RESPIRATORY SYSTEM د. سرى سلمان عجام
Aim of studying pathology of Respiratory system
1.To know the types of lesions affecting this system2. To study the gross & microscopical features of these lesions
3. To correlate the signs & symptoms
Anatomy
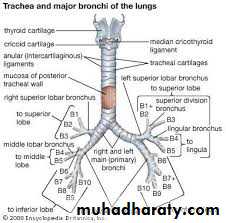
Respiratory tract consist of:
Nose,nasopharynx,larynx,trachea,right & left bronchi.
The bronchi lead to respiratory lobule or acinus
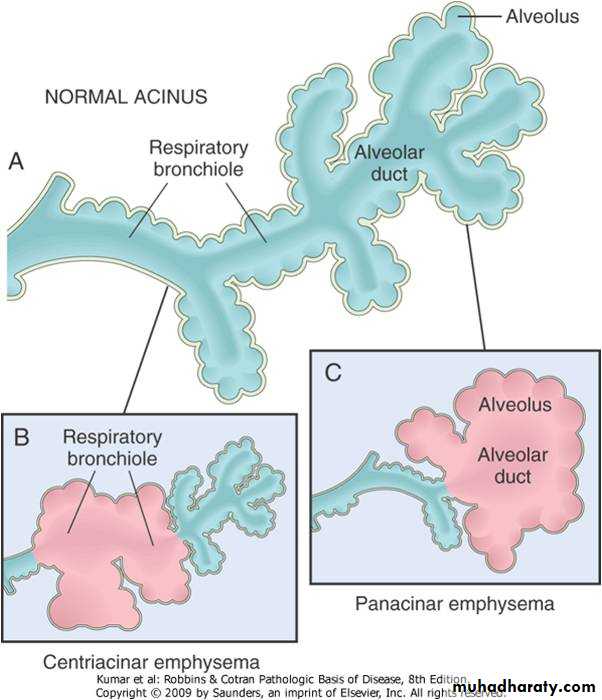
Acinus
The part of the lung distal to terminal bronchiole is called Respiratory Lobule or acinus it Consist of respiratory bronchioles and alveolar ducts and alveoli .
Alveoli arise from both respiratory bronchioles and alveolar duct .
Upper & lower respiratory tract
The respiratory tract are roughly divided in toUpper respiratory tract : Above cricoid cartilage
Lower respiratory tract : Below cricoid cartilage
Histology
Trachea The trachea is a wide flexible tube, the lumen of which is kept open by 20 tracheal cartilages, which are C-shaped rings of hyaline cartilage. The gaps between the rings of cartilage are filled by the trachealis muscle - a bundle of smooth muscle, and fibroelastic tissue.
The respiratory mucosa is made up of the epithelium and supporting lamina propria). The epithelium is tall columnar pseudostratified with cilia and goblet cells. The supporting lamina propria underneath the epithelium contains elastin, that plays a role in the elastic recoil of the trachea during inspiration and expiration, together with blood vessels that warm the air.
The sub-mucosa contains glands which are mixed sero-mucous glands. The watery secretions from the serous glands humidify the inspired air. The mucous, together with mucous from the goblet cells traps particles from the air which are transported upwards towards the pharynx by the cilia on the epithlium. This helps to keep the lungs free of particles and bacteria
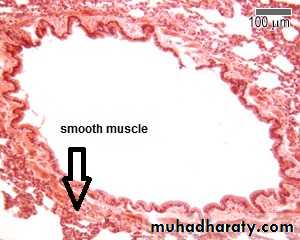
Bronchioles
The epithelium is made up of ciliated columnar cells in larger bronchioles, or non-ciliated in smaller bronchioles (difficult to see at this magnification). There are no goblet cells, but there are cells called Clara cells. These cells are secretory - they secrete one of the components of surfactantTheres no cartilage in the wall
The nose, nasopharynx, bronchi are lined by pseudo stratified tall columnar ciliated epithelium &contain goblet cells and neuroendocrine cells.
True vocal cord are lined by squamous epithelium. Submucosa contain mucus glands.
