
BACTERIAL MENINGITIS
Dr. Ameer kadhim Hussein
M.B.Ch.B. FICMS (COM.)
Neisseria meningitidis ,Streptococcus pneumoniae and
Haemophilus influenzae (type b)
constitute more than
75% of all cases of bacterial meningitis and 90%of
bacterial meningitis in children .
The less common bacterial causes of meningitis including
staphylococci ,enteric bacteria, group B streptococci
and Listeria
which occurring in persons with specific
susceptibilities such as neonates and patients with
impaired immunity and those with head injury.
Introduction
Meningococcal meningitis or cerebrospinal fever is a
bacterial form of meningitis which is a serious infection of
the thin lining that surrounds the brain and spinal cord
. It is
an acute communicable disease caused by
N. meningitidis .
This disease characterized by headache ,vomiting ,stiff
neck and photophobia with petechial rash.
Case fatality rate exceeded 50% but with treatment it
decrease to 8% to 15% .
Meningococcal meningitis
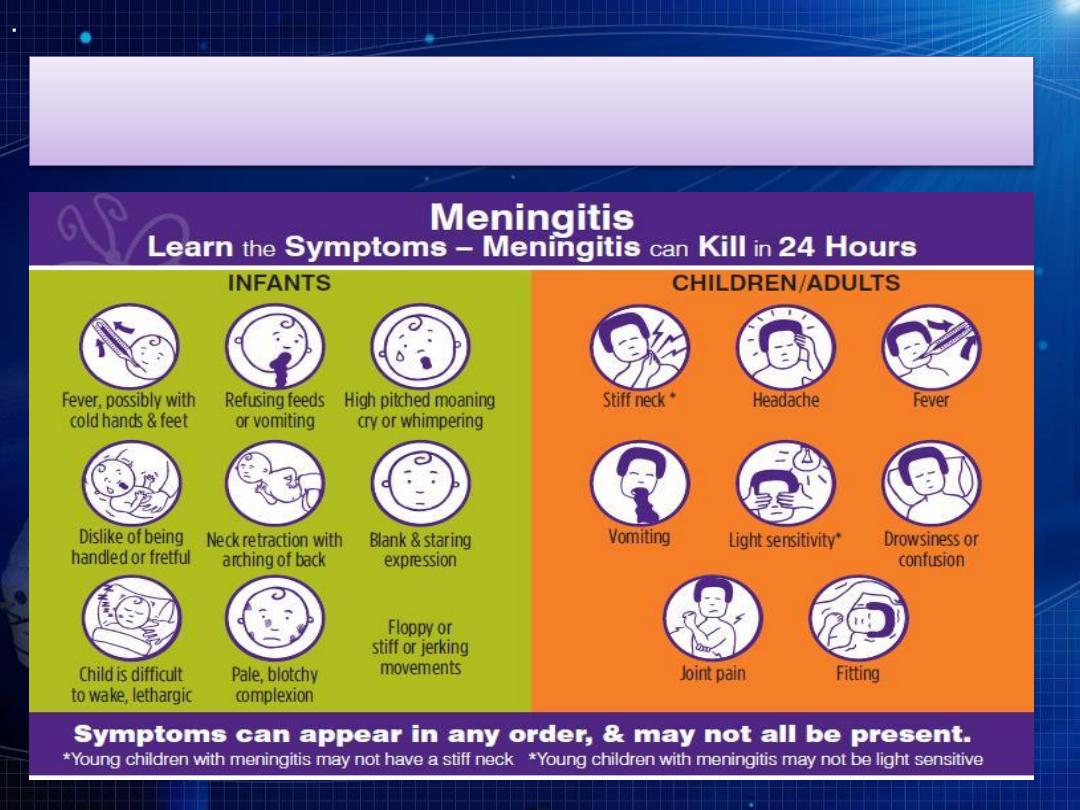
Clinical features

Clinical features
In Europe and north America the incidence is higher during
winter and spring while in Africa it is higher among dry season.
Infants have higher risk of disease and incidence decrease after
infancy but in increase in adolescence and young adults. In
some countries male affected more than female.
Immune deficiency such as asplenia, overcrowding, low socio-
economic status, exposure to tobacco and concurrent upper
respiratory tract infections increase the risk of disease.
