
Bullous diseases

• Vesicles and bullae are accumulations of fluid within or
under the epidermis.
• Subepidermal blisters occur between the dermis and
the epidermis. Their roofs are relatively thick and so
they tend to be tense and intact.
• Intra-epidermal blisters appear within the prickle cell
layer of the epidermis, and so have thin roofs and
rupture easily to leave an oozing denuded surface.
• Subcorneal blisters, which form just beneath the
stratum corneum at the outermost edge of the viable
epidermis, and therefore have even thinner roofs.
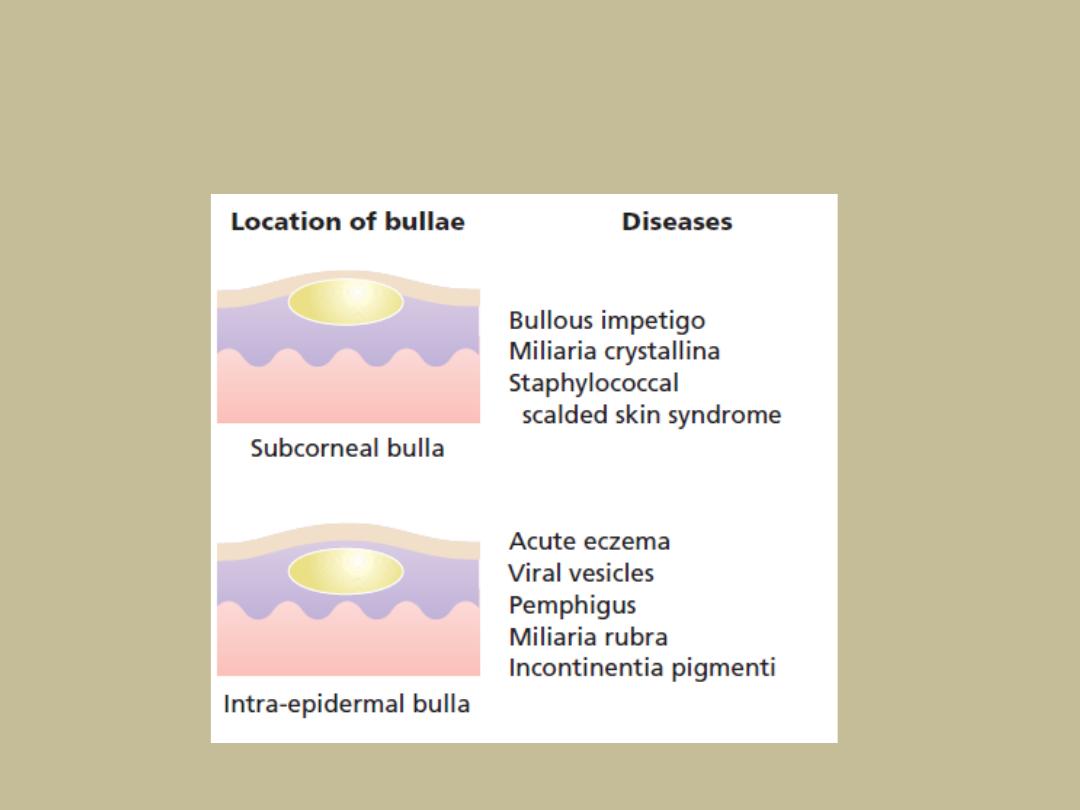
Causes of bullae
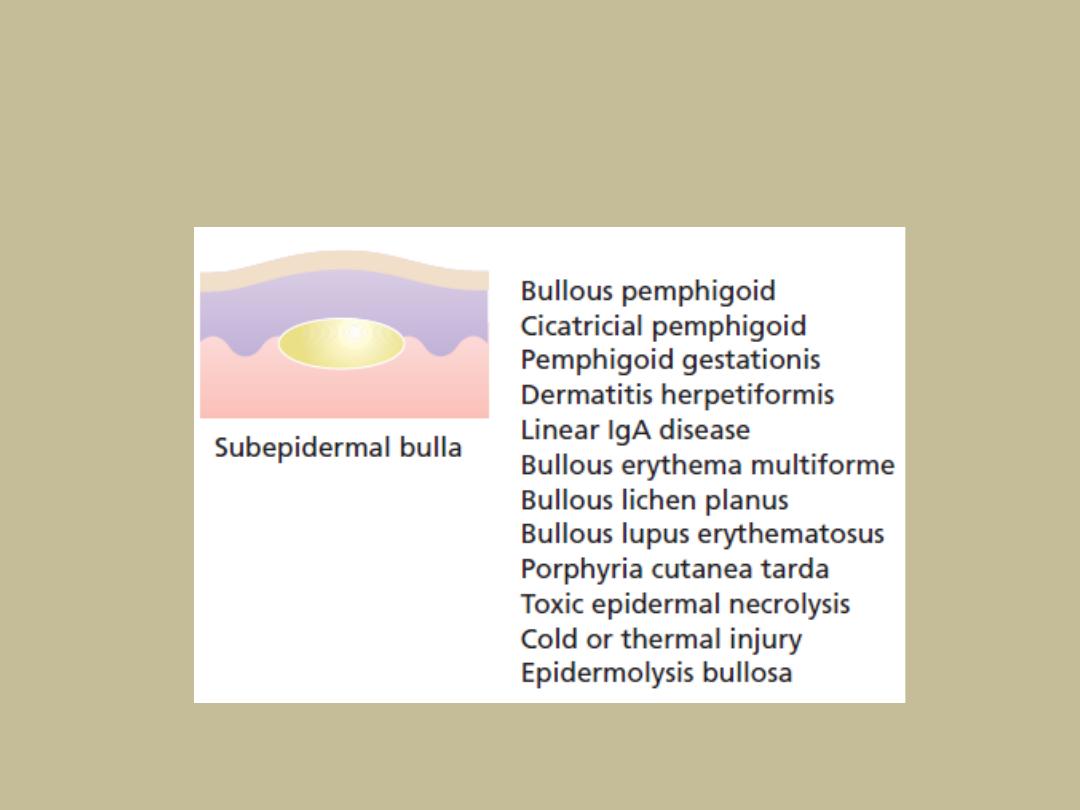
Causes of bullae
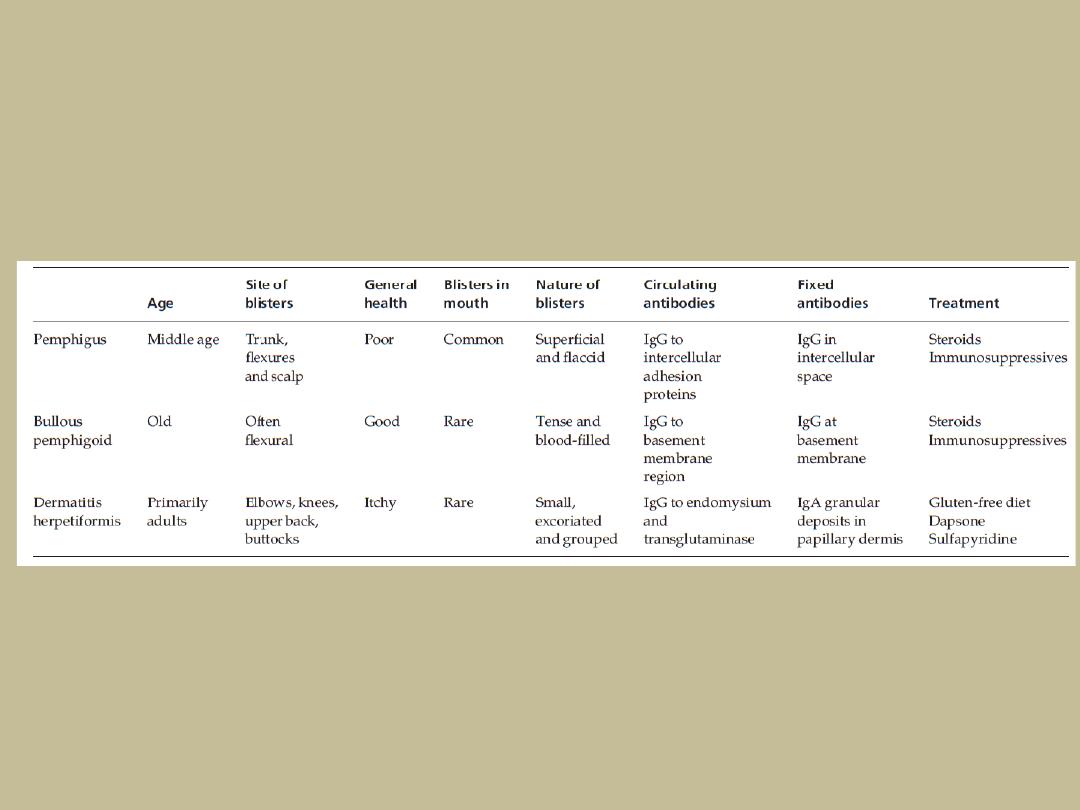
Distinguishing features of the three
main immunobullous diseases
The pemphigus family
• Pemphigus is severe and potentially life-threatening.
