Hypertensive Disorders
of Pregnancy
Dr.Nadia Mudher Al-Hilli
FICOG
Department of Obs&Gyn
College of Medicine
University of babylon
LEARNING OBJECTIVES
To understand the classification of hypertension
in pregnancy.
To appreciate and be able to differentiate the
different risk factors
To understand the pathophysiology of pre-
eclampsia.
To be aware of the clinical presentation of pre-
eclampsia and understand the principles of
management.
Hypertension:
One measurement of diastolic BP of 110 mmHg
or more; or
Two consecutive measurements of diastolic BP of
≥ 90 mmHg 4 hours or more apart.
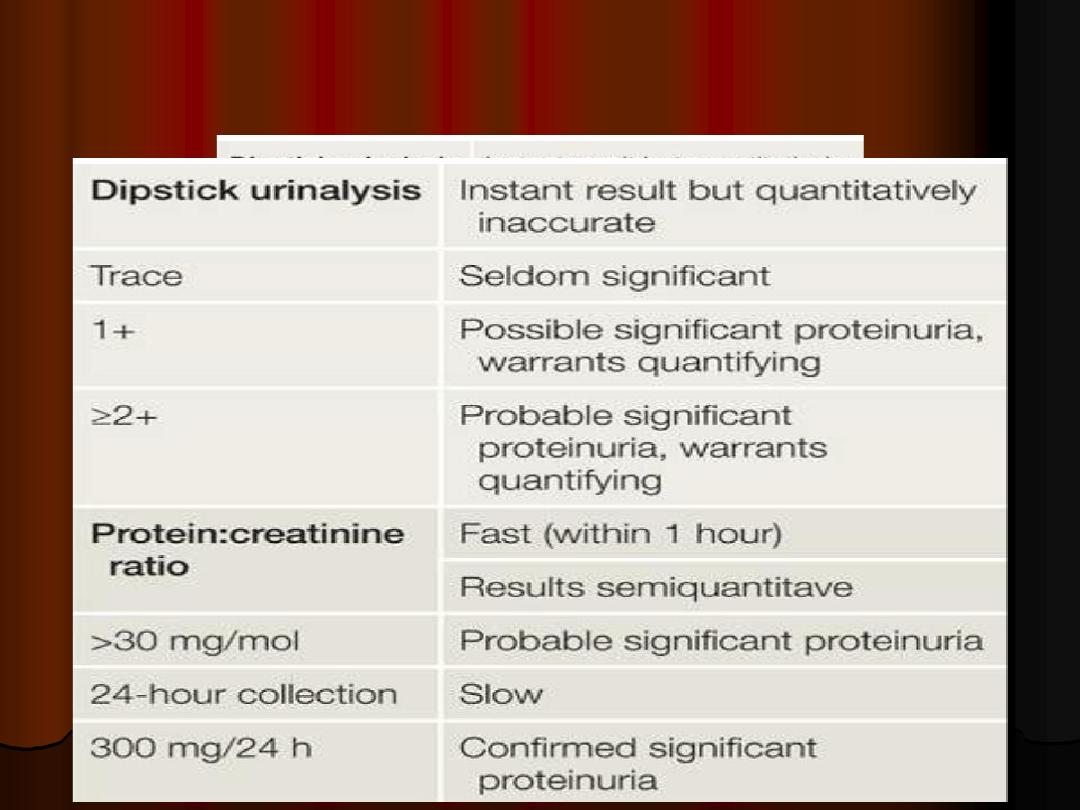
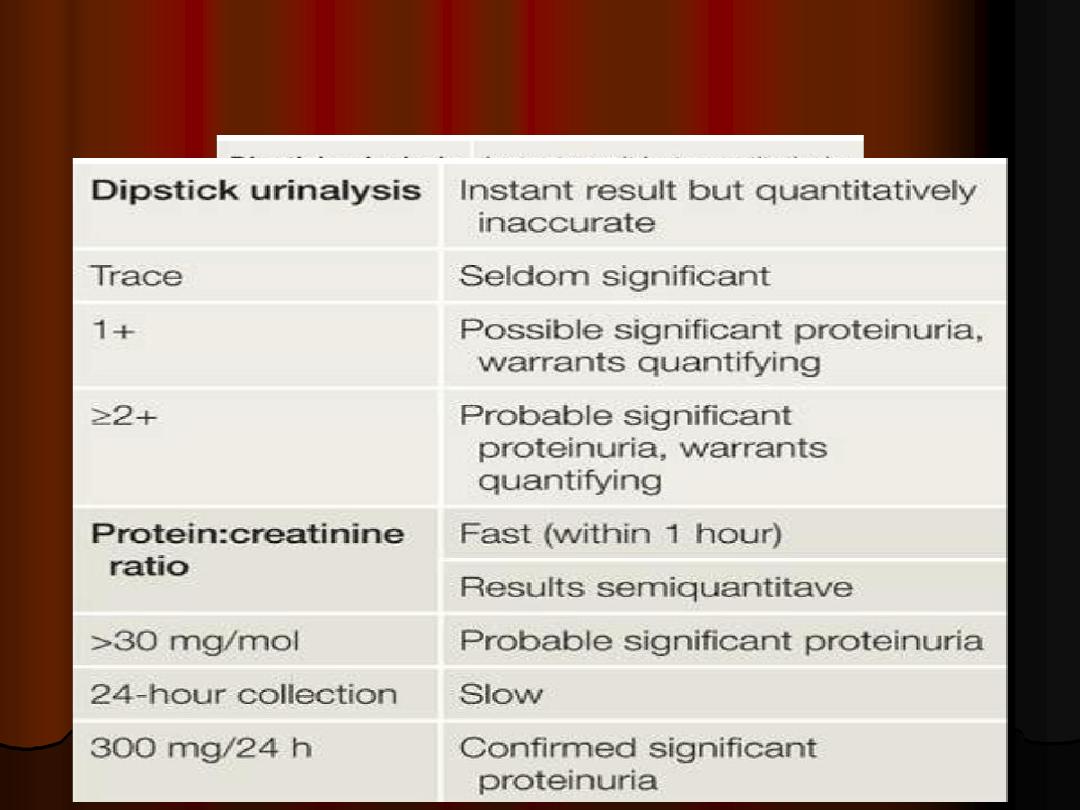
proteinuria:
One 24-h urine collection with a total protein
excretion of 300 mg or more; or
Two random clean-catch urine specimen with a
1+ or more on reagent strip
If dipstick screening is positive (1+ or more), use
albumin:creatinine ratio or protein:creatinine
ratio to quantify proteinuria in pregnant women.
