MATERNAL MORTALITY
المرحلة الخامسة
–
رعاية صحية
م
.
د
.
ميادة كامل محمد
مدرس فرع طب االسرة والمجتمع
MATERNAL MORTALITY
Introduction
Definition
Determinants
Prevention
2
SOME FACTS
85 % women will deliver normally
10-15
% women will develop complications
3-5 % women will
need surgical interventions
(blood/Cesarean etc.)
More chances of
women having a normal delivery
However delivery complications can occur suddenly, without any
warning signals
3
SOME FACTS
20-25% deaths occur during pregnancy.
40-50% deaths occur during
labour and
delivery
25-40% deaths occur after childbirth
(
More during the first seven days)
It is important to focus attention during pregnancy and also
after childbirth
MATERNAL
MORTALITY
Death of a woman who is pregnant or within
42 days of termination of
pregnancy,
irrespective of the site or duration
of
pregnancy, from any cause related to or
aggravated
by
the
pregnancy
or
its
management
DIRECT OBSTETRIC DEATHS
The deaths resulting from obstetric
complications of the pregnant state
(pregnancy, labour and the puerperium), from
interventions, omissions, or incorrect
treatment, or from a chain of events
resulting from any of the above are called
direct obstetric deaths.
Indirect obstetric deaths
Those resulting from previous existing disease or disease that
developed during pregnancy and that was not due to direct
obstetric causes but was aggravated by the physiological effects
of pregnancy.
Late maternal death
Late maternal is death of a woman from direct or indirect obstetric
causes, more than 42 days but less than one year, after
termination of pregnancy.
Pregnancy related death
defined as : the death of a woman while pregnant or within
42 days of termination of pregnancy, irrespective of the
cause of death.
To facilitate the identification of maternal death in circumstances
in which cause of death attribution is inadequate, ICD-10
introduced a new category, that of
“pregnancy-related death”.
MEASUREMENT OF MATERNAL MORTALITY
There are three main measures of maternal
mortality-
maternal mortality ratio,
maternal mortality rate
lifetime risk of maternal death.
MATERNAL MORTALITY RATIO
This represents the risk associated with each
pregnancy, i.e. the obstetric risk.
It is calculated as the number of maternal
deaths during a given year per 100,000 live
births during the same period. This is usually
referred to as rate though it is a ratio.
NOTE - MMR
The appropriate denominator for the maternal
mortality ratio would be the
total number of
pregnancies
(live births, fetal deaths or stillbirths,
induced and spontaneous abortions, ectopic and
molar pregnancies).
However, this figure is seldom available and
