Disorders of pigmentation
Normal skin colour
The colour of normal skin comes from a mixture of
pigments
1.
pink by oxyhaemoglobin in the blood within the dermis.
2.
brown of melanin
3.
yellow from carotene mainly in subcutaneous fat and in
the horny layer of the epidermis.
There is no natural blue pigment
Hair colour is determined by the relative amounts of the
different types of melanin. Eumelanin predominates in
black hair and phaeomelanin in red.

Melanogenesis
Melanin is formed from the essential aminoacid
phenylalanine through a series of enzymatic steps in the
liver and skin.
Melanin is made within melanosomes
fully melanized melanosomes pass into the dendritic
processes of the melanocyte to be injected into
neighbouring keratinocytes and distributed throughout
the cytoplasm.
Skin color depend on nummber and size of melanosomes
Melanins protect against UVR damage by absorbing and
scattering the rays, and by scavenging free radicals.
Control of melanogenesis
Melanogenesis can be increased by several stimuli:
1.
UVR is the most important
2.
Melanocytestimulating hormone (MSH) peptides from
the pituitary and other areas of the brain
3.
Oestrogens and progestogens (and possibly
testosterone too) may stimulate melanogenesis, either
directly (by acting on oestrogen and progestogen
receptors in the melanocyte) or by increasing the
release of MSH peptides from the pituitary
Tanning
involves two distinct reactions.
A-Immediate pigment darkening (IPD) following exposure
to longwave ultraviolet (UVA 320–400 nm).
This pigment darkening occurs over minutes to days
responsible for the well-known phenomenon of a ‘false tan’.
It is not brought about by melanin synthesis but oxidation of
preformed melanin and redistribution of melanin from
perinuclear melanosomes to peripheral dendrites.
B-Delayed tanning (DT): the production of new pigment
occurs some 3–4 days after exposure to medium-wave
ultraviolet (UVB: 290–320 nm) and UVA and is maximal at 7
days
Genetics and skin pigmentation
Genetic differences determine the pigmentation of the
different races
A black person living in Britain and a white person living
in Africa will remain black and white, respectively
Abnormal skin colours
These may be caused by:
1.
Imbalance of the normal pigments
2.
Presence of abnormal pigments
Some abnormal pigments
Endogenous
Haemoglobin-derived
Methaemoglobin, Sulphaemoglobin - Blue
colour in vessels, cyanosis
Carboxyhaemoglobin -Pink
Bilirubin, Biliverdin -Yellow–green
Haemosiderin- Brown
Drugs
Gold- Blue-grey (chrysiasis)
Silver -Blue-grey (argyria)
Amiodarone- Blue-grey
Bismuth -Grey
Mepacrine- Yellow
Clofazamine- Red
Phenothiazines- Slate-grey
Diet
Carotene Orange
Exogenous
Tattoo pigments
Local medications
•
Silver nitrate- Black
•
Magenta paint- Magenta
•
Gentian violet- Violet
•
Eosin- Pink
•
Potassium permanganate-
Brown
•
