lec3 Dr.hassan aljumaily
Functional
dyspepsia
Gastroparesis
IBS

Zahraa Ali 35y old divorce with
Hx of abdominal discomfort ,
nausea bloating after meals for
2m.
No drug Hx, not smoker ,not
alcoholic…OGD and Abd.US was
normal. what are the possible
DDx?
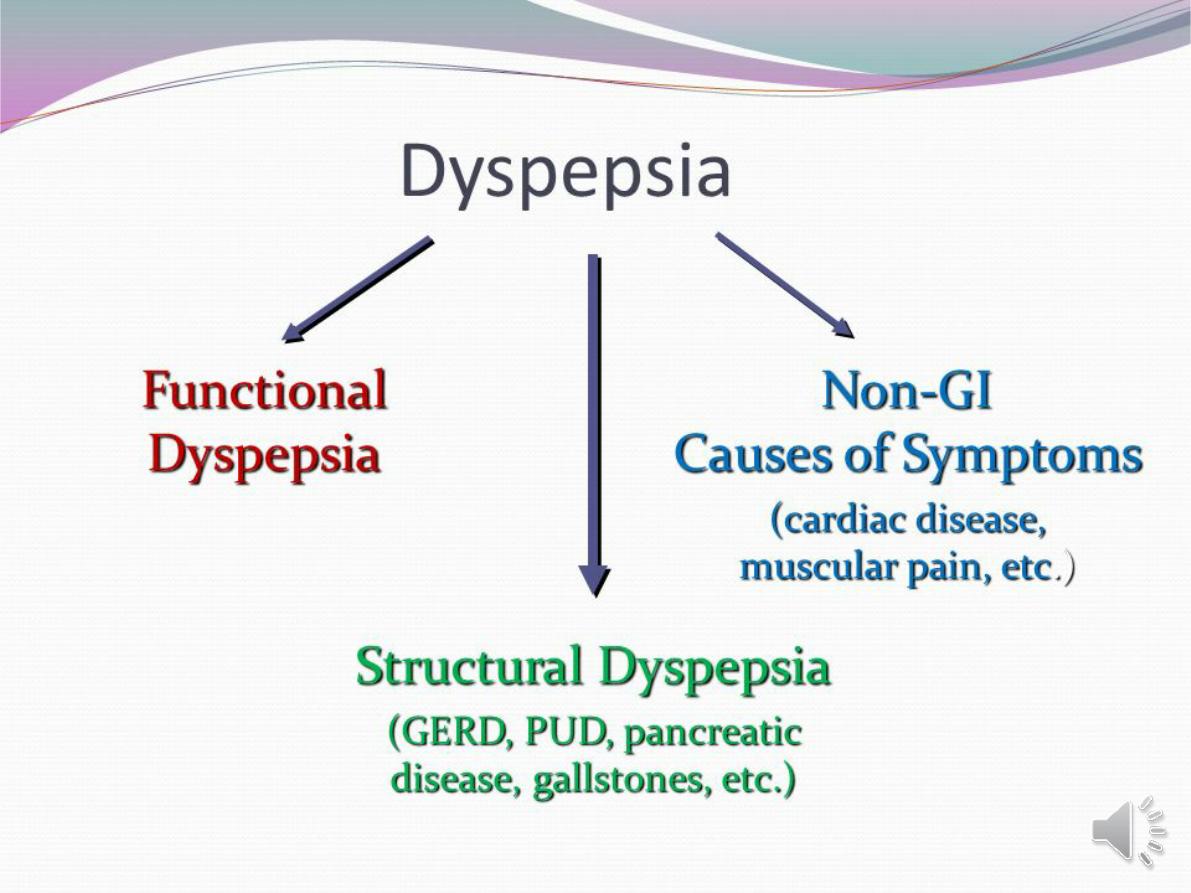
Functional dyspepsia
chronic dyspepsia in the absence of organic disease.
Pathophysiology
spectrum of mucosal, motility and psychiatric disorders.
Clinical features
young (< 40 years) . women >men.
Abdominal discomfort , nausea and bloating after meals.
Morning symptoms are characteristic
DDX
: irritable bowel syndrome, Peptic ulcer disease in older subjects
intra-abdominal malignancy.
