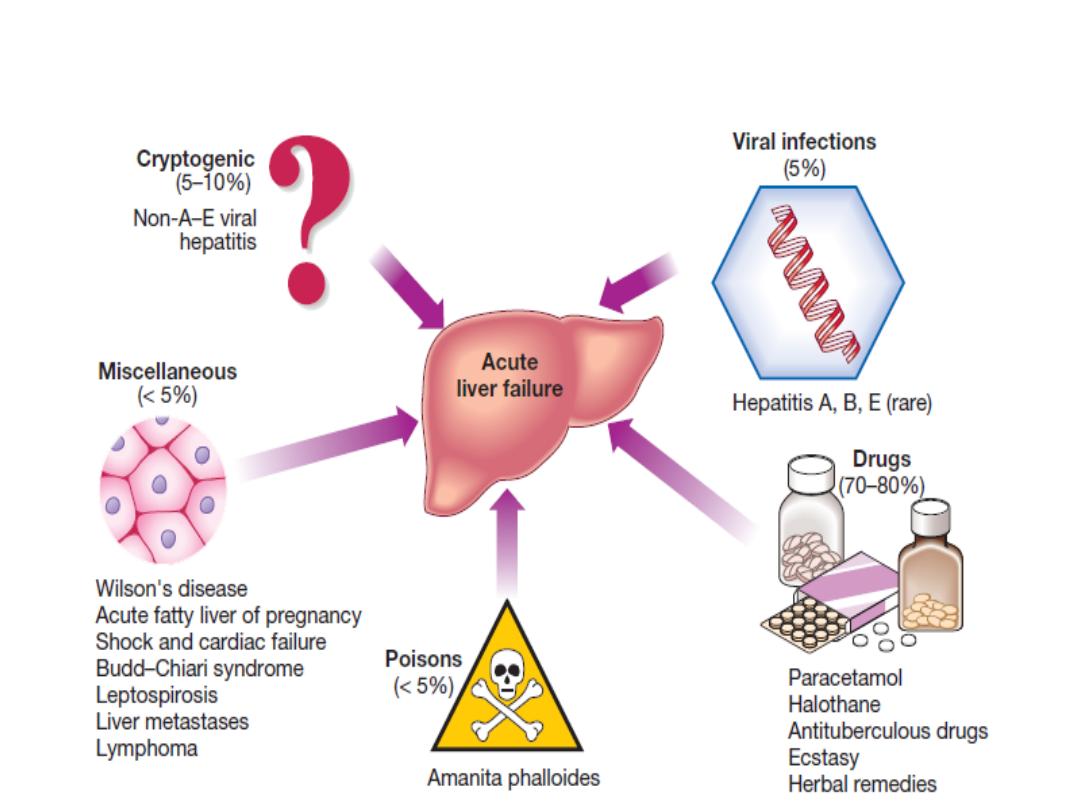
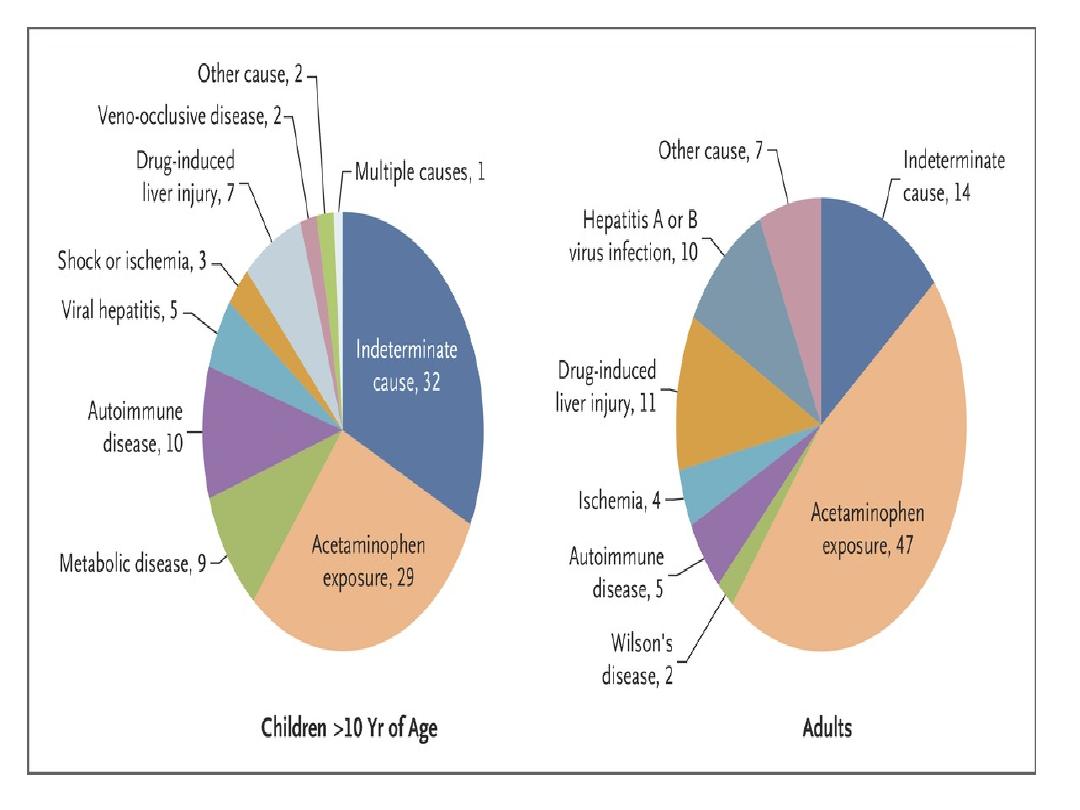
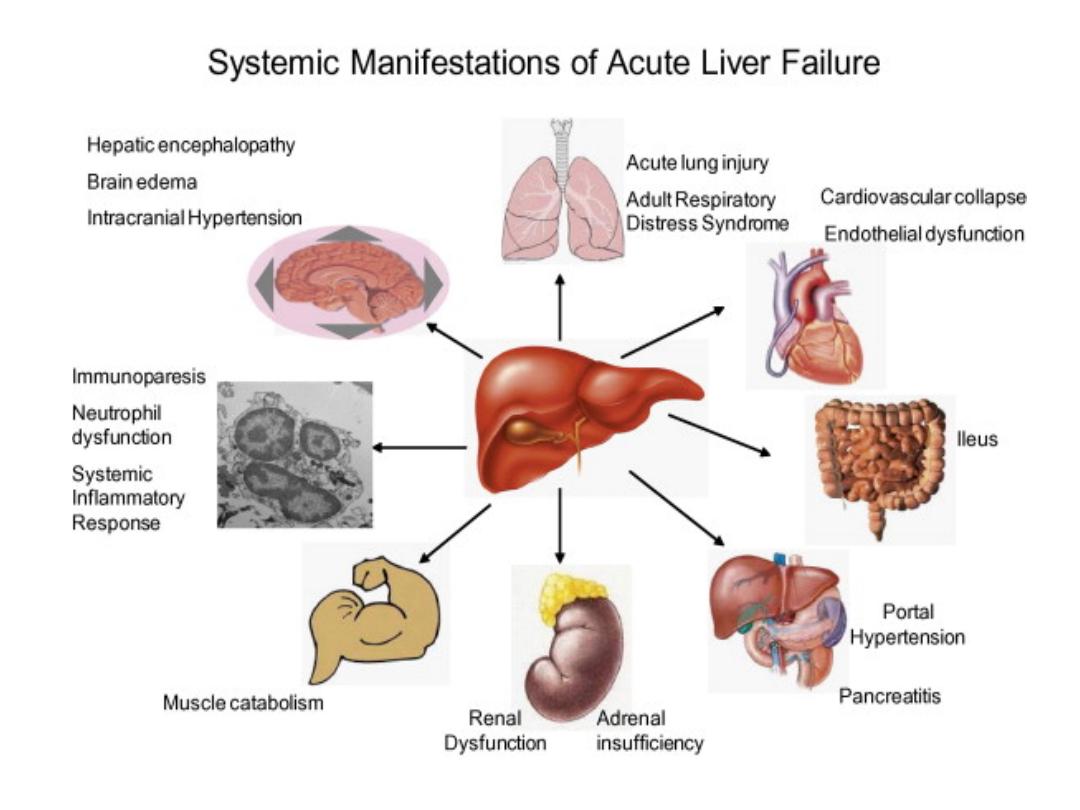
Acute liver failure:
progressive deterioration in liver
function and mental changes
progressing from confusion to
coma in absence of evidence of
preexisting liver disease.
Pathophysiology
. Clinical assessment
1-Cerebral disturbance
(hepatic encephalopathy and/or cerebral oedema) is the
cardinal manifestation of acute
liver failure. Cerebral oedema may occur due to increased intracranial pressure
-unequal or abnormally reacting pupils, fixed pupils
- hypertensive episodes bradycardia, hyperventilation, profuse sweating, local or
general myoclonus, focal fits or decerebrate posturing.
-Papilloedema occurs rarely and is a late sign.
2-
nausea and vomiting. Right hypochondrial discomfort
. The patient may be
jaundiced
.
- death may occur in fulminant cases of acute liver failure before jaundice develops.
-
Fetor hepaticus
can be present.
-The
liver
is usually of normal size but later becomes smaller.
- Hepatomegaly is unusual and, in the presence of a sudden onset of ascites, suggests
venous outflow obstruction as the cause (Budd–Chiari syndrome.
Splenomegaly is
uncommon
and never prominent.
-
Ascites and oedema
are late due to fluid therapy.