thus number of live births is used as the
denominator.
In countries where maternal mortality is high
denominator used
is per 1000 live births but as this
indicator is reduced with better services, the
denominator used is per 1,00,000 live births to avoid
figure in decimals.
DELAY
Onset, time and death
APH-12 hours
PPH
– 02hours
Rupture uterus- 24 hours
Eclampsia
– 48 hours
Infection
– 06 days
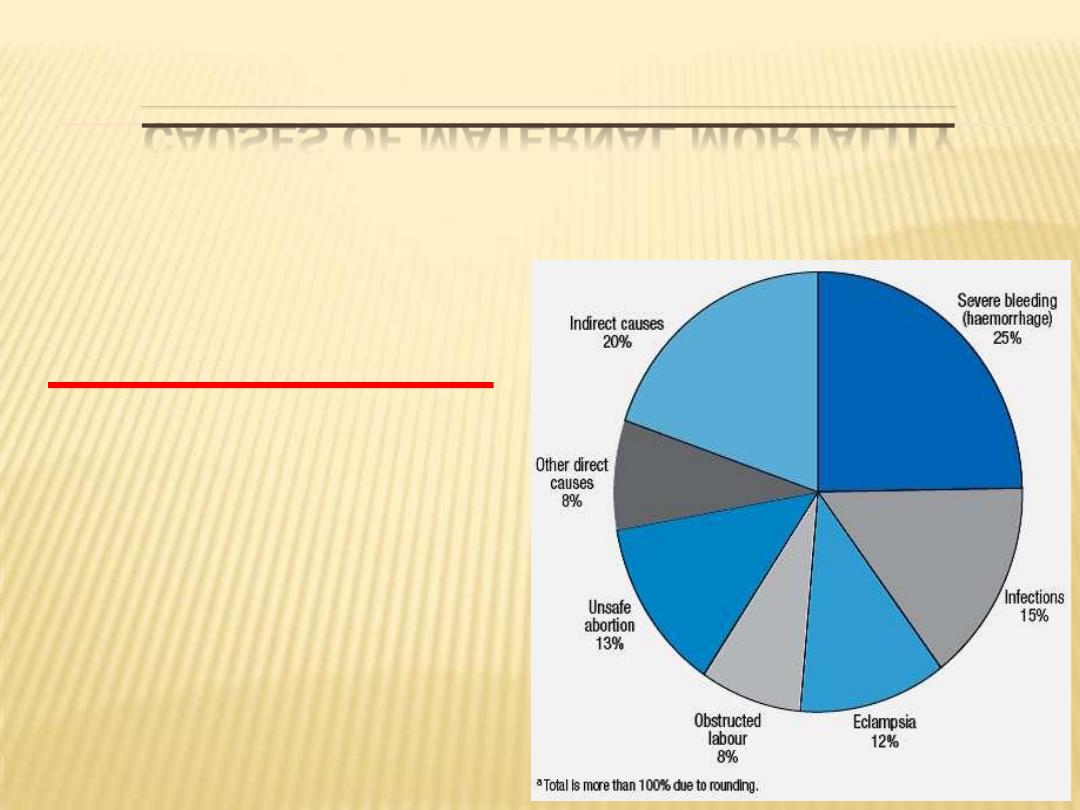
CAUSES OF MATERNAL MORTALITY
20 % - indirect
80 % - direct
Four Major causes
Haemorrhage
Infection (sepsis)
Eclampsia
Obstructed
Labour
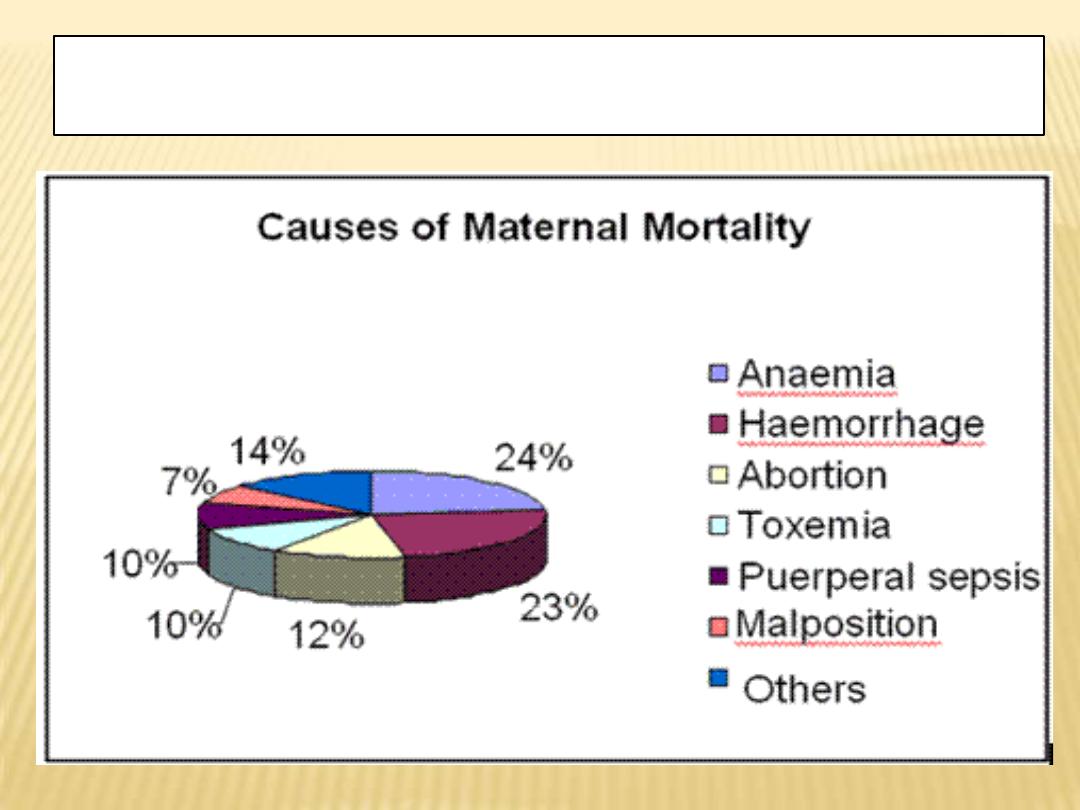
Source- Registrar General India. Causes of Maternal
Mortality in Rural India
UNDER LYING FACTORS
Socio-economic
Nutritional
IMPACT OF MATERNAL DEATHS
Children who lost their mothers are more likely
to die within two years of maternal death
10 times the chance of death for the neonate
7 times the chance of death for infants older
than one month
3 times the chance of death for children 1 to5
years
Enrolment in school for younger children is
delayed and older children often leave school to
support their family.
WHAT IS COMMON TO ALL THESE
CAUSES ?
They all are preventable to a great extent
IF THEY ARE ALL PREVENTABLE THEN
WHY NOT?
The reasons are
Social
Economical
Medical
SOCIAL ISSUES
Early marriage
Gender discrimination
Illiteracy
Desire for selective sex of child-
female feticide
Domestic violence
ECONOMIC ISSUES
Lack of money
Lack of timely transport and communication
Delay in taking decision to shift
Improper dietary habits
MEDICAL ISSUES
Lack of ANC
Lack of emergency obstetric care
Lack of blood and blood products
Lack of essential drugs
Junior staff dealing with high risk cases without
supervision
Delay in diagnosis / wrong diagnosis
PREVENTION OF MATERNAL MORTALITY
Health Education
Age at marriage
Utilization of services
Awareness of antenatal care
Nutritional education
Importance of Immunization
Spacing / Limitation of births
PREVENTION OF MATERNAL MORTALITY
Safe Abortion services
PREVENTION OF MATERNAL MORTALITY
Health delivery infrastructure
Improved staffing
Facilities for Essential / Emergency obstetric
care
Training of traditional birth attendants
( TBAs )
PREVENTION OF MATERNAL MORTALITY
Health care delivery
Emergency management of Eclampsia / Third
stage complications at PHC level
Flying squad services
PREVENTION OF MATERNAL MORTALITY
Adoption of small family norm
PREVENTION OF MATERNAL MORTALITY
Prevention of anaemia
Concept of 100 tablets
at puberty
at the time of marriage
during pregnancy
during lactation
FINAL MESSAGE
Child birth
– a miracle of life should not
become a nightmare of death