Types
1. Pemphigus vulgaris
• is the most common, which accounts for at least three-
quarters of all cases, and for most of the deaths.
2. Pemphigus vegetans
3. Superficial pemphigus
• also has two variants: the generalized foliaceus type and
localized erythematosus type.
4. Paraneoplastic pemphigus
• arrises in association with a neoplasm such as thymoma,
Castleman’s tumour or lymphoma.

Cause
• Autoimmune diseases, (IgG) antibodies bind to
antigens within the epidermis, mainly desmoglein
3 (in pemphigus vulgaris) and desmoglein 1 (in
superficial pemphigus), causing the keratinocytes
to fall apart (acantholysis).
• Pemphigus vulgaris is particularly common in
Ashkenazi Jews and people of Mediterranean or
Indian origin.

Presentation
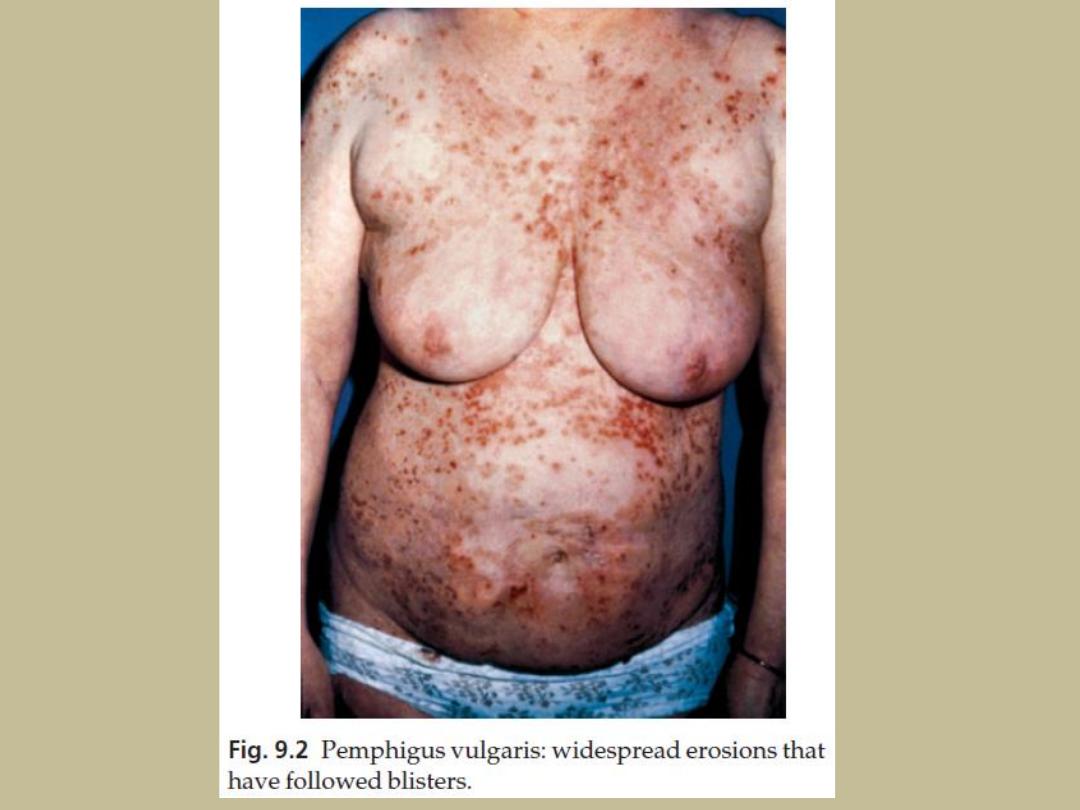
Pemphigus vulgaris
• is characterized by flaccid blisters of the skin and
mouth which rupture easily to leave widespread
painful erosions.