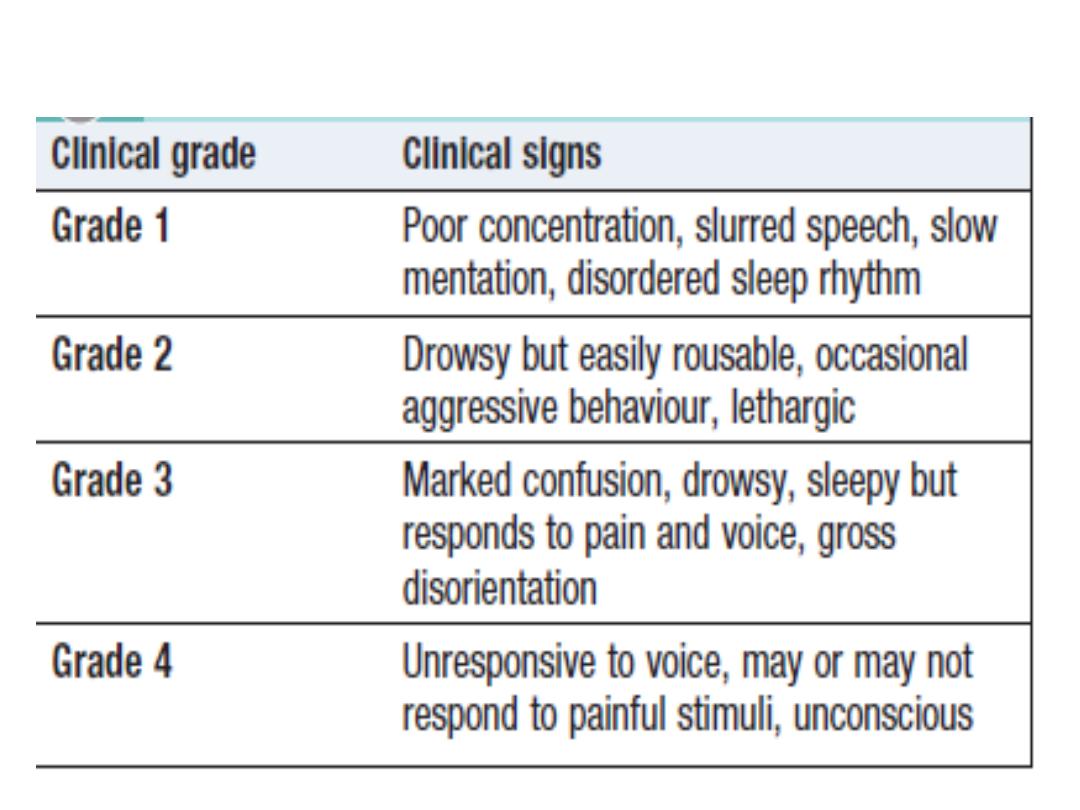
WEST HAVEN CLASSIFICATION
invex:
PT, bilirubin, Plasma aminotransferase.
Plasma albumin remains normal unless the course is
prolonged. Percutaneous liver biopsy is contraindicated
because of the severe coagulopathy,.

Management
1-high-dependency or intensive care unit
2-Conservative treatment ..GW, mannitol,bowel sterlization
by metronidazole and neomycin.
3- N-acetylcysteine therapy may improve outcome,
particularly in patients with acute liver failure
due to paracetamol poisoning.
4-earlytransfer to a specialized transplant unit . Survival
following liver transplantation for acute liver failure
is improving, and 1-year survival rates of about 60%
can be expected.
