Peripheral Vascular
Disease
Acute & Chronic Limb Ischemia
Lipi Shukla
What is PVD?
Definition:
. Definition:
Sudden occlusion of an artery is commonly due to either
emboli or trauma & it may also happen when thrombosis
occur on plaque pre-existing atheroma.
•
Occlusive disease of the arteries of the lower
extremity.
•
Most common cause:
o
Atherothrombosis
o
Others: arteritis, aneurysm + embolism.
•
Has both ACUTE and CHRONIC Px
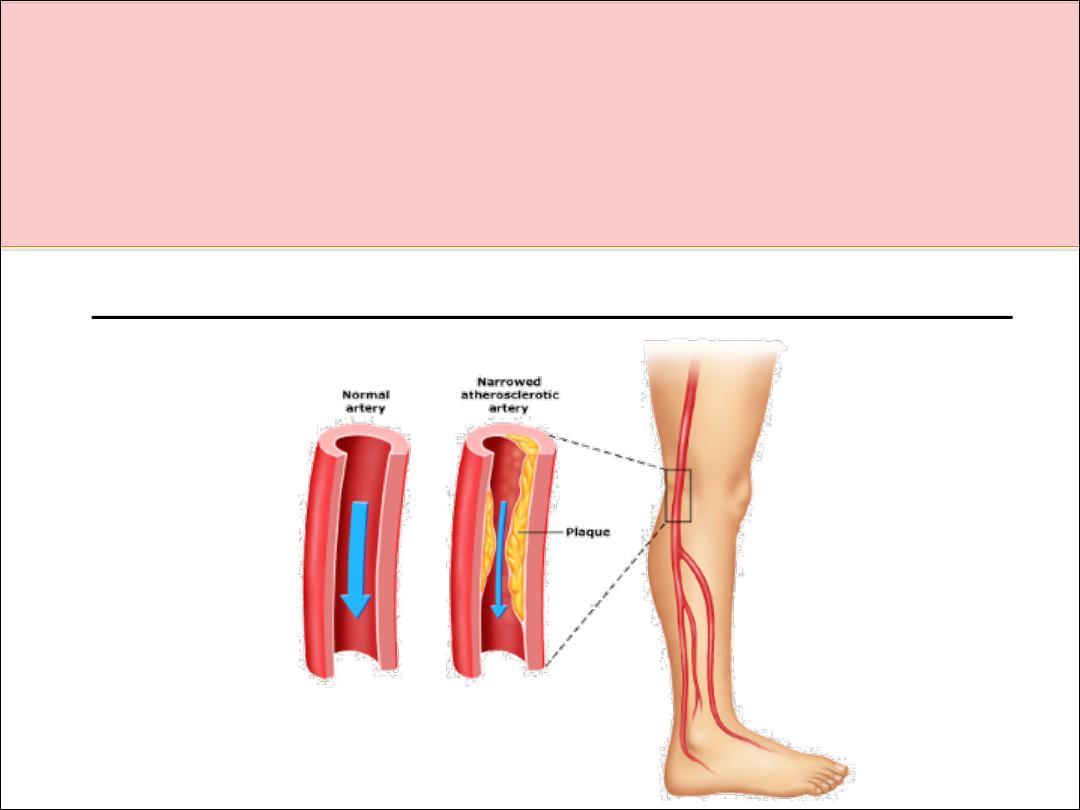
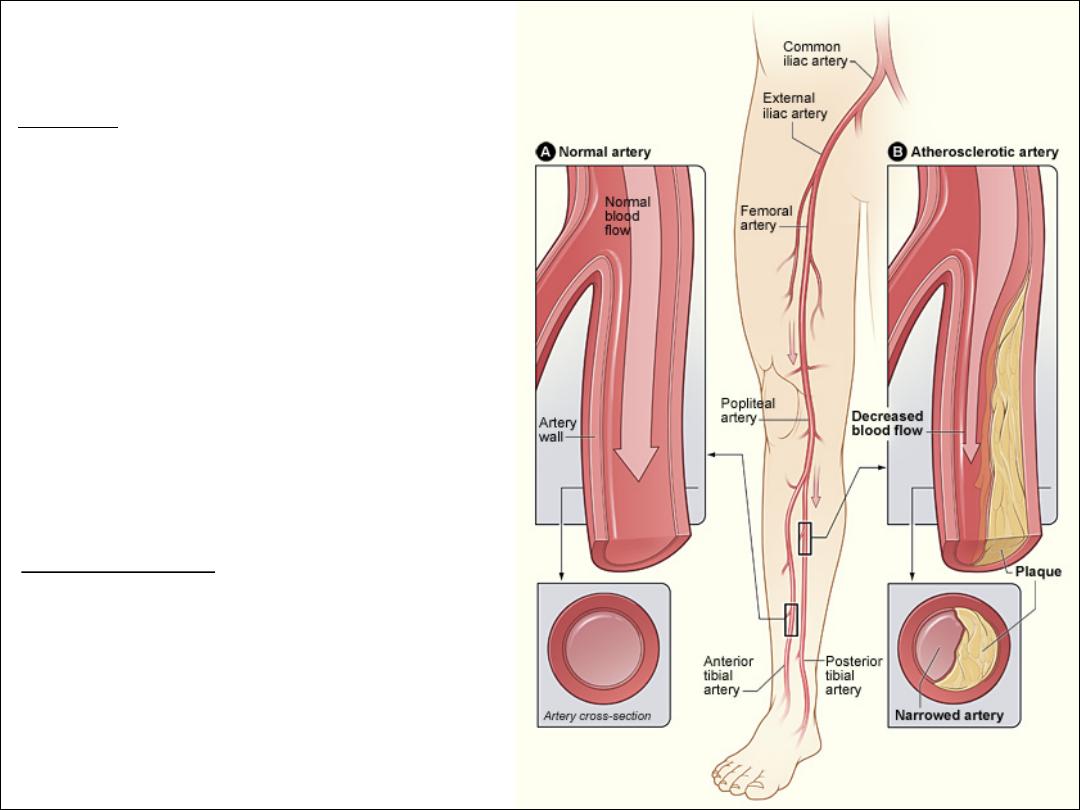
Pathophysiology:
•
Arterial narrowing à Decreased
blood flow = Pain
•
Pain results from an imbalance
between supply and demand of
blood flow that fails to satisfy
ongoing metabolic requirements.