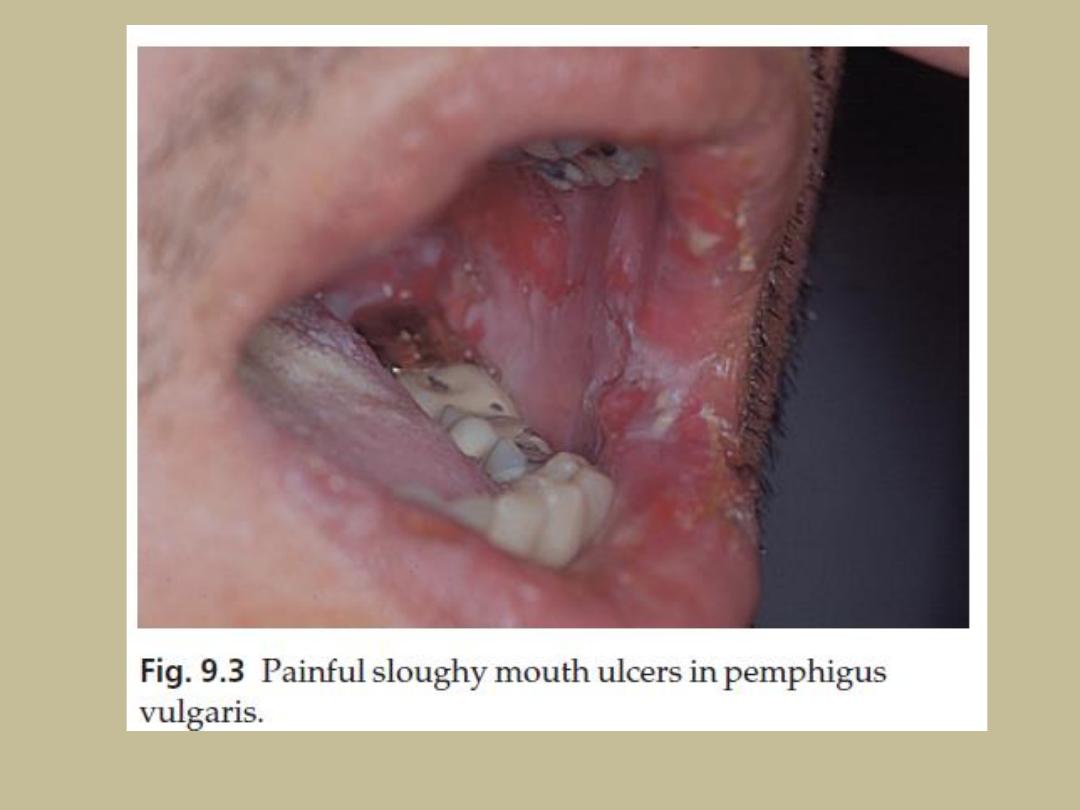
• Most patients develop the mouth lesions first.
• Shearing stresses on normal skin can cause new
erosions to form (a positive Nikolsky sign).
Other types
•
In the vegetans variant, heaped-up cauliflower-like weeping areas are present in
the groin and body folds.
•
In pemphigus foliaceus blisters are so superficial, and rupture so easily, that the
clinical picture is dominated more by weeping and crusting erosions than by
blisters.


Course
• Prolonged, even with treatment
• the mortality rate of pemphigus vulgaris is still at
least 15%.
• About one-third of patients with pemphigus
vulgaris will go into complete remission within 3
years.
• Superficial pemphigus is less severe.