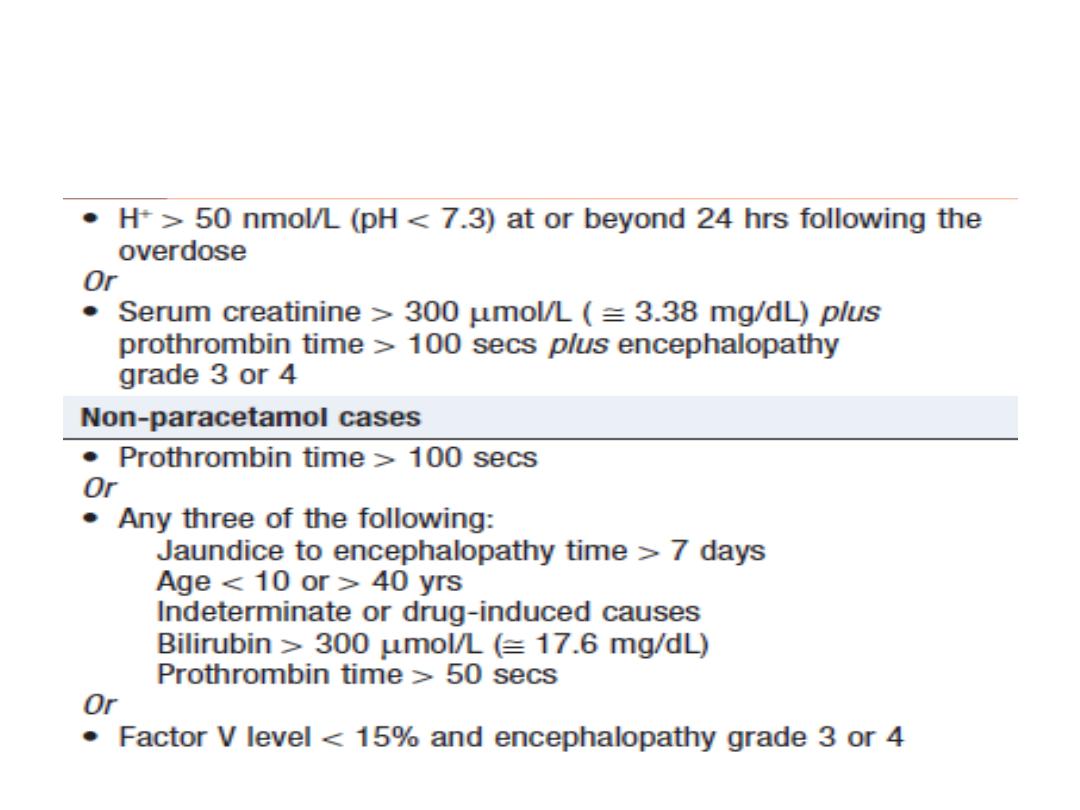
Adverse prognostic criteria in
acute liver failure….
Indication for transplant in paracetamol poisoning

Complications of acute liver failure
Encephalopathy and cerebral oedema
Hypoglycaemia
Metabolic acidosis
Infection (bacterial, fungal)
Renal failure
Multi-organ failure (hypotension and
respiratory failure)
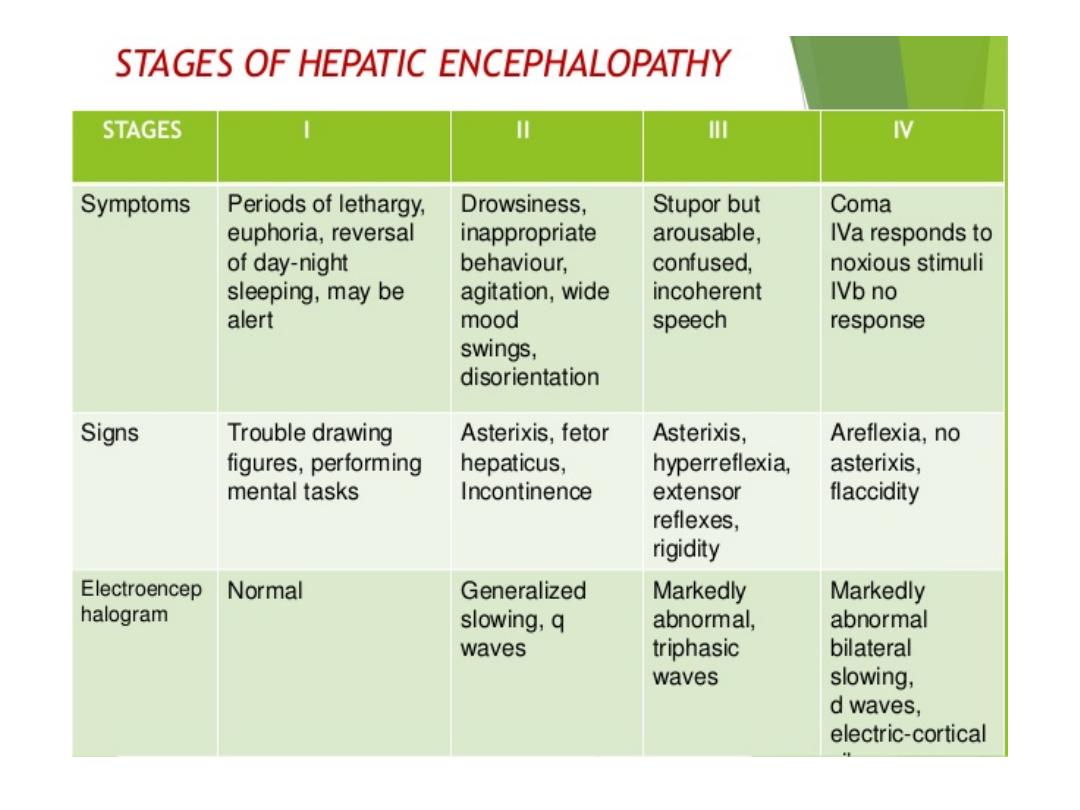
Hepatic encephalopathy
neuropsychiatric syndrome caused by liver disease. As it
