
Part I : Complications of Severe Pre-
eclampsia
Part II : Chronic Hypertension in
Pregnancy
Dr.Nadia Mudher Al-Hilli
FICOG
Department of Obs&Gyn
College of Medicine
University of babylon

Objectives of this lecture
• Learn the complicatios that might develop in a
patient with severe PE & how to deal with
them
• How to deal with a patient with eclamptic fit
• Understand the risk & complications of
chronic HT in pregnancy
• Managing chronic HT in pregnancy
Complications of Preeclampsia

Complication of severe pre-eclampsia are:
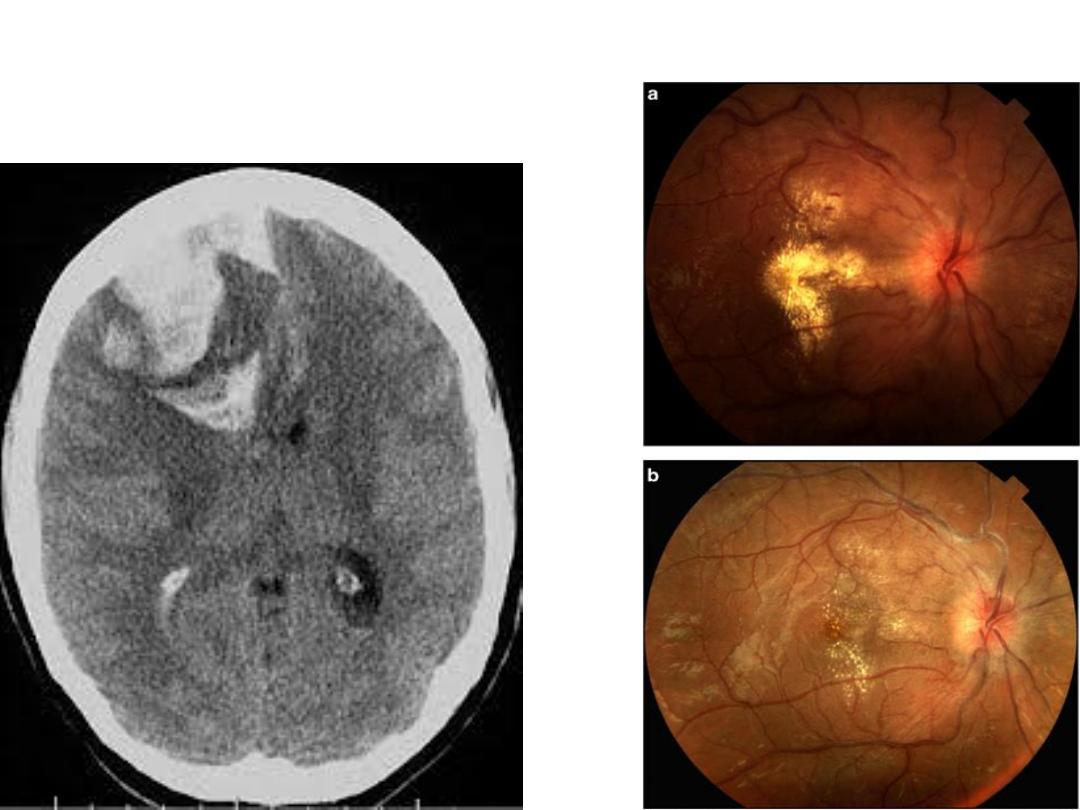
• Eclampsia
• HELLP syndrome
• DIC
• Adult Respiratory Distress Syndrome (ARDS)
• Pulmonary oedema
• Acute renal failure
• Placental abruption
• Intrauterine growth restriction (IUGR)
• Intrauterine fetal death
Eclampsia:
• defined as new-onset
an otherwise healthy woman
with hypertensive disorder of pregnancy
• 44% occur postnatally, 38% antepartum &
18% intrapartum.
• The pathophysiology
•is associated with high maternal and neonatal
morbidity and mortality.


Management:
• General measures:
• Do not leave the patient alone
• Call for help
• Inform consultant
• Prevent maternal injury during
convulsion
–Air way:
–Breathing:
–Circulation:
–Secure intravenous access
–Urinary catheter to assess urinary
out put
–Fluid input/output chart &
monitoring of BP every 15-30 min
and other vital signs

anticonvulsant therapy
• Magnesium sulphate:
membrane stabilizer &
vasodilator & reduces intracerebral ischaemia
• Loading dose 4gm bolus iv over 15-20 min followed
by continuous infusion of 1gm/hr for 24 hrs fron last
fit or from delivery
signs of magnesium toxicity
• loss of deep tendon reflexes
• respiratory depression
• cardiac standstill.
• So, the patient should be monitored hourly by
patellar reflex, respiratory rate & oxygen saturation.
& urine output

Mg sulphate indications in severe PE
• Consider the need for magnesium sulfate treatment, if
1 or more of the following features of severe pre-
eclampsia is present :
• ongoing or recurring severe headaches
• visual scotomata
• nausea or vomiting
• epigastric pain
• oliguria and severe hypertension
• progressive deterioration in laboratory blood tests
(such as rising creatinine or liver transaminases, or
falling platelet count).

