By
Dr. Ameer kadhim Hussein
M.B.Ch.B. FICMS (Community Medicine)
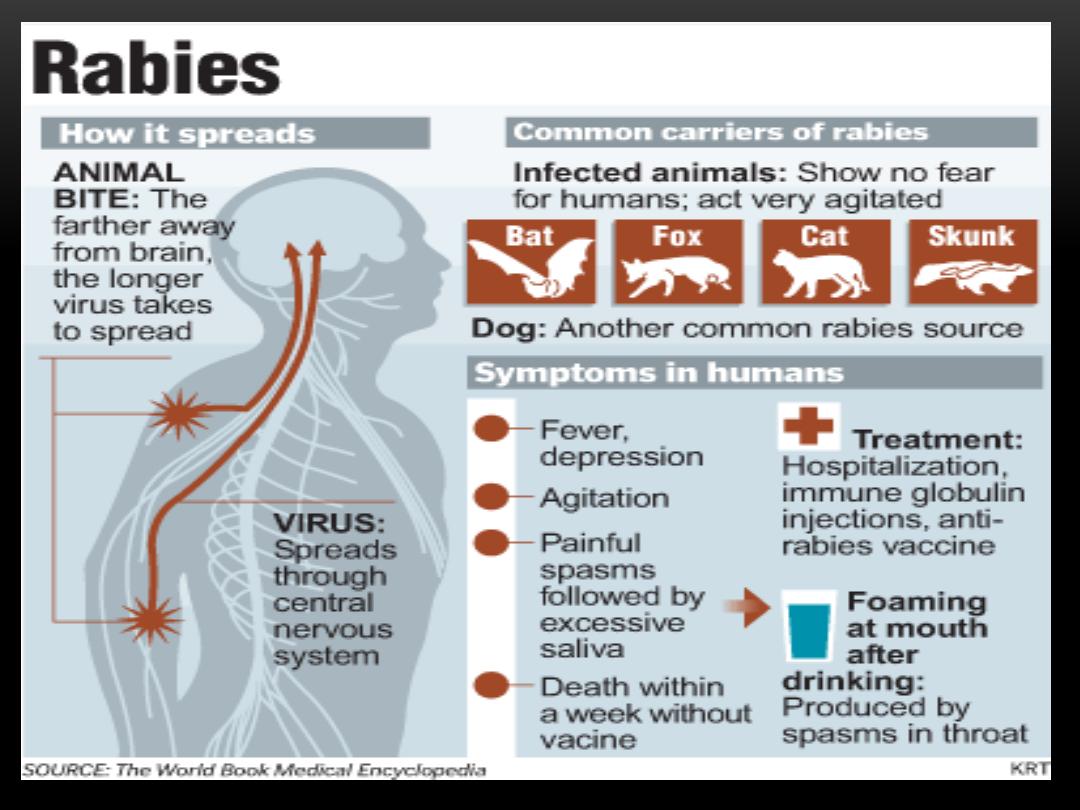
RABIES
DEFINITION
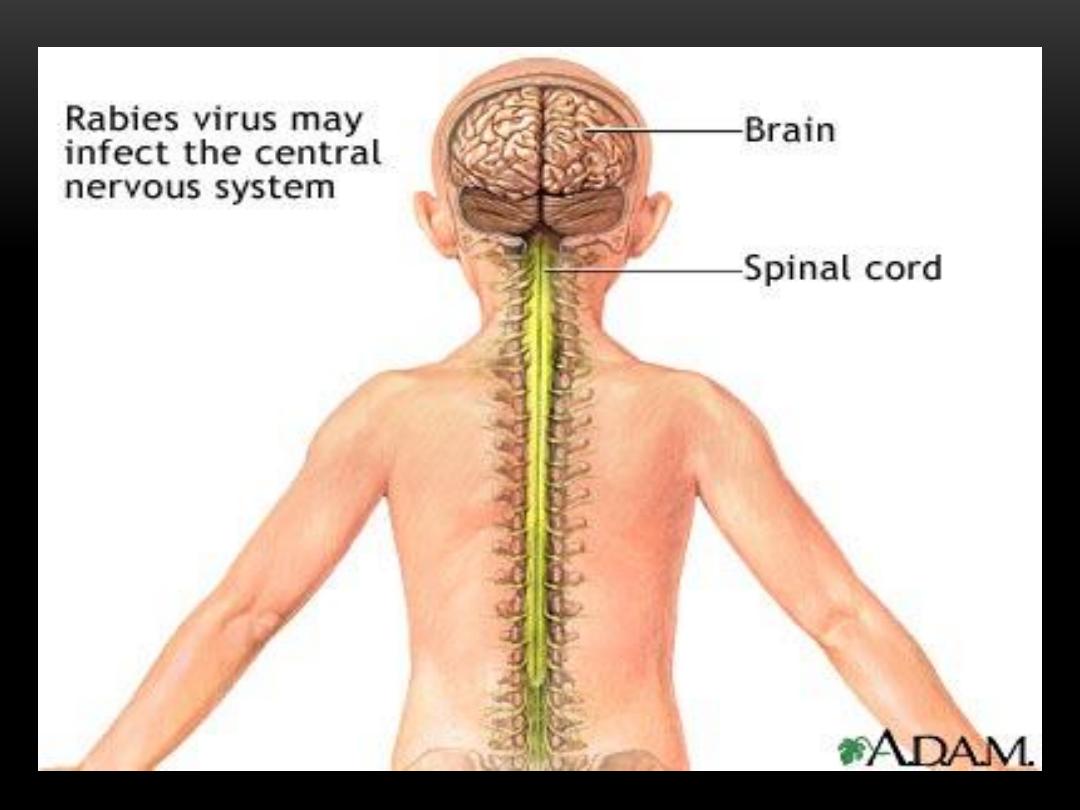
Rabies is an acute highly fatal viral disease of
central nervous system caused by Lyssa virus
type 1.