progresses, confusion is followed by coma. The
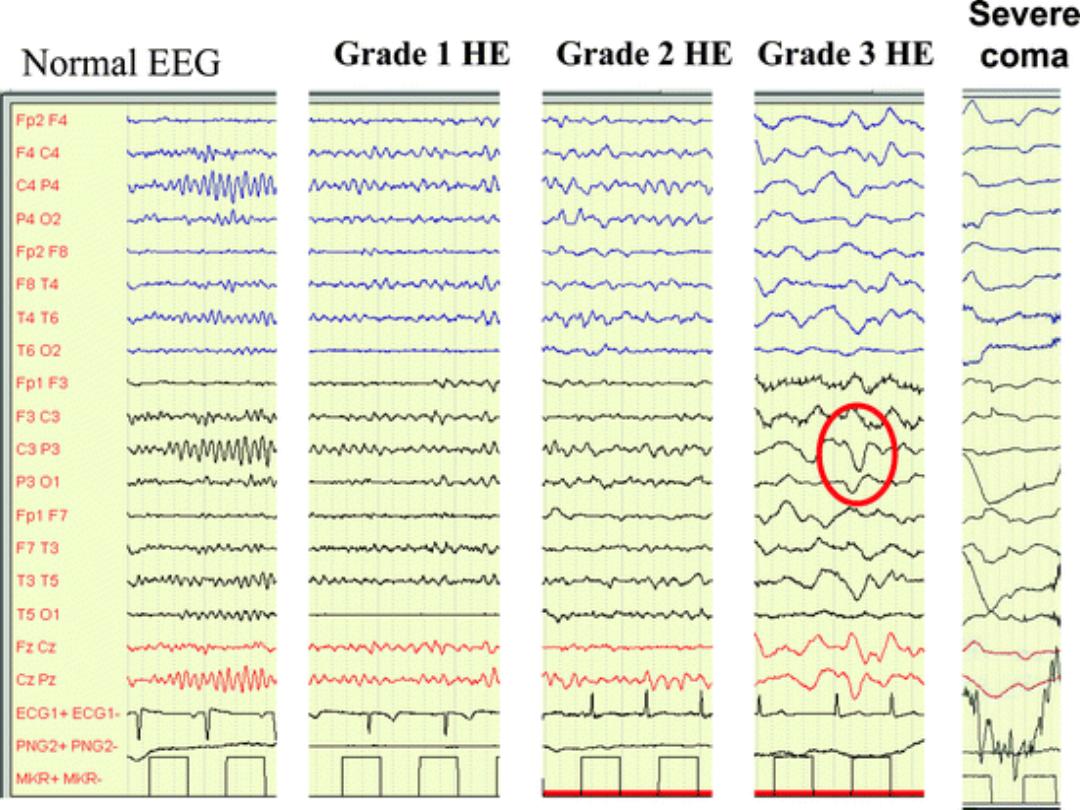
degree of encephalopathy can be graded from 1 to 4,
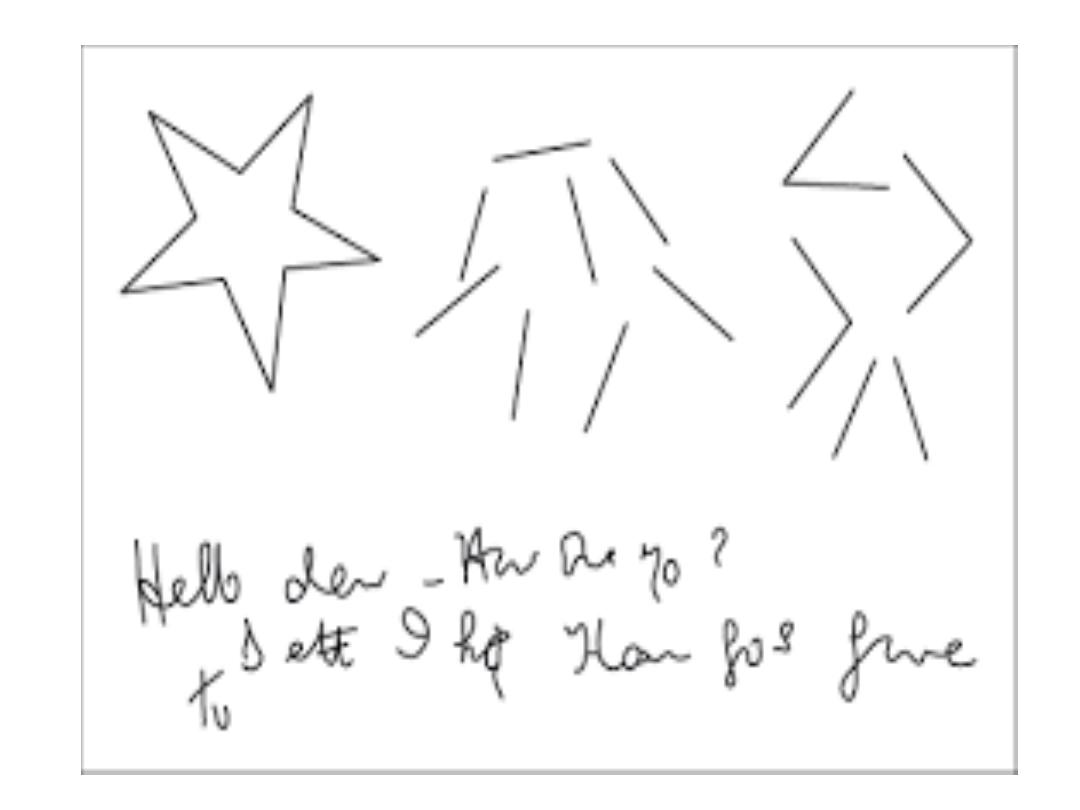
Examination --a flapping tremor (
asterixis)
,
inability to perform simple mental arithmetic tasks or
to draw objects such as a star (
constructional apraxia
;
and, as the condition progresses,
hyper-reflexia
and
bilateral extensor plantar responses
.