▲There are no diagnostic signs apart from tenderness on abdominal
palpation. no weight loss. Patients often appear anxious.
▲A drug history should be taken and the possibility of a depressive
illness should be considered.
▲ Alcohol misuse should be suspected when early morning nausea
and retching are prominent.
Investigations
1-The history.
2-
H. pylori test
3-age > 55 years ----endoscopy to exclude mucosal disease.
4-an ultrasound ----gallstones
Management
▲explanation and reassurance. Possible psychological
factors
▲Up to 10% of patients benefit from
H. pylori
eradication
and this should be offered to infected patients.
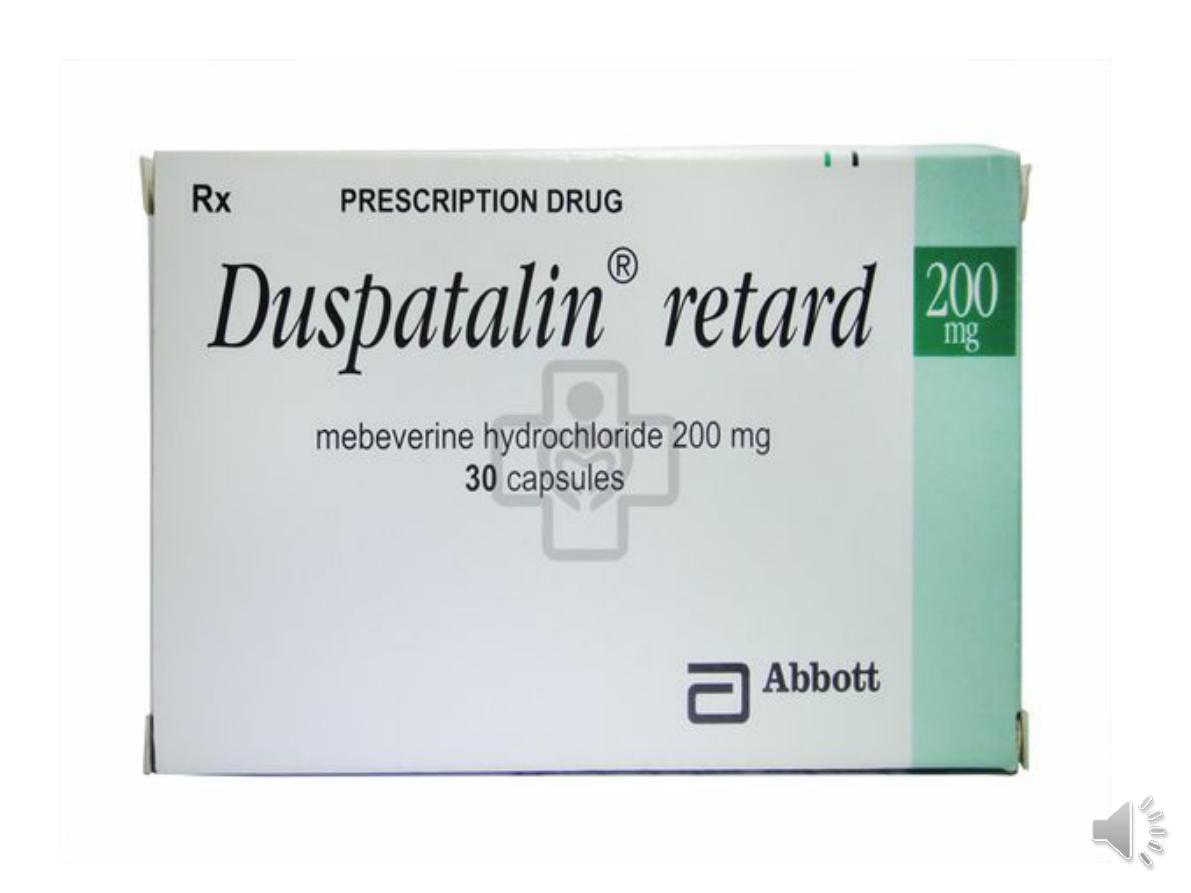
▲ Drugs:.
Antacids
Prokinetic drugs
: such as metoclopramide ,domperidone
may be given before meals if nausea, vomiting or bloating is
prominent..
H2-receptor antagonist
drugs may be tried if night pain or
heartburn
Low-dose tricyclic agents
,, are of value in up to two-thirds.