The Facts:
1. The prevalence: >55 years is 20%
2. 70%–80% of affected individuals are asymptomatic
3. Pt’s with PVD alone have the same relative risk of death from
cardiovascular causes as those CAD or CVD
4. PVD pt’s = 4X more likely to die within 10 years than pt’s without
the disease.
5. The ankle–brachial pressure index (ABPI) is a simple, non-invasive
bedside tool for diagnosing PAD — an ABPI <0.9 = diagnostic for PAD
6. Patients with PAD require medical management to prevent future
coronary and cerebral vascular events.
7. Prognosis at 1 yr in patient’s with Critical Limb Ischemia (rest pain):
•
Alive with two limbs — 50%
•
Amputation — 25%
•
Cardiovascular mortality 25%
Risk Factors:
Typical Patient:
•
Smoker (2.5-3x)
•
Diabetic (3-4x)
•
Hypertension
•
Hx of Hypercholesterolemia/AF/IHD/CVA
•
Age ≥ 70 years.
•
Age 50 - 69 years with a history of smoking or diabetes.
•
Age 40 - 49 with diabetes and at least one other risk factor for
atherosclerosis.
•
Leg symptoms suggestive of claudication with exertion or
ischemic pain at rest.
•
Abnormal lower extremity pulse examination.
•
Known atherosclerosis at other sites (eg, coronary, carotid, or
renal artery disease).

Factors influencing the clinical manifestations of
peripheral arterial disease
1- Anatomical site
q
Cerebral circulation
q
Renal arteries
q
Mesenteric arteries
q
Limbs (legs [Gt ] arms)
2- Collateral supply
3- Speed of onset
4- Mechanism of injury Haemodynamic
q
Thrombotic
q
Atheroembolic
q
Thromboembolic
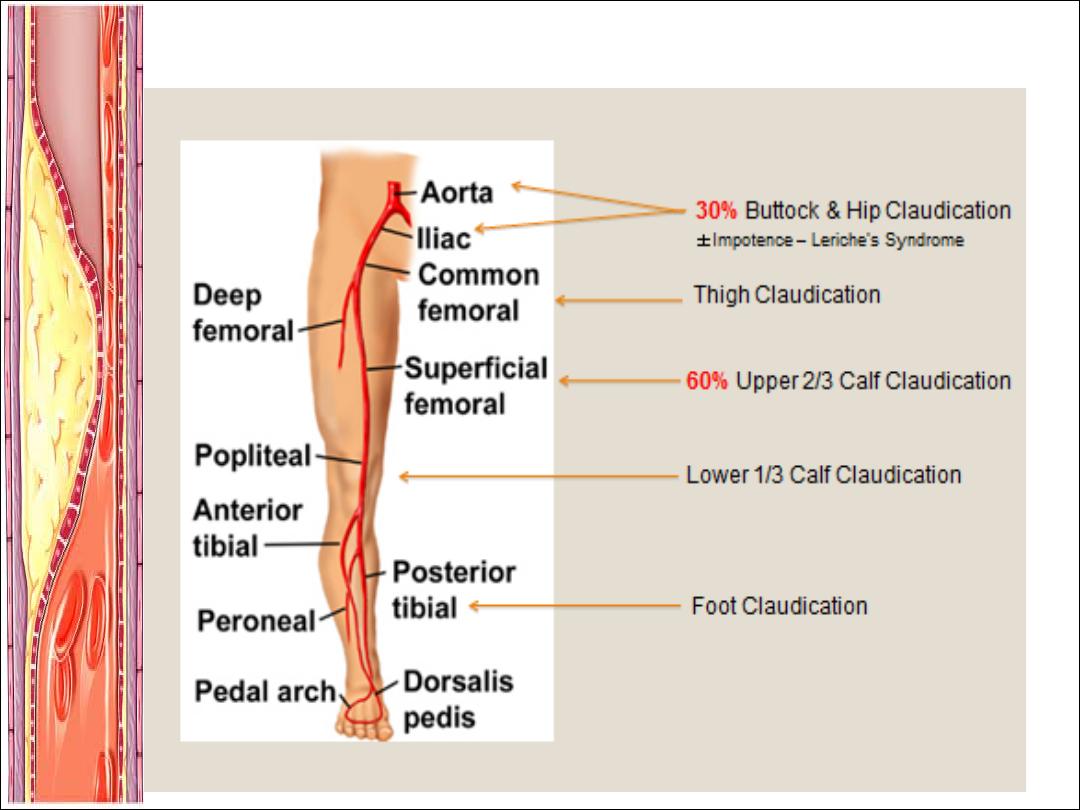
Chronic lower limb arterial disease
Intermittent claudication (IC)
Ø
Derived from the latin word ( to limp )
Ø
ischaemic pain affecting the muscles of the leg upon walking.
