The skin in systemic disease

The skin and internal
malignancy
acne seen with some adrenal tumours
flushing in the carcinoid syndrome
jaundice with a bile duct carcinoma
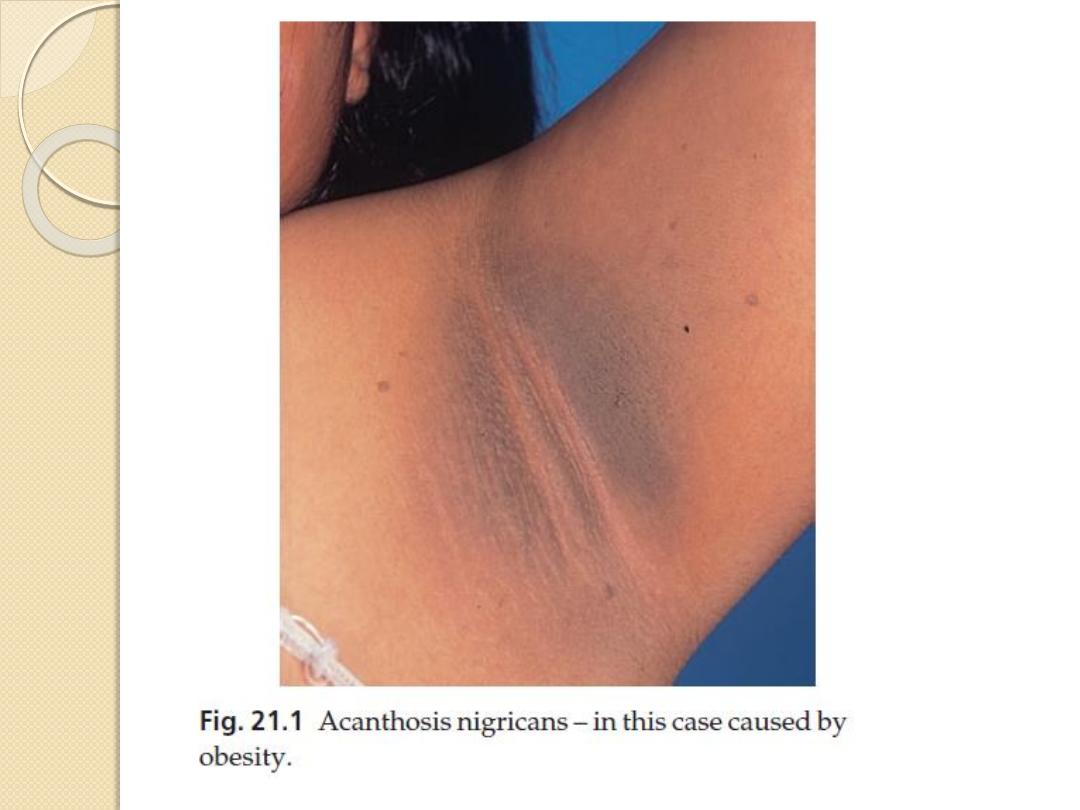
Acanthosis nigricans
is a velvety thickening and pigmentation of the major flexures
caused by:
obesity
metabolic syndrome (including type 2 diabetes with insulin
resistance)
Drugs as nicotinic acid used to treat hyperlipidaemia
the chances are high that a malignant tumour is present,
usually within the abdominal cavity.
Erythema gyratum repens
looks like the grain on wood

The skin and internal
malignancy
Acquired hypertrichosis lanuginosa (‘malignant down’)
is an excessive and widespread growth of fine lanugo hair.
Necrolytic migratory erythema
is a figurate erythema with a moving crusted edge it signals
the presence of a glucagonsecreting tumour of the pancreas.
Bazex syndrome
is a papulosquamous eruption of the fingers and toes, ears
and nose, seen with some tumours of the upper respiratory
tract.
Dermatomyositis, other than in childhood
About 30% of adult patients have an underlying malignancy.
Pay special attention to the ovaries where ovarian cancer
may lurk undetected.

The skin and internal
malignancy
Generalized pruritus
usually a lymphoma
Superficial thrombophlebitis.
the migratory type associated with carcinomas of the
pancreas.