The extended meningitis belt of sub-Saharan Africa
,
stretching from
Senegal in the west to Ethiopia in the east
(26 countries), has the highest rates of the disease.
Occurrence
In the United States, about 4,100 cases of bacterial
meningitis, including 500 deaths, occurred each year
between 2003–2007.
During the 2014 epidemic season, 19 African countries
implementing enhanced surveillance reported 11908
suspected cases including 1146 deaths, the lowest
numbers since the implementation of enhanced
surveillance through a functional network (2004). As
of June 2015, over 220 million persons aged 1 to 29
years have received meningococcal A conjugate
vaccine in 15 countries of the African belt.
Occurrence
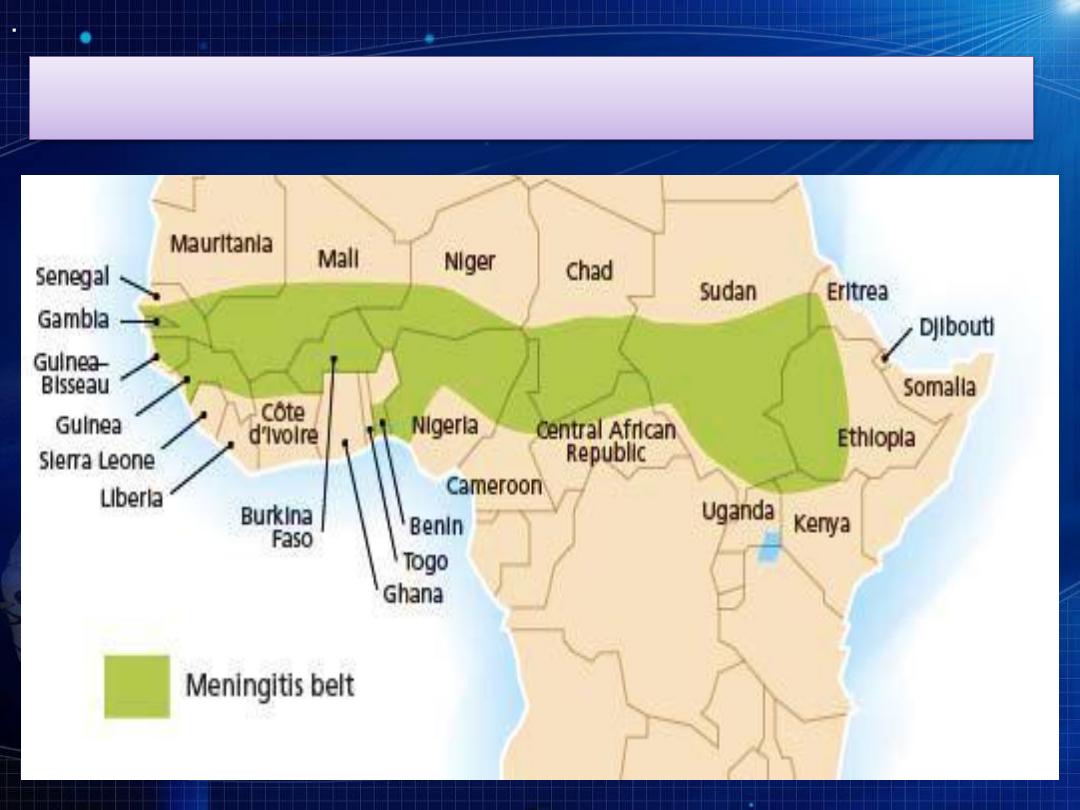
The classical meningitis belt in Africa
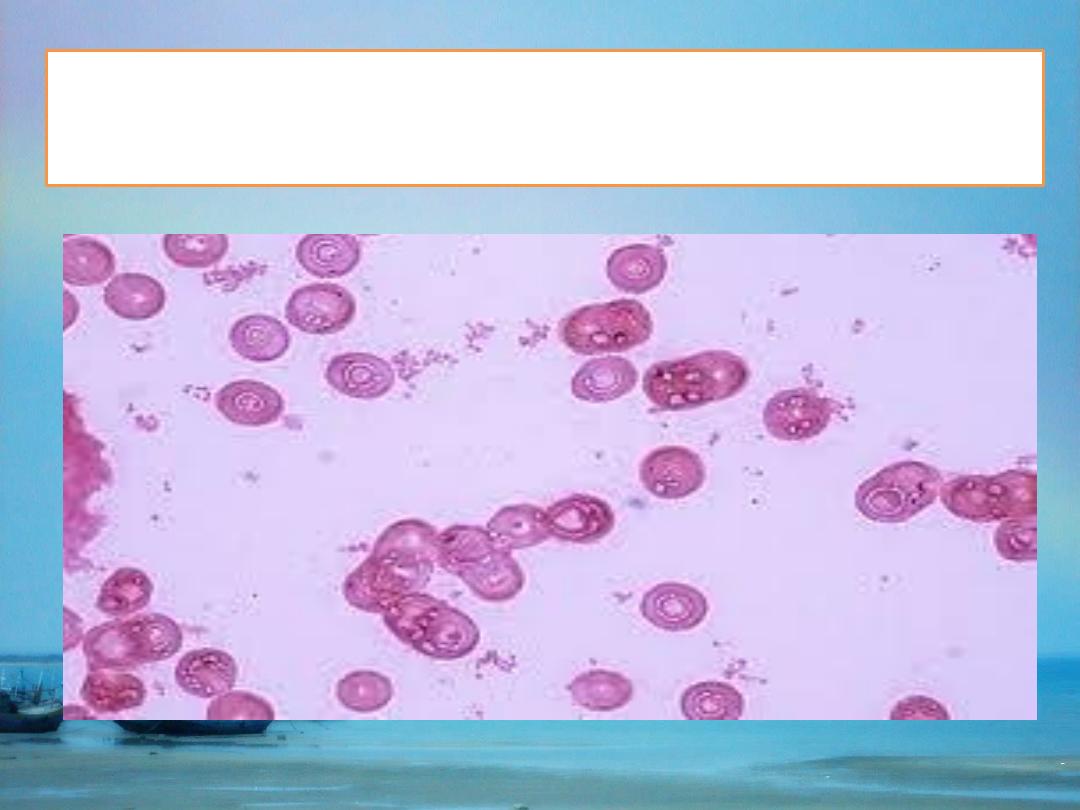
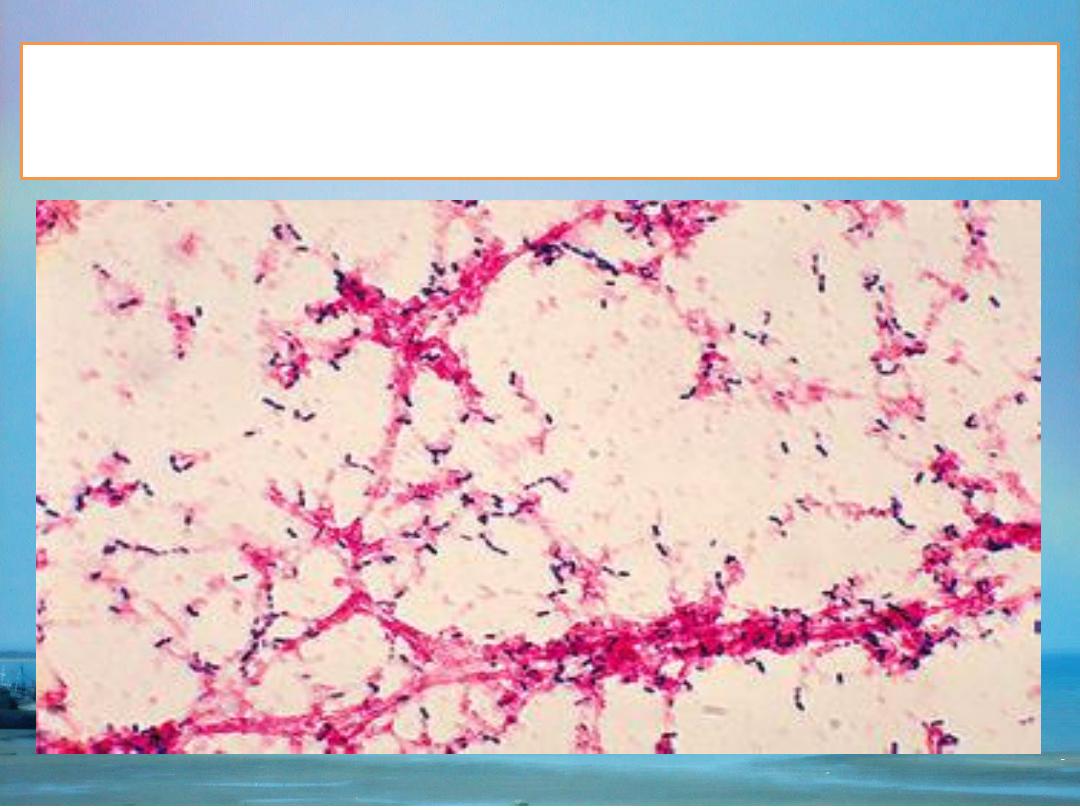
N. Meningitidis is gram negative diplococcus,
aerobic bacteria which divided into serogroups
including ( A,B, C,D,X,Y,W135, 29E..etc).
