OSTEOARTHRITIS
Dr. Nizar AbdulateefAssistant Professor & Consultant Rheumatologist
Learning objectives
1. To understand the pathophysiologic mechanisms that result in development of osteoarthritis (OA).2. To define the clinical features & radiologic findings of OA.
3. To define the principles of therapy of OA.Osteoarthritis
Degenerative, or wear and tear arthritisMost common form of arthritis
Strongly associated with ageing
Major cause of pain and disability in older people
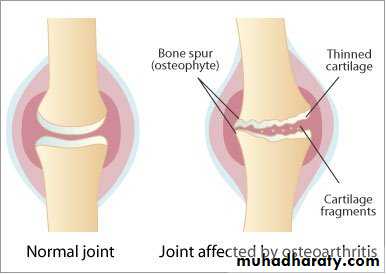
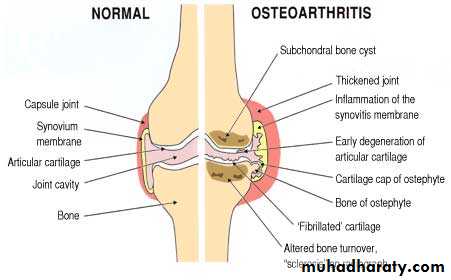
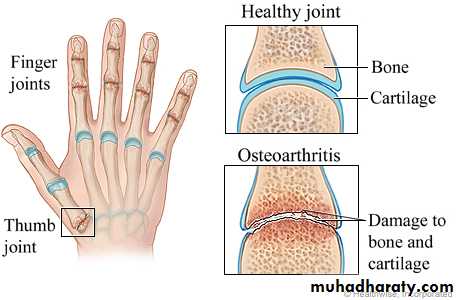
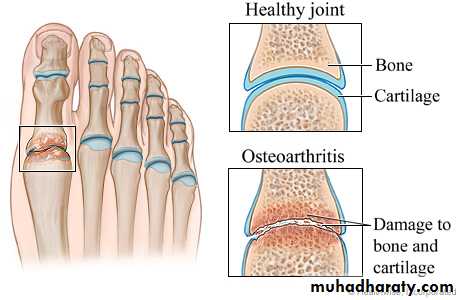
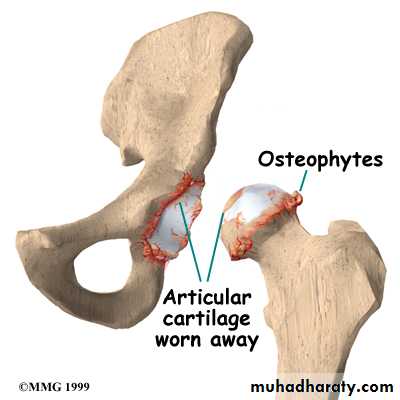
Characterised by:Focal loss of articular cartilage
Subchondral osteosclerosisOsteophyte formation at the joint margin
Remodelling of joint contour with enlargement of affected jointsInflammation is not a prominent feature
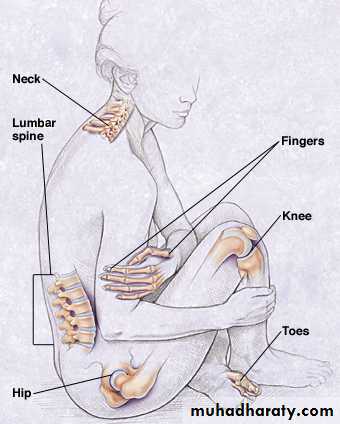
Joints involved in OA:
KneesHips
PIP and DIP joints of the handsCervical and lumbar spine
Epidemiology
The prevalence of OA rises progressively with age.45% of all people develop knee OA and 25% hip OA at some point during life.
The lifetime risk of having a total hip or knee replacement for OA in someone aged 50 is about 11% in women and 8% in men.
OA are more prevalent in women, except at the hip, where men are equally affected.
PathophysiologyOA is a complex disorder with both genetic and environmental components.