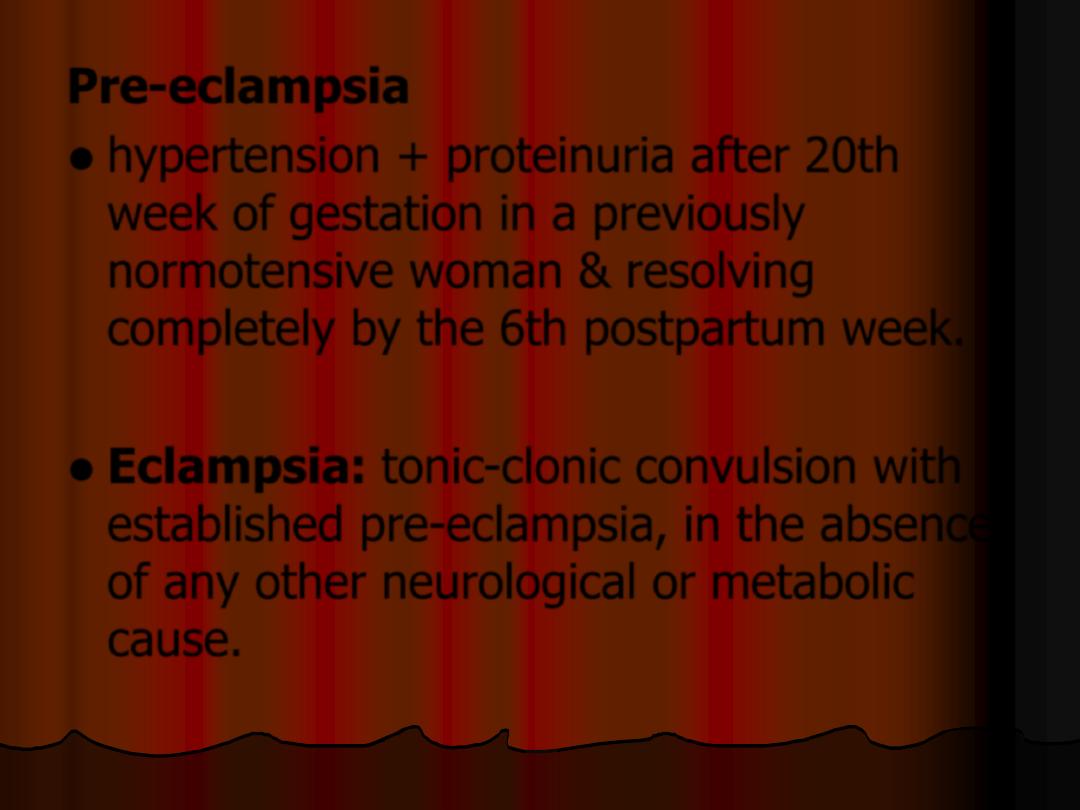
Pre-eclampsia
hypertension + proteinuria after 20th
week of gestation in a previously
normotensive woman & resolving
completely by the 6th postpartum week.
Eclampsia: tonic-clonic convulsion with
established pre-eclampsia, in the absence
of any other neurological or metabolic
cause.
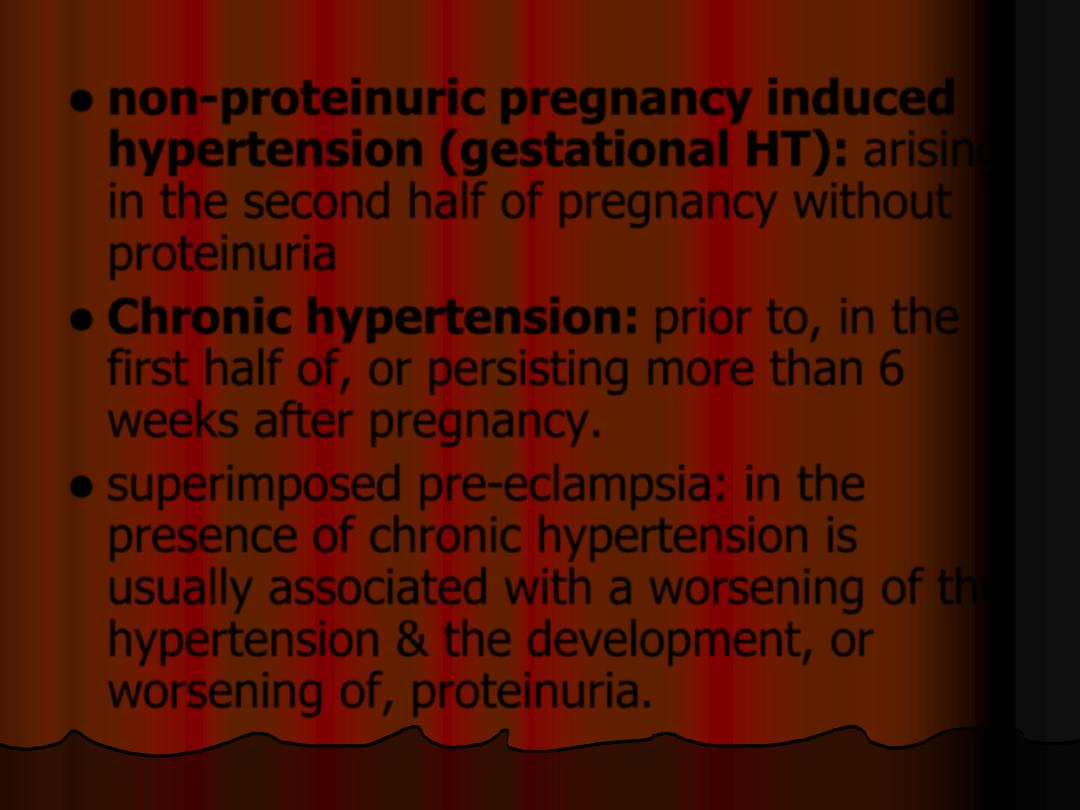
non-proteinuric pregnancy induced
hypertension (gestational HT): arising
in the second half of pregnancy without
proteinuria
Chronic hypertension: prior to, in the
first half of, or persisting more than 6
weeks after pregnancy.
superimposed pre-eclampsia: in the
presence of chronic hypertension is
usually associated with a worsening of the
hypertension & the development, or
worsening of, proteinuria.
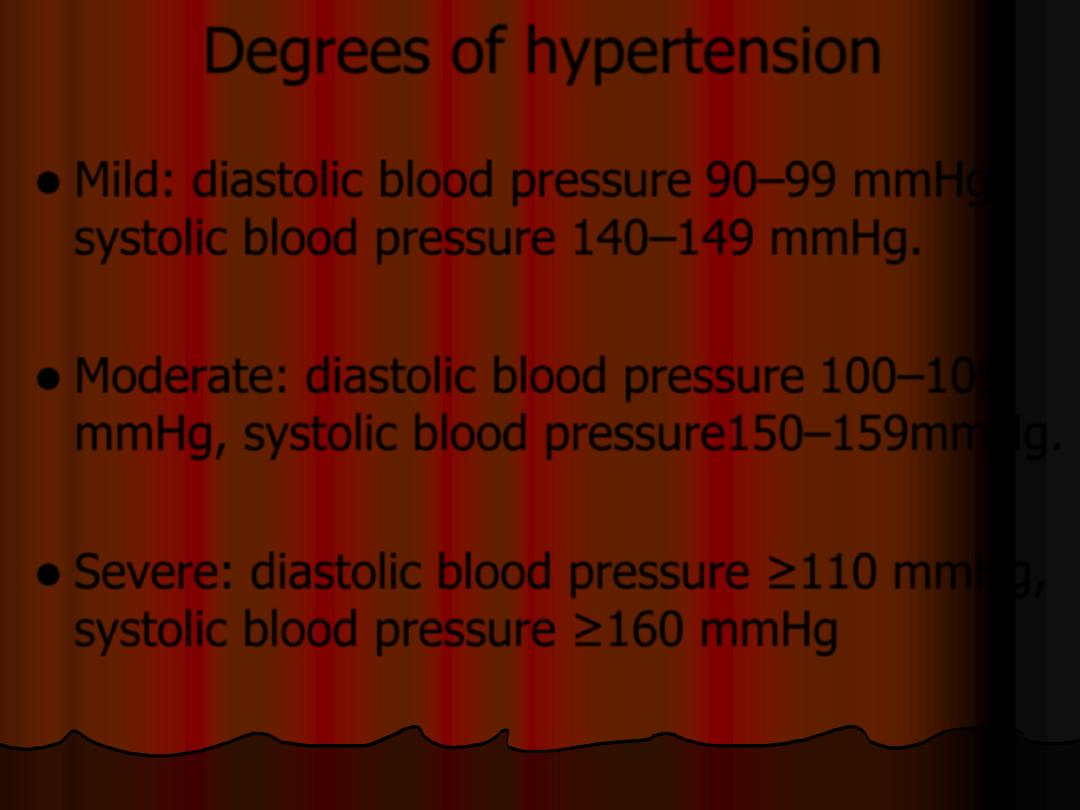