It is zoonotic disease of warm blooded animals
especially carnivorous animals such as dogs,
cats and wolves.
It is transmitted to man usually by bites or licks
of rabid animals.
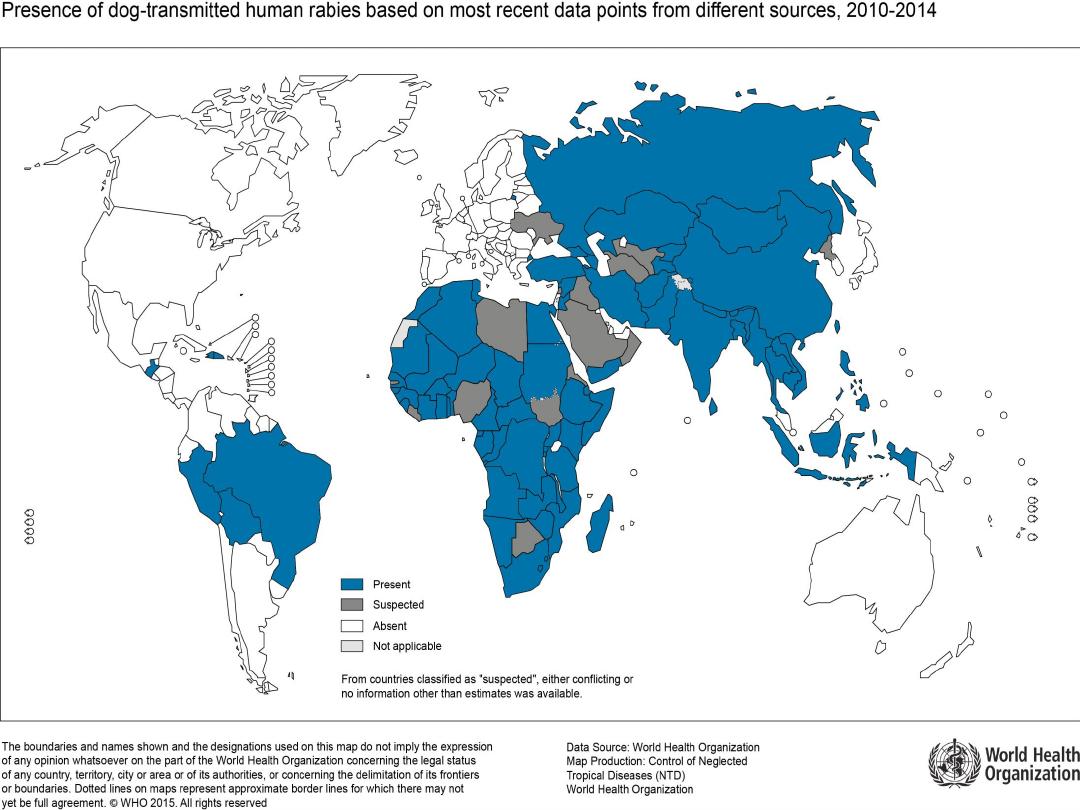
GEOGRAPHICAL DISTRIBUTION
Rabies is an
enzootic and epizootic
disease of world
wide importance. Some countries have achieved
(rabies free) by vigorous campaign of elimination
while in others the disease has never been introduced.
Water
is regard as the most important barrier for
rabies.
Rabies free area is defined as area in which no case
of indigenously acquired rabies has been reported in
man or animal in previous 2 years in presence of
surveillance system and health regulations.