Ø
claudication distance
Ø
5% of middle-aged men report IC
Ø
only 1-2% per year amputation and/or revascularisation is
required
Ø
annual mortality rate >5%( 2-3 times higher than in non-claudicant)
Claudication vs. Pseudoclaudication
Claudication
Pseudoclaudication
Characteristic of
discomfort
Cramping, tightness,
aching, fatigue
Same as claudication
plus tingling, burning,
numbness
Location of
discomfort
Buttock, hip, thigh,
calf, foot
Same as
claudication
Exercise-induced
Yes
Variable
Distance
Consistent
Variable
Occurs with standing
No
Yes
Action for relief
Stand
Sit, change position
Time to relief
<5 minutes
£30 minutes
Also see Table 4 of Hirsch AT, et al. J Am Coll Cardiol. 2006;47:e1-e192.
Physical Examination:
Examination:
What do to:
Inspection
Expose the skin
and look for:
•
Thick Shiny Skin
•
Hair Loss
•
Brittle Nails
•
Colour Changes (pallor)
•
Ulcers
•
Muscle Wasting
Palpation
•
Temperature (cool, bilateral/unilateral)
•
Pulses: ?Regular, ?AAA
•
Capillary Refill
•
Sensation/Movement
Auscultation
•
Femoral Bruits
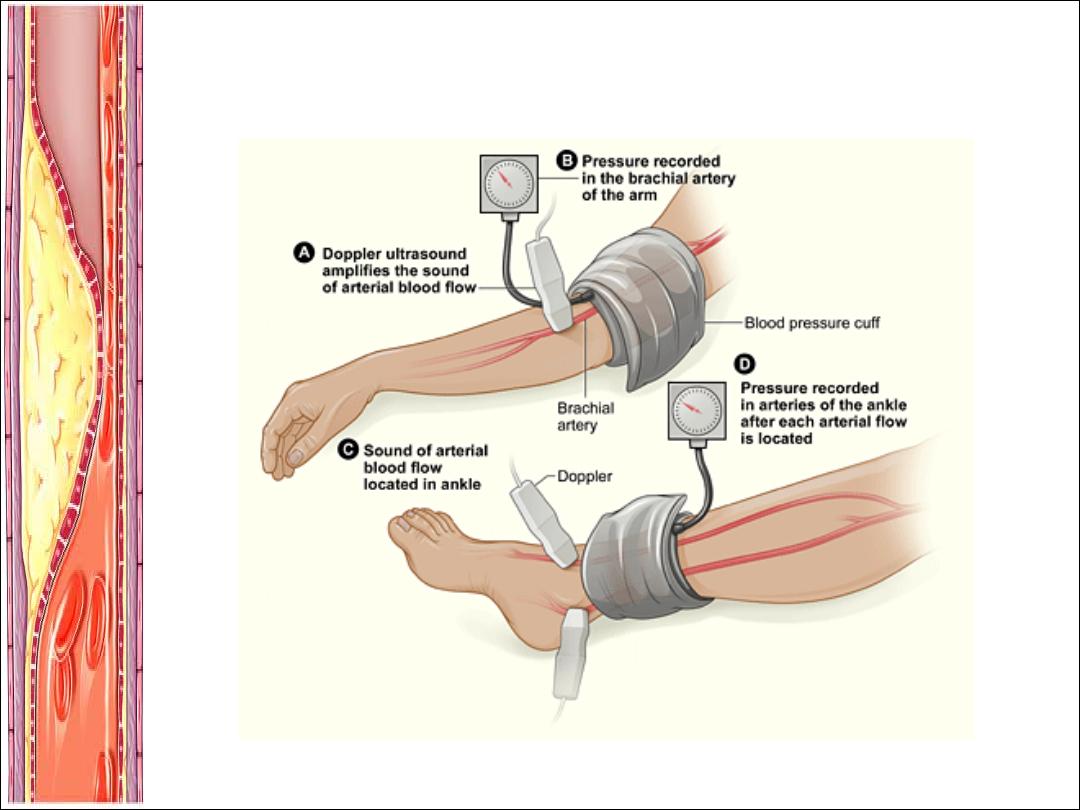
Ankle Brachial
Index (ABI)
= Systolic BP in ankle
Systolic BP in brachial artery
Buerger’s Test
•
Elevate the leg to 45° - and look for pallor
•
Place the leg in a dependent position 90°& look
for a red flushed foot before returning to normal
•
Pallor at <20° = severe PAD.