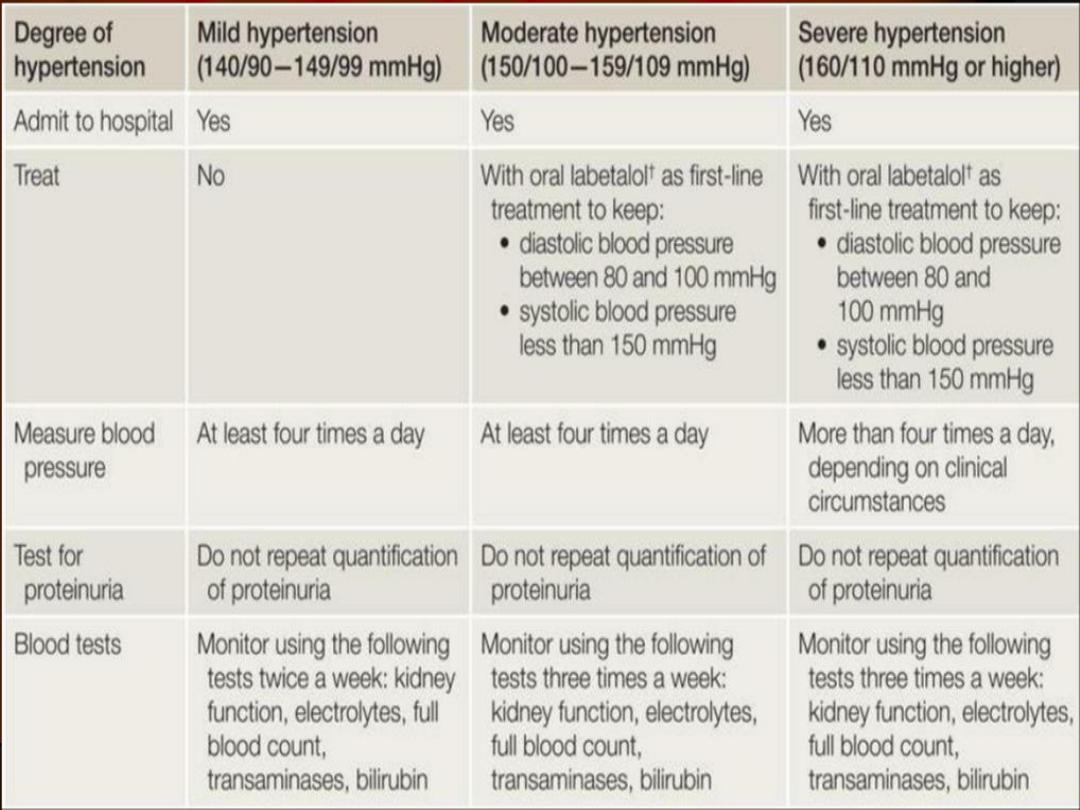
Degrees of hypertension
Mild: diastolic blood pressure 90–99 mmHg,
systolic blood pressure 140–149 mmHg.
Moderate: diastolic blood pressure 100–109
mmHg, systolic blood pressure150–159mmHg.
Severe: diastolic blood pressure ≥110 mmHg,
systolic blood pressure ≥160 mmHg
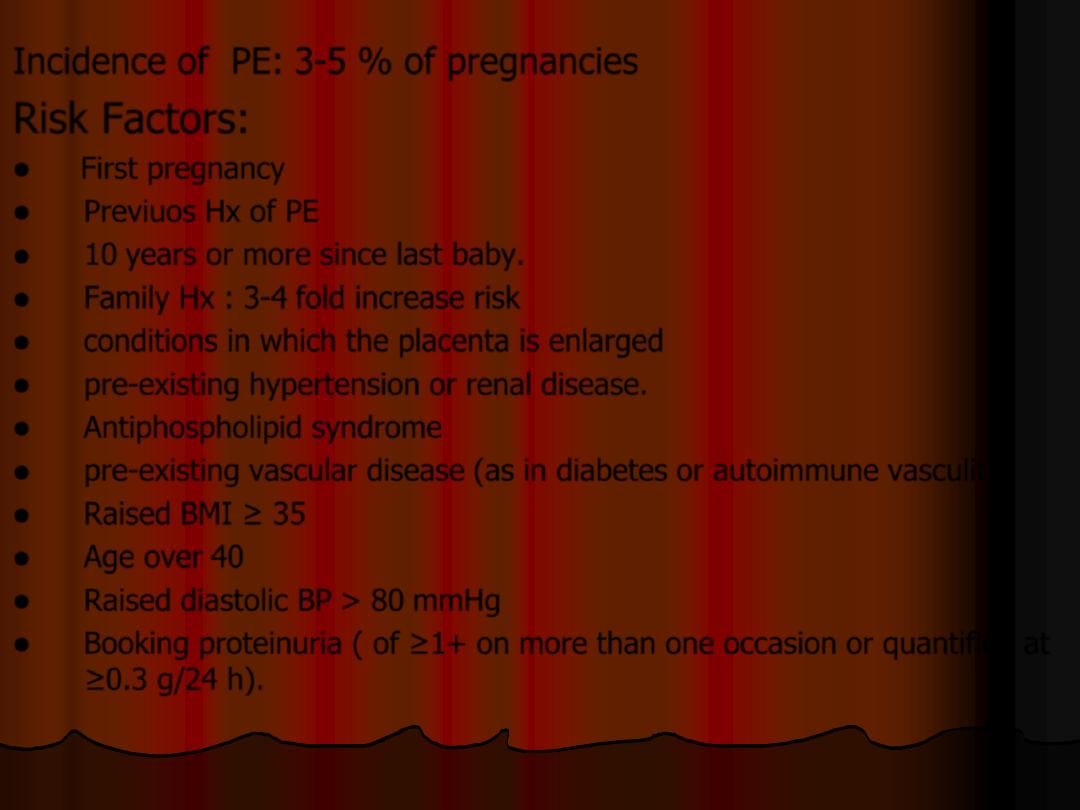
Incidence of PE: 3-5 % of pregnancies
Risk Factors:
First pregnancy
Previuos Hx of PE
10 years or more since last baby.
Family Hx : 3-4 fold increase risk
conditions in which the placenta is enlarged
pre-existing hypertension or renal disease.
Antiphospholipid syndrome
pre-existing vascular disease (as in diabetes or autoimmune vasculitis
Raised BMI ≥ 35
Age over 40
Raised diastolic BP > 80 mmHg
Booking proteinuria ( of ≥1+ on more than one occasion or quantified at
≥0.3 g/24 h).