Dithranol (anthralin)- Purple
•
Tar- Brown
•
Iodine- Yellow
Decreased melanin pigmentation
Some causes of hypopigmentation.
Genetic
Albinism
Piebaldism
Phenylketonuria
Waardenburg’s syndrome
Chediak–Higashi syndrome
Tuberous sclerosis
Endocrine
Hypopituitarism
Chemical
Contact with substituted phenols
(in rubber industry) Chloroquine
and hydroxychloroquine
Post-inflammatory
•
Eczema
•
Pityriasis alba
•
Psoriasis
•
Sarcoidosis
•
Lupus erythematosus
•
Lichen sclerosus et atrophicus
•
Cryotherapy
Infections
•
Leprosy
•
Pityriasis versicolor
•
Syphilis, yaws and pinta
Tumours
•
Halo naevus
•
Malignant melanoma
Miscellaneous
•
Vitiligo
•
Idiopathic guttate hypomelanosis
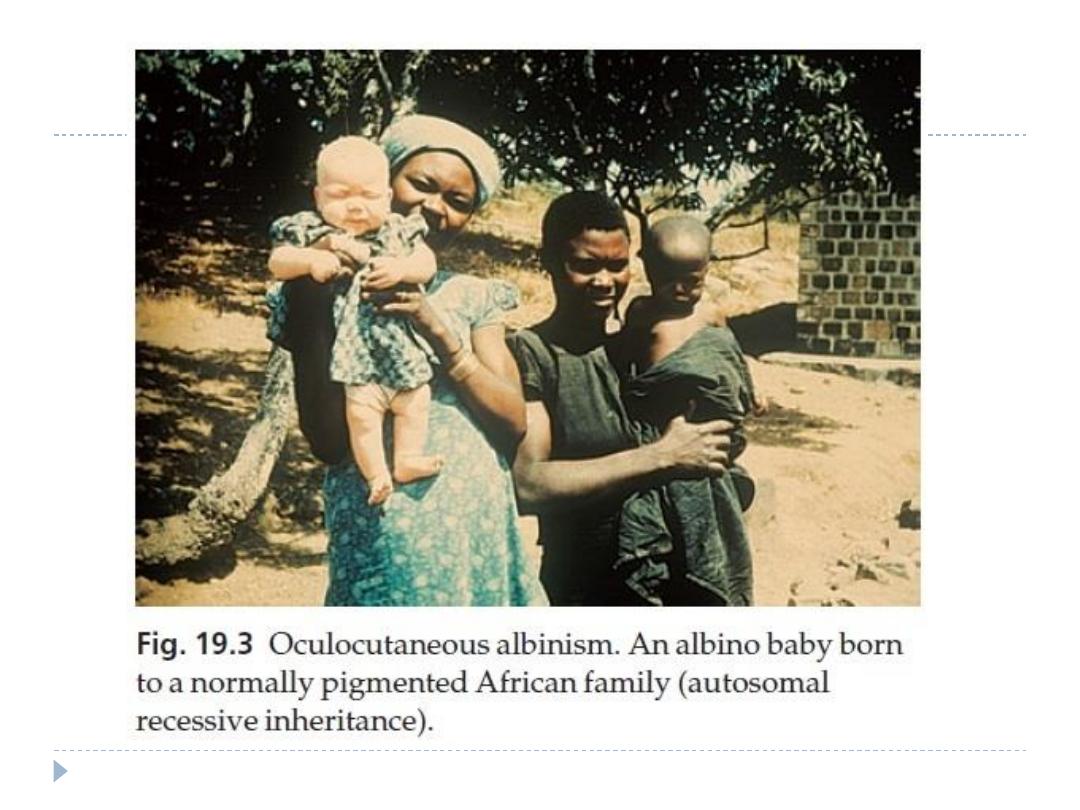
Oculocutaneous albinism
genetic conditions in which there is a defect in the synthesis of
melanin in the melanocyte, or a defective transfer of
melanosomes to surrounding keratinocytes
Types
1.
skin and eyes (oculocutaneous albinism)
2.
eyes alone (ocular albinis)
Cause
oculocutaneous albinism of two main types:
1.
tyrosinase negative, lies on chromosome 11q14- q21
2.
tyrosinase positive, mapped to chromosome 15q11- q13
both being inherited as autosomal recessive traits. This
explains how children with two albino parents can sometimes
themselves be normally pigmented, the genes being
complementary in the double heterozygote
Presentation and course
The whole epidermis is white
Albinos have poor sight, photophobia and a rotatory
Nystagmus as pigment is also lacking in the hair, iris and
retina
As they grow older, tyrosinasepositive albinos gain a little
pigment in their skin, iris and hair, also develop freckles.
Sunburn is common on unprotected skin.
As melanocytes are present, albinos have non-pigmented
melanocytic naevi and may develop amelanotic malignant
melanomas.
Complications
sun-induced skin cancers even when they are young,
confirming the protective role of melanin
Differential diagnosis
Piebaldism and vitiligo
Investigations
Prenatal diagnosis of albinism is now possible
The hair bulb test to distinguishes tyrosinase-positive from
tyrosinase-negative types.
Treatment
Avoidance of sun exposure and protection with opaque
clothing, wide-brimmed hats and sunscreen creams are
essential and allow albinos in temperate climates to live a
relatively normal life.
Early diagnosis and treatment of skin tumours is critical.
Piebaldism
a white forelock of hair
patches of depigmentation lying symmetrically on the
limbs, trunk and central part of the face, especially the
chin.
present at birth
inherited as an autosomal dominant
Melanocytes are absent from the hypopigmented areas.
The depigmentation, often mistaken for vitiligo, may
improve with age.
There is no effective treatment.
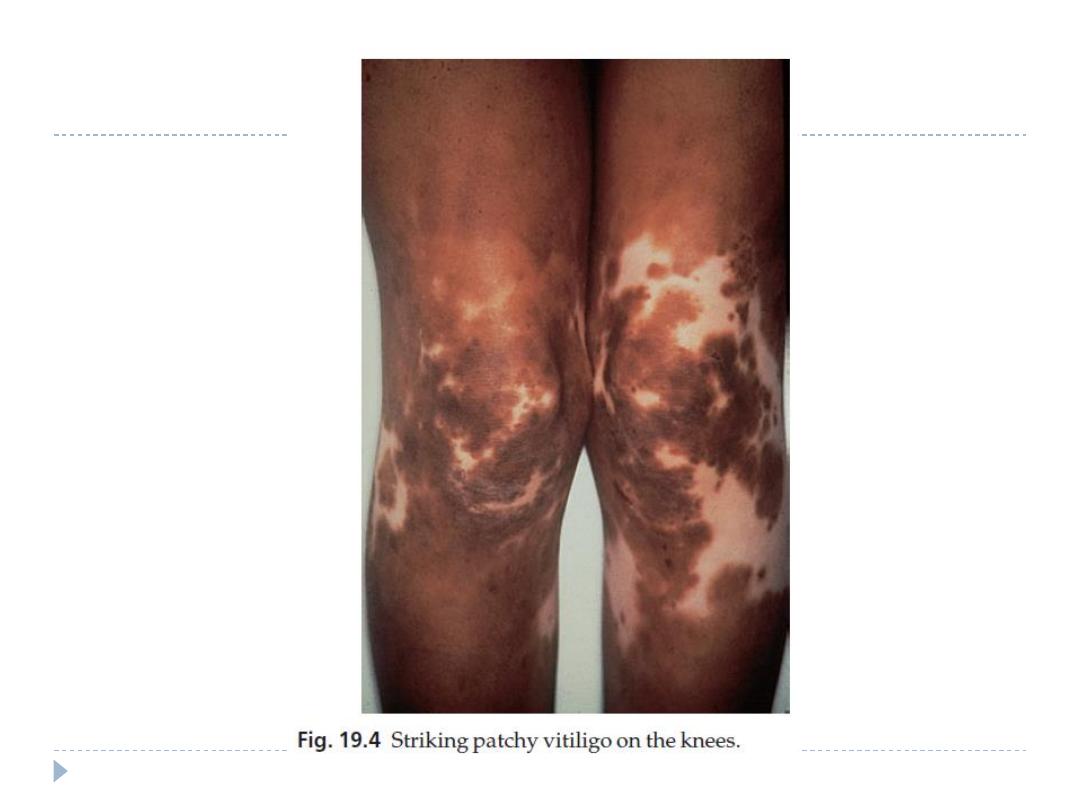
Vitiligo
The word vitiligo comes from the Latin word vitellus meaning
‘veal’ (pale, pink flesh).