Repetitive adverse loading of joints during occupation or competitive sports is an important predisposing factor.
Congenital abnormalities of the joint (slipped femoral epiphysis)
Obesity (increased mechanical loading of the joints, cytokines released from adipose tissue)Sex hormones may play a causal role.
Genetic factors play a key role in the pathogenesis of OA, the heritability of OA ranges between about 43% at the knee to between 60% and 65% at the hip and hand, respectively.Major alterations in cartilage structure are characteristic of OA.
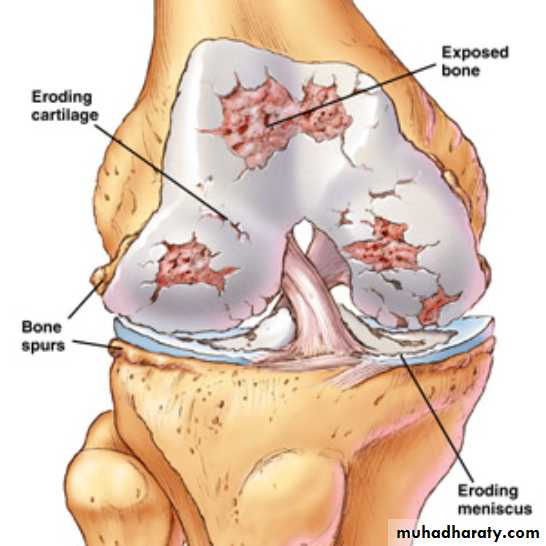
Chondrocytes divide to produce nests of metabolically active cells.Increased degradation of the major structural components of cartilage, including aggrecan and type II collagen
Fissuring of the cartilage surface (‘fibrillation’) development of deep vertical clefts, localised chondrocyte death and decreased cartilage thickness
The subchondral bone is abnormal, with osteosclerosis and subchondral cyst formation.
Fibrocartilage is produced at the joint margin, which undergoes ossification to form osteophytes.Bone remodelling and cartilage thinning slowly alter the shape of the OA joint, increasing its surface area.
Synovial hyperplasia and inflammation (to a much lesser extent than in RA)
Clinical features
Pain & functional restriction of the hands, knees or hips over the age of 45, but more often over 60 years.Pain
• Insidious onset over months or years• Variable or intermittent over time
• Mainly related to movement and weight-bearing, relieved by rest• Only brief (< 15 mins) morning stiffness and brief (< 5 mins) ‘gelling’ after rest
• Usually only one or a few joints painful