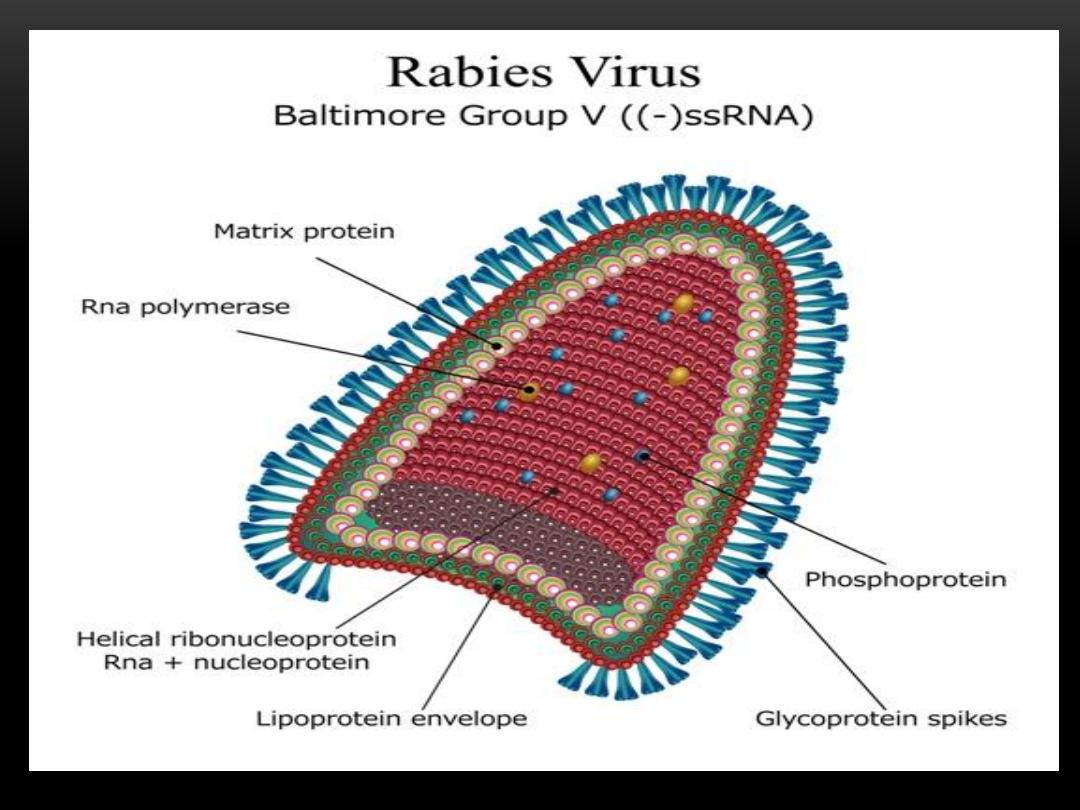
Infectious agent:
Lyssa virus type1 which is RNA virus belong to
rhabdoviridae family.
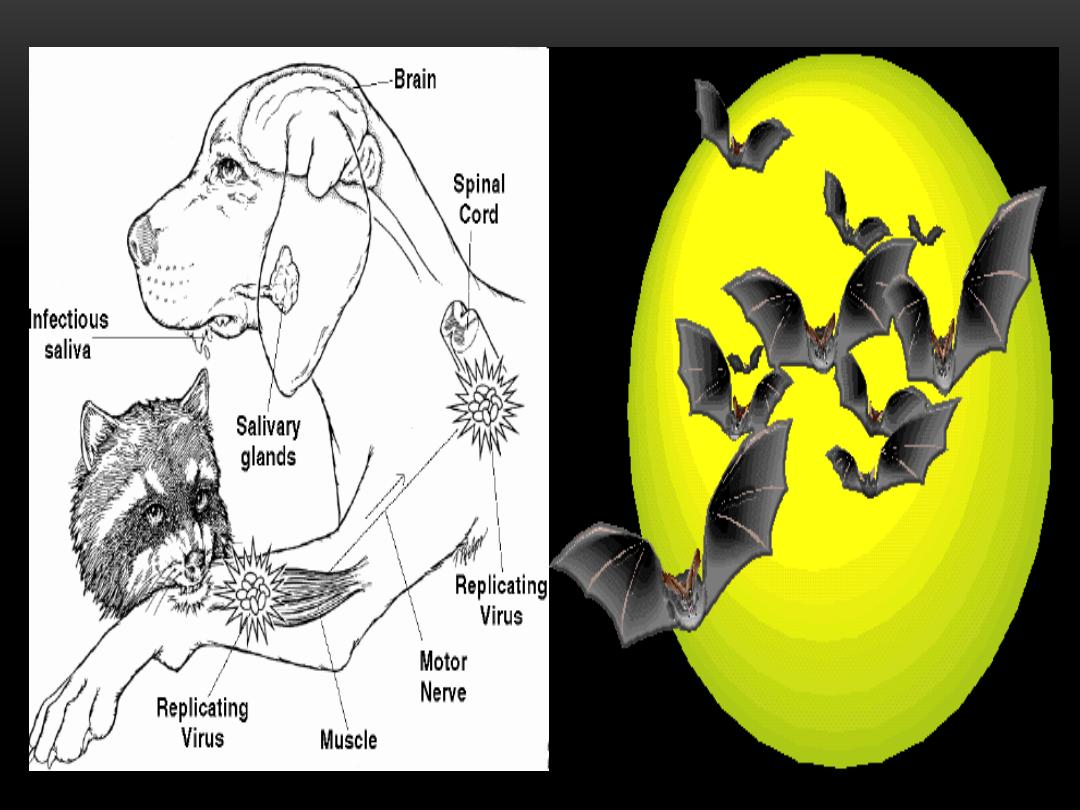
Reservoir of infection:
Wild and domestic animal including dogs, foxes,
wolves and other biting animals. Bats also regard as a
reservoir of infection in some area like Mexico.