Pictures:
DDx of Leg Pain
1. Vascular
a) DVT (as for risk factors)
b) PVD (claudication)
2. Neurospinal
a) Disc Disease
b) Spinal Stenosis (Pseudoclaudication)
3. Neuropathic
a) Diabetes
b) Chronic EtOH abuse
4. Musculoskeletal
a) OA (variation with weather + time of day)
b) Chronic compartment syndrome
What does the ABI mean?
ABI
Clinical Correlation
>0.9
Normal Limb
0.5-0.9
Intermittent Claudication
<0.4
Rest Pain
<0.15
Gangrene
CAUTION:
Patient’s with Diabetes + Renal Failure:
They have calcified arterial walls which can falsely elevate their ABI.
Understanding the ABI
The ratio of the higher brachial systolic pressure and the
higher ankle systolic pressure for each leg:
Ankle systolic pressure
Higher brachial artery systolic pressure
ABI =
Interpreting the Ankle-Brachial Index
Adapted from Hirsch AT, et al. J Am Coll Cardiol. 2006;47:e1-e192. Figure 6.
ABI
Interpretation
1.00–1.29
Normal
0.91–0.99
Borderline
0.41–0.90
Mild-to-moderate disease
≤0.40
Severe disease
≥1.30
Noncompressible

ABI Limitations
•
Incompressible arteries (elderly patients, patients
with diabetes, renal failure, etc.)
•
Resting ABI may be insensitive for detecting mild
aorto-iliac occlusive disease
•
Not designed to define degree of functional
limitation
•
Normal resting values in symptomatic patients
may become abnormal after exercise

Toe-Brachial Index Measurement
•
The toe-brachial index
(TBI) is calculated by
dividing the toe pressure
by the higher of the two
brachial pressures.
•
TBI values remain
accurate when ABI values
are not possible due to
non-compressible pedal
pulses.
•
TBI values ≤ 0.7 are
usually considered
diagnostic for lower
extremity PAD.
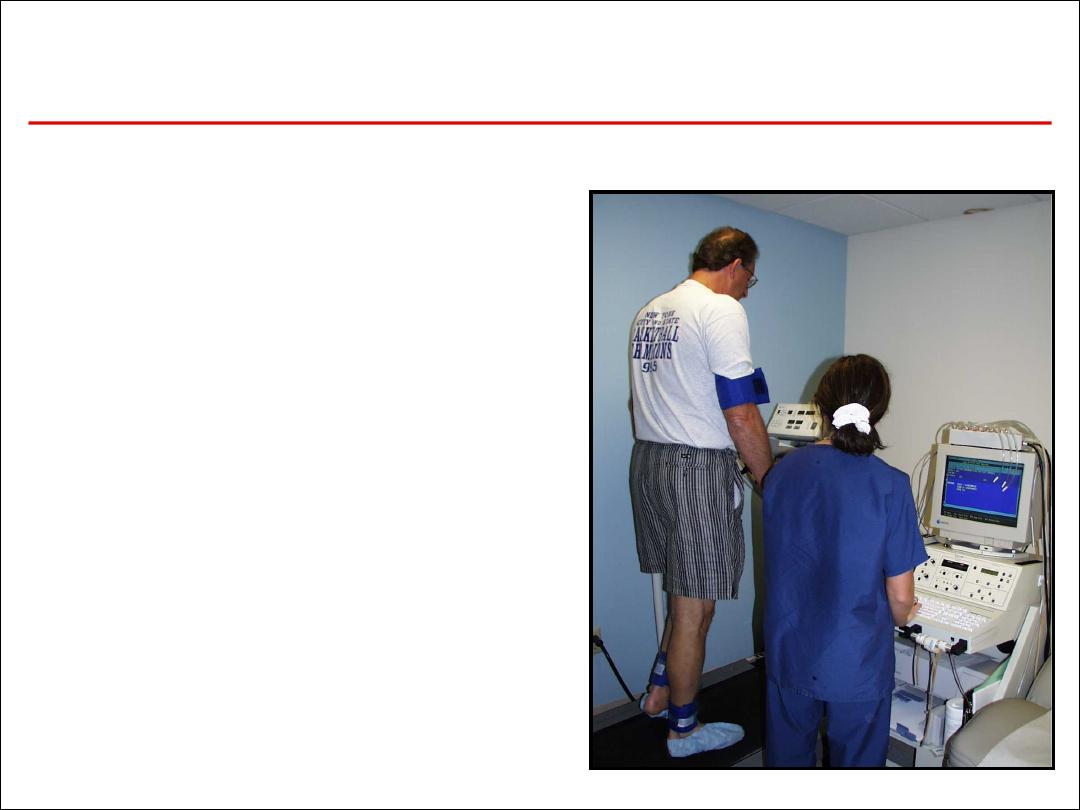
Exercise ABI Testing
•
Confirms the PAD diagnosis
•
Assesses the functional
severity of claudication
•
May “unmask” PAD when
resting ABI is normal
•
Aids differentiation of
intermittent claudication
vs. pseudoclaudication
diagnoses

Critical limb ischaemia (CLI)
defined as rest (night) pain, requiring opiate analgesia,
and/or tissue loss (ulceration or gangrene), present for
more than 2 weeks, in the presence of an ankle BP of < 50
mmHg.