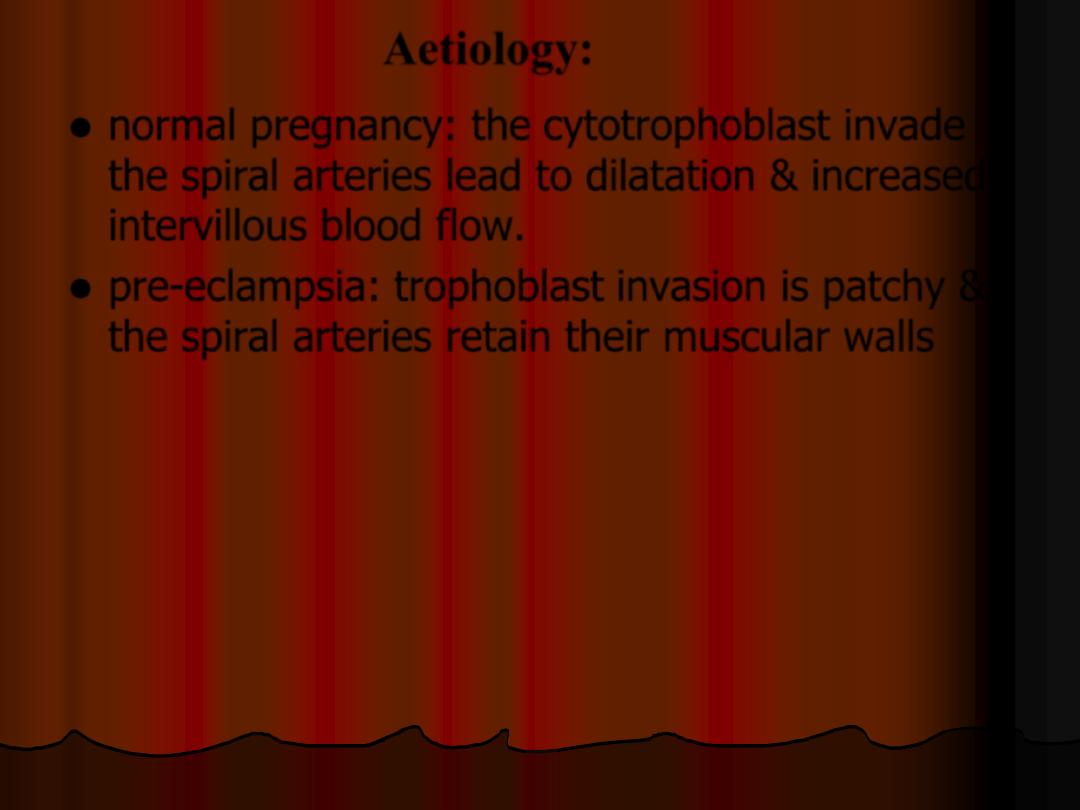
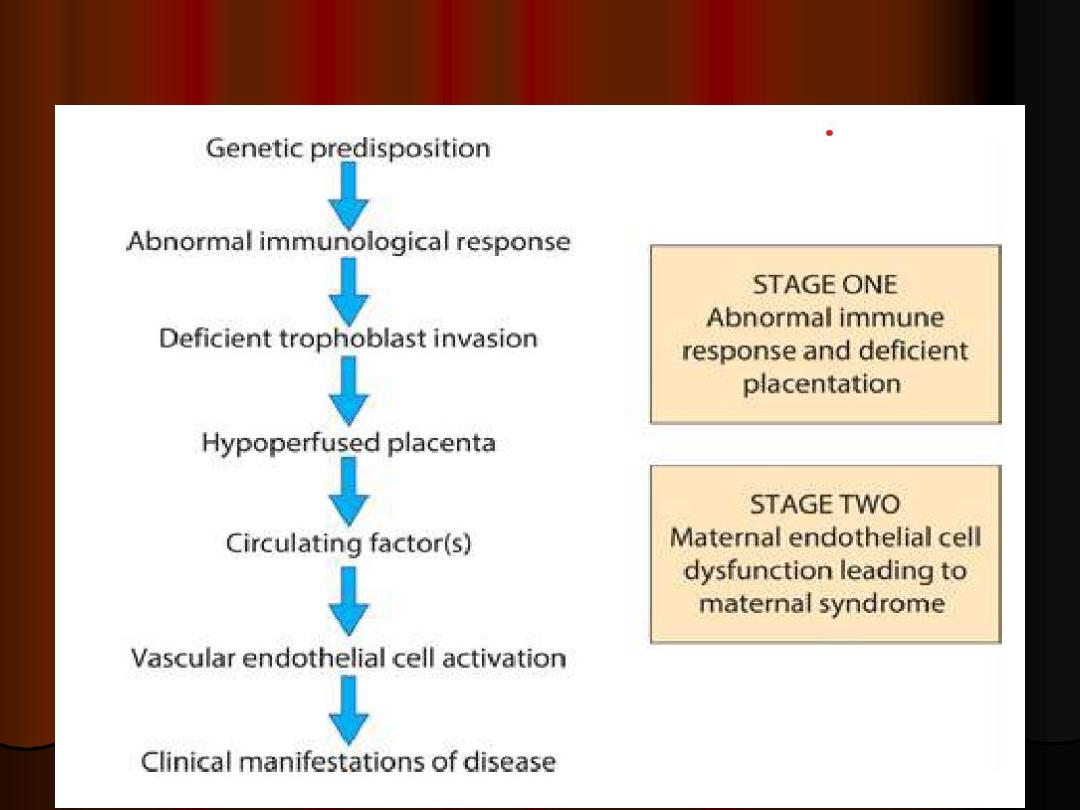
Aetiology:
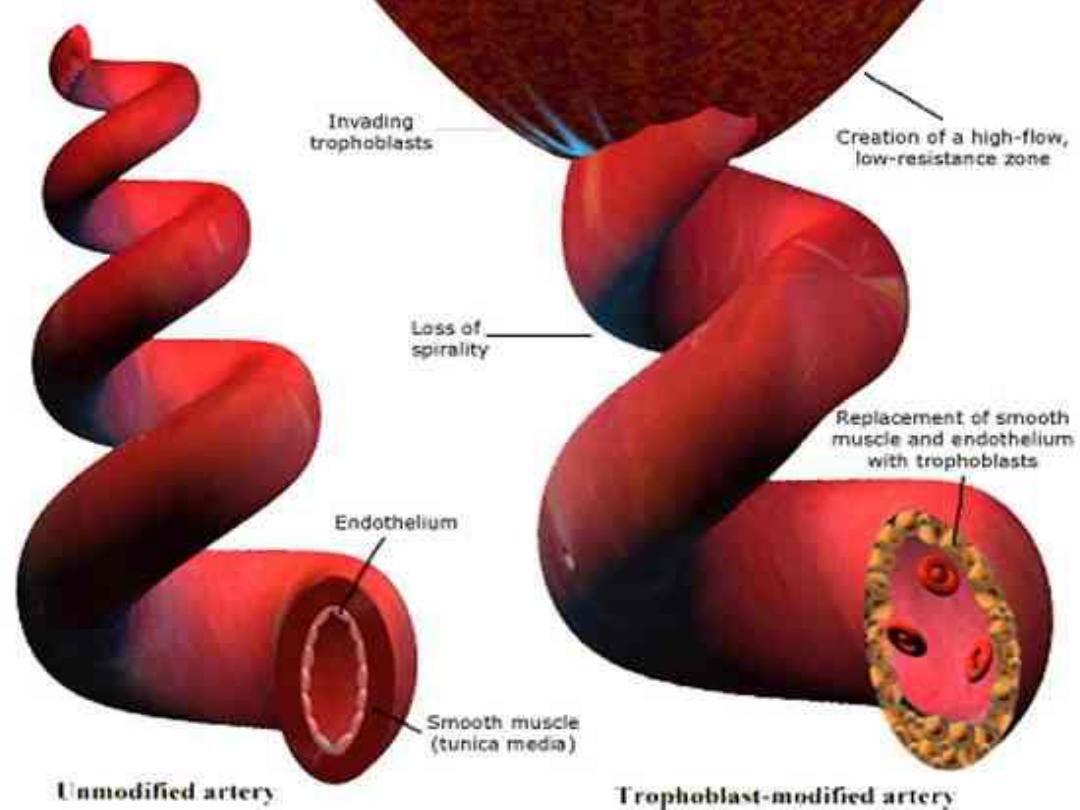
normal pregnancy: the cytotrophoblast invade
the spiral arteries lead to dilatation & increased
intervillous blood flow.