Source of infection:
The source of infection to man is the saliva of rabid
animals. In dogs and cats the virus may be present in
the saliva for 3 to 4 days before the onset of disease
and persist during the course of illness until death.
Susceptibility:
All mammals are susceptible. Studies show that not
every person bite by rabid animal and not receive
treatment develop disease but those develop disease
represent about 40%.
Mode of transmission:
1. Animal bites.
2. Licks on abraded skin and mucosa.
3. Aerosols: in caves harboring rabies infected bats.
4. Person to person: man to man transmission although
rare but possible by corneal and organ transplants.

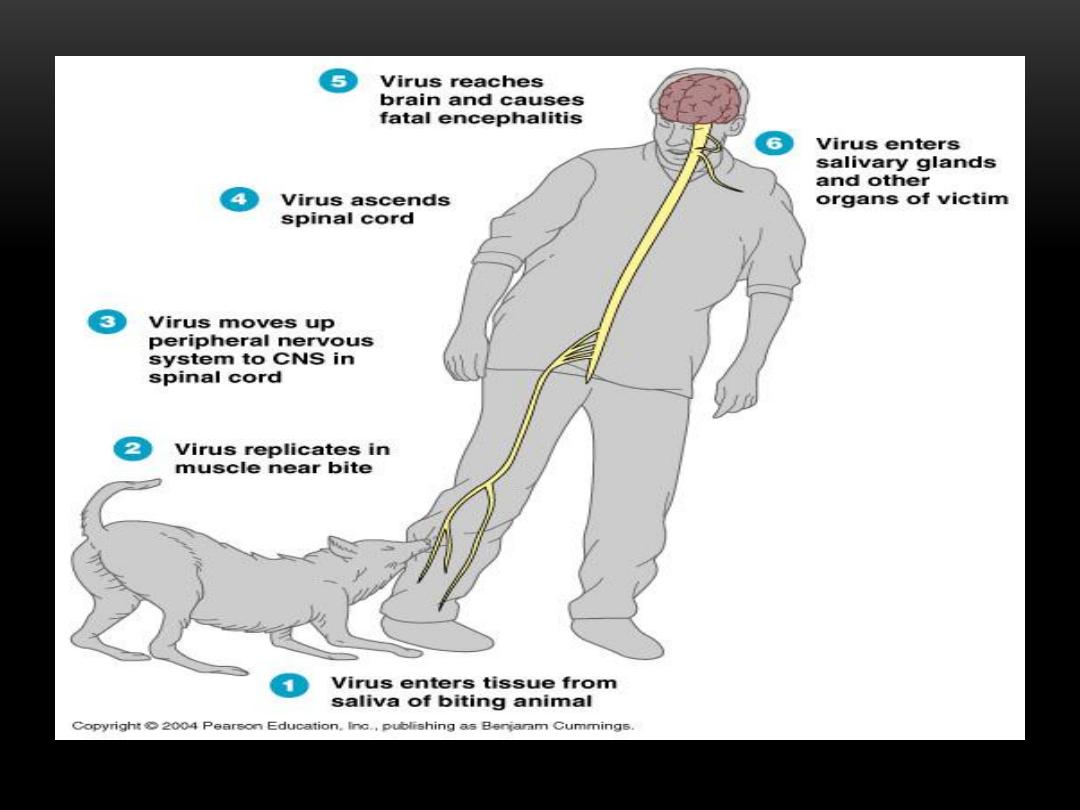
Incubation period:
The incubation period in man is highly variable commonly 3 to 8
weeks (sometimes as short as 4 days and may persist to many
years).
The incubation period depend on the following:
1. Site of bite.
2. Severity of bite.
3. Number of the wounds.
4. Amount of virus injected.
5 . Species of the biting animal.
6 . Protection provided by clothes and treatment.
Shorter incubation period occur in:
(Sever exposure, bite in head, neck, face and upper extremities
and bite by wild animal).
CLINICAL PICTURE AND DIAGNOSIS
Clinical picture:
The disease begins with prodromal symptoms such as headache,
malaise, sore throat and slight fever for 3-4 days.
This stage is followed by widespread excitation of nervous
system. The patient is intolerant to noise, bright light with
aerophobia and hydrophobia which pathognomonic of rabies.
Duration of disease is 2 to 3 days the patient may be die abruptly
during convulsions or may pass to paralysis or coma.
Diagnosis:
Rabies can be confirmed in patients by antigen detection using
immunofluorescence of skin biopsy and by virus isolation from
saliva and other secretions.

METHODS OF CONTROL
A .PREVENTIVE MEASURES
1. Immunize all dogs and cats in enzootic countries.
2. Maintain active surveillance for rabies in animals.

3.Observe clinically for
10 days
any dog or cat known
to have bitten person (unwanted dog or cat can be
sacrificed immediately and examine for rabies) if the
biting animal was infected at time of bite, sign of
rabies will usually occur within 4-7 days with
paralysis followed by death.
The head of animal must be send to laboratory to
confirm diagnosis of rabies by microscopically
identification of
Negri bodies
.