A 25-year-old woman with history of type 1
diabetes mellitus of 8 years' duration
presents with episodes of postprandial
nausea, vomiting, epigastric pain, fullness,
and bloating. Her diabetes has been poorly
controlled over the years and is complicated
by peripheral neuropathy, retinopathy, and
nephropathy. She reports that she has had
multiple emergency department visits and
admissions to hospital as a
result of dehydration from nausea and
vomiting.
DX?
.

Gastroparesis
Defective gastric emptying without mechanical obstruction
of the stomach or duodenum.
Primary
: due to inherited or acquired disorders of the gastric
pacemaker
secondary
:
▲
disorders of autonomic nerves
(particularly diabetic
neuropathy)
▲
gastroduodenal musculature
(systemic sclerosis,
myotonic dystrophies and amyloidosis).
▲
Drugs
such as opiates, calcium channel antagonists and
those with anticholinergic activity (tricyclics,
phenothiazines)
C.F: Early satiety and recurrent vomiting are the major
symptoms; abdominal fullness and
a succussion splash
may be present on examination
Treatment
-small, frequent,
low-fat meals
-use of
metoclopramide and domperidone
.
-Insevere cases, nutritional failure can occur
and long-term
jejunostomy feeding or total
TPN is required.
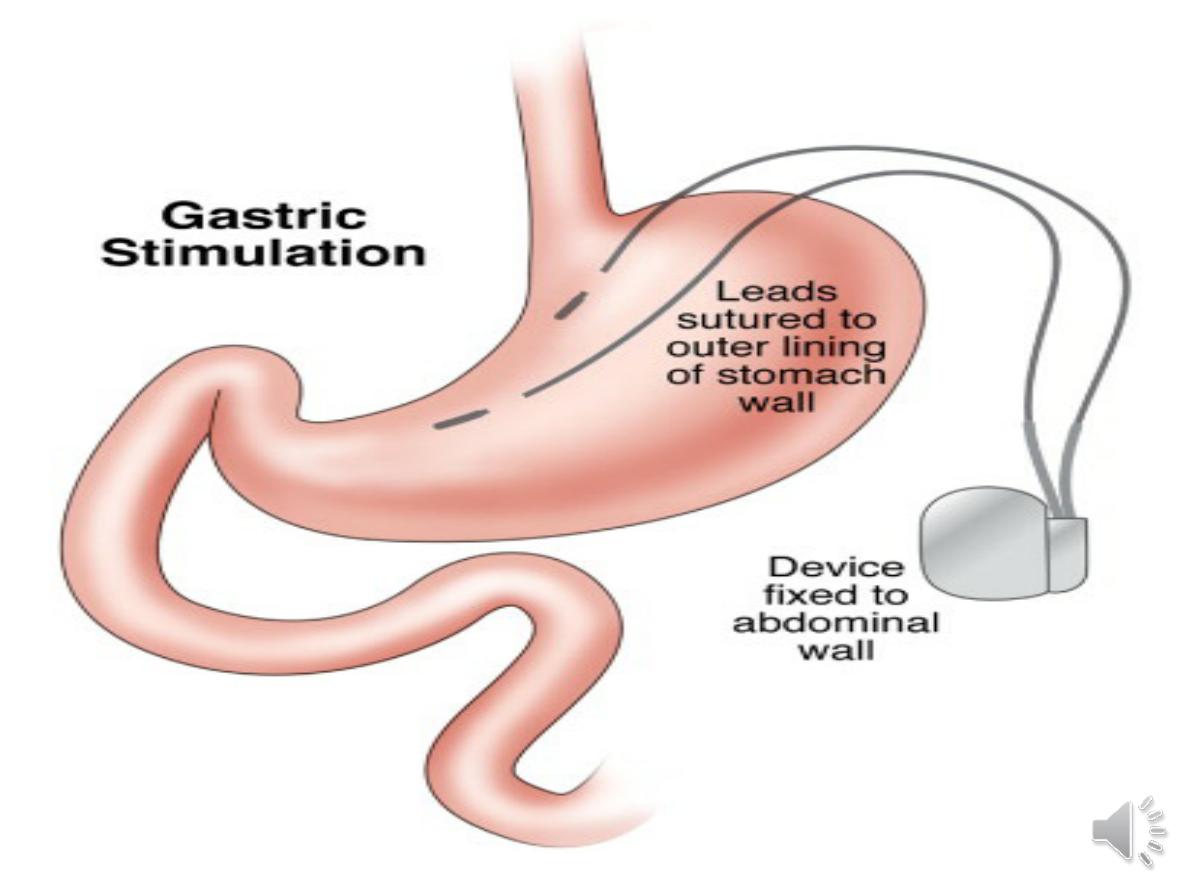
-Surgical insertion of a
gastric
neurostimulator
has been successful in
some cases, especially those complicating
diabetic autonomic neuropathy.