It is an acquired circumscribed depigmentation, found in all
races
its inheritance is polygenic.
Cause and types
There is a complete loss of melanocytes from affected areas.
There are two main patterns:
1.
Generalized
2.
Segmental, rare
Trauma and sunburn can precipitate both types.
Generalized vitiligo
including the acrofacial variant
Is a common type
usually starts after the second decade
positive family history in 30% of patients
associated with autoimmune diseases such as diabetes,
thyroid disorders and pernicious anaemia.
in this type, melanocytes are the target of a cell-mediated
autoimmune attack or self-destruct because of an inability
to remove toxic melanin precursors.
Segmental vitiligo
is restricted to one part of the body, but not necessarily
to a dermatome.
It occurs earlier than generalized vitiligo
not associated with autoimmune diseases
Clinical course
Generalized type
sharply defined, usually symmetrical white patches are especially
common on the backs of the hands, wrists, fronts of knees, neck and
around body orifices.
The hair of the scalp and beard may depigment too. In
Caucasoids, the surrounding skin is sometimes partially depigmented
or hyperpigmented (trichrome vitiligo).
The course is unpredictable: lesions may remain static or spread,
sometimes following minor trauma (Köbner phenomenon)
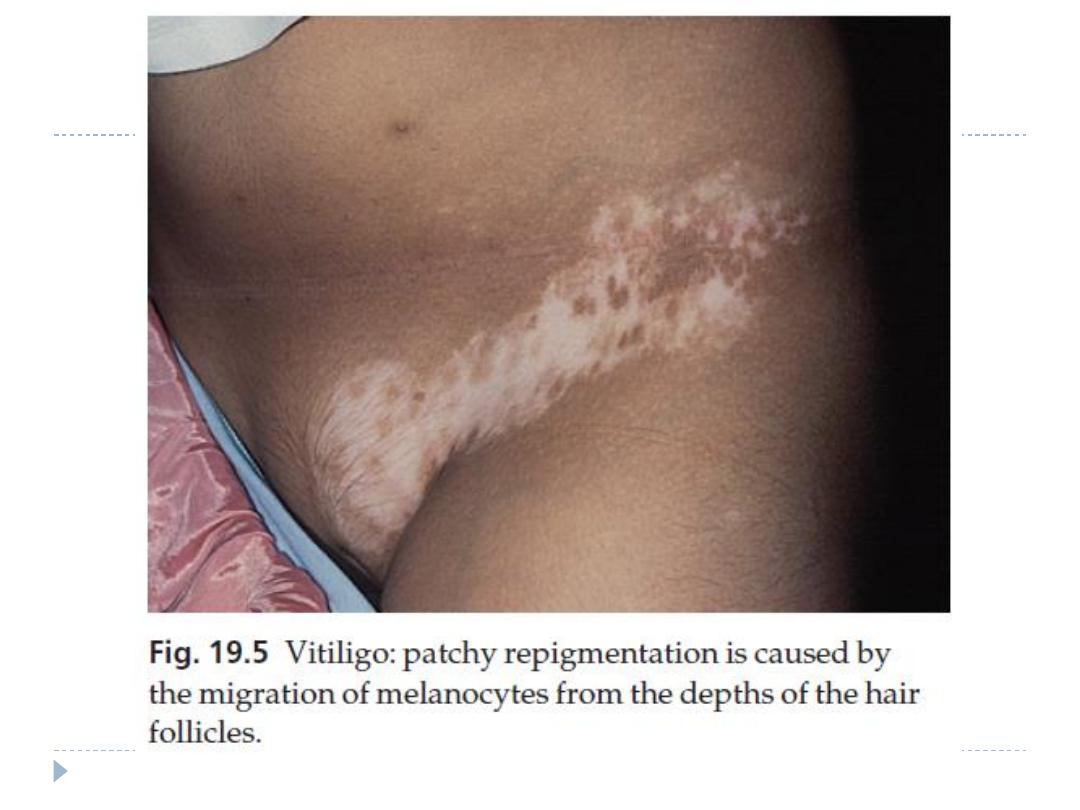
they repigment spontaneously from the hair follicles.
Segmental type
look like the generalized type but their segmental distribution is
striking.
Spontaneous repigmentation occurs more often in this type than in
generalized vitiligo
Differential diagnosis
1.