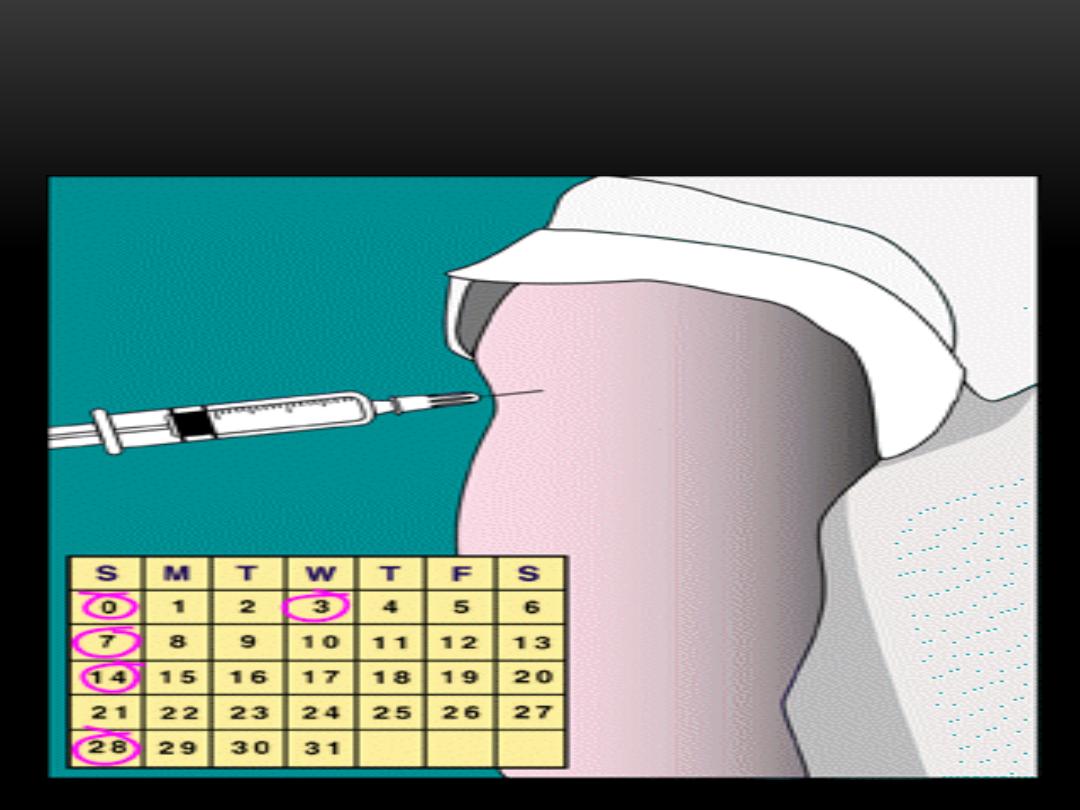
4. Individuals who are at high risk for rabies should be
protected by
pre exposure immunization
using potent and safe
cell culture vaccine which given in 3 doses of (1ml) IM on days
(
0,7,21 or 28
). If the risk of exposure continue booster doses
need to be given at interval of 2 years.
Those individuals include the following:
a. Laboratory staff working with rabies virus.
b. Veterinarians.
c. Animal handlers.
d . Wild life officers.
e. Long term travelers to rabies endemic area.
5. Post exposure prophylaxis:
Which is usually done for prevention of rabies after animal bites.