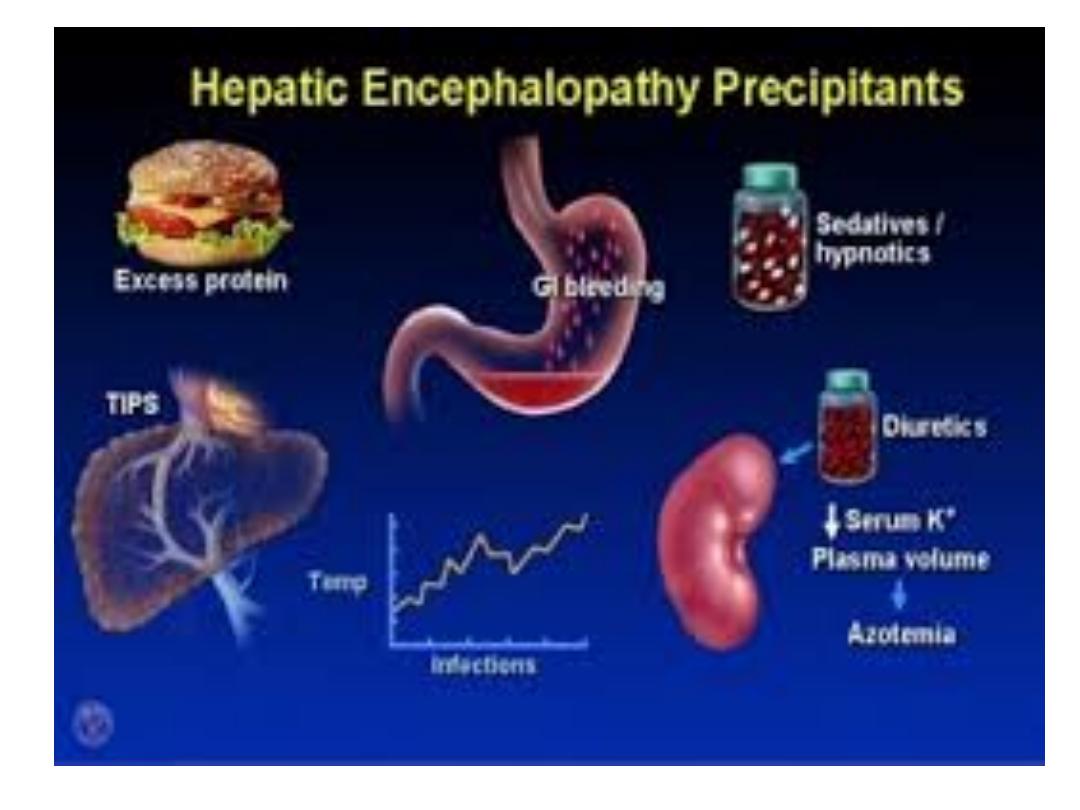
When an episode develops acutely, a precipitating
factor :may be found

• Drugs
(especially sedatives antidepressants)
• Dehydration (
including diuretics paracentesis)
• Infection
• Hypokalaemia
• Constipation
• TIPS
• ↑Protein load (including GI bleeding)

Pathophysiology
disturbance of brain function by neurotoxins that are
normally metabolised by the liver. mainly nitrogenous
substances produced in the gut,
Ammonia
has
traditionally been considered an important factor.
Other:
γ-aminobutyric acid
(GABA) as a mediator
octopamine,
amino acids, mercaptans and fatty acids
that can act
as neurotransmitters
.

Investigations
1-clinical
2-(
EEG
)shows diffuse slowing of
the normal alpha waves with
eventual development of delta
waves.
3-The arterial ammonia is ↑

Rx;
1-precipitatingfactors
2-suppress the production of neurotoxins by bacteria in the bowel.
Rifaximin
(400 mg 3 times daily) is a well tolerated,
non-absorbed antibiotic that acts by reducing
the bacterial content of the bowel and has been shown
to be effective..