• With modern treatments, most patients with
pemphigus can live relatively normal lives, with
occasional exacerbations.
Complications
• Side effects of high doses of steroids and
immunosuppressive drugs and are now the leading
cause of death.
• Infections of all types are common.
• Severe oral ulcers make eating painful.
Differential diagnosis
• Widespread erosions may suggest a pyoderma,
impetigo, epidermolysis bullosa or ecthyma.
• Mouth ulcers can be mistaken for aphthae, Behçet’s
disease or a herpes simplex infection.
• Scalp erosions suggest bacterial or fungal infections.

Investigations
• Biopsy shows that the vesicles are intra-
epidermal, with rounded keratinocytes floating
freely within the blister cavity (acantholysis).
• Direct immunofluorescence of adjacent normal
skin shows intercellular epidermal deposits of IgG
and C3
• Indirect immunofluorescence or assays (ELISA)
can also be used to confirm the diagnosis.
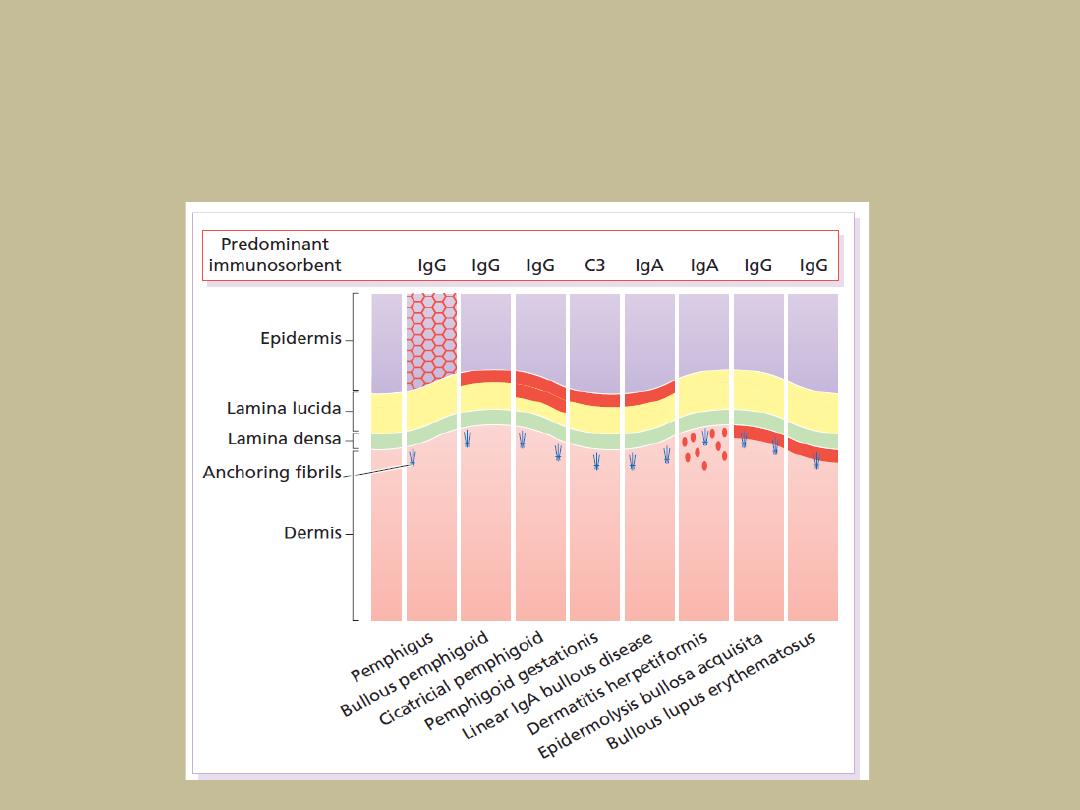
Immunofluorescence (red)
in bullous diseases

Treatment
Systemic steroids
• Resistant and severe cases need very high doses of systemic
steroids, such as 80–180 mg/day prednisolone because
prednisolone up-regulates the expression of desmoglein molecules
on the surfaces of keratinocytes, in addition to their anti-
inflammatory effect
• The dose is reduced only when new blisters stop appearing.