A 34-year-old mother of 3 presents to her family
physician with a 3-week history of abdominal
cramping pain in both lower quadrants. She has
been having frequent small, soft stools
accompanied by some mucus but no blood. Her
symptoms are improved with bowel movement or
passage of flatus.. Family history is negative for
colon cancer.. Personal/social history reveals that
she is an accountant working long hours. Review of
systems is otherwise negative. She has not lost any
weight. On physical examination, the only finding is
some mild tenderness in the RLQ. No mass is felt.

A 40-year-old housewife complains of recurrent
constipation. She has had problems since her 20s,
but they are worse now. The constipation is
accompanied by abdominal bloating and abdominal
pain, and the discomfort is only better when she has
a bowel movement. Her past history includes a
cholecystectomy and a hysterectomy. Physical
examination is entirely normal. Rectal examination
reveals normal consistency stool. Stool samples
test negative for occult blood.
. Young women are affected 2–3 times more often than men
Rome III criteria for diagnosis of irritable bowel syndrome:
Recurrent abdominal pain or discomfort at least 3 days/mth
in
the last 3 months, associated with
two or more
of the
following:
• Improvement with defecation
• Onset associated with a change in frequency of stool
• Onset associated with a change in form (appearance) of
stool
.
@ Most patients alternate between episodes of diarrhea and
constipation.
@ Passage of mucus is common but rectal bleeding does
not occur. Patients do not lose weight and are
constitutionally well
@ Physical examination -------variable tenderness to
palpation.
@ Coexisting conditions, such as
non-ulcer dyspepsia
,
chronic fatigue syndrome, dysmenorrhoea and fibromyalgia
,
are common
Pathophysiology
Behavioural and psychosocial factors
50% of patients have a psychiatric illness, such as anxiety,
depression, neurosis. Panic attacks are also common. alter
visceral perception and GI motility.
Physiological factors
1-excessive release
of 5-HT
in diarrhoea-predominant IBS (D-
IBS) and relative deficiency with constipation-predominant
IBS (C-IBS).
2- low-grade gut inflammation or , immune activation ---
raised numbers of mucosal mast cells, which sensitise
enteric neurons by releasing
histamine
. Some patients
respond positively to mast cell stabilisers, such as
ketotifen
.
3-immune activation may be associated with altered CNS
processing of visceral pain signals.
This is more common in women and in D-IBS, and may be
triggered by a prior episode of gastroenteritis with
Salmonella
or
Campylobacter
species.
Luminal factors
1-. Small intestinal
bacterial overgrowth ---
may
explain the response to
probiotics
("good" or "helpful"
bacteria because they help keep your gut healthy .or
the non-absorbable antibiotic.
rifaximin
2-Some patients have chemical food intolerances
(not allergy) to
FODMAPs
(fermentable oligo-, di-
and monosaccharides, and polyols). Their
fermentation in the colon leads to
bloating, pain,
wind and altered bowel habit
. Non coeliac
gluten
sensitivity (negative coeliac serology and normal
duodenal biopsies) seems to be present in some
IBS patients
,
Alarm features
• Age > 50 yrs; male gender
• Weight loss
• Nocturnal symptoms
• Family history of colon cancer
• Anaemia
• Rectal bleeding

♠
faecal calprotectin
, with or without
sigmoidoscopy
, are usually done and are
normal in IBS.
♠
Colonoscopy
should be undertaken in
older patients (over 40 years of age) to
exclude colorectal cancer.