The causes of pain in OA:
increased pressure in subchondral bonetrabecular microfractures
capsular distension
low-grade synovitis
bursitis and enthesopathy secondary to altered joint mechanicsClinical signs
• Restricted movement due to capsular thickening, or blocking by osteophyte• Palpable, coarse crepitus due to rough articular surfaces
• Bony swelling around joint margins• Deformity, usually without instability
• Joint-line or periarticular tenderness• Muscle weakness and wasting
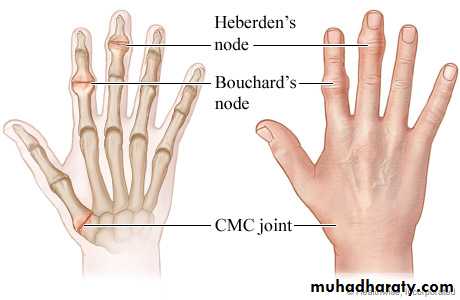
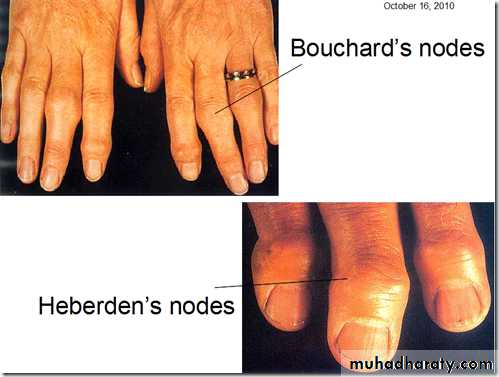
• Synovitis mild or absentGeneralised nodal OA
Polyarticular finger interphalangeal joint OA
Heberden’s & Bouchard’s nodesInvolvement of the first carpometacarpal joint (CMC) is also common
Marked female preponderancePeak onset in middle age
Good functional outcome for handsPredisposition to OA at other joints, especially knees
Strong genetic predispositionKnee OA
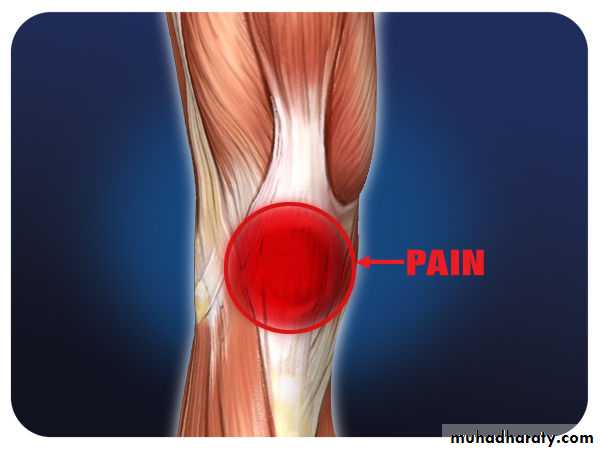
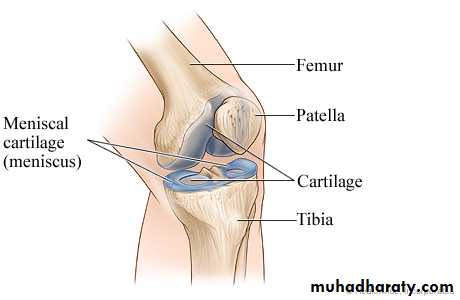
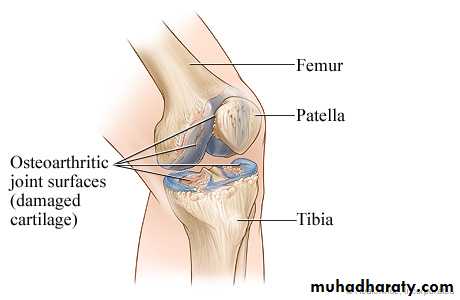
It targets the patello-femoral and medial tibio-femoral compartments.
It may be isolated or occur as part of generalised nodal OA.
Most patients, particularly women, have bilateral and symmetrical involvement.The pain is usually localised to the anterior or medial aspect of the knee and upper tibia.
Patello-femoral pain is usually worse going up and down stairs or inclines.
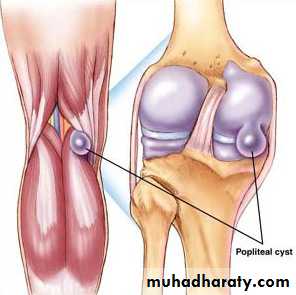
Posterior knee pain suggests the presence of a complicating popliteal cyst (Baker’s cyst).Prolonged walking, rising from a chair, getting in or out of a car, or bending to put on shoes and socks may be difficult.