Rest pain only, with ankle pressures > 50 mmHg, is known
as subcritical limb ischaemia (SCLI).
The term severe limb ischaemia (SLI) is used to describe
both CLI and SCLI
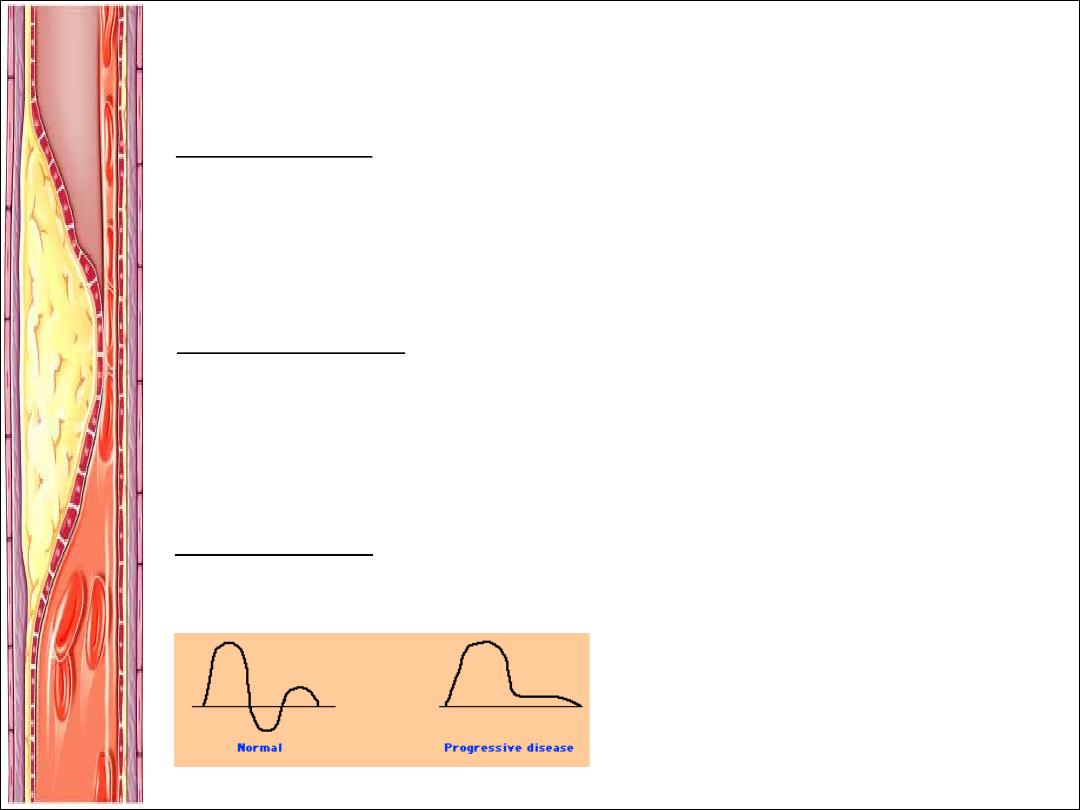
Investigations:
NON INVASIVE:
Duplex Ultrasound
à
normal is triphasic à biphasic à monophasic à absent
BLOOD TESTS:
1.
FBE/EUC/Homocysteine Levels
2.
Coagulation Studies
3.
Fasting Lipids and Fasting Glucose
4.
HBA1C
WHEN TO IMAGE:
1.
To image = to intervene
2.