Groups
(A, B and C) account for at least 90% of cases.
Before 2010 and the mass preventive immunization
campaigns, Group A meningococcus accounted for
an estimated 80–85% of all cases in the meningitis
african belt, with epidemics occurring at intervals
of 7–14 years. Since then, the proportion of the A
serogroup has declined dramatically.
Infectious agent
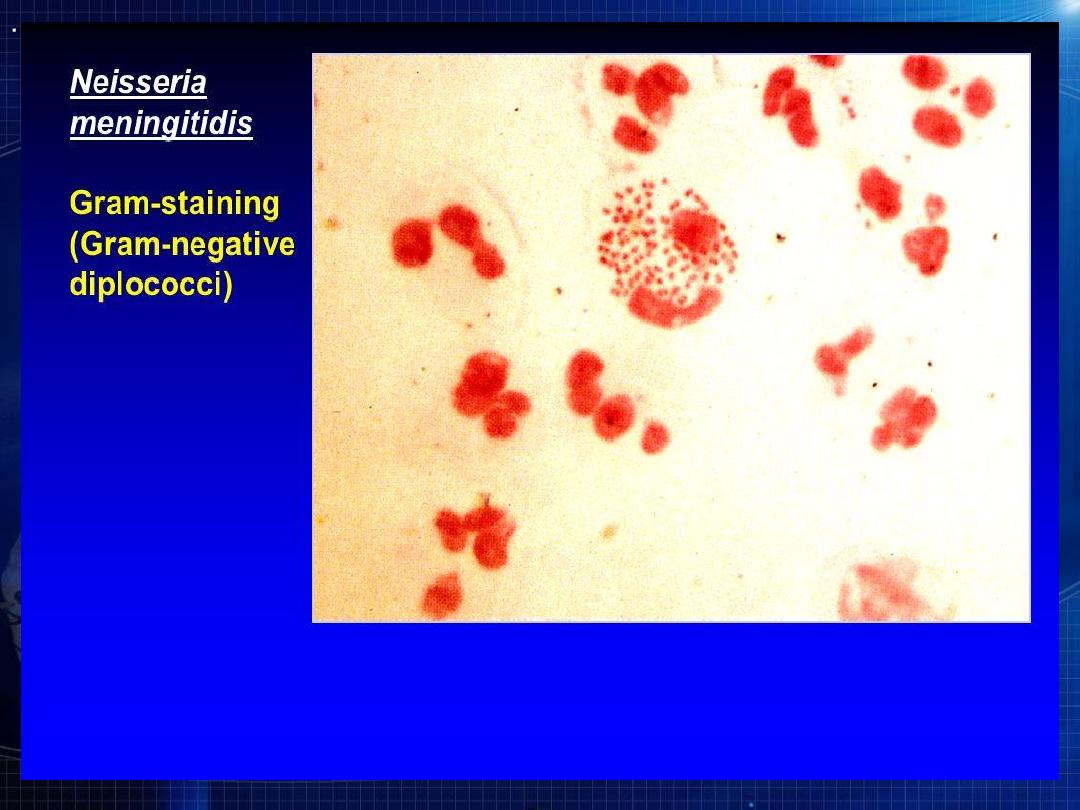

in EM
meningitidis
Neisseria
Incubation period:
2 to 10 days, commonly 3-4 days.
Mode of transmission:
Direct contact including respiratory droplets from
nose and throat of infected people.