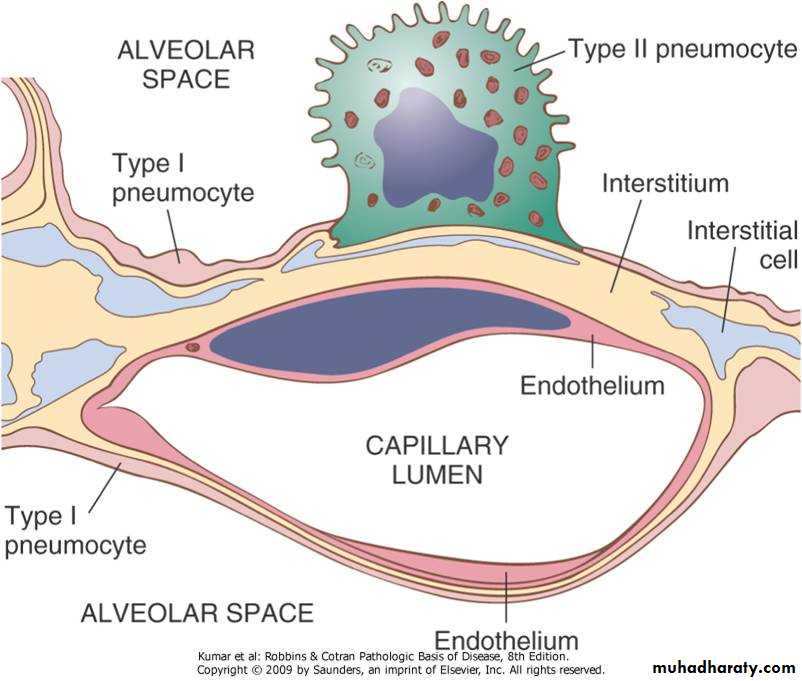
The alveoli are lined by:
Type I pneumocytes: Flattened cellsType II pneumocytes :Rounded. It is the sources of pulmonary surfactant & repair of type I pneumocytes
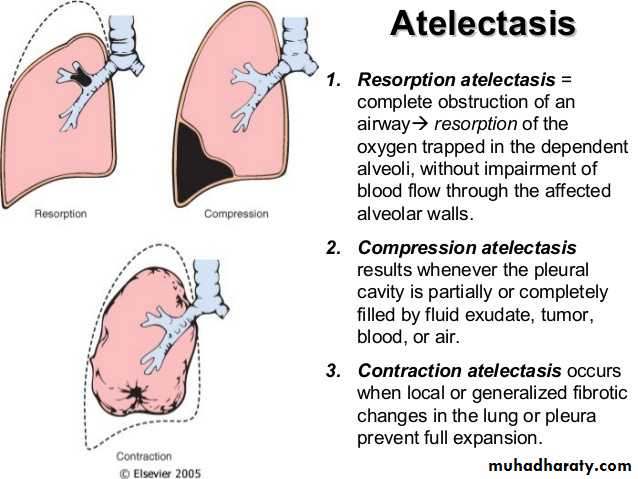
Atelectasis
Definition : is loss of lung volume caused by inadequate expansion of airspaces. It is associated with shunting of inadequately oxygenated blood from pulmonary arteries into pulmonary veins, thus giving rise to a ventilation – perfusion imbalance and hypoxia.Types :
1- Resorption Atelectasis :
It occurs when an obstruction prevents air from reaching distal airways, the air already present gradually becomes absorbed and alveolar collapse follows. The most common cause of this type is obstruction of bronchus by mucus plug, other causes include foreign body, tumor, enlarged lymph nodes.
2- Compression Atelectasis :
It is associated with accumulations of fluid, blood and air within the plural cavity, which mechanically collapse the adjacent lung,, this is frequent occurrence with plural effusions caused most commonly with congestive heart failure.
3-Microatelectasis :
It is a generalized loss of lung expansion caused by a complex set of events, the most important of which is loss of surfactant in both adult and neonatal respiratory distress syndrome.
4- Contraction Atelectasis :
It occurs when either local or generalized fibrotic changes in the lung or pleura hamper expansion and increase elastic recoil during expiration.
Chronic Obstructive Airway Diseases
(COPD)COPD is a group of disorders characterized by airflow obstruction. Their characteristics include a marked decreased in first second forced expiratory volume (FEV1) and increased or normal forced vital capacity (FVC), resulting in decreased FEV1 : FVC ratio.
COPD include :
1- Asthma.
2- Emphysema.
3-Chronic Bronchitis.
4- Bronchiectasis.
Asthma :-
Definition : is characterized by episodic , reversible bronchospasm resulting form an exaggerated bronchoconstricter response to various stimuli .