pre-eclampsia: trophoblast invasion is patchy &
the spiral arteries retain their muscular walls
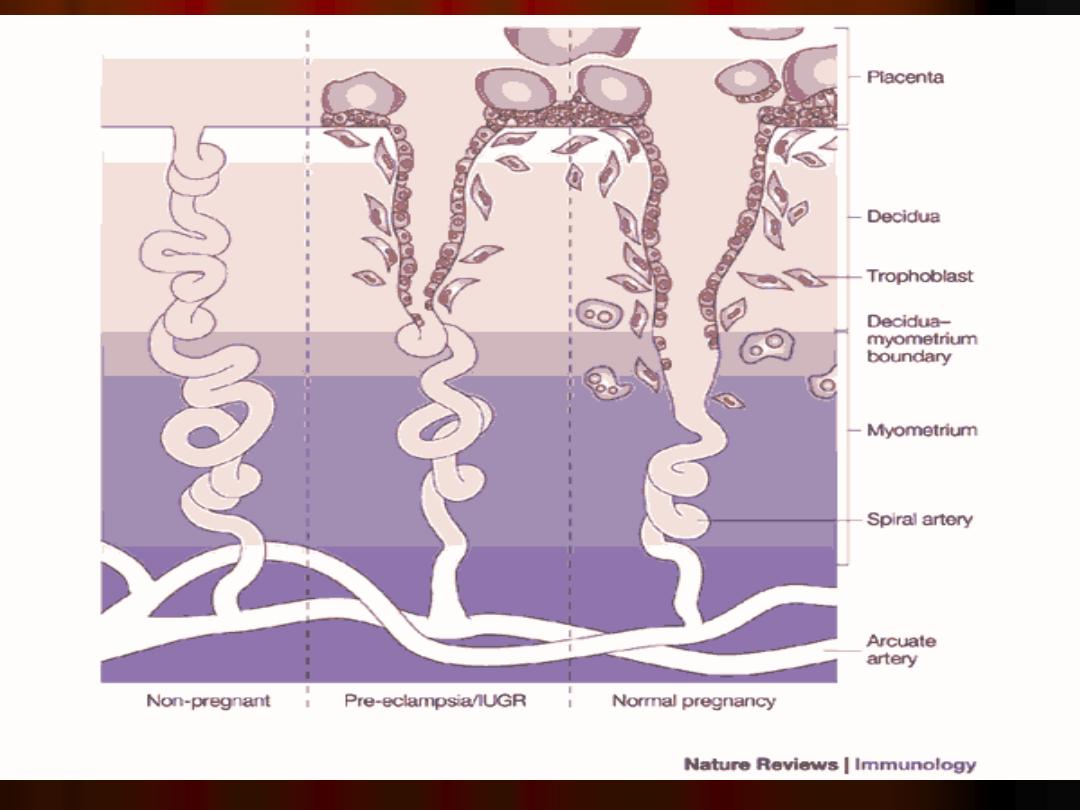
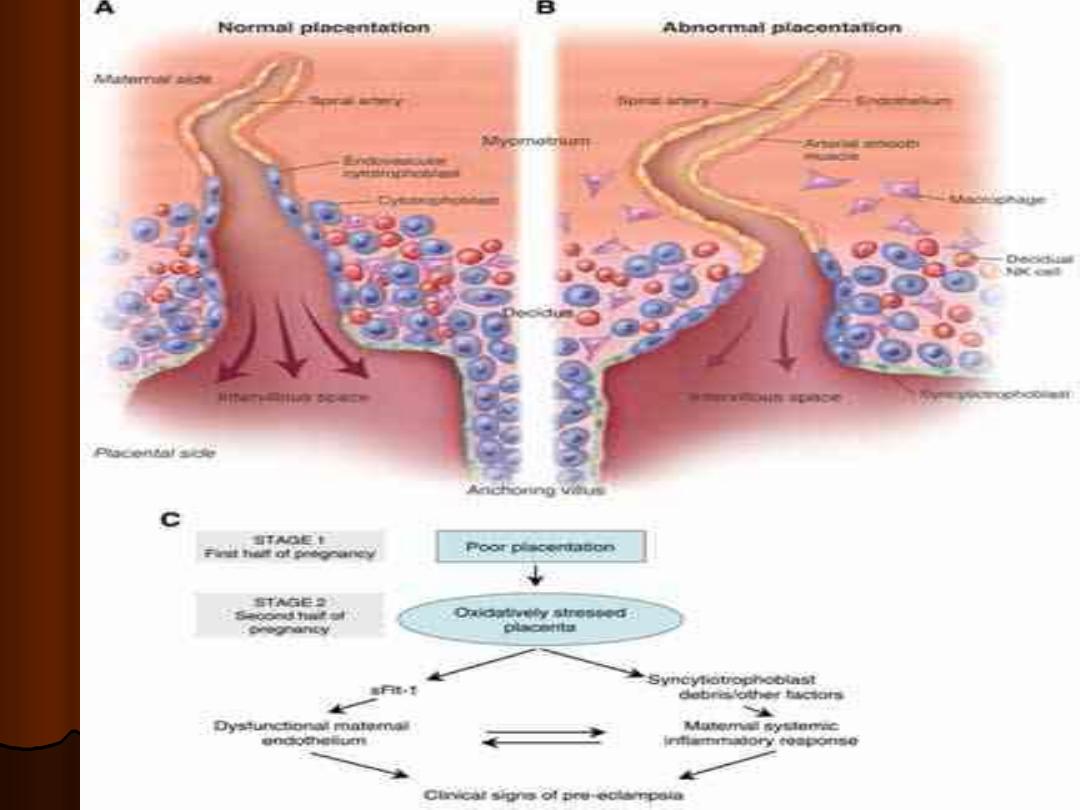
Impaired perfusion of placenta &
ischaemia result in production of reactive
oxygen species & a condition of oxidative
stress
Placenta release certain factors (adhesion
molecules, von-Willebrand factor) into the
maternal circulation which target the
vascular endothelium & cause dysfunction.
Normal pregnancy:
peripheral vasodilatation is accomplished
through a reduced vascular sensitivity to
vasoconstrictors such as angiotensin.
In pre-eclampsia the insensitivity to
vasoconstrictors is lost.
Vasospasm & endothelial cell dysfunction,
with subsequent platelet activation &