Source of infection :
Carriers are the most important source of infection
while cases represent only negligible source of
infection.
Reservoir : Humans.
Meningococcal meningitis
Period of communicability:
The patient still contagious until live meningococci are
no longer present in discharges from nose and mouth.
Meningococci usually disappear from the nasopharynx
within 24 hours after initiation of antimicrobial
treatment.
Susceptibility:
1. Susceptibility to clinical disease is low and decrease
with age leading to high carriers to cases ratio.
2. Deficiency in complement component and
splenectomy increase risk of disease.
Meningococcal meningitis
Initial diagnosis of meningococcal meningitis can
be made by clinical examination followed by
lumber puncture which show turbid CSF.
The bacteria can be isolated by microscopically
examination of CSF but the diagnosis confirmed
by culture of CSF or blood or by using PCR
(polymerase chain reaction).
Diagnosis
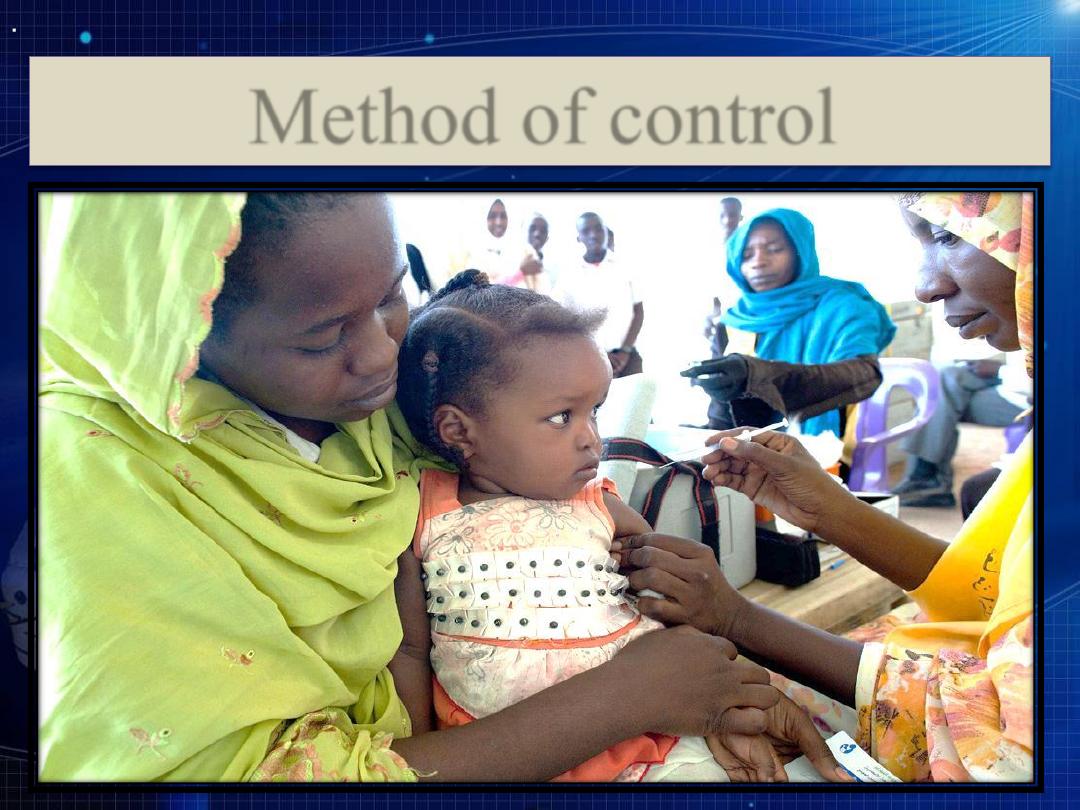
Method of control
Preventive measures
1. Educate the public on the need to reduce direct contact
and exposure to droplet infection.
2. Reduce overcrowding in living quarters and workplace
such as schools and ships.
3. Meningococcal polysaccharide vaccines are available in
either bivalent (groups A and C), trivalent (groups A, C
and W), or tetravalent (groups A, C, Y and W)forms to
control the disease.
A meningococcal A conjugate vaccine, C conjugate
vaccines, tetravalent A, C, Y and W conjugate vaccines
are also available.