Immunosuppressive agents
• such as azathioprine, gold salts or cyclophosphamide and, recently,
mycophenylate mofetil, are often used as steroid-sparing agents.
• Plasmapheresis and administration of intravenous immunoglobulin.
Other
• Rituximab
• Dapsone

The pemphigoid family
• Pemphigoid is an autoimmune disease.
• The IgG antibodies bind to two main antigens:
most commonly to BP230, and less often to
BP180 at the basement membrane activating
complement starting an inflammatory cascade
causing the epidermis to separate from the
dermis
• Antibodies titre does not correlate with
clinical disease activity.

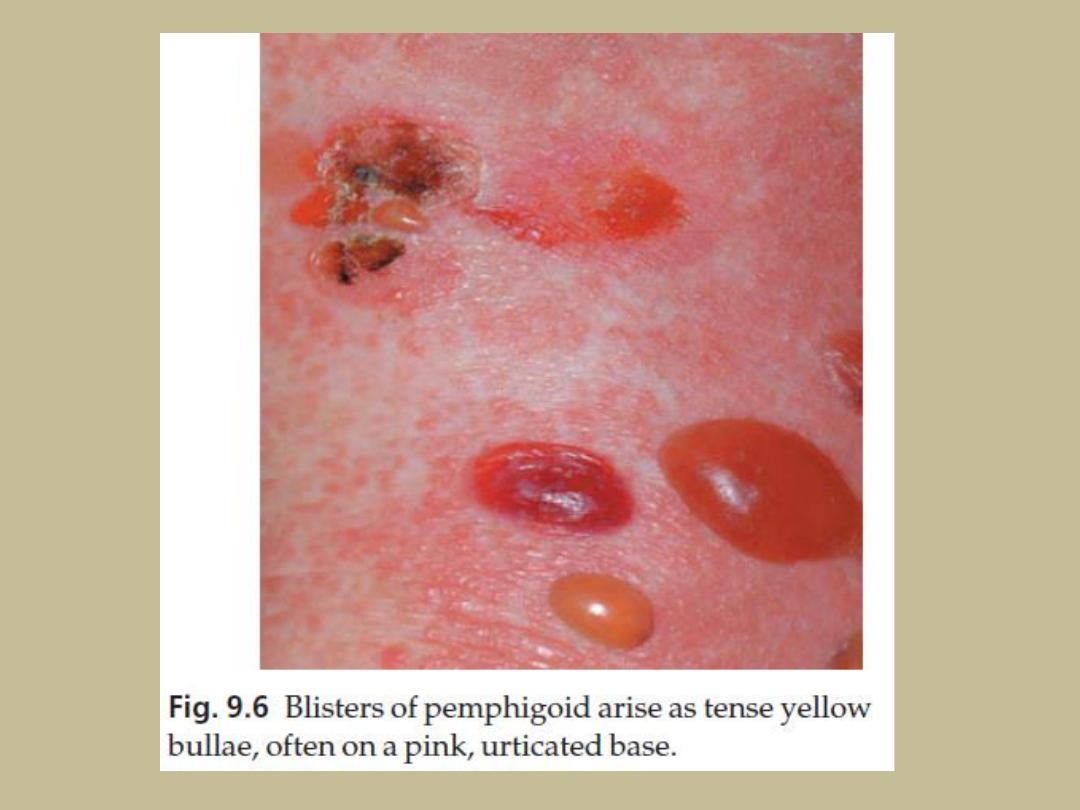
Presentation
• Chronic, usually itchy, blistering disease, mainly affecting
the elderly.
• Usually no precipitating factors can be found, but rarely
ultraviolet light or radiation therapy
• The skin often erupts with smooth, itching red plaques in
which tense vesicles and bullae form
• Occasionally they arise from normal skin.
• The flexures are often affected
• mucous membranes usually are not.
• The Nikolsky test is negative.
• It is not fatal
• factors carrying a high risk include old age, the need for
high steroid dosage and low serum albumin levels.

Course
• Pemphigoid is usually self-limiting and treatment can
often be stopped after 1–2 years.
Complications
• Discomfort and loss of fluid from ruptured bullae.