Post exposure prophylaxis include the following:
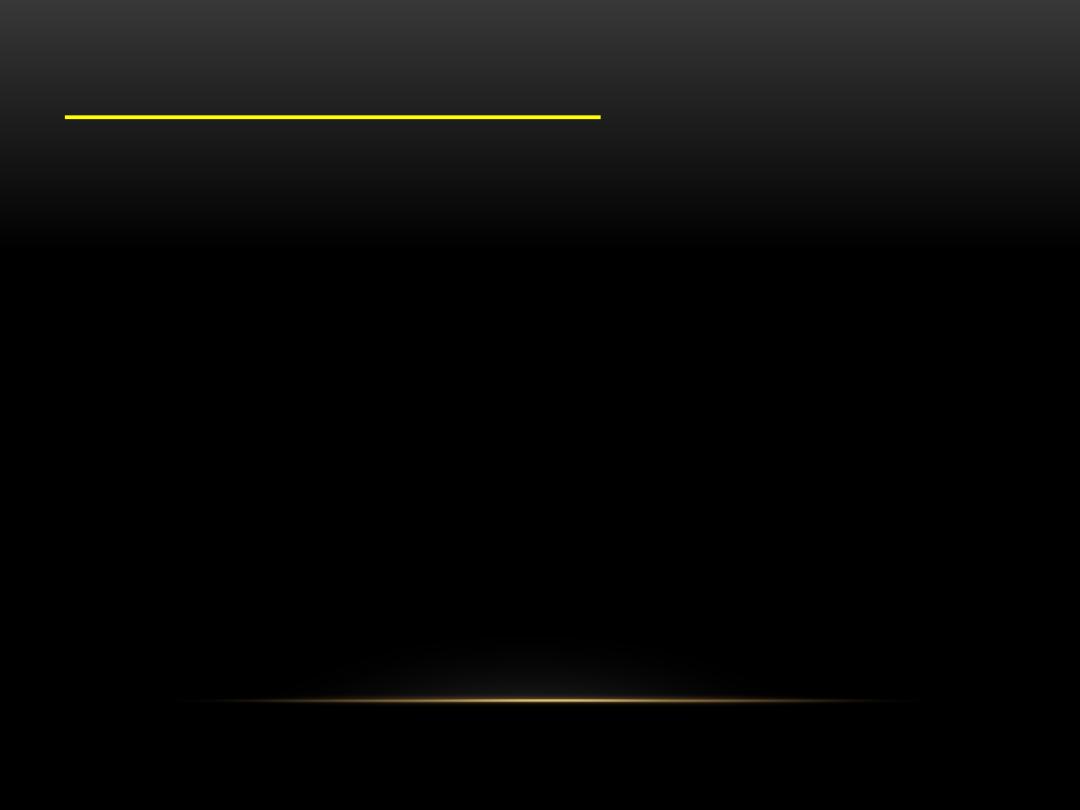
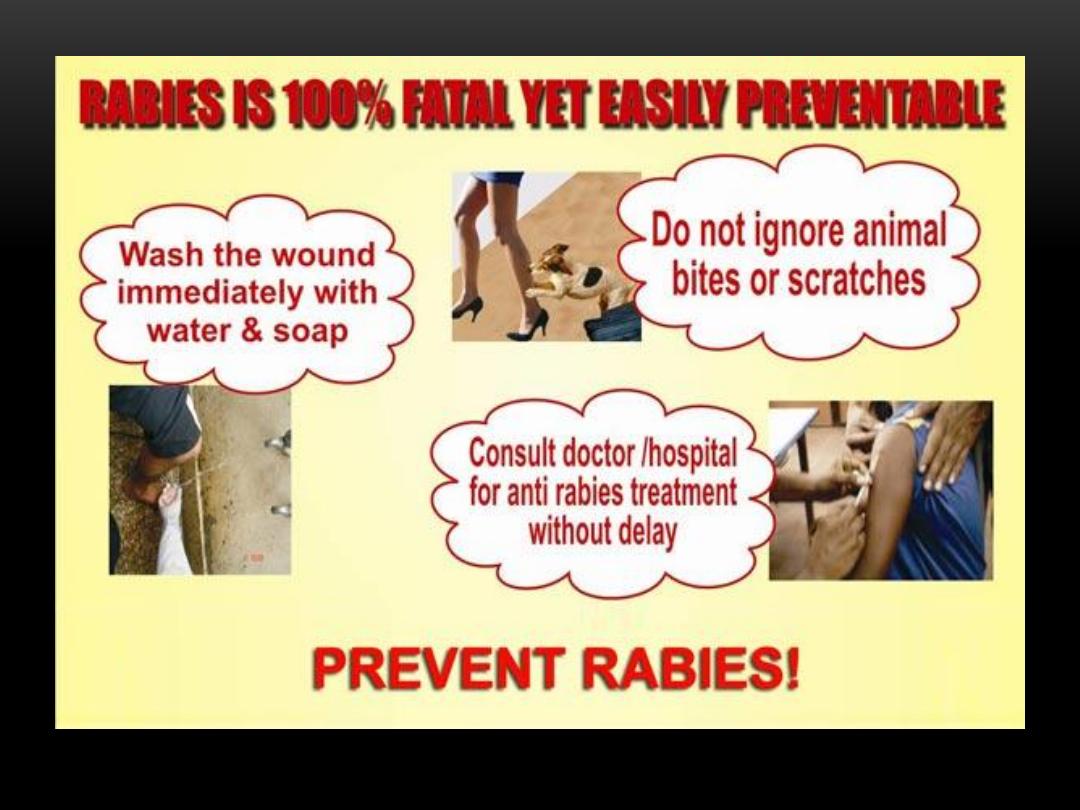
a. First aid:
Immediate washing the wound with plenty of soap
and water under a running tap with at least 15 minutes.
b. Chemical treatment:
using virucidal agents including alcohol
or 0.01% aqueous solution of iodine or povidone iodine.
c. Suturing:
Bite wounds should be not sutured immediately to
prevent additional trauma which may lead to spread the virus to
deeper tissues , if suturing is necessary it should be done 24 to
48 hours later with minimum possible stitches under cover of
anti rabies serum.