♠ Diarrhoea predominant patients justify
investigations to exclude
coeliac disease ,
microscopic colitis lactose intolerance ,bile
acid malabsorption , thyrotoxicosis and,
parasitic infection
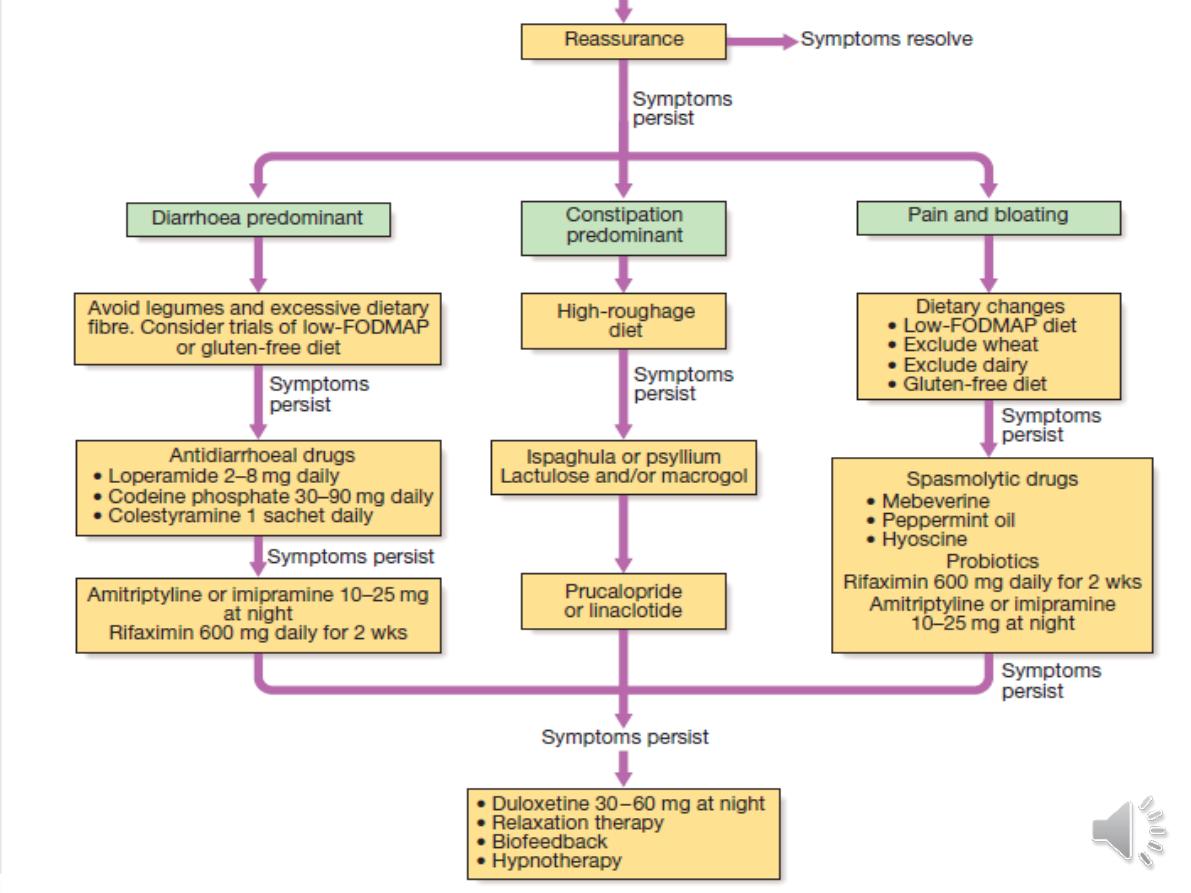
Management
♠
reassure the patient
.
♠. Up to 20% may benefit from
a wheat-free diet, some may
respond to lactose exclusion, and excess intake of caffeine
or artificial sweeteners,..
♠
Probiotics
--for intractable symptoms
♠ a
tricyclic antidepressant
, such as amitriptyline or
imipramine (. It may act by reducing visceral sensation and
by altering gastrointestinal motility..
♠The
5-HT4 agonist
prucalopride
, the guanylate cyclase-C
receptor agonist
linaclotide
, and chloride channel activators,
such as
lubiprostone
, can be effective in constipation
predominant IBS.
♠Trials of anti-inflammatory agents, such as
ketotifen
, and
the
antibiotic rifaximin
may be considered in.
♠Psychological interventions