Varus (less commonly valgus) deformity &/or fixed flexion deformity
Joint-line &/or periarticular tenderness (secondary anserine bursitis and medial ligament enthesopathy)Weakness and wasting of the quadriceps muscle
Restricted flexion/extension with coarse crepitusBony swelling around the joint line
Varus deformity of the knee
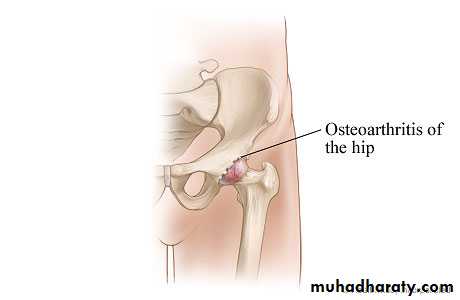
Hip OA
Superior aspect of the jointHip pain is usually maximal deep in the anterior groin, with variable radiation to the buttock, anterolateral thigh, knee or shin
Functional difficulties are the same as for knee OA
Weakness and wasting of quadriceps and gluteal musclesPain and restriction of internal rotation with the hip flexed – the earliest and most sensitive sign of hip OA; other movements may subsequently be restricted and painful
Anterior groin tenderness just lateral to the femoral pulse
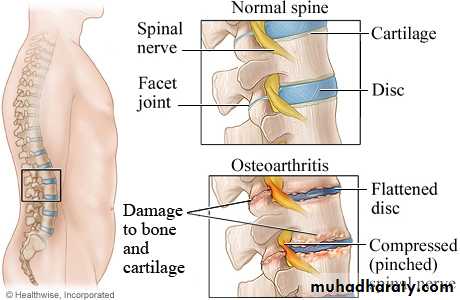
Spine OA
The cervical and lumbar spine are predominantly targeted by OA (spondylosis).Spine OA may occur in isolation or as part of generalised OA.
The typical presentation is with pain localised to the low back region or the neck, although radiation of pain to the arms, buttocks and legs may also occur due to nerve root compression.The pain is typically relieved by rest and worse on movement.
On physical examination, the range of movement may be limited and loss of lumbar lordosis is typical.The straight leg-raising test or femoral stretch test may be positive and neurological signs may be seen in the legs where there is complicating spinal stenosis or nerve root compression.
Early-onset OA
It presents before the age of 45.In most cases, a single joint is affected and there is a clear history of previous trauma.
Specific causes of OA need to be considered in people with early-onset disease affecting several joints, especially those not normally targeted by OA, rare causes need to be considered.Causes of early-onset osteoarthritis
Monoarticular- Previous trauma, localised instability
Pauciarticular or polyarticular
- Juvenile idiopathic arthritis- Metabolic or endocrine disease (Haemochromatosis, ochronosis & acromegaly)
- Late avascular necrosis
- Neuropathic joint
Investigations
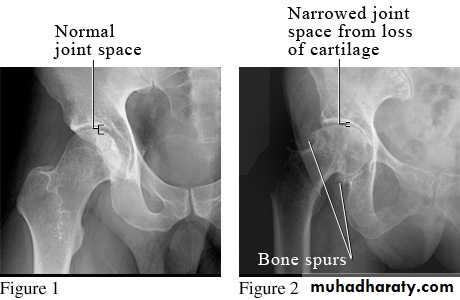
Plain X-ray of the affected joint (diagnostic features, severity of structural damage)Non-weight bearing postero-anterior views of the pelvis are adequate for assessing hip OA.
Patients with suspected knee OA should have standing antero-posterior radiographs taken to assess tibio-femoral cartilage loss, and a flexed skyline view to assess patello-femoral involvement.
Spine OA can often be diagnosed on plain X-ray, which typically shows evidence of disc space narrowing and osteophytes.
MRI (nerve root compression or spinal stenosis)
Routine biochemistry, haematology and autoantibody tests are usually normal.
Synovial fluid aspirated from an affected joint is viscous with a low cell count.Management
Non-pharmacological
Pharmacological
SurgeryEducation and other general measures
Explain the nature of the condition, outlining the role of relevant risk factors (obesity, heredity, trauma) and the fact that established structural changes are permanent but that pain and function can improve.The prognosis should be discussed (good for nodal hand OA, more optimistic for knee than hip OA.