• Systemic steroids and immunosuppressive agents carry
their usual complications if used long term
Differential diagnosis
• other bullous diseases
• Immunofluorescence helps to separate it from these

Investigations
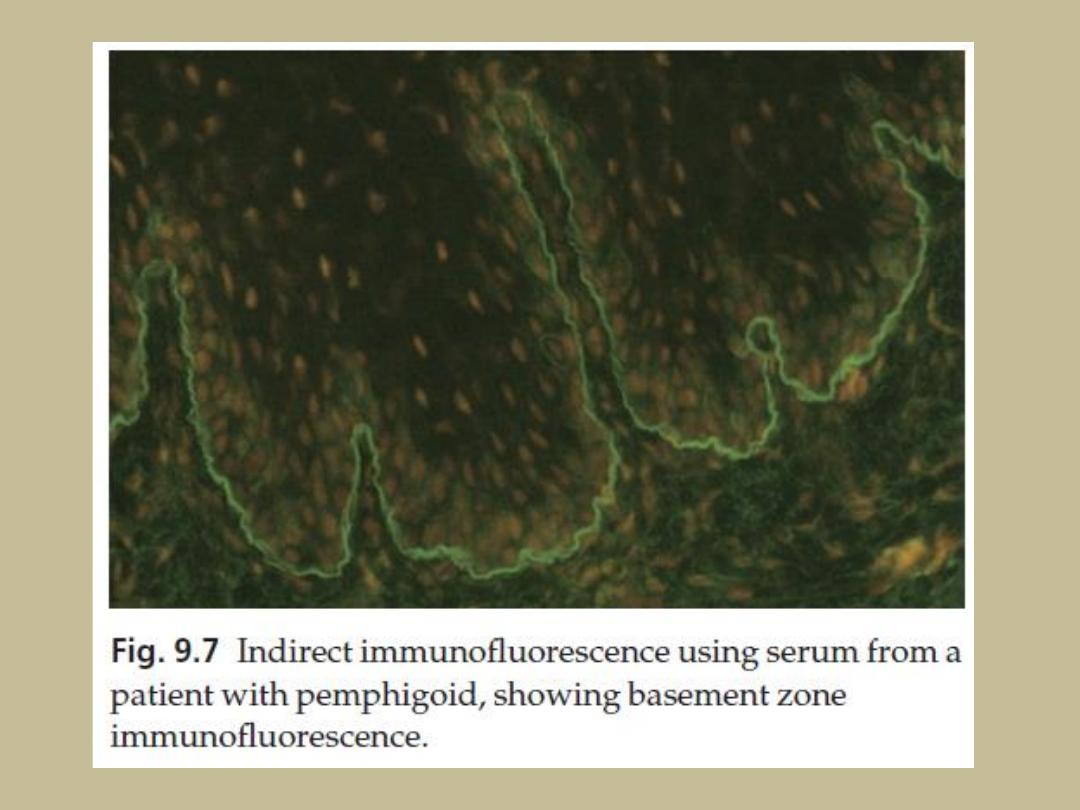
• Direct immunofluorescence shows a linear band
of IgG and C3 along the basement membrane
zone.
• Indirect immunofluorescence identifies IgG
antibodies that react with the basement
membrane zone in some 70% of patients
• A subepidermal blister is often filled with
eosinophils.
• Most patients have peripheral blood eosinophilia.

Treatment
• in the acute phase, prednisolone or prednisone at
a dosage of 40–60 mg/day is usually needed to
control the eruption
• The dosage is reduced as soon as possible, and
patients end up on a low maintenance regimen of
systemic steroids, taken on alternate days until
treatment is stopped.
• Immunosuppressive agents such as azathioprine
may also be required.
• For unknown reasons, tetracyclines and
niacinamide help some patients.

Pemphigoid gestationis (herpes
gestationis)
• This is pemphigoid occurring in pregnancy, or in the
presence of a hydatidiform mole or a choriocarcinoma.
• As in pemphigoid, most patients have linear deposits of
C3 along the basement membrane zone
• The condition usually remits after the birth but may
return in future pregnancies.
• It is not caused by a herpes virus: the name herpes
gestationis should be discarded now
• Treatment is with systemic steroids.