Pt’s with disabling symptoms where revascularisation is considered
3.
To accurately depict anatomy of stenosis and plan for PCI or Surgery
4.
Sometimes in pt’s with discrepancy in hx and clinical findings
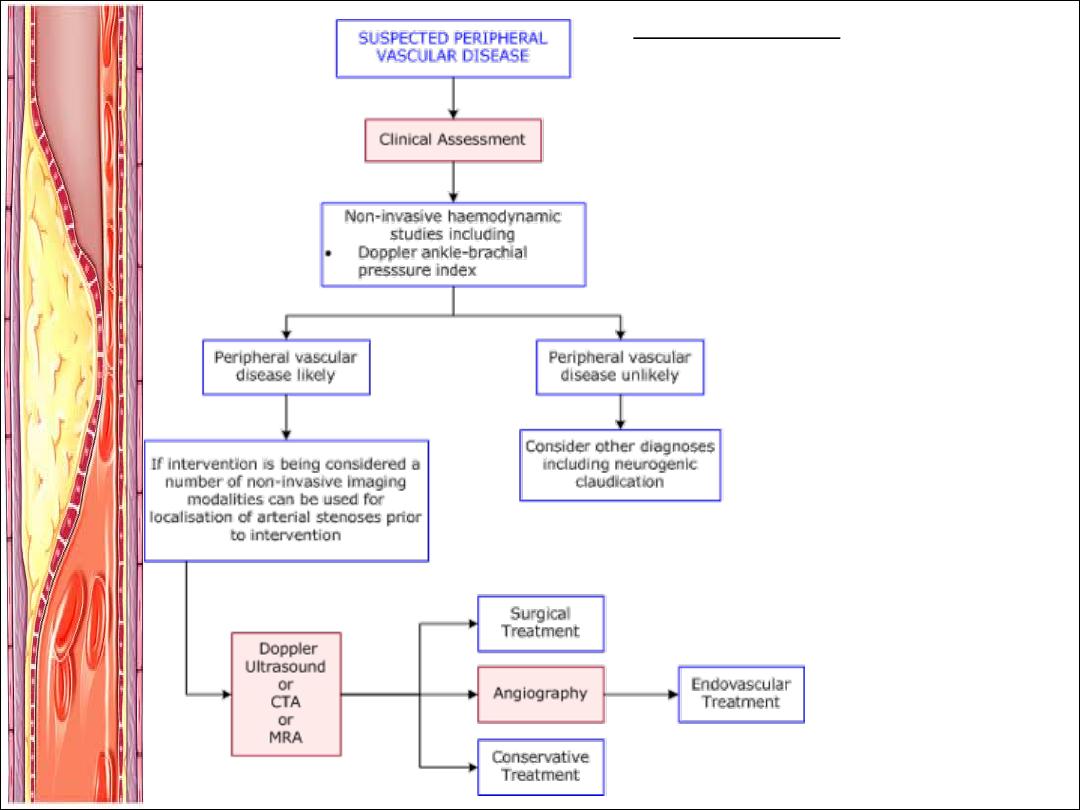
ANGIOGRAPHY:
Non-invasive:
•
CT Angiogram
•
MR Angiogram
Invasive:
•
Digital Subtraction Angiography
à
Gold Standard
à
Intervention at the same time
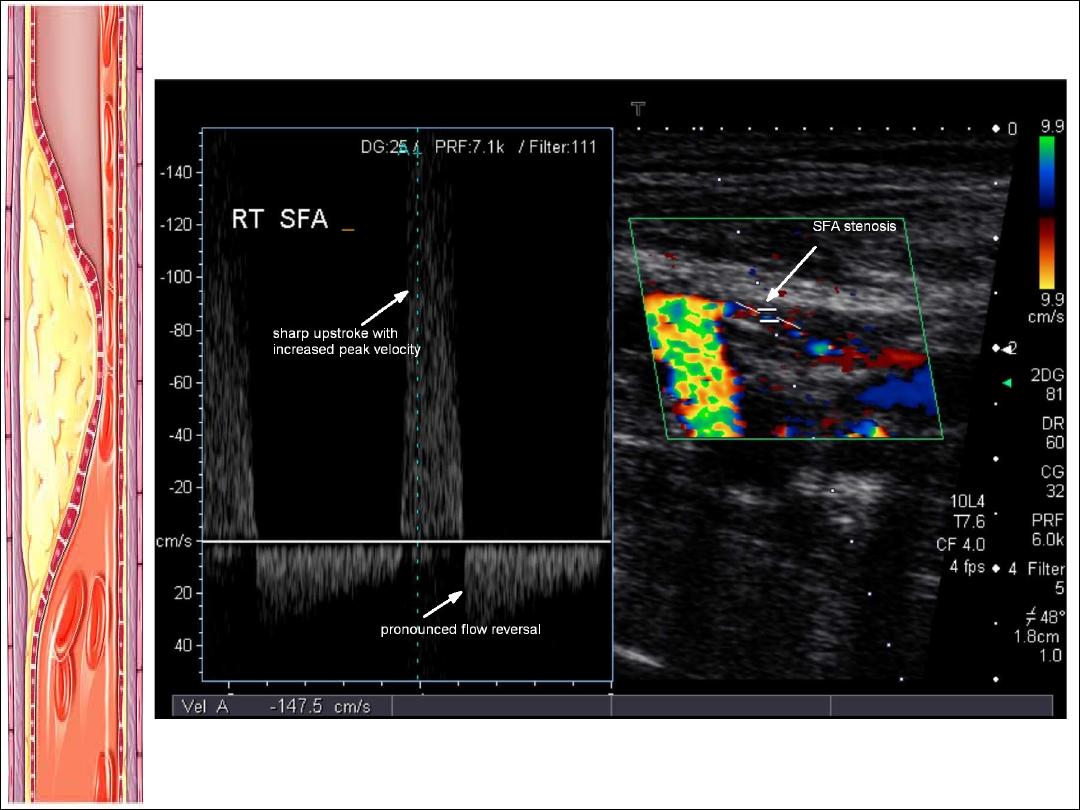
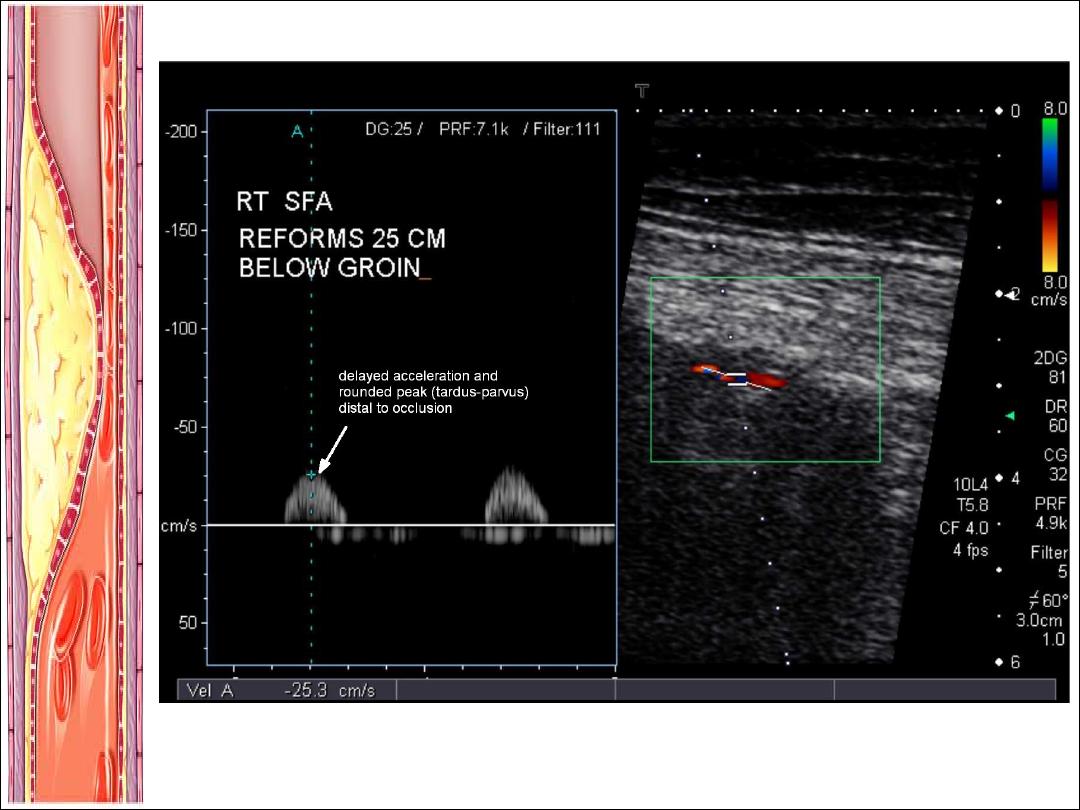