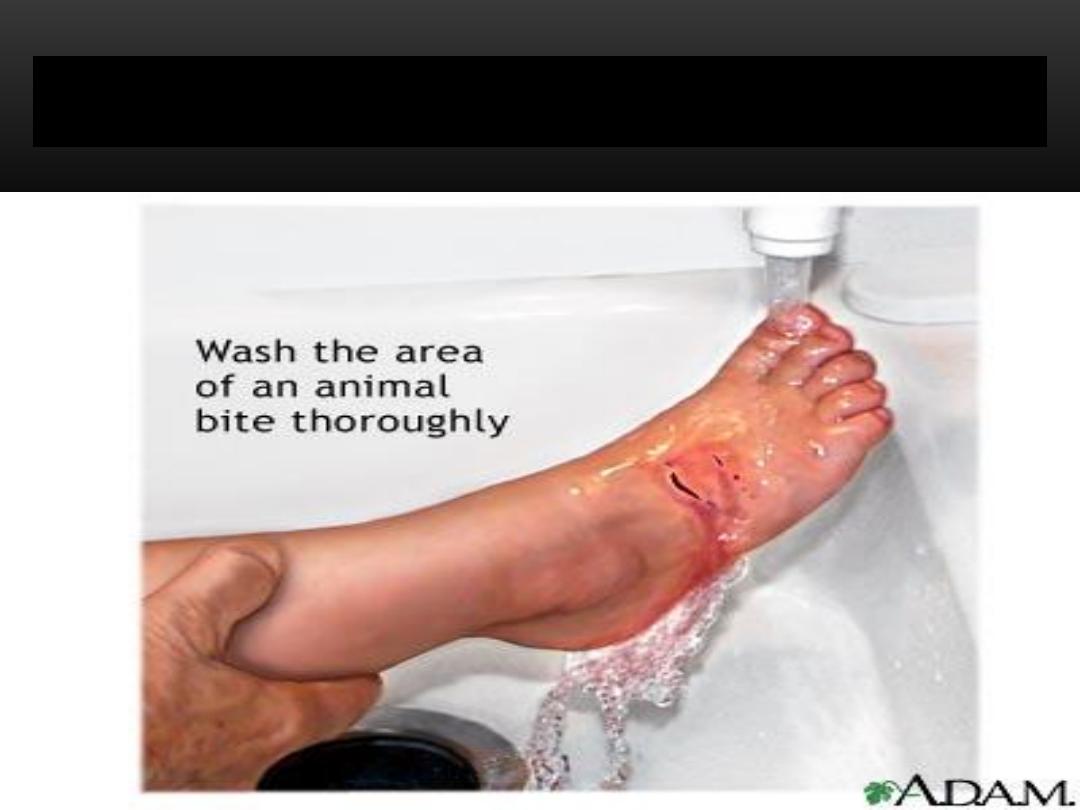
Wound cleaning & treatment
d. Anti rabies serum:
local application of anti rabies serum is
very effective in preventing rabies.
e . Antibiotics and anti tetanus measures.
f . Observe the animal for 10 days:
if the animal show sign of
rabies it should be killed and the head send to laboratory
examination to ensure the diagnosis. If the animal remain alive
and healthy at the end of 10 days there is no indication of anti
rabies treatment.
g. Vaccine administration:
By using modern cell culture vaccine with routine intra muscular
schedule in deltoid muscle which consist of 6 doses of (1 ml) on
days (0, 3, 7, 14 , 28 and 90).
VACCINE ADMINISTRATION
Indications of anti rabies treatment:
a. If the animal show sign of rabies or die within
10 days of observation.
b. If the biting animal cannot be identified.
c. All bites by wild animals.
d. If laboratory tests of brain of animal is positive
for rabies.
e. Unprovoked bites.
6.Post exposure prophylaxis of person who
have been vaccinated previously
If the patient antibody titre is unknown or the
bite is severe we use (
3 IM doses of vaccine on
days 0, 3 and 7
) while if titre is high or bite is
not so severe so give (
2 doses on days 0 and 3
).
No need for systemic passive immunization (IG).
Treatment
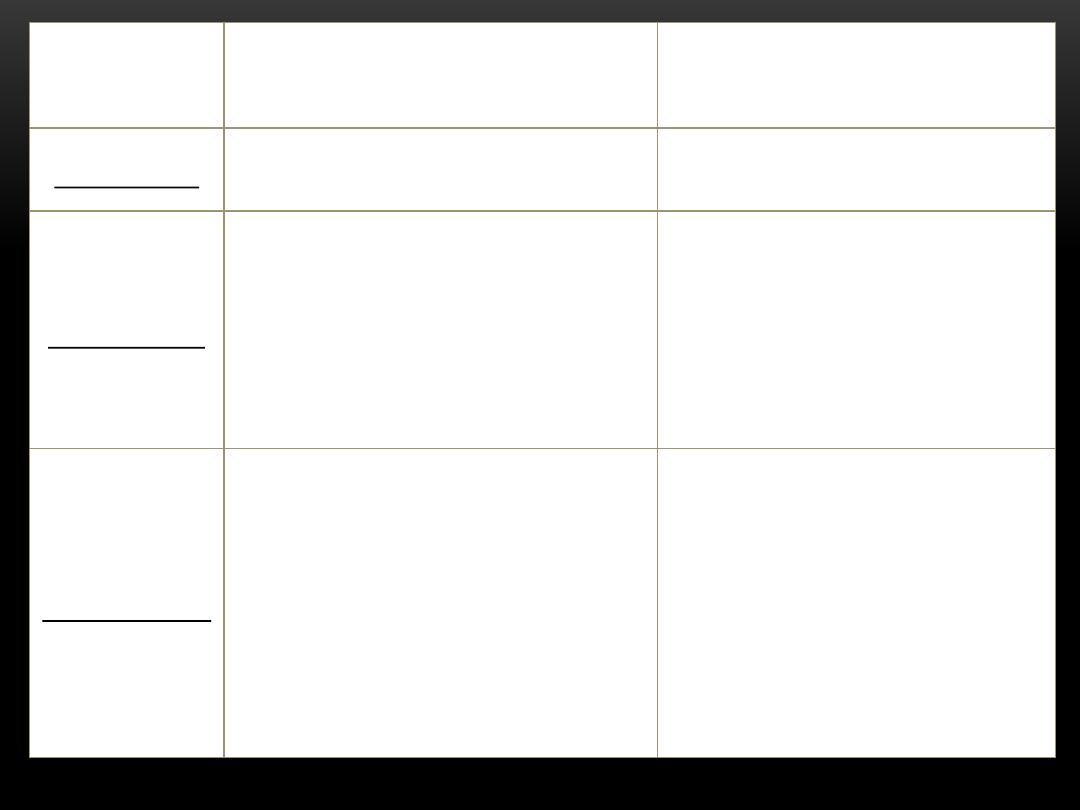
Type of contact with
suspected rabid animal
Exposure
category
None
touching or feeding animals, licks
on intact skin
category I
Administer vaccine
immediately , stop treatment if
animal remain healthy
throughout 10 days of
observation or laboratory test
negative for rabies
nibbling of uncovered skin, minor
scratches or abrasions without
bleeding, licks on broken skin
category II
Administer vaccine and
immunoglobulin immediately ,
stop treatment if animal remain
healthy throughout 10 days of
observation or laboratory test
negative for rabies
single or multiple transdermal
bites or scratches, contamination
of mucous membrane with saliva
from licks
category III

RABIES VACCINE
B. CONTROL OF PATIENT, CONTACTS
AND IMMEDIATE ENVIRONMENT
1. Report to local health authority.
2. Concurrent disinfection: of saliva and articles
soiled with them.
3. Immunization of contacts: contacts who have open
wound or mucus membrane expose to patient
saliva should receive anti rabies treatment.
4. Investigation of contacts and source of infection
by searching for rabid animals.
6. Specific treatment: only by supportive medical
care.
SUMMARY
Rabies is a vaccine-preventable viral disease which occurs in
more than 150 countries and territories.
Dogs are the source of the vast majority of human rabies
deaths and Rabies elimination is feasible by vaccinating dogs.