• Oral contraceptives should be avoided, because their
hormones may precipitate the disease.

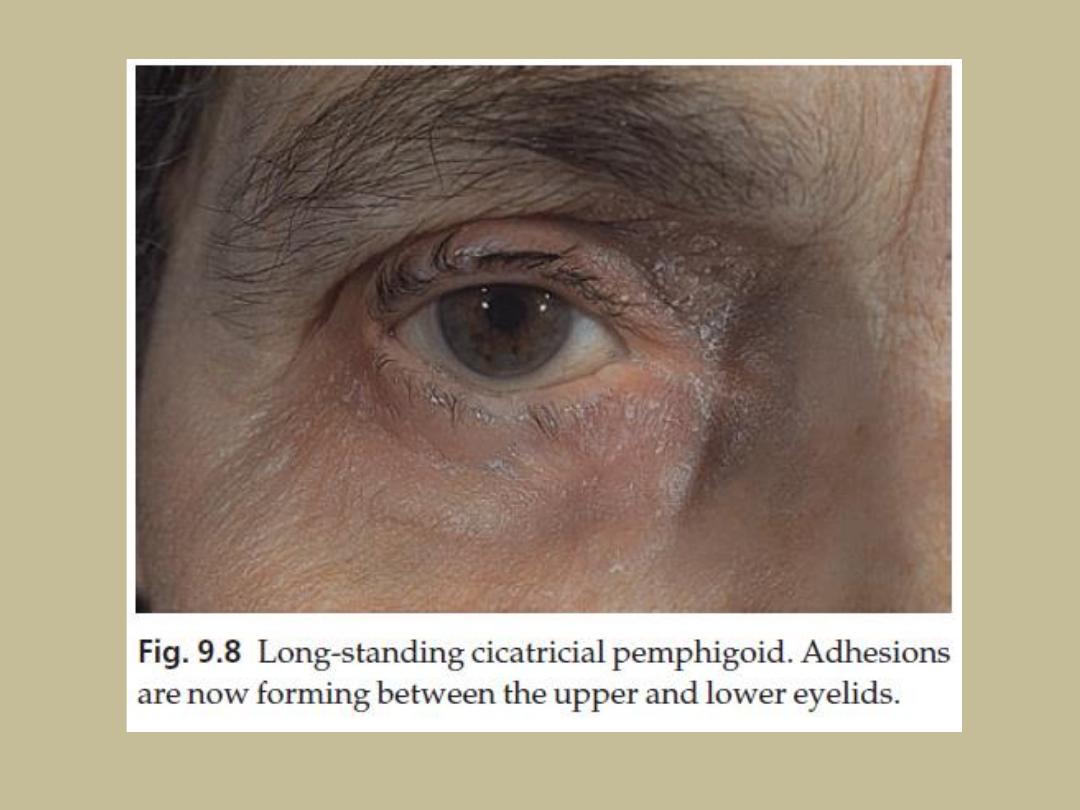
Cicatricial pemphigoid
Like pemphigoid itself, but
• other antigens at the dermal–epidermal junction are sometimes
targeted such as laminin 5
• its blisters and ulcers occur mainly on mucous membranes such as
the conjunctivae, the mouth and genital tract, but bullae on the
skin itself are uncommon.
• Lesions heal with scarring; around the eyes this may cause
blindness, especially when the palpebral conjunctivae are affected
• The condition tends to persist and treatment is relatively ineffective
• Very potent local steroids, dapsone, systemic steroids and
immunosuppressive agents are usually tried.
• Good eye hygiene and the removal of ingrowing eyelashes are
important.

Linear IgA bullous disease
• clinically similar to pemphigoid, but affects children as well
as adults.
• Blisters arise on urticarial plaques, and often grouped, and
on extensor surfaces, than is the case with pemphigoid.
• The so-called ‘string of pearls sign’, seen in some affected
children, is the presence of blistering around the rim of
polycyclic urticarial plaques.
• The conjunctivae may be involved.
• linear deposits of IgA and C3 at the basement membrane
zone
• IgG is sometimes also found.
• The disorder responds well to oral dapsone.