Acquired ichthyosis
especially lymphomas
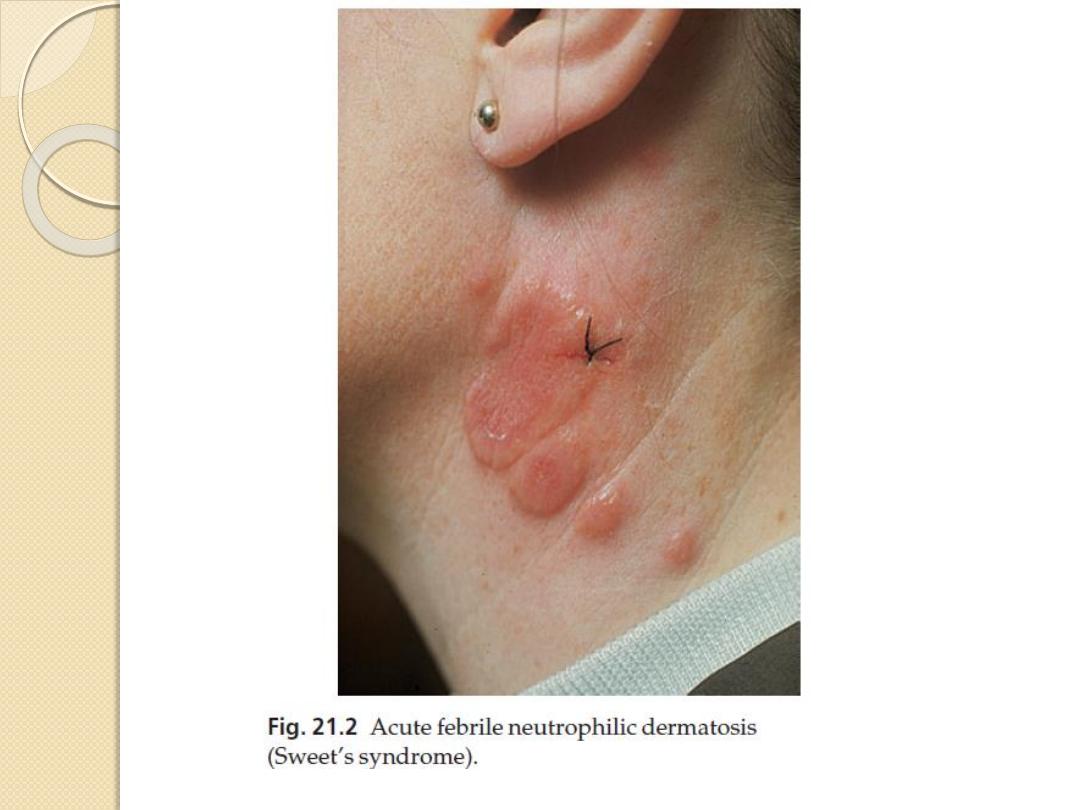
Acute febrile neutrophilic dermatosis (Sweet’s syndrome)
The classic triad found in association with the red
oedematous plaques consists of fever, a raised erythrocyte
sedimentation rate (ESR) and a raised blood neutrophil
count. The most important internal association is with
myeloproliferative disorders.

The skin and internal
malignancy
Paraneoplastic pemphigus
similar to pemphigus vulgaris but with
extensive and persistent mucosal
ulceration.
It is associated with myeloproliferative
malignancies as well as underlying
carcinomas.
Others. Pachydermoperiostosis
The skin and diabetes mellitus
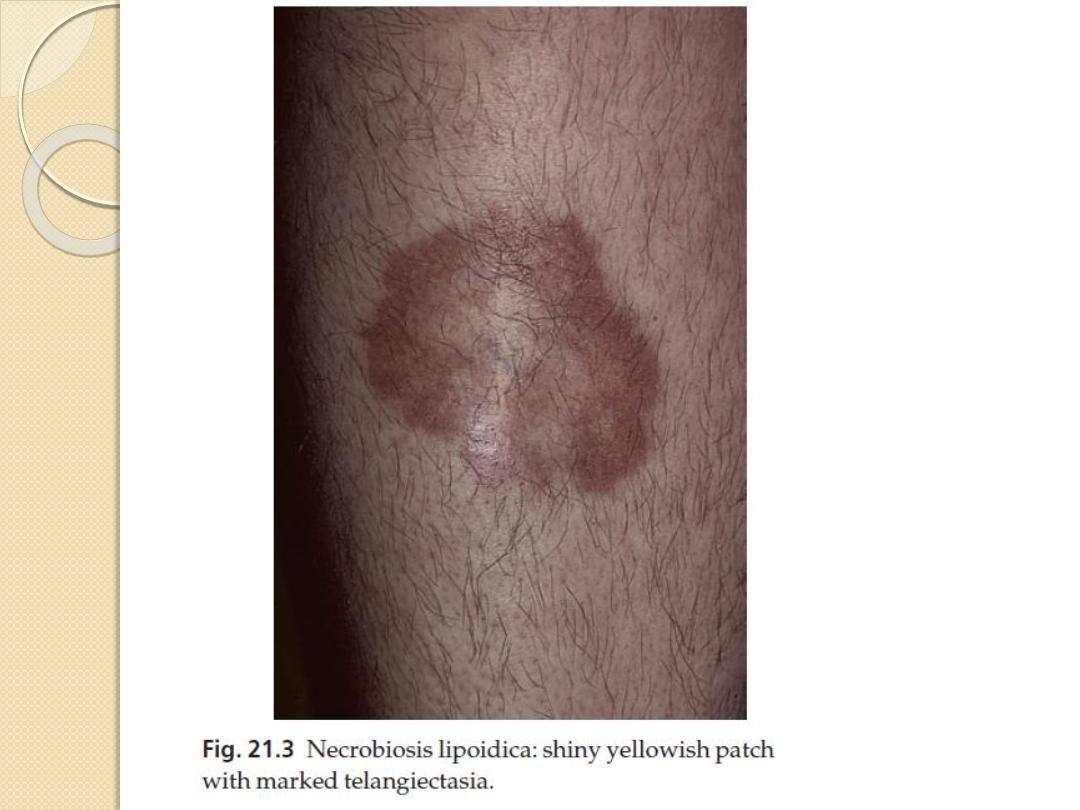
Necrobiosis lipoidica.
Less than 3% of diabetics have necrobiosis, but 11–62%
of patients with necrobiosis will have diabetes.
Non-diabetic necrobiosis patients should be screened
for diabetes as some will have impaired glucose