Contact with depigmenting chemicals, such as
hydroquinones and substituted phenols in the rubber
industry
2.
Pityriasis versicolor
3.
Post-inflammatory depigmentation
4.
patches of piebaldism
5.
Leprosy must be excluded
6.
leishmaniasis and pinta.
Treatment
Treatment is unsatisfactory
The cosmetic disfigurement from vitiligo can be
devastating to affected paients..
In the white patches pigment cells are only present deep
in the hair follicles and treatments mostly try to get
melanocytes to divide and migrate into affected skin.
Repigmentation is thus often heralded by freckling at
follicles within patches
Recent patches
1.
Potent or very potent topical corticosteroid, applied
for 1–2 months. After this, the strength should be gradually
tapered to a mildly potent steroid for maintenance
treatment.
2.
Alternatively, calcineurin inhibitors, such as 0.1%
tacrolimus ointment
3.
Psoralens (trimethylpsoralen or 8-methoxypsoralen, in a
dosage of 0.4–0.6 mg/kg body weight), taken 1–2 h before
graduated exposure to natural sunshine or to artificial UVA
4.
Narrow-band (311 nm) UVB may also be effective
New lesions seem to respond best.
1.
Less reliable treatments include excimer laser and
antioxidant therapy
2.
Autologous skin grafts if pigment is absent in hair follicles
or skin without hair follicles
Established vitiligo
As a general rule,it is best left untreated in most white
people
Advice about suitable camouflage preparations
Sun avoidance and screening preparations are needed to
avoid sunburn of the affected areas and a heightened
contrast between the pale and dark areas.
Black patients with extensive vitiligo can be completely
and irreversibly depigmented
Post-inflammatory depigmentation
1.
Eczema
2.
Psoriasis
3.
Sarcoidosis
4.
Lupus erythematosus
5.
lichen planus
6.
cryotherapy or a burn
In general, the more severe the inflammation, the more likely
pigment is to decrease rather than increase
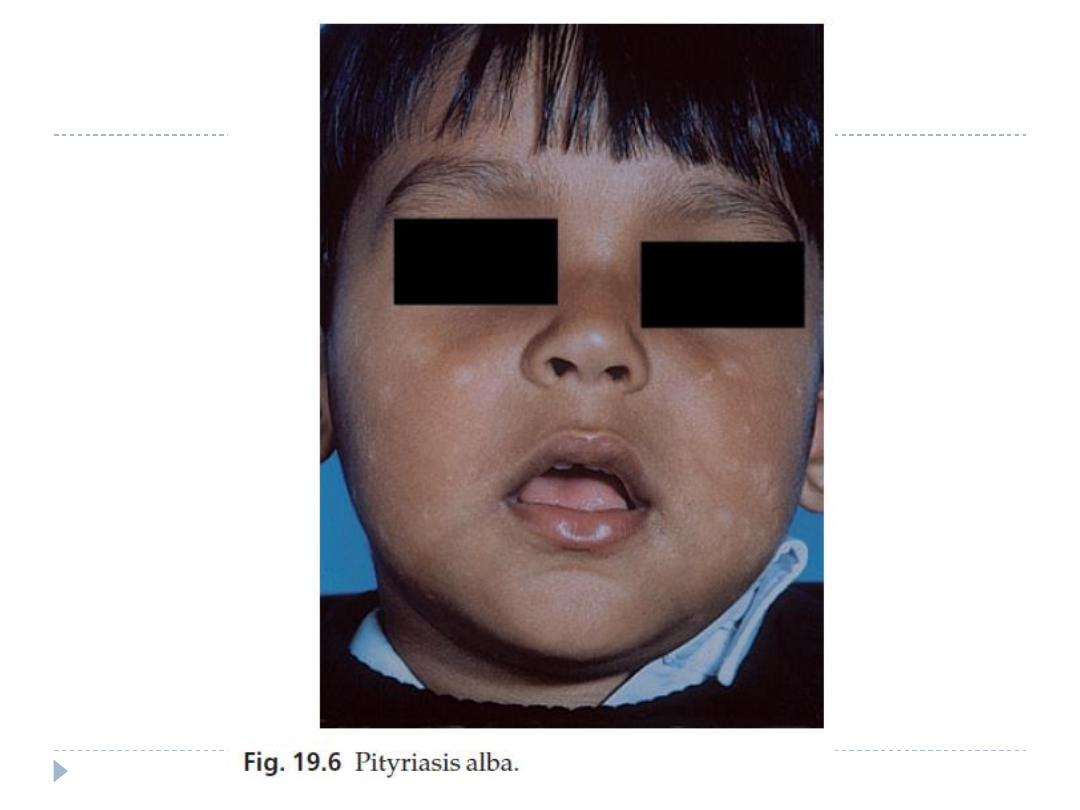
Pityriasis alba
is common on the faces of children.
The initial lesion is probably a variant of eczema (pinkish with fine
scaling), which fades leaving one or more pale, slightly scaly, areas.
Exposure to the sun makes the patches more obvious.
Disorders with increased pigmentation
(hypermelanosis)
Some causes of hyperpigmentation.