Preventive measures
As of January 2015, over 220 million persons have
received meningococcal A conjugate vaccine in 15
countries of the African belt.
Vaccines are effective for
outbreak control and
prevention among high risk groups
such as:
a. Travelers to country where disease is epidemic.
b. Hajj pilgrims.
c. Military groups.
d. Individual with immune dysfunctions.


Control of patient ,contacts and immediate
environment
1.Report to local heath authority.
2. Isolation: Respiratory isolation for 24 hours after
start of chemotherapy.
3. Concurrent disinfection : of discharges from the
nose and throat and articles soiled with them.
4. Quarantine : Not applicable.
5. Protection of contacts : by chemoprophylaxis
using Rifampicin , ceftriaxone and ciprofloxacin
which are equally effective as prophylactic agents
given to close and household contacts of patients
with meningococcal meningitis.
Control of patient ,contacts and immediate
environment
Rifampicin is given twice daily for 2 days, adult
(600 mg) per dose , children over one month 10 mg
per kg and children under one month 5 mg per Kg.
For adult ,ceftriaxone 250 mg IM given as single
dose ,125 mg for children under 15 years.
Ciprofloxacin 500 mg given as single dose for
adult.
Control of patient ,contacts and immediate
environment
6. Investigation of contacts and source of infection
Throat or nasopharyngeal cultures are of no value in
deciding who should receive chemoprophylaxis.
7.Specific treatment: Penicillin is drug of choice for
meningococcal disease, ampicillin and chloramphenicol
are also effective.
Patients with meningococcal disease must receive
rifampicin prior to discharge to ensure elimination of
organism (if neither 3
rd
generation cephalosporin nor
ciprofloxacin was given as treatment).
8. Carrier : use rifampicin to remove carrier state.
Epidemic Measures
1. Careful surveillance , early diagnosis and immediate
treatment for suspected cases must be made when
outbreak occur.
2. Reduce overcrowding and ventilate living and sleeping
quarters.
3. Mass chemoprophylaxis is not advisable but when
outbreak involve small population , chemoprophylaxis to
all members of population is considered.
4.The use of vaccine is strongly considered when the
outbreak caused by groups (A,C,Y and W-135 ). The
vaccine are polysaccharide vaccine or conjugate vaccine.
Disaster implications and international measures
Disaster implications:
When epidemic occur in area with forced
crowding area.
International measures:
Some countries required valid certificate of
immunization against meningococcal
meningitis eg. Saudi Arabia for Hajj pilgrims.
Hemophilus meningitis
Before use of H. Influenzae type b vaccine, H. Influenzae
type b is regard as the most common cause of meningitis
in children aged 2 months to 5 years.
The onset of disease is usually sudden with fever,
vomiting and bulging fontanelle in infant and stiff neck in
older children.
Diagnosis by isolation of organism from blood or CSF.
Causative agent : Haemophilus influenzae which
classified into 6 types from a to f . H. influenzae type b is
the most pathogenic type.
Hemophilus meningitis
Hemophilus meningitis
: worldwide, most prevalent among the
Occurrence
children aged 2 months to 3 years.
: Humans.
Reservoir
days.
4
-
2
:
Incubation period
: As long as the organism are
Period of communicability
present. The patient is non further infectious 24-48 hours
following start of effective antibiotic therapy.
: assumed to be universal. Immunity can
Susceptibility
be acquired transplacentally, from prior infection or
through immunization.

Preventive Measures
Routine childhood immunization using H.
influenzae b conjugate vaccines which
prevent meningitis in children.
In Iraq the vaccine start to be given from
2011 at the age of second,4
th
and 6
th
months
and booster dose at 18
th
months.

Preventive Measures
Control patient , contacts and immediate
environment
1. Report to local health authority.
2. Isolation: for 24 hours after start of
chemotherapy.
3. Protection of contacts : by rifampicin
chemoprophylaxis (orally once daily for 4
days).
4. Specific treatment : Ampicillin is drug of
choice and cefotaxime or chloramphenicol are
alternatives.