Clinical features :
During attack of asthma there are sever dyspnea and wheezing and chief difficulty lies in expiration. Associated hypercapnia acidosis and sever hypoxia may be fatal .Classification of asthma:
intrinsic asthma :- in which the triggering mechanisms are non-immune such as aspirin , pulmonary infection , cold , viruses, psychological stress , there is no family history of allergic manifestation , and normal IgE level in serum .Extrinsic asthma :- in which the asthmatic episode is typically initiated by type I hypersensitivity reaction induced by exposure to extrinsic antigen, there are several type of extrinsic asthma , the most common one is atopic asthma. Which is usually occur in first 2 decades of life associated with allergic manifestation and increase serum IgE.
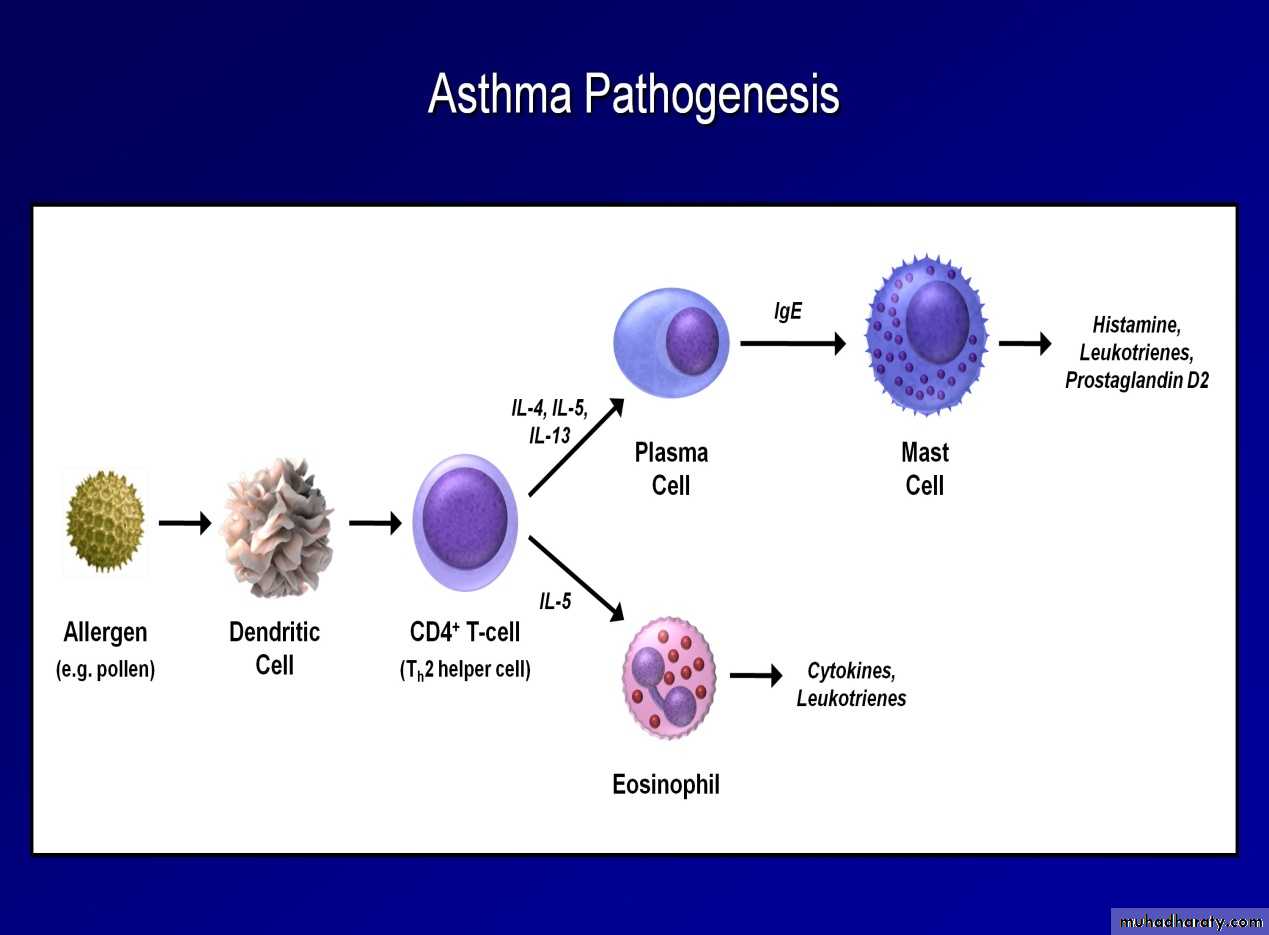
Pathogenisis :
we discuss pathogenesis of atopic asthma because it is most common .