Infection causes tens of thousands of deaths every year,
mostly in Asia and Africa.
40% of people who are bitten by suspect rabid animals are
children under 15 years of age.
Immediate wound cleansing with soap and water after contact
with a suspect rabid animal can be life-saving.
Every year, more than 15 million people worldwide receive a
post-bite vaccination to prevent the disease; this is estimated
to prevent hundreds of thousands of rabies deaths annually.
Rabies, a zoonotic disease, requires close co-ordination
between animal and human health sectors at the national,
regional and continental levels. In December 2015, a
global framework to reach zero human rabies deaths by
2030 was launched by WHO and the World Organization
for Animal Health (OIE), in collaboration with the Food
and Agriculture Organization of United Nations (FAO)
and the Global Alliance for Rabies Control. This initiative
marks the first time that the human and animal health
sectors have come together to adopt a common strategy
against this devastating but massively neglected disease.
SUMMARY
Rabies transmitted by dogs has been eliminated in many
Latin American countries, including Chile, Costa Rica,
Panama, Uruguay, most of Argentina, the states of São
Paulo and Rio de Janeiro in Brazil, and large parts of
Mexico and Peru.
Many countries in the WHO South-East Asia Region have
embarked on elimination campaigns in line with the target
of regional elimination by 2020.
Bangladesh launched an elimination programme in 2010
and, through the
management of dog bites, mass dog
vaccination and increased availability of vaccines free of
charge
, human rabies deaths decreased by 50% during
2010–2013.
SUMMARY

WORLD'S RABIES DAY (ON SEPTEMBER 28)
World Rabies Day is celebrated
annually to raise awareness
about rabies prevention and to
highlight progress in defeating
this horrifying disease.
28 September also marks the
anniversary of Louis Pasteur's
death, the French chemist and
microbiologist, who developed
the first rabies vaccine
.
28 September 2016, the World Health Organization
(WHO) estimates that up to 99% of human rabies cases
are transmitted by the bite of infected dogs and that the
infection causes tens of thousands of deaths every year,
mostly in Africa and Asia.
Four out of every 10 deaths from rabies are in children
aged under 15 years.
Although immediate wound cleansing with soap and
water after contact with a suspected rabid animal can be
life-saving, it is crucial also that people living in at-risk
and endemic areas access prompt wound management
and vaccines
.
SUMMARY
GLOBAL PARTNERS ANNOUNCE PLAN TO END
HUMAN DEATHS FROM DOG-TRANSMITTED
RABIES BY 2030

Thank you