• Blood pressure
should be controlled using
intravenous hydralazin or labetolol
• limit maintenance fluids to 80 ml/hour unless there
are other ongoing fluid losses (for example,
haemorrhage)
• Delivery
: Choose mode of birth according to the
clinical circumstances and the woman's preference.
• Postpartum care
: should be in critical care setting
• Transfusion
of red cells, platelets, fresh frozen
plasma and cryoprecipitate or fibrinogen
concentrate are required as indicated clinically and
by blood and coagulation tests.

• HELLP Syndrome: the association of
haemolysis (H) elevated liver enzymes (EL) &
low platelet count ( LP)
• DIC with low fibrinogen may coexist.

• Definitive treatment of severe pre-eclampsia
and HELLP requires delivery of the fetus
• Give antenatal corticosteroid for fetal lung
maturation.

Chronic Hypertension:
• Effect 2-4 % of pregnant women. Over 90% of cases
are due to essential hypertension
• causes of chronic hypertension ( secondary) include:
• Chronic renal disease
• Renal artery stenosis
• Coarctation of the aorta
• Collagen vascular disease
• Pheochromocytoma
• Cushing's syndrome
• Conn's syndrome (primary hyperaldosteronism)

High-risk characteristics in women with CHT include:
• Maternal age >40 years
• Duration of hypertension > 15 years
• BP ≥160/110 mmHg
• Diabetes
• Renal disease
• Cardiomyopathy
• Connective tissue disease
• Coarctation of the aorta
• Previous pregnancy with perinatal loss

Preconception assessment & councelling:
• life style modification
• anti-hypertensive therapy:
• Physical examination
• Investigations:
renal function test,
urinalysis,
24 h urine collection for protein excretion
creatinine clearance
CXR
ECG
echocardiography

Complications of CHT in pregnancy:
• Superimposed PE
• Abruptio placentae
Antihypertensive therapy: reduces the risk of severe
hypertension but does not reduce the risk of
superimposed PE, preterm delivery or perinatal death
• diuretics decrease blood volume & cause undesirable
physiological effect, congenital anomalies & neonatal
complications.
• beta-blockers cause IUGR
• ACE inhibitors & angiotensin receptor blockers cause
renal toxicity & increased risk of congenital abnormalities
in the fetus & should be changed

Treatment of chronic hypertension
Offer pregnant women with chronic
hypertension advice on:
• weight management
• exercise
• healthy eating
• lowering the amount of salt in their diet.
Continue with existing antihypertensive treatment if safe in
pregnancy, or switch to an alternative treatment, unless:
• sustained systolic blood pressure is less than 110 mmHg or
• sustained diastolic blood pressure is less than 70 mmHg or
• the woman has symptomatic hypotension.
• Offer antihypertensive treatment to pregnant women who have
chronic hypertension and who are not already on treatment if they
have:
• sustained systolic blood pressure of 140 mmHg or higher or
• sustained diastolic blood pressure of 90 mmHg or higher.
• When using medicines to treat hypertension in pregnancy, aim for
a target blood pressure of 135/85 mmHg . (NICE Guigelines 2019)

• Consider labetalol to treat chronic hypertension in pregnant
women.
• Consider nifedipine for women in whom labetalol is not
suitable, or methyldopa if both labetalol and nifedipine are
not suitable.
• Offer pregnant women with chronic hypertension aspirin 75–
150 mg once daily from 12 weeks.
• Offer placental growth factor (PlGF)-based testing to help rule
out pre-eclampsia between 20 weeks and up to 35 weeks of
pregnancy, if women with chronic hypertension are suspected
of developing pre-eclampsia.

Fetal monitoring in chronic
hypertension:
• carry out an ultrasound for fetal growth and
amniotic fluid volume assessment, and
umbilical artery doppler velocimetry at 28
weeks, 32 weeks and 36 weeks.
• only carry out cardiotocography if clinically
indicated.

• For women with chronic hypertension whose
blood pressure is lower than 160/110 mmHg
deliver after 37 weeks.
• After delivery continue follow up of BP &
antihypertensive therapy as needed