micro-aggregate formation.
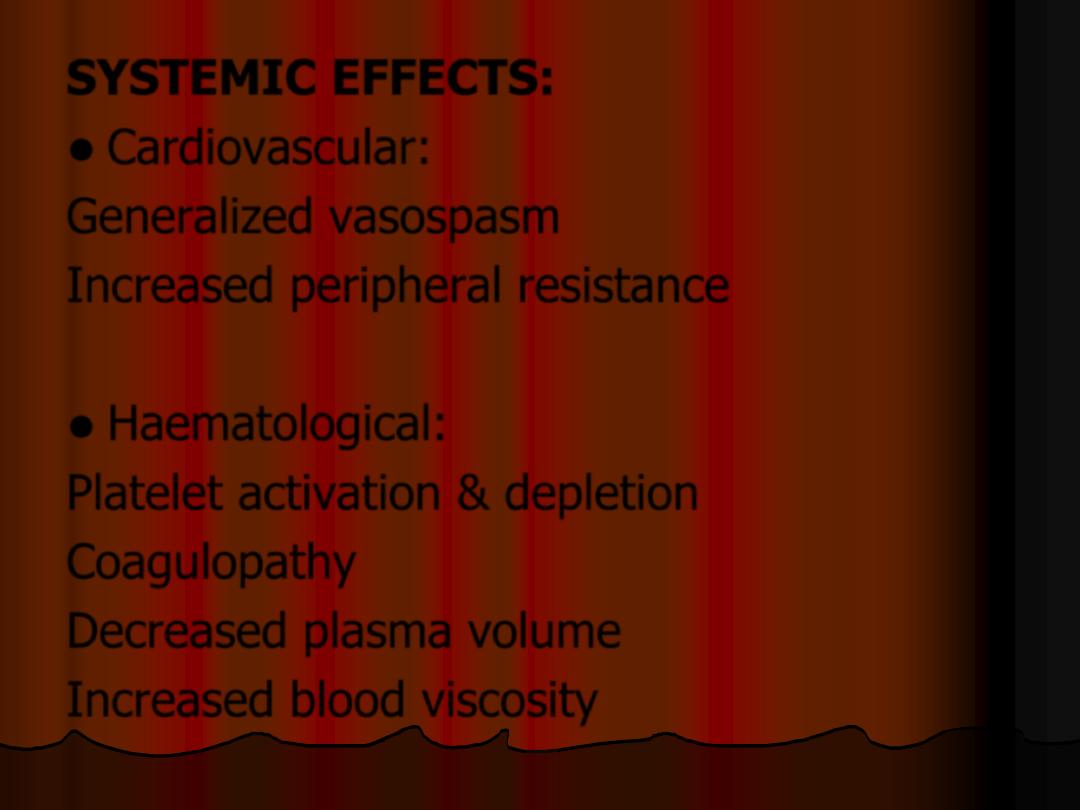
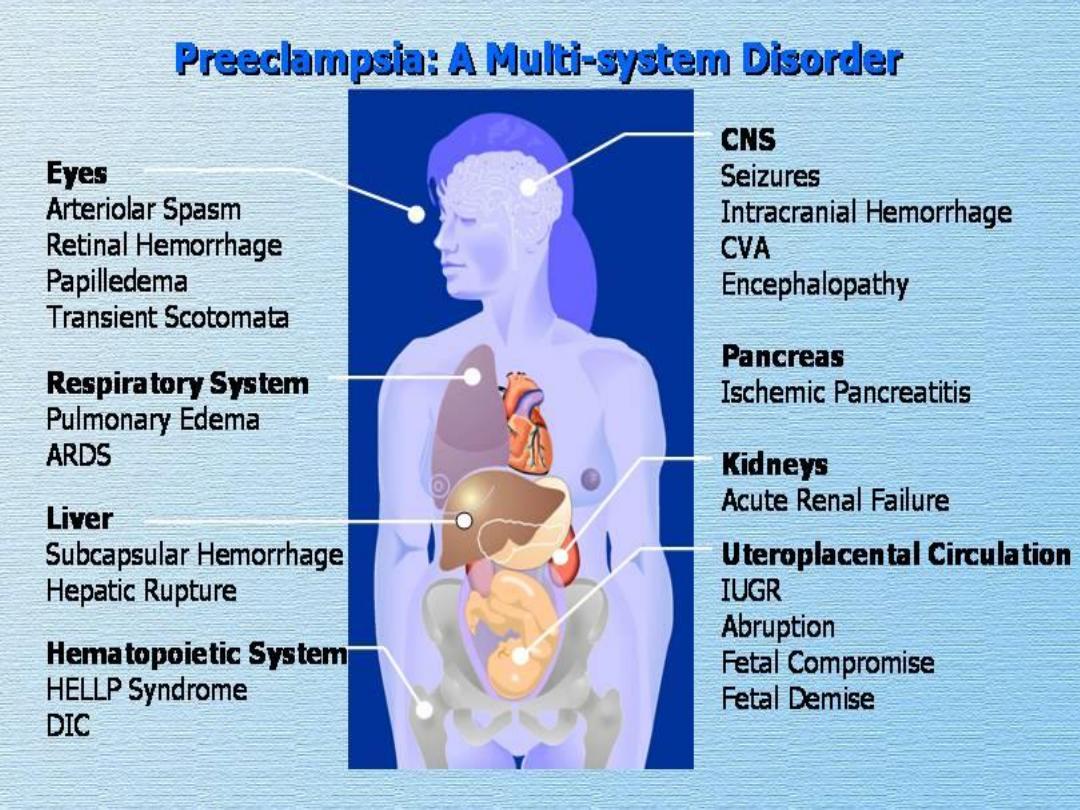
SYSTEMIC EFFECTS:
Cardiovascular:
Generalized vasospasm
Increased peripheral resistance
Haematological:
Platelet activation & depletion
Coagulopathy
Decreased plasma volume
Increased blood viscosity
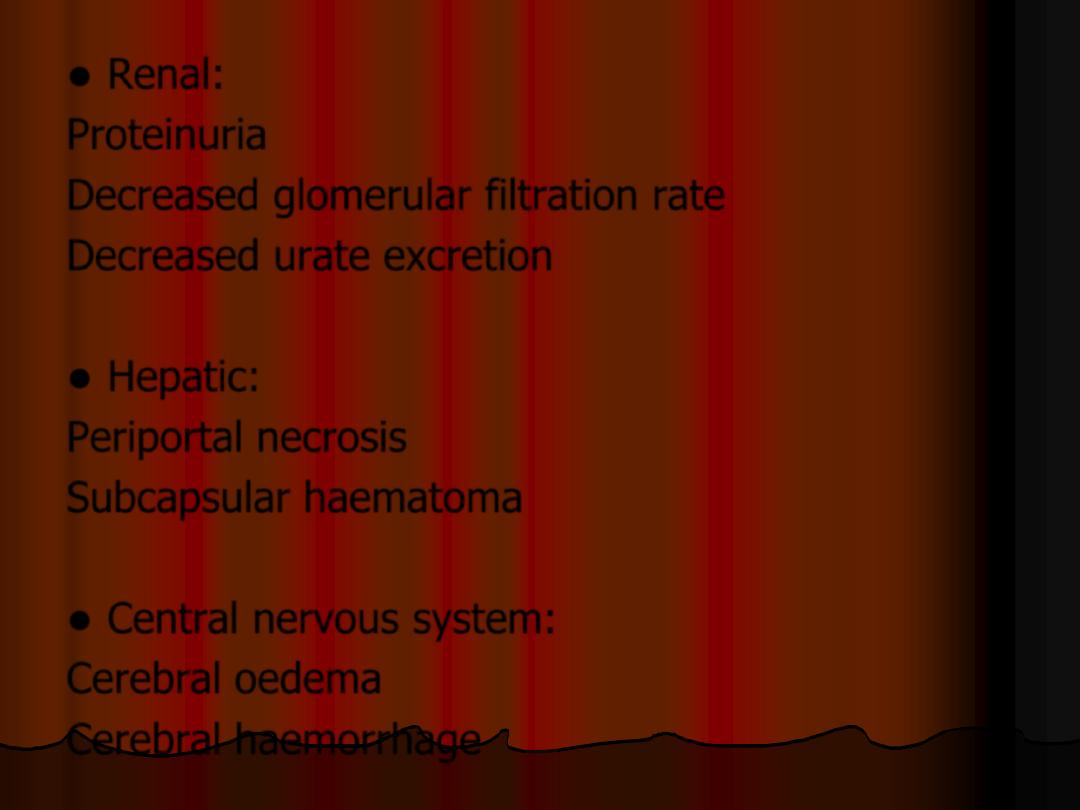
Renal:
Proteinuria
Decreased glomerular filtration rate
Decreased urate excretion
Hepatic:
Periportal necrosis
Subcapsular haematoma
Central nervous system:
Cerebral oedema
Cerebral haemorrhage
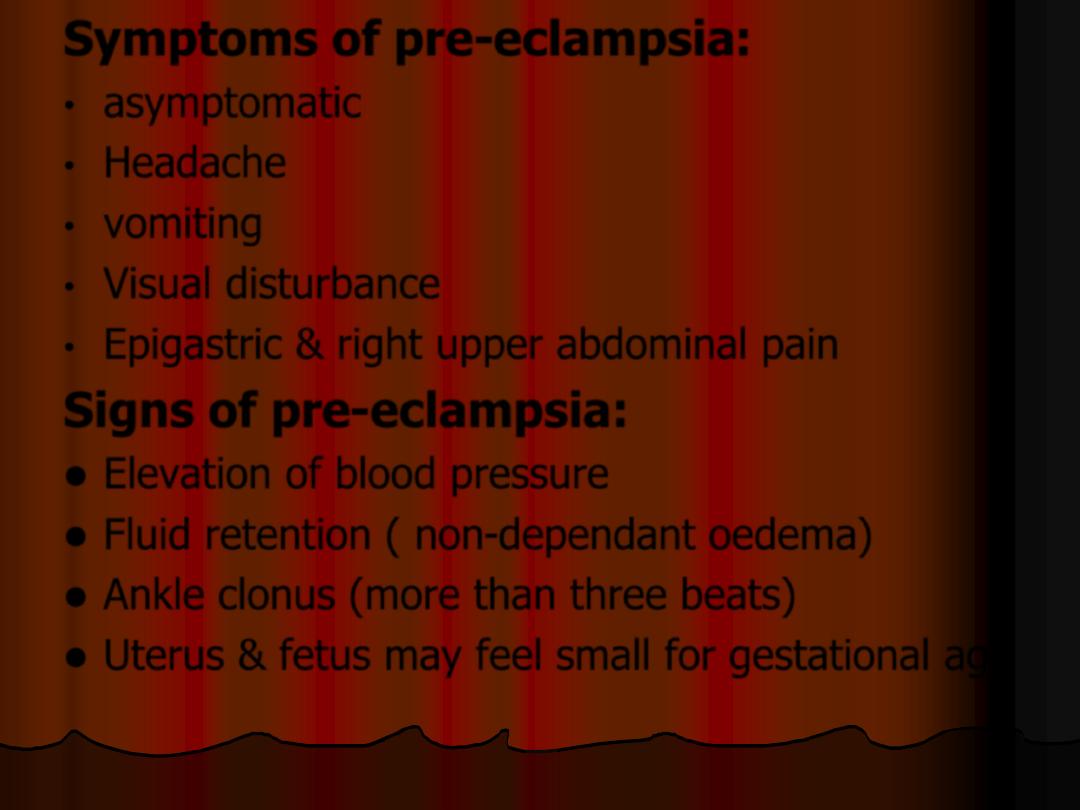
Symptoms of pre-eclampsia:
•
asymptomatic
•
Headache
•
vomiting
•
Visual disturbance
•
Epigastric & right upper abdominal pain