The common dominator underlying asthma is an airway hyperresposiveness , bronchial inflammation is the substrate of hyperresposiveness , the cause of inflammation in atopic asthma is type I hypersensitivity reaction which is driven by sensitization of CD4 cells of TH2 type.
TH2 cells release cytokines (IL4,5,13 ) which favor synthesis of IgE, growth of mast cells and activation of eosinophils
1- role of IgE:-
IgE bind to the foreign antigen and then it will bind to mast cells leading to release mast cell mediators like histamine.
2- role of mast cells :- the initial triggering of mast cells occur in mucosal surface , the resultant mediators release opens mucosal intercellular junctions allowing penetration of antigens to more numerous mucosal mast cells , in addition to direct stimulators of parasympathetic receptors provokes reflex bronchospasm .
Examples of mast cells mediators :
Histamine , IL4 , IL5prostaglandin E2 ,D2 , F2α , leukotrienes ...,etc.
3- role of eosinophils:-
Eosinophils contain the following :
A- major basic protein and eosinophilic cationic protein which are directly toxic to the epithelial cells
B- eosinophilic peroxidase causes tissue damage through oxidative stress.
C- activated eosinophils are rich in leukotriene C4 and platelet activating factors.
Morphology:
Grossly In patients dying of status asthmaticus the lungs are overdistended because of overinflation, with small areas of atelectasis. The most striking macroscopic finding is occlusion of bronchi and bronchioles by thick, tenacious mucus plugs. Histologically, the mucus plugs contain whorls of shed epithelium, which give rise to the well-known spiral shaped mucus plugs called Curschmann spirals (these result either from mucus plugging in subepithelial mucous gland ducts which later become extruded or from plugs in bronchioles). Numerous eosinophils and Charcot-Leyden crystals are present; the latter are collections of crystalloid made up of an eosinophil lysophospholipase binding protein called galectin-10.Microscopically
- edema , hyperemia and inflammatory infiltrate in the bronchial walls (eosinophils 5-50% of cellular infiltrate , mast cells , basophils , macrophage and neutrophils
The other characteristic histologic findings of asthma, collectively called “airway remodeling” include:
•
Overall thickening of airway wall•
Sub-basement membrane fibrosis (due to deposition of type I and III collagen beneath the classic basement membrane composed of type IV collagen and laminin)
•
Increased vascularity•
An increase in size of the submucosal glands and mucous metaplasia of airway epithelial cells
•
Hypertrophy and/or hyperplasia of the bronchial wall muscle (this has led to the novel therapy of bronchial thermoplasty in which radiofrequency current is applied to the walls of the central airways through a bronchoscopically placed probe, which reduces airway hyper-responsiveness for up to at least a year).
Clinical Course.
The classic acute asthmatic attack lasts up to several hours. In some patients these symptoms of chest tightness, dyspnea, wheezing, and cough with or without sputum production, persist at a low level constantly. In its most severe form, status asthmaticus, the severe acute paroxysm persists for days and even weeks, and under these circumstances airflow obstruction might be so extreme as to cause severe cyanosis and even death Up to 50% of childhood asthma remits in adolescence only to return in adulthood in a significant number of patients. In other cases there is a variable decline in baseline lung function.Genetics of Asthma.
Asthma is a complex genetic trait in which multiple susceptibility genes interact with environmental factors to initiate the pathologic reaction. As in other complex traits ( Chapter 5 ), there is considerable variability in the expression of these genes and in the combinations of polymorphisms present in individual patients, and even in the significance and reproducibility of reported polymorphisms. Of the more than 100 genes that have been reported to be associated with the disease, relatively few have been replicated in multiple patient populations. Many of these affect the immune response or tissue remodeling. Some genes may influence the development of asthma, while others modify asthma severity or the patient's response to therapy.[36]
36. Moffat MF: Genes in asthma: new genes and new ways. Curr Opin Allergy Clin Immunol 2008; 8:411