-
Lactulose
(15–30 mL 3 times daily) is increased gradually until the
bowels are moving twice daily. It produces an osmotic laxative
effect, reduces the pH of the colonic content, thereby limiting
colonic ammonia absorption
Neomycin
(1-4 g 4-6-hourly) is an antibiotic which acts by reducing the
bacterial content of the bowel
3-Chronic or refractory encephalopathy is one of the main
indications for liver transplantation
.
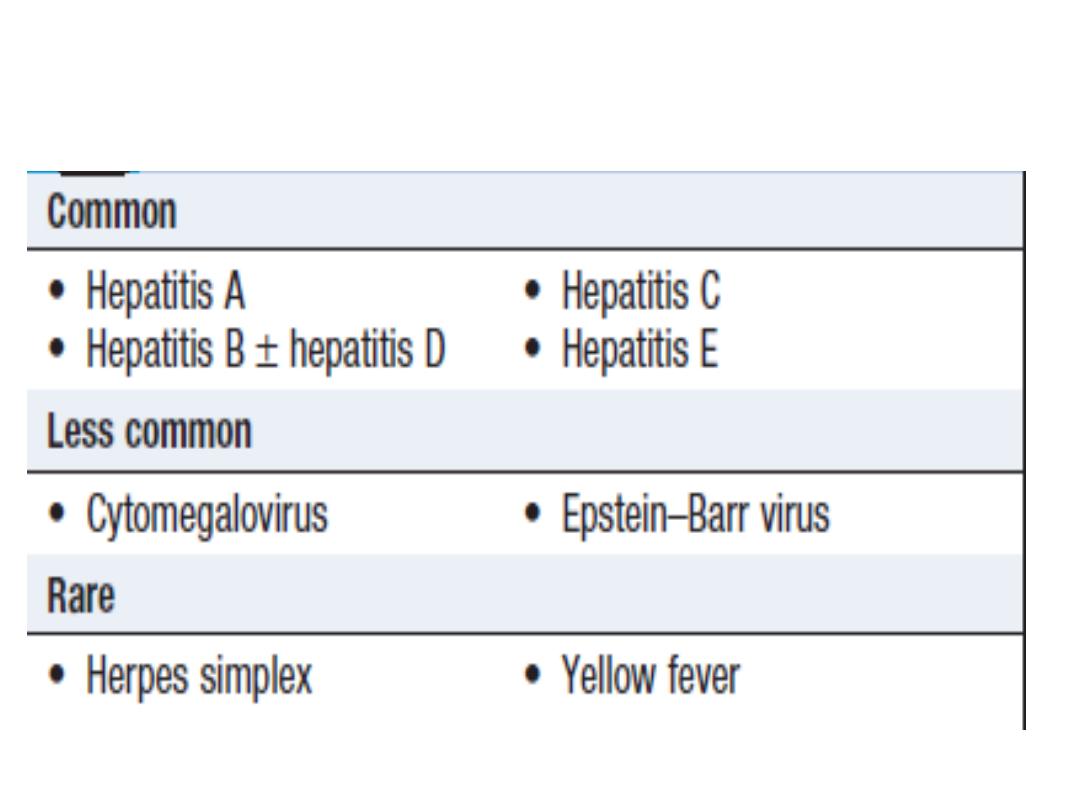
Viral hepatitis
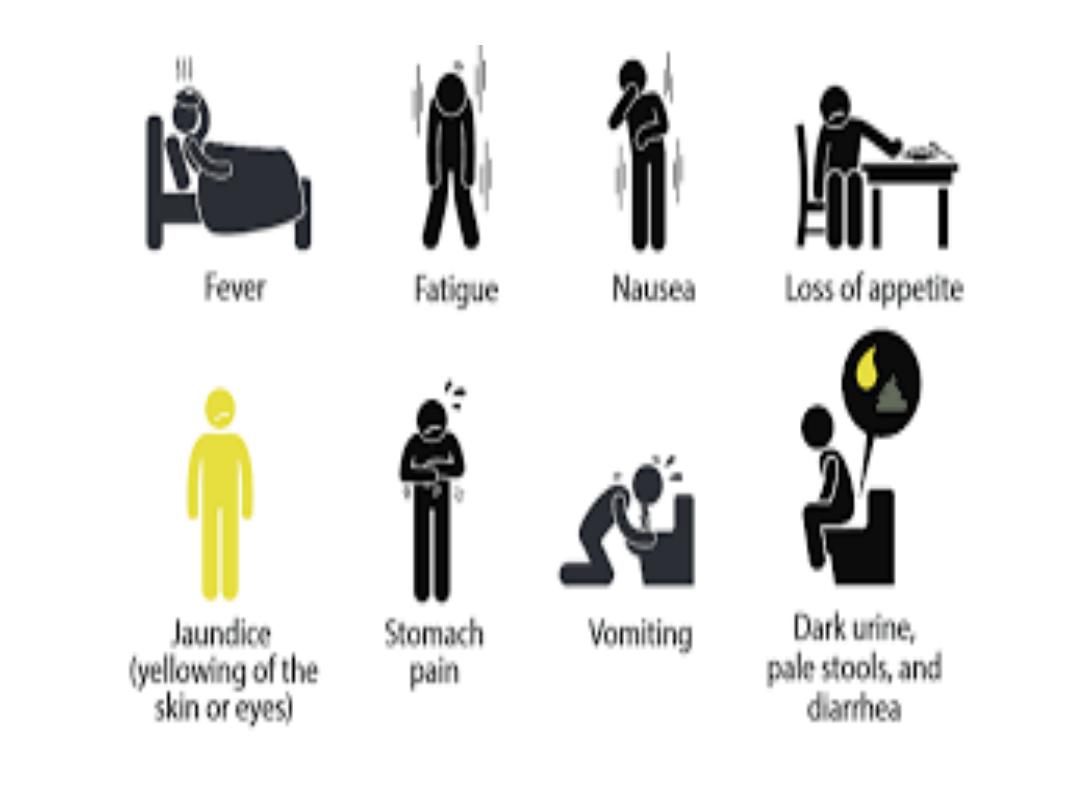
Clinical features of acute infection
-prodromal illness --headache, myalgia, arthralgia, nausea
and anorexia usually precedes the development of jaundice
by a few days to 2 week.
-Vomiting ,diarrhoea ,abdominal discomfort is common.
-Dark urine and pale stools may precede jaundice.
Exam:. The
liver
is often tender but minimally enlarged.
mild splenomegaly and cervical LAP
:Complications

•
Acute liver failure
•
Cholestatic hepatitis (hepatitis A)
• Aplastic anaemia
• Chronic liver disease and cirrhosis
(hepatitis B and C)
• Relapsing hepatitis

Investigations
1-A hepatitic pattern of LFTs
,transaminases
between 200 and 2000 U/L in an acute infection (usually
lower and fluctuating in chronic infections)
2-
bilirubin
reflects the degree of liver damage.
3-
ALP
rarely exceeds twice the upper limit of normal
4-
PT
Prolong indicates the severity of the hepatitis but
rarely exceeds 25 seconds
5-
WBC
=normal with a relative lymphocytosis.
6-
Serological tests
confirm the aetiology of the infection.
Management
→
Most individuals do not need hospital care
.
→
sedatives and narcotics, which are metabolised in the
liver, should be avoided
.
→
No specific dietary modifications are needed
.
→ Alcohol should be avoided during the acute illness.
→
Elective surgery should be avoided in cases
of acute viral hepatitis, as there is a risk of post-operative
liver failure.
→ Liver transplantation is very rarely indicated for
acute viral hepatitis complicated by liver failure
hepatitis A virus