Signs of pre-eclampsia:
Elevation of blood pressure
Fluid retention ( non-dependant oedema)
Ankle clonus (more than three beats)
Uterus & fetus may feel small for gestational age
Prevention:
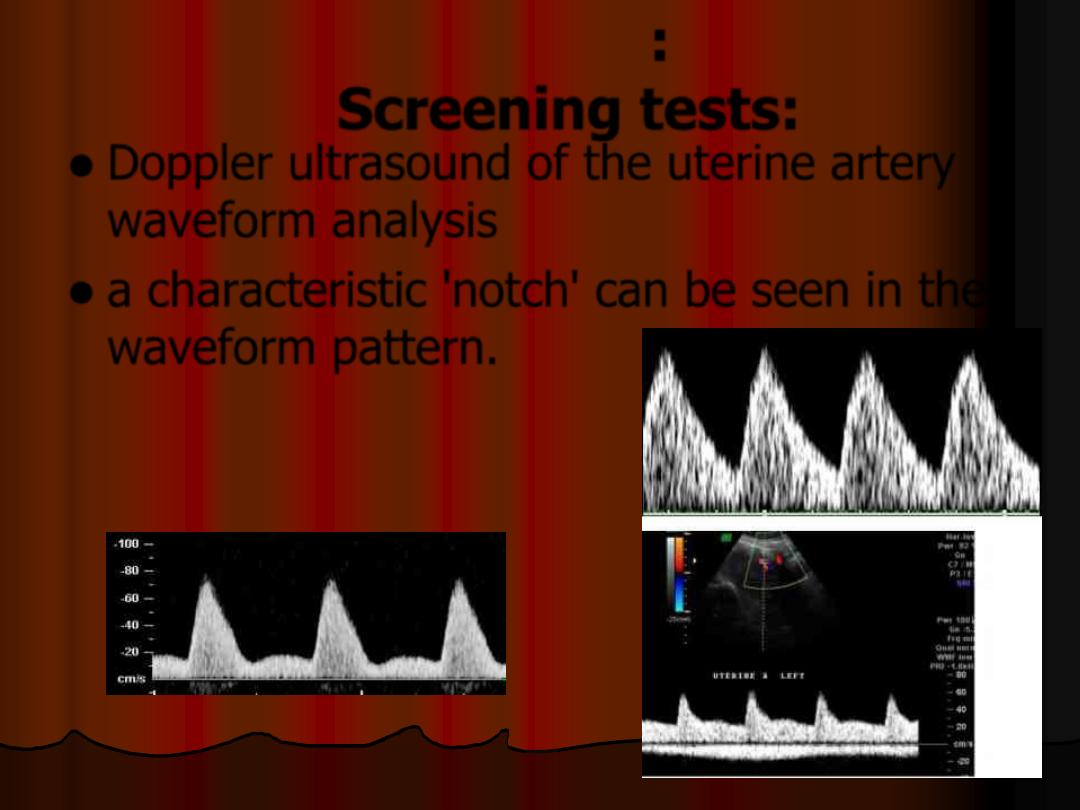
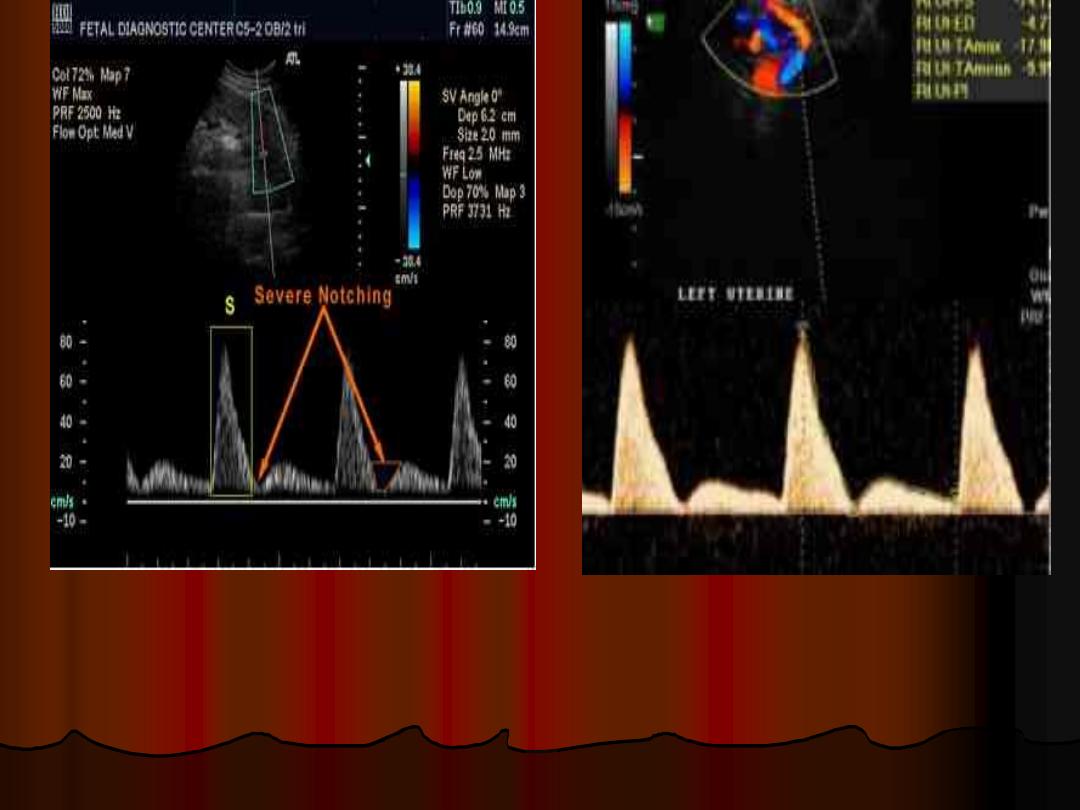
Screening tests:
Doppler ultrasound of the uterine artery
waveform analysis
a characteristic 'notch' can be seen in the
waveform pattern.
Prevention of PE
Advise pregnant women at high risk of
pre-eclampsia to take 75–150 mg of
aspirin[1] daily from 12 weeks until the
birth of the baby. (NICE guidelines 2019)
..\..\..\..\Downloads\hypertension-in-
pregnancy-diagnosis-and-management-
calcium supplementation may also reduce
risk, but only in women with low dietary
intake.