tolerance or diabetes, and some will become diabetic
later.
The association is with both type 1 and type 2
diabetes.
The lesions appear as one or more discoloured areas
on the fronts of the shins
Early plaques are violaceous but atrophy as the
inflammation goes on and are then shiny, atrophic and
brown–red or slightly yellow.
The skin and diabetes mellitus
The underlying blood vessels are easily seen through the
atrophic skin and the margin may be erythematous or violet.
Minor knocks or biopsy can lead to slow-healing ulcers
Treatment
No treatment is reliably helpful, the atrophy is permanent
the best one can expect from medical treatments is halting
of disease progression.
A strong topical corticosteroid applied to the edge of an
enlarging lesion may halt its expansion.
There is little evidence that good control of the diabetes will
help the necrobiosis.
The skin and diabetes mellitus
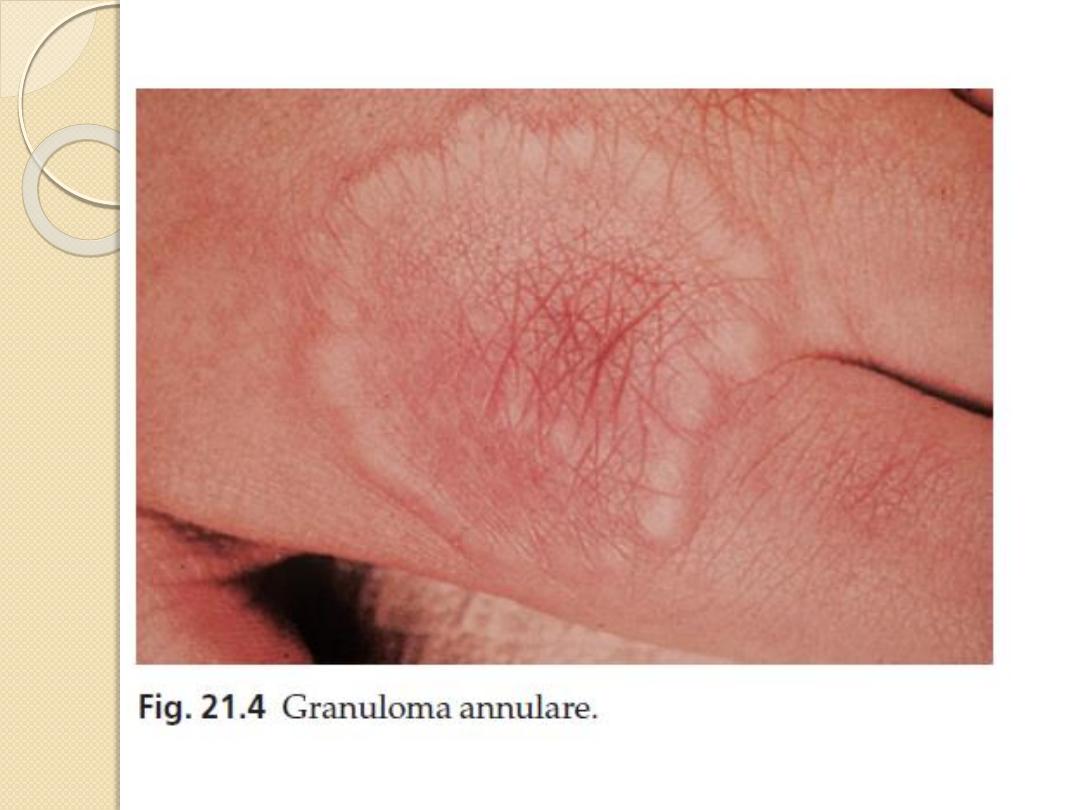
Granuloma annulare.