Genetic
Freckles
Lentigines
Café au lait macules
Peutz–Jeghers syndrome
Xeroderma pigmentosum
Endocrine
Addison’s disease
Cushing’s syndrome
Pregnancy
Renal failure
Metabolic
Biliary cirrhosis
Haemochromatosis
Porphyria
Nutritional
Malabsorption
Carcinomatosis
Kwashiorkor
Pellagra
Drugs
•
Photosensitizing drugs
•
ACTH and synthetic analogues
•
Oestrogens and progestogens
•
Psoralens
•
Arsenic
•
Busulfan
•
Minocycline
Post inflammatory
•
Lichen planus
•
Eczema
•
Secondary syphilis
•
Systemic sclerosis
•
Lichen and macular amyloidosis
•
Cryotherapy
•
Poikiloderma
Tumours
•
Acanthosis nigricans
•
Pigmented naevi
•
Malignant melanoma
•
Mastocytosis
Freckles (ephelides)
so common that to describe them seems unnecessary
They are seen most often in the redhaired or blond
person as sharply demarcated, light brown–ginger
macules, usually less than 5 mm in diameter.
They multiply and become darker with sun exposure.
Increased melanin is seen in the basal layer of the
epidermis without any increase in the number of
melanocytes, and without elongation of the rete ridges
No treatment is necessary.
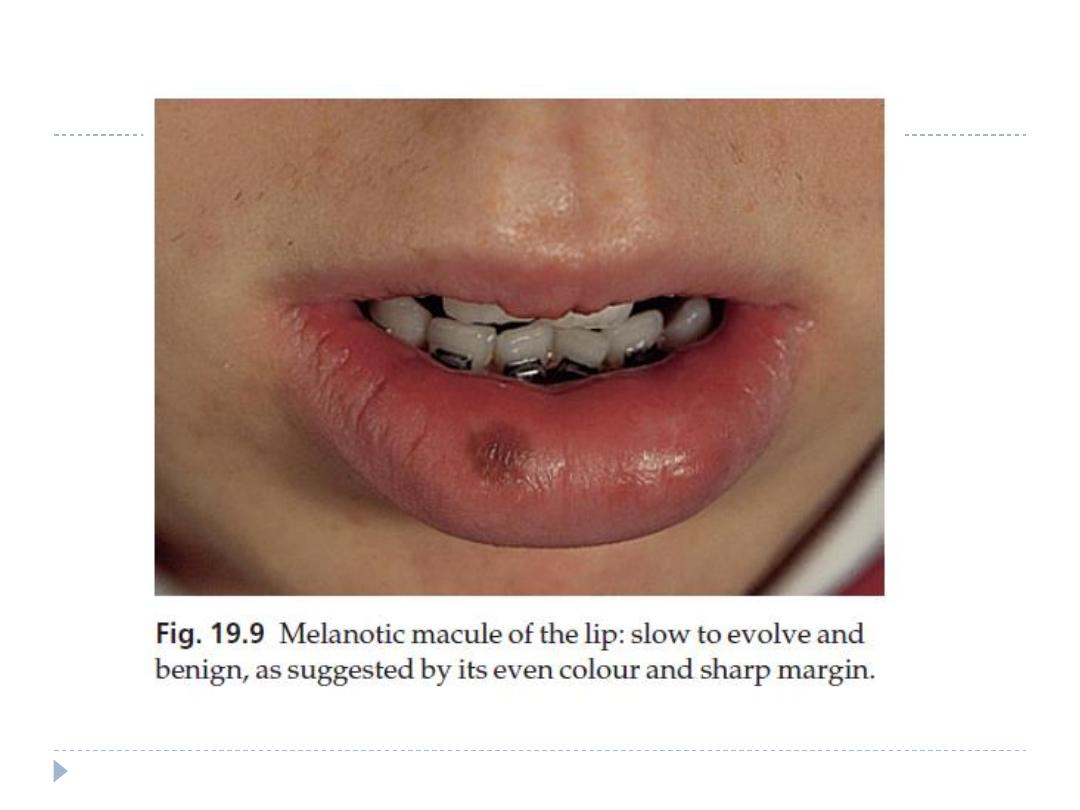
Lentigo
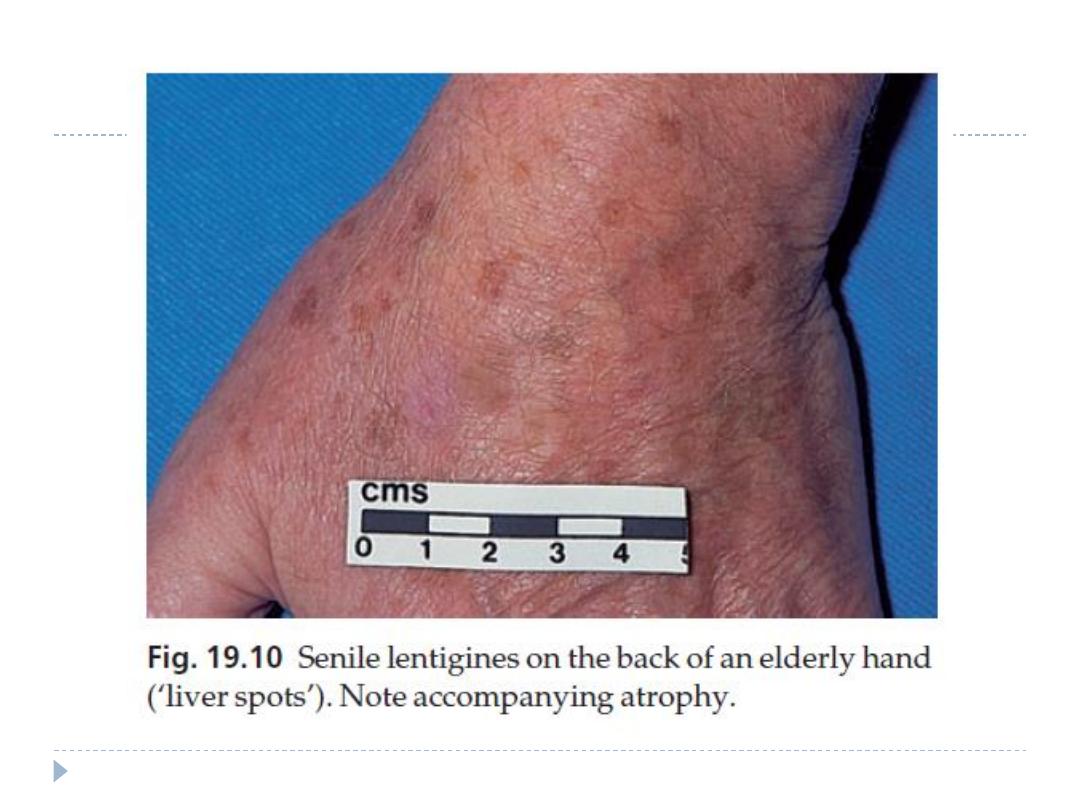
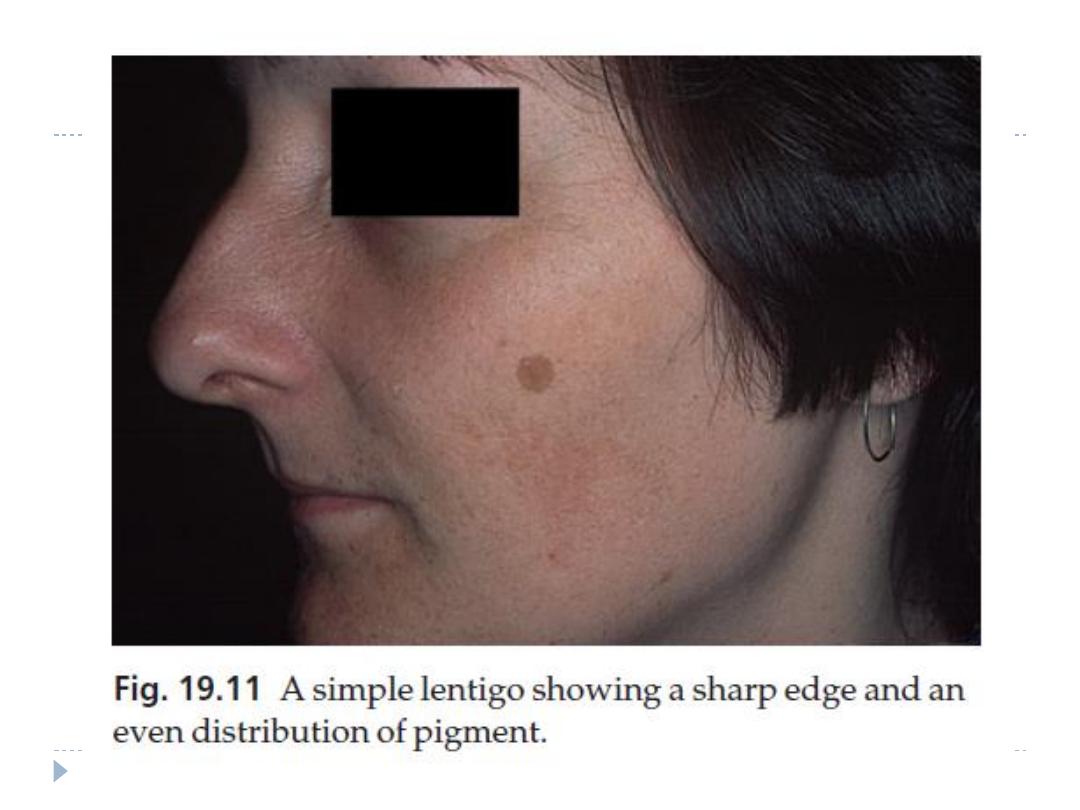
Simple and senile lentigines look alike.
They are light or dark brown macules, ranging from 1 mm to 1 cm across.
Are usually discrete, and may have an irregular outline.
Simple lentigines arise most often in childhood as a few scattered lesions, often
on areas not exposed to sun, including the mucous membranes.
Senile or solar lentigines are common after middle age on the backs of the
hands (‘age spots’, ‘liver spots’and on the face
lentigines have increased numbers of melanocytes.