Tardus et parvus = small amplitude + slow rising pulse
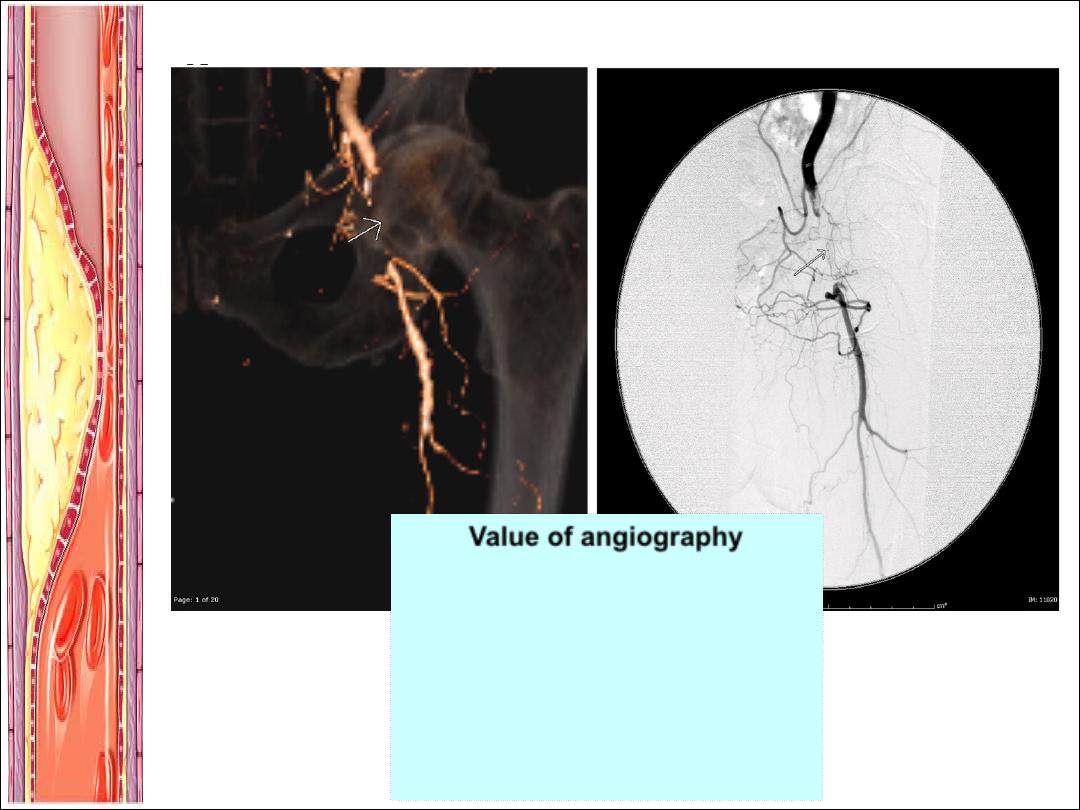
CT Angiography
Digital Subtraction Angiography
Value of angiography
§
Localizes the obstruction
§
Visualize the arterial tree & distal
run-off
§
Can diagnose an embolus:
Sharp cutoff, reversed meniscus or clot
silhouette

Treatment:
1. RISK FACTOR MODIFICATION:
a) Smoking Cessation
b) Rigorous BSL control
c) BP reduction
d) Lipid Lowering Therapy
3. MEDICAL MANAGEMENT:
a) Antiplatelet therapy e.g.