-picornavirus group of enteroviruses.
-highly infectious , spread by the faecal–oral route.
-asymptomatic, excrete the virus in faeces
for about 2–3 weeks before the onset then for a
further 2 weeks.
-Infection is common in children
-common in areas of overcrowding and poor
sanitation.
- In contrast to hepatitis B, achronic carrier state
does not occur.
Investigations
▲ HAV is only present in the
blood
transiently
during the incubation period. Excretion in the
stools
occurs for only 7–14 days after the onset of
the clinical symptoms
▲Anti-HAV IgM is diagnostic of an acute HAV
infection.
▲ Titres of this antibody fall to low levels within
about 3 months of recovery
▲ Anti-HAV IgG is marker of previous HAV
infection. Its presence indicates immunity to HAV.
MX:
▲-prevented
by improving social conditions
, especially overcrowding and
poor sanitation
▲ -
inactivated virus vaccine
..immunization should be considered for
1- chronic hepatitis B or C infections.
2- those at particular risk, such as close contacts of HAV-infected patients,
the elderly, those with other major disease &pregnant women.
3- People travelling to endemic areas
▲ Immediate protection by
immune serum globulin
---
1- after exposure
2-outbreak of hepatitis, in a school or nursery those at risk prevents
secondary spread to families.
Three imp.notes:
-
no role
for antiviral drugs in the therapy of HAV infection
-Acute liver failure is rare in hepatitis A (0.1%) and chronic infection does
not occur
.
-
In adults, a cholestatic phase with elevated ALP levels may complicate
infection
.
Hepatiti s E
RNA virus
-The clinical presentation and management of hepatitis
E are similar to that of hepatitis A.
- faecal–oral route;
-does
not usually
cause chronic liver disease, although
some cases have been described, usually in
immunocompromised patients
Hepatitis E differs from hepatitis A in that infection
during pregnancy is associated with the development of
acute liver failure, which has a high mortality
.
-IgM antibodies to HEV are positive
.