They should be distinguished from a lentigo maligna
Treatment is usually unnecessary and prevention, by sun avoidance and the use of
sunscreens is the best approach.
cryotherapy
laser
daily application of 0.1% tretinoin cream or 2–4% hydroquinone or a combination
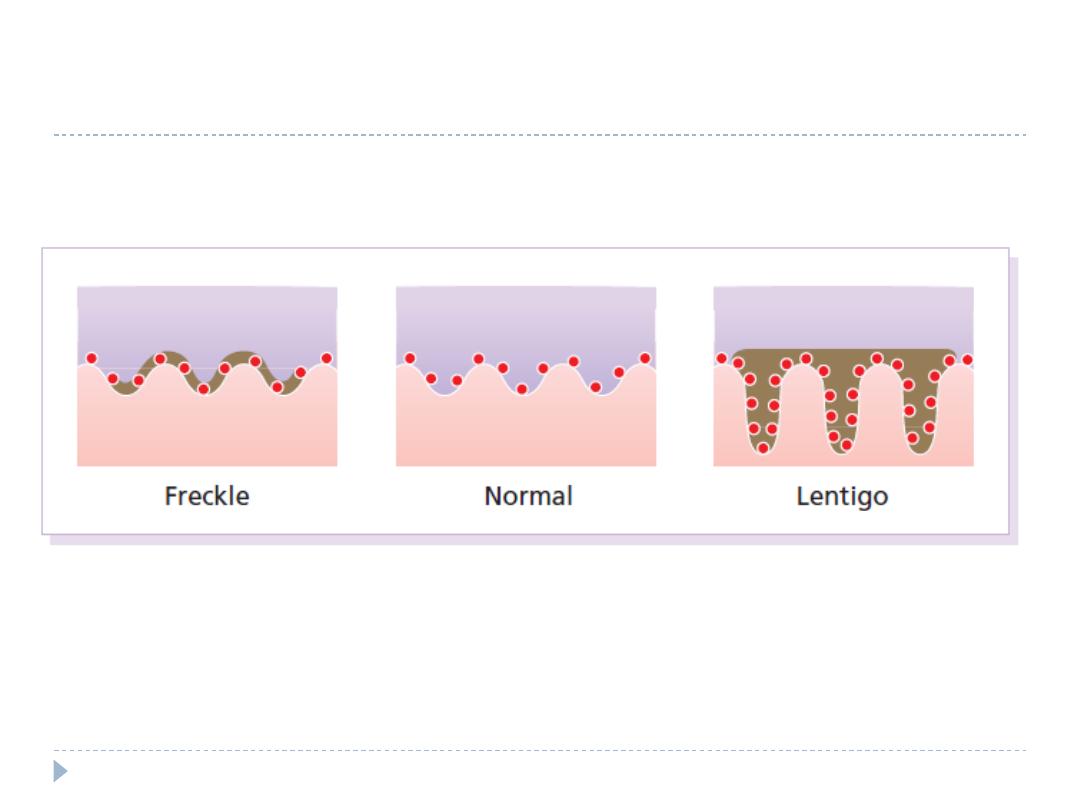
Histology of a freckle and lentigo
Conditions associated with multiple
lentigines
1.
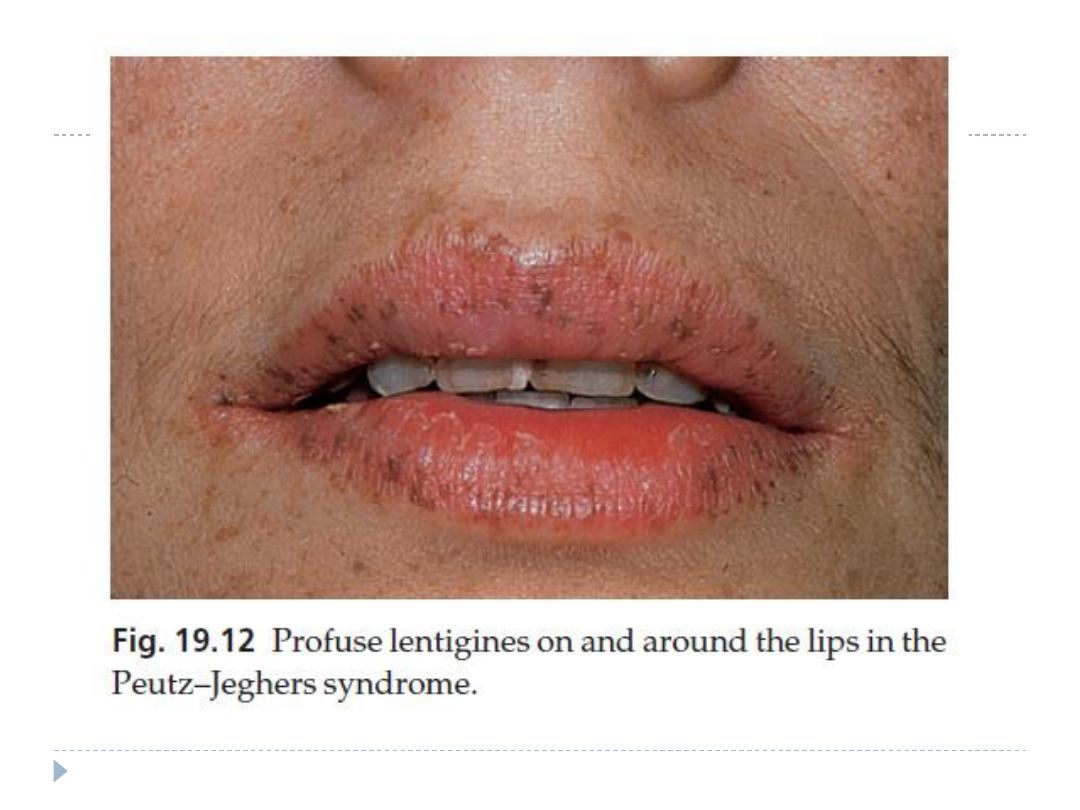
Peutz–Jeghers syndrome
autosomal dominant condition
Scattered lentigines also occur on the buccal mucosa,
gums, hard palate, hands and feet.
association with polyposis of the small intestine
10 % of affected women have ovarian tumours.