Aspirin/Clopidogrel
b) Phosphodiesterase Inhibitor e.g.
Cilostazol
c) Foot Care
2. EXERCISE:
a) Claudication exercise
rehabilitation program
b) 45-60mins 3x weekly for 12 weeks
PTA/Surgery:
Indications/Considerations:
•Poor response to exercise rehabilitation + pharmacologic therapy.
•Significantly disabled by claudication, poor QOL
•The patient is able to benefit from an improvement in claudication
•The individual’s anticipated natural hx and prognosis
•Morphology of the lesion (low risk + high probabilty of operation
success)
PTA:
•Angioplasty and Stenting
•Should be offered first to patients with significant comorbidities who are
not expected to live more than 1-2 years
Bypass Surgery:
•Reverse the saphenous vein for femoro-popliteal bypass
•Synthetic prosthesis for aorto-iliac or ilio-femoral bypass
•Others = iliac endarterectomy & thrombolysis
•Current Cochrane review = not enough evidence for Bypass>PCI
Amputation: Last Resort
What are the features of an
acute ischemic limb?
REMEMBER THE 6 P’S:
1. PAIN
2. PALLOR
3. PULSELESNESS
4. PERISHING COLD (POIKILOTHERMIA)
5. PARASTHESIAS
6. PARALYSIS
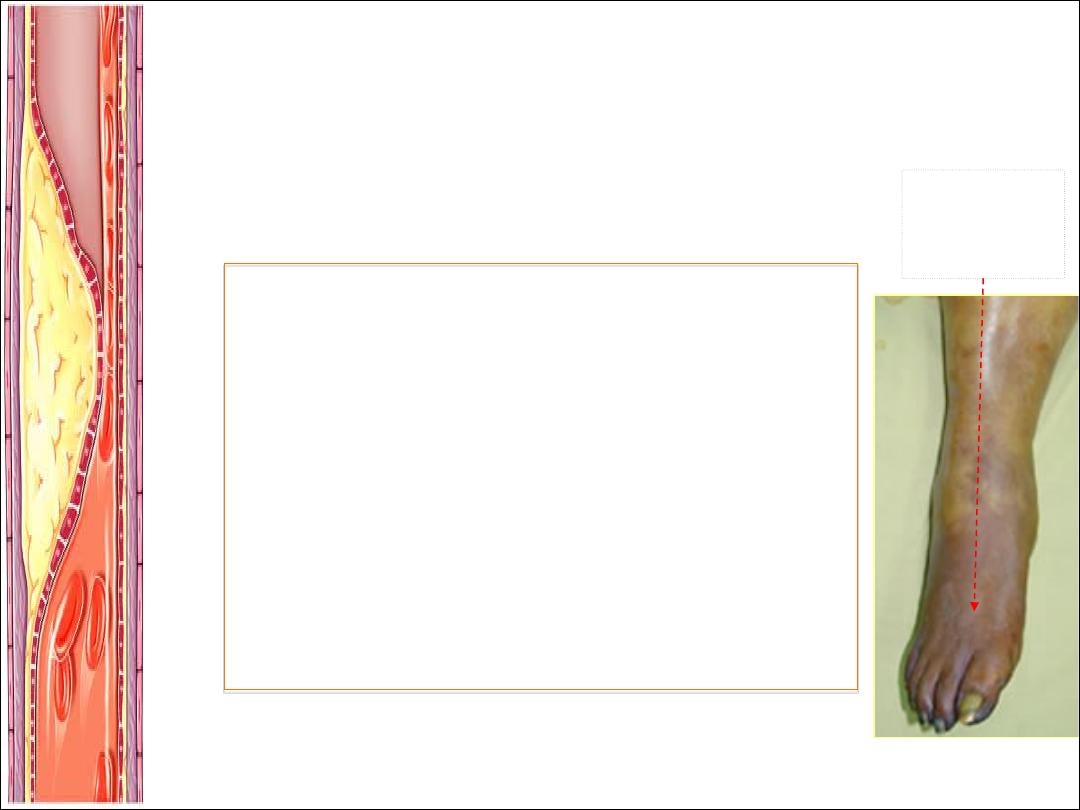
Fixed
mottling &
cyanosis
What will you do now?
1. CALL THE VASCULAR SURGEON OR
INTERVENTIONALIST
2. ORDER INVESTIGATIONS
a) FBE
b) EUC
c) Coagulation Studies
d) Group and Hold
e) 12 Lead ECG
f) Chest XR
3. INITATE ACUTE MANAGEMENT:
a) Analgesia
b) Commence IV heparin
c) Call Radiology for Angiography if limb still viable
d) Discuss for :
i) Thrombotic cause à ?cathetar induced thrombolysis
ii) Embolic cause à ?embolectomy
iii) All other measures not possible à Bypass/Amputation
Simple measures to improve
existing perfusion:
•
Keep the foot dependant
•
Avoid pressure over the heel
•
Avoid extremes of temperature
(cold induces vasospasm)
•
Maximum tissue oxygenation
(oxygen inhalation)
•
Correct hypotension
Questions?