Clinically, the lesions of the common type of granuloma
annulare often lie over the knuckles and are composed of
dermal nodules fused into a rough ring shape
On the hands the lesions are skin-coloured or slightly pink;
elsewhere a purple colour may be seen.
histology shows a diagnostic palisading granuloma
Lesions tend to go away over the course of a year or two.
Stubborn ones respond to intralesional triamcinolone
injections.
Diabetic dermopathy
In about 50% of type 1 diabetics, multiple small (0.5–1 cm in
diameter) slightly sunken brownish scars can be found on the
limbs, most obviously over the shins.
The skin and diabetes mellitus
Candidal infections
Staphylococcal infections
Vitiligo
Eruptive xanthomas
Stiff thick skin (diabetic sclerodactyly or
cheiroarthropathy)
on the fingers and hands, demonstrated by the
‘prayer sign’ in which the fingers and palms
cannot be opposed properly
Atherosclerosis with ischaemia or gangrene of feet.
Neuropathic foot ulcers.
The skin in liver disease
Pruritus
This is related to obstructive jaundice and
may precede it
Pigmentation
With bile pigments and sometimes melanin
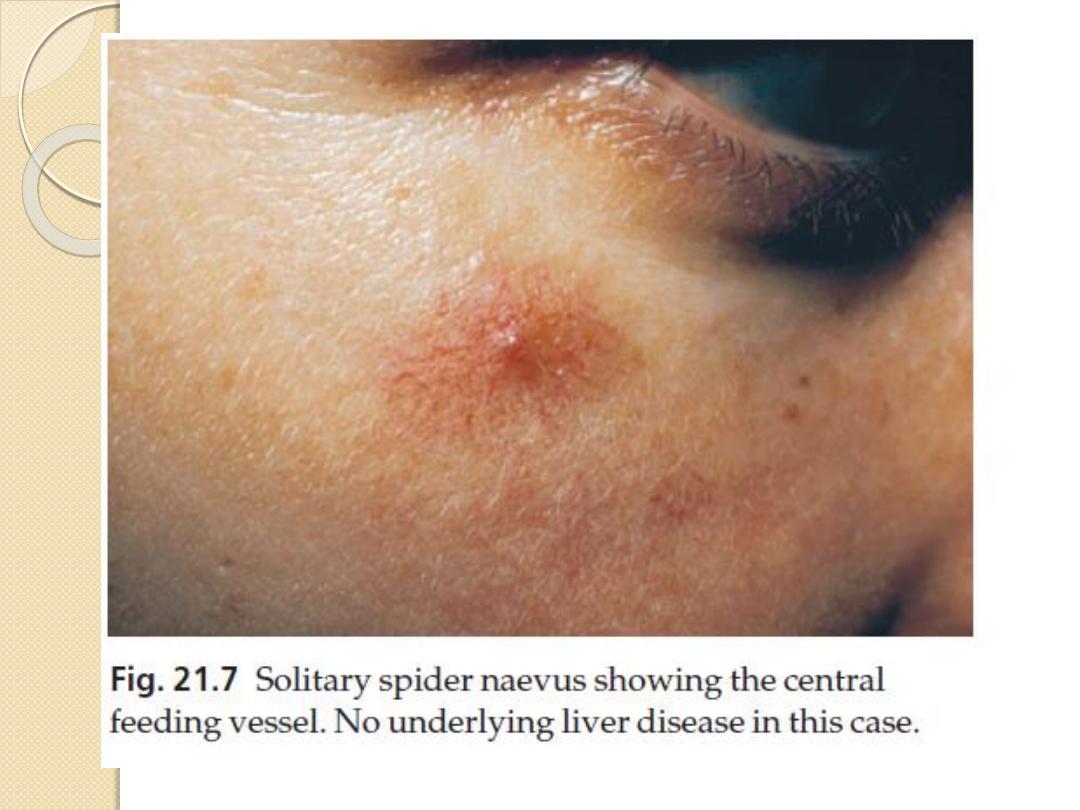
Spider naevi (These are often multiple in
chronic liver disease
Palmar erythema
White nails
These associate with hypoalbuminaemia
The skin in liver disease
Lichen planus and cryoglobulinaemia
with hepatitis C infection.
Polyarteritis nodosa with hepatitis B
infection.
Porphyria cutanea tarda .
Xanthomas With primary biliary
cirrhosis
Hair loss and generalized asteatotic
eczema may occur in alcoholics with
cirrhosis who have become zinc deficient.
The skin in renal disease
Pruritus and a generally dry skin.
Pigmentation A yellowish sallow colour
and pallor from anaemia.
Half-and-half nail The proximal half is
white and the distal half is pink or
brownish.
Perforating disorders Small papules in
which collagen or elastic fibres are being
extruded through the epidermis.
Pseudoporphyria
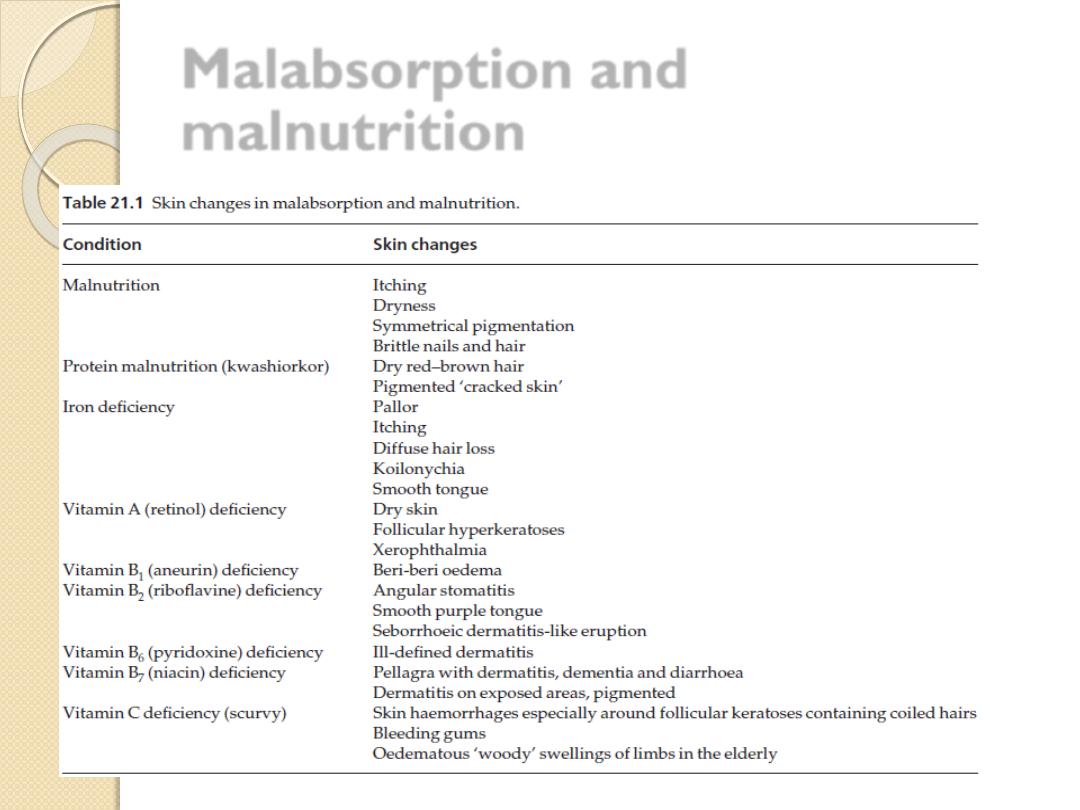
Malabsorption and
malnutrition
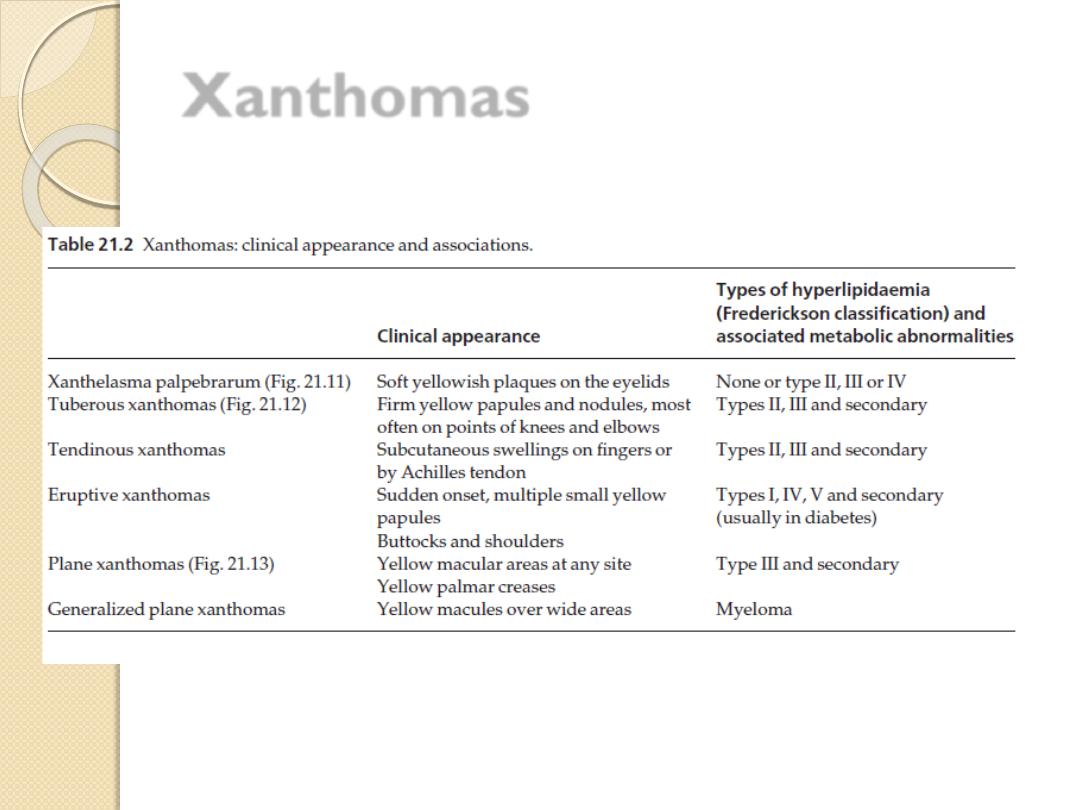
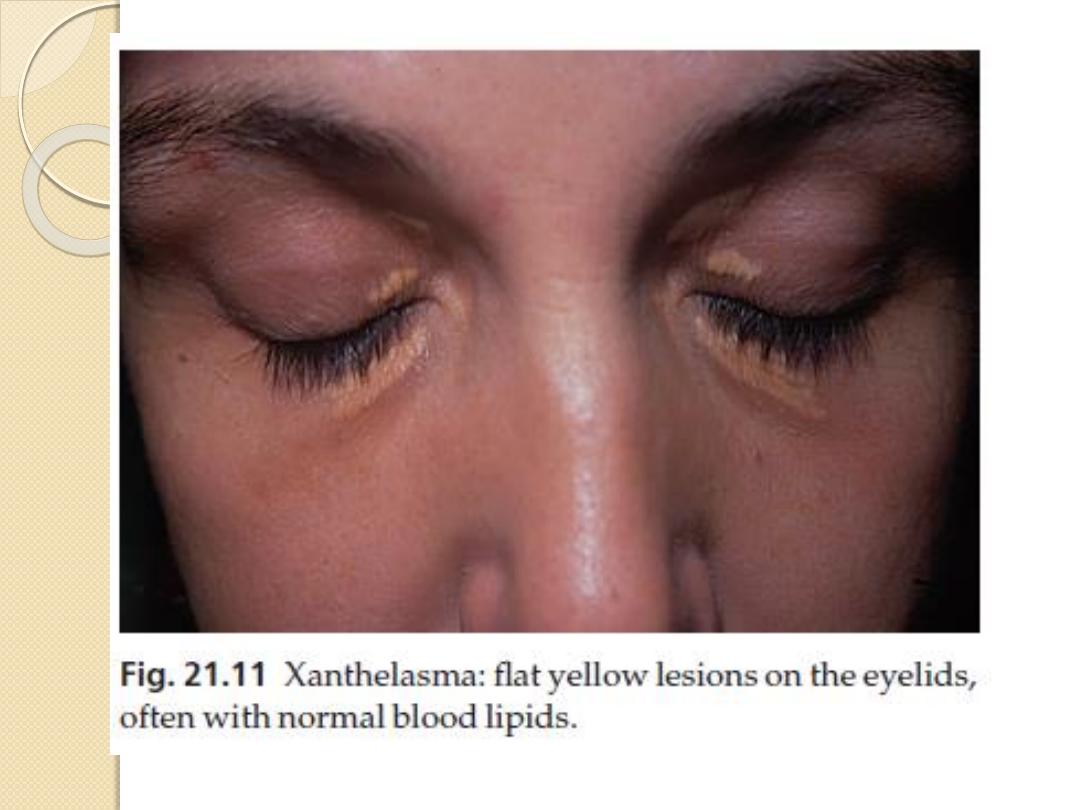
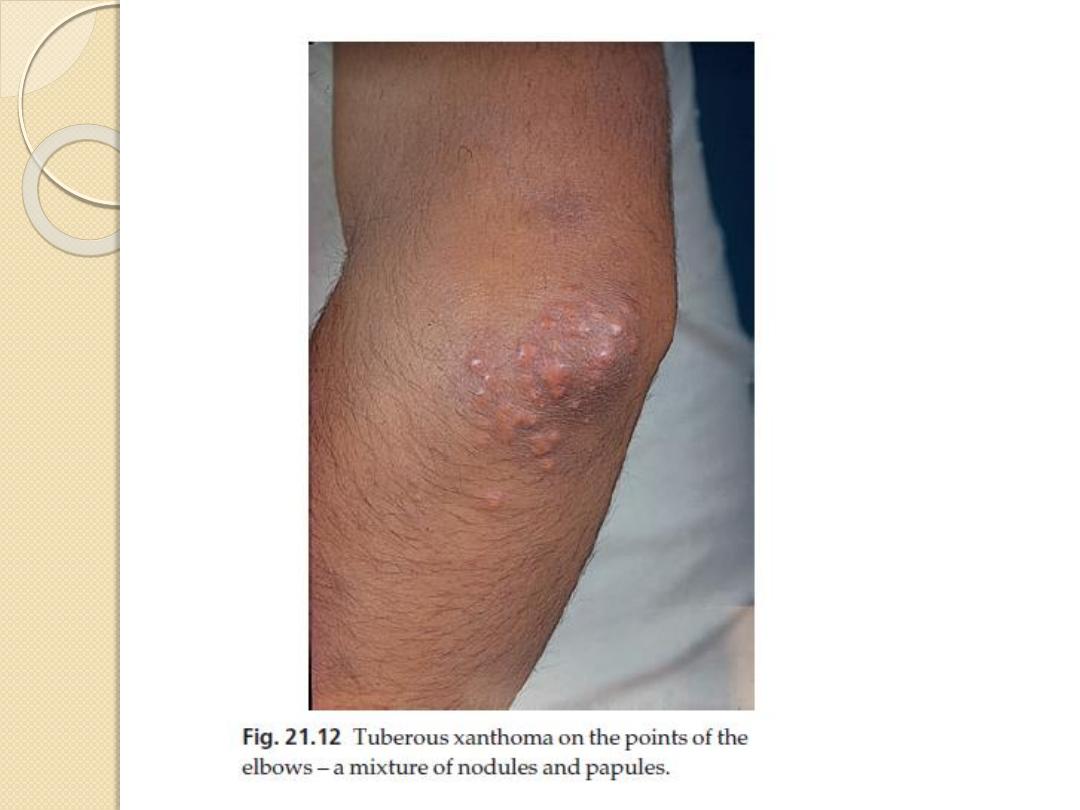
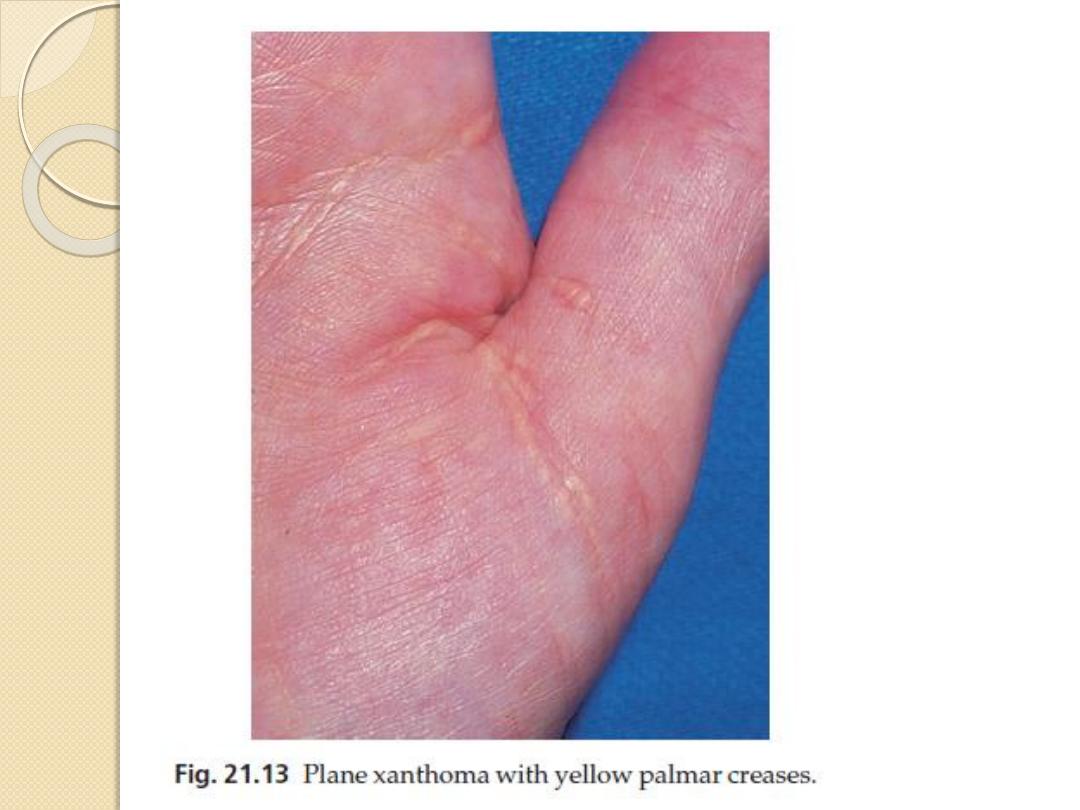
Xanthomas
Deposits of fatty material in the skin and
subcutaneous tissues (xanthomas) may provide