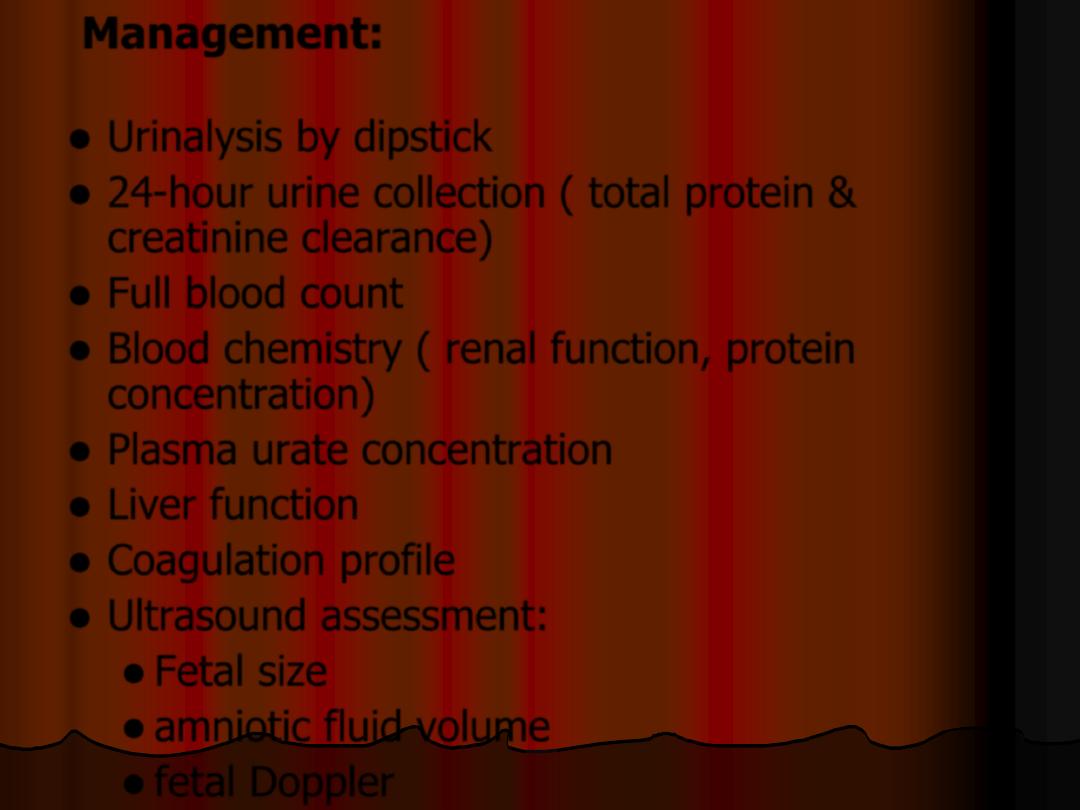
Management:
Assess severity
Urinalysis by dipstick
24-hour urine collection ( total protein &
creatinine clearance)
Full blood count
Blood chemistry ( renal function, protein
concentration)
Plasma urate concentration
Liver function
Coagulation profile
Ultrasound assessment:
Fetal size
amniotic fluid volume
fetal Doppler
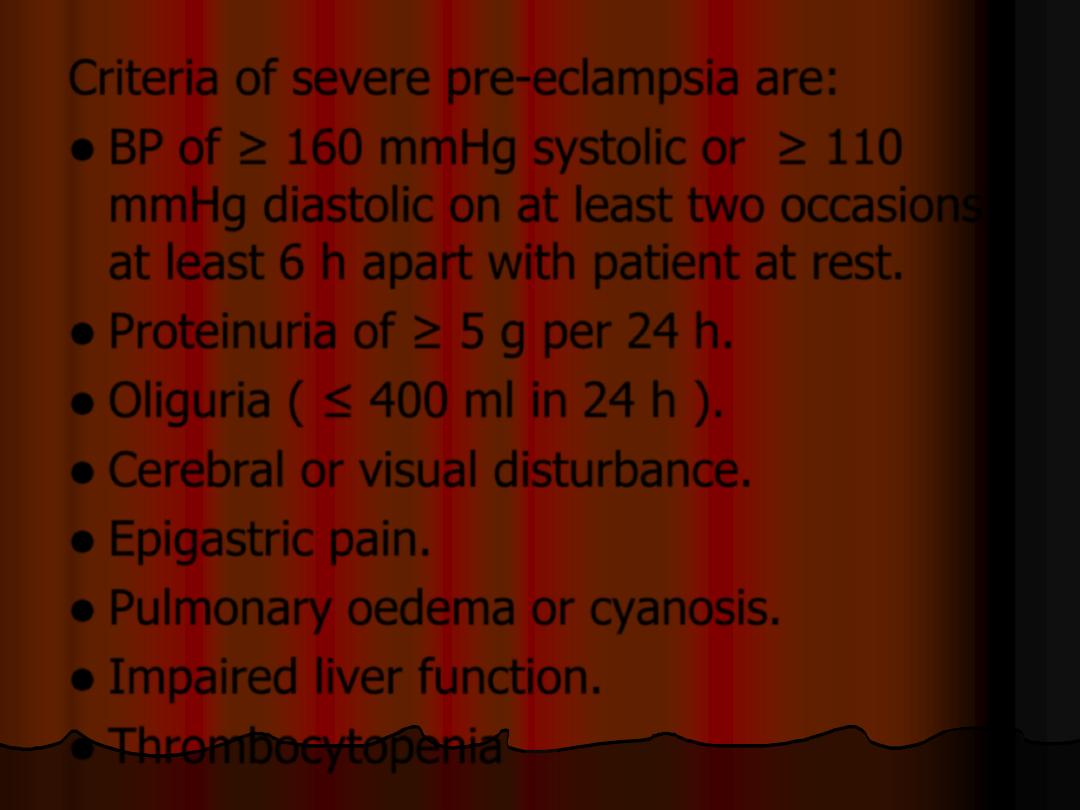
Criteria of severe pre-eclampsia are:
BP of ≥ 160 mmHg systolic or ≥ 110
mmHg diastolic on at least two occasions
at least 6 h apart with patient at rest.
Proteinuria of ≥ 5 g per 24 h.
Oliguria ( ≤ 400 ml in 24 h ).
Cerebral or visual disturbance.
Epigastric pain.
Pulmonary oedema or cyanosis.
Impaired liver function.
Thrombocytopenia
The mainstay of treatment of PE is by
termination of pregnancy by delivering the fetus
& the placenta.
For those who are remote from term :
Corticosteroids are administered to accelerate
lung maturity for fetuses between 24 and 34
weeks gestation
Antihypertensives: for those with diastolic
BP ≥100 & systolic ≥150
The aim of antihypertensive therapy is to
lower blood pressure & reduce the risk of
maternal cerebrovascular accident without
reducing uterine blood flow &
compromising the fetus.
Types of Antihypertensives:
Labetolol: alpha & beta- blocking agent
Methyldopa: centrally acting
antihypertensive agent, takes up to 24
hours to take effect.
Nifedipine: calcium channel blocker with a
rapid onset of action.
Hydralazine: arterial vasodilator, used in
emergency situation for rapid control.
Management of labour &
delivery
expectant management should be
continued to 37-38 weeks gestation
Indication for preterm delivery are:
severe uncontrolled hypertension ( ≥ 160/110
mmHg) despite 3 antihypertensive in
appropriate doses.
haemolysis with thrombocytopenia & elevated
ALT
progressive symptoms (headache, visual
disturbance, epigastric pain)
maternal pulse oximetry less than 90%
pulmonary oedema
renal compromise with oliguria
eclampsia
fetal distress
The mode of delivery is determined by
gestational age, the state of the cervix &
fetal condition
Prolonged pushing should be avoided
ergometrine should not be used
Fluid management is important in severe
PE: 1 litre Ringer lactate / 12 h).
diuretics should be confined to women
with pulmonary oedema
After delivery BP monitoring is needed
antihypertensive medication if BP still
elevated
Protienuria, S.creatinine & transaminases
monitoring if initially were abnormal.
Postnatal councelling
The risk of recurrence is increased with
increased severity of PE.
increased risk of death from
cardiovascular disease in the future
particularly in those who remain
hypertensive in the puerperium.