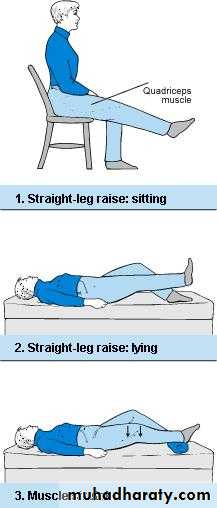
Exercise has beneficial effects in OA, including both strengthening and aerobic exercise, preferably with reinforcement by a physiotherapist (Quadriceps strengthening exercises are particularly beneficial in knee OA)
Weight loss
Pacing of activities, use of a walking stick for painful knee or hip OA, or provision of built-up shoes to equalise leg lengths can all improve symptoms.Analgesics and anti-inflammatory drugs
ParacetamolAddition of a topical NSAID, and then capsaicin, for knee and hand OA can also be helpful.
Oral NSAID should be considered in patients who remain symptomatic.
These drugs are significantly more effective than paracetamol and can be successfully combined with paracetamol.
Opiates may occasionally be required.
For temporary benefit of moderate to severe pain, intra-articular injection of corticosteroids can be helpful.
Local physical therapies such as heat or cold can sometimes give temporary relief.
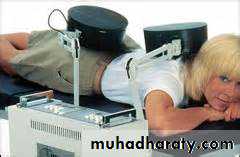
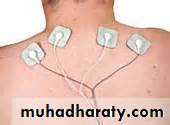
Acupuncture and transcutaneous electrical nerve stimulation (TENS) have also been shown to be effective in knee OA.
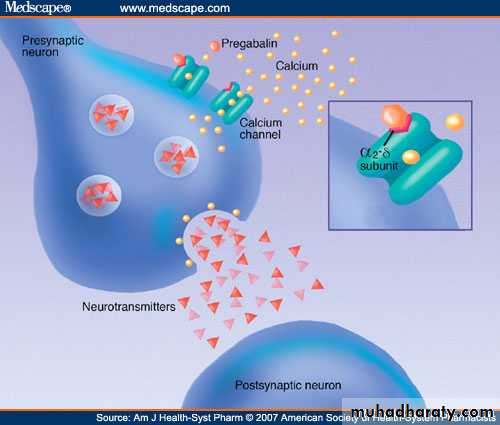
Antineuropathic drugs, such as amitriptyline, gabapentin and pregabalin
Chondroitin and glucosamine
Used alone and in combination for the treatment of knee OA.There is evidence from randomised controlled trials that these agents can improve knee pain to a small extent (3–5%), as compared with placebo.
Hyaluronan injections
In knee OA, intra-articular injection of hyaluronan usually given as a course of weekly injections for 3–5 weeks, may give modest pain relief for several months.Evidence for efficacy is heterogeneous and the expense of this treatment and the common requirement for serial injection should be considered.
Disease-modifying therapies
There are no licensed drugs that can halt the progression of OA.Glucosamine sulphate was shown in one study to slow the rate of radiological progression in knee OA and to reduce the number of subjects who progressed to joint replacement.
A recent randomised controlled trial suggested that strontium ranelate might also be effective in reducing the rate of progression of knee OA.
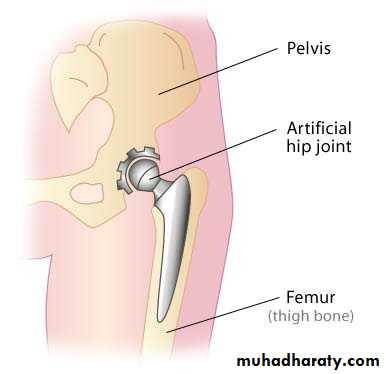
Surgery
Patients with OA whose pain, stiffness and reduced function impact significantly on their quality of life and are refractory to other treatments.Osteotomy can prolong the life of malaligned joints and relieve pain by reducing intraosseous pressure, but is performed infrequently.
Total joint replacement surgery is by far the most common surgical procedure for patients with OA.
Although surgery should not be undertaken at an early stage during the development of OA, it is important to consider it before functional limitation has become advanced since this may compromise the surgical outcome.
Only a small proportion of patients with OA progress to the extent that total joint replacement is required, but OA is by far the most frequent indication for a total joint replacement.
Over 95% of joint replacements continue to function well into the second decade after surgery and most provide life-long, pain-free function.