the first clue to important disorders of lipid
metabolism.
Primary hyperlipidaemias are usually genetic.
Secondary hyperlipidaemia can be found in a variety
of diseases including diabetes, primary biliary
cirrhosis, the nephrotic syndrome and
hypothyroidism.
Lipid-regulating drugs (e.g. statins and fibrates)
not only stop xanthomas from appearing, but they
also allow them to resolve.
Xanthomas
Generalized pruritus
Pruritus is a symptom with many causes, but not
a disease in its own right.
Itchy patients fall into two groups:
1.
those whose pruritus is caused simply by
surface causes (e.g. eczema, lichen planus and
scabies)
2.
those who may or may not have an internal
cause for their itching. These patients require a
detailed physical examination, including a careful
search for lymphadenopathy
Investigations including a full blood count, iron
status, urea and electrolytes, liver function tests,
thyroid function tests and a chest X-ray
Causes
Liver disease
Itching signals biliary obstruction.
It is an early symptom of primary biliary cirrhosis.
Colestyramine may help cholestatic pruritus, possibly
by promoting the elimination of bile salts.
Other treatments include naltrexone, rifampicin and
ultraviolet B.
Chronic renal failure
Ultraviolet B phototherapy, naltrexone or
administration of oral activated charcoal may help.
Iron deficiency
Treatment with iron may help the itching.
Causes
Polycythaemia
The itching here is usually triggered by a hot bath; it has a
curious pricking quality and lasts about an hour.
Thyroid disease
Itching and urticaria may occur in hyperthyroidism.
The dry skin of hypothyroidism may also be itchy.
Diabetes
Internal malignancy
The prevalence of itching in Hodgkin’s disease may be as high
as 30%.
It may be unbearable, yet the skin often looks normal.
Pruritus may occur long before other manifestations of the
disease.
Itching is uncommon in carcinomatosis.
Causes
Neurological disease
Paroxysmal pruritus has been recorded in multiple sclerosis
and in neurofibromatosis.
Brain tumours infiltrating the floor of the fourth ventricle may
cause a fierce persistent itching of the nostrils.
Diffuse scleroderma
may start as itching associated with increasing pigmentation
and early signs of sclerosis.
Itching is usually severe
The skin of the elderly may itch because it is too dry, or
because it is being irritated.
Pregnancy
Drugs
Treatment
Therapy is symptomatic and consists of
sedative antihistamines
skin moisturizers, and the avoidance of
rough clothing, overheating and
vasodilatation, including that brought on by
alcohol.
Ultraviolet B often helps all kinds of itching,
including the itching associated with chronic
renal and liver disease.
Local applications include calamine and
mixtures containing small amounts of
menthol or phenol
THE END
THANKS