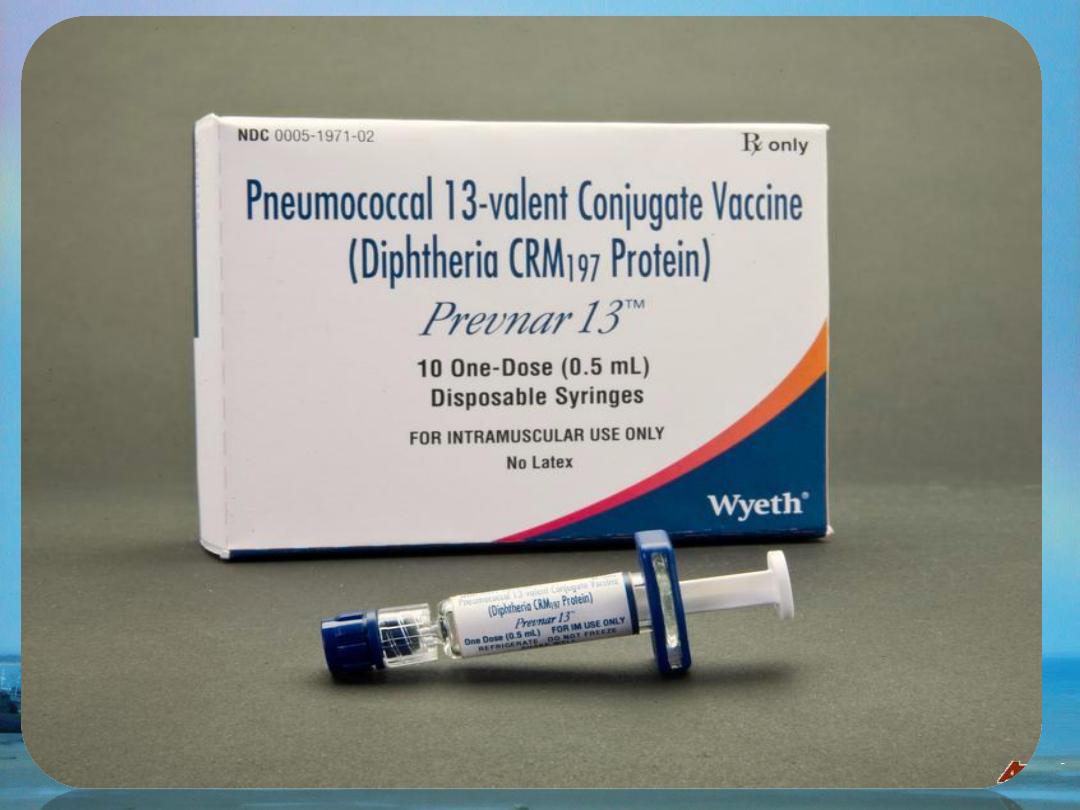
Pneumococcal meningitis
Infectious agent : Streptococcus pneumoniae.
Occurrence : worldwide.
Reservoir : Humans.
Mode of transmission : Droplet infection and
contact with respiratory secretions.
Incubation period : 1-4 days.
Susceptibility : assume to be universal. The
immunity can be acquired transplacentally, from
prior infection and from immunization.
Pneumococcal meningitis
Methods of control
Preventive measures:
Vaccination is the mainstay of prevention using
pneumococcal conjugate vaccine.
Control patient , contacts and immediate environment :
1. Report to local health authority.
2. Isolation : Standard precautions for hospitalized patients.
3. Concurrent disinfection: of nasal and throat secretions.
4. Specific treatment : Penicillin, ceftriaxone or cefotaxime
are drugs of choice.

Neonatal Meningitis
Infants with neonatal meningitis develop lethargy,
poor feeding, seizures.
In first week of life, the causative agents may be
group B streptococci, Listeria monocytogenes
acquired from the birth canal.
Infants 2 weeks to 2 months, the causative agents
group B streptococci or Klebsiella acquired from
nursery environment.Treatment include ampicillin
plus third generation cephalosporin.
Neonatal Meningitis
Common causes of bacterial meningitis
according to age group
Age Group
Causes
Newborns
Group B Streptococcus, Escherichia coli,
Listeria monocytogenes
Infants and
Children
Streptococcus pneumoniae, Neisseria
meningitidis, Haemophilus influenzae type b
Adolescents and
Young Adults
Neisseria meningitidis, Streptococcus
pneumoniae
Older Adults
Streptococcus pneumoniae, Neisseria
meningitidis, Listeria monocytogenes