2.
Cronkhite–Canada syndrome
3.
LEOPARD syndrome
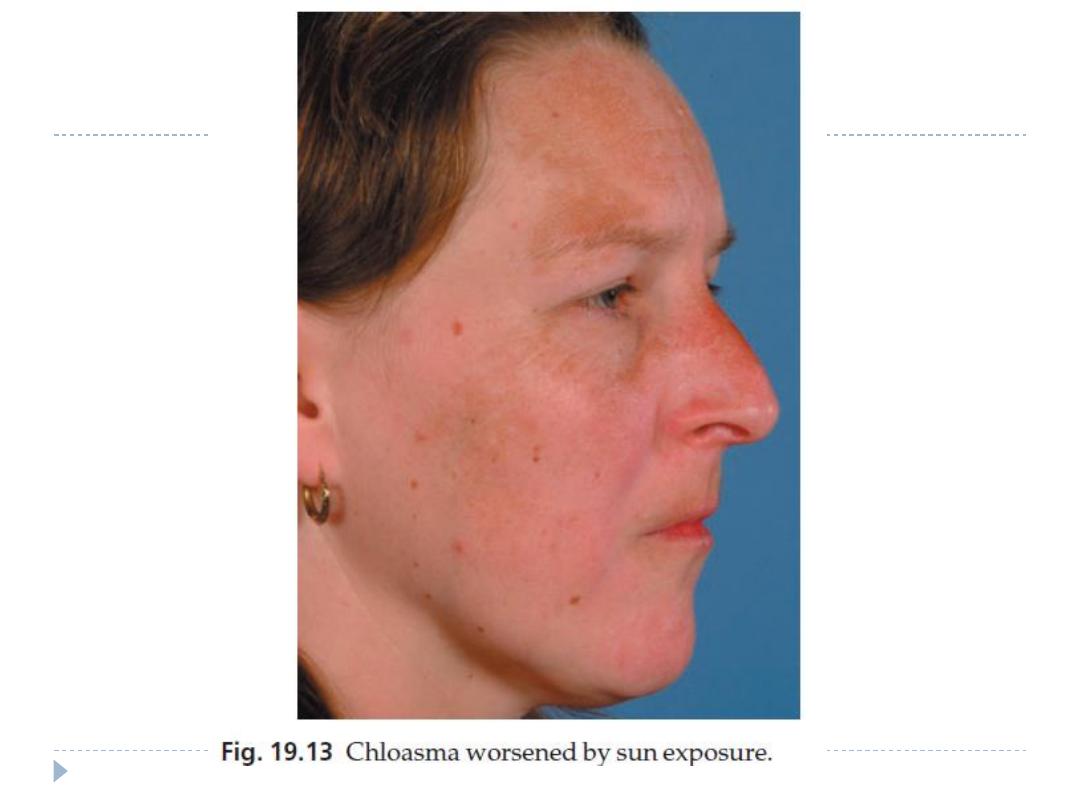
Melasma (chloasma)
acquired, symmetrical hypermelanosis occurring on sun-exposed
skin, especially the face.
The areas of increased pigmentation are well defined and their
edges may be scalloped.
more common in women, affects all races but is most prevalent in
dark-skinnned individuals with skin types IV–VI
hypermelanosis becomes darker after exposure to the sun.
There are many causes including:
1.
Sunlight
2.
pregnancy ‘the mask of pregnancy’
3.
oestrogens and oral contraceptives
4.
thyroid dysfunction
5.
photosensitizing drugs
The placenta may secrete sex hormones that stimulate melanocytes.
Melasma Treatment
This is unsatisfactory
sunscreen
bleaching agents that contain 2–5% hydroquinone, applied
for 6–10 weeks.
Chemical peels
Endocrine hyperpigmentation
Addison’s disease
caused by the overproduction of ACTH
generalized or limited to the skin folds, creases of the palms,
scars and the buccal mucosa.
Cushing’s syndrome
Increased ACTH production may cause a picture like that of
Addison’s disease.
Pregnancy
There is a generalized increase in pigmentation during
pregnancy, especially of the nipples and areolae, and of the
linea alba. Melasma
The nipples and areolae may remain pigmented for a while
after parturition.
Chronic renal failure
The hyperpigmentation is caused by an increase in levels of
pituitary melanotrophic peptides, normally cleared by the
kidney.
Porphyria
Formed porphyrins, especially uroporphyrins is endogenous
photosensitizers induce hyperpigmentation on exposed areas
Nutritional hyperpigmentation
Any severe wasting disease, such as malabsorption, AIDS,
tuberculosis or cancer, may be accompanied by diffuse
hyperpigmentation.
Kwashiorkor presents a mixed picture of generalized
hypopigmentation and patchy post-inflammatory
hyperpigmentation,
Post-inflammatory
hyperpigmentation
common after lichen planus
systemic sclerosis
some types of cutaneous amyloidosis
cryotherapy
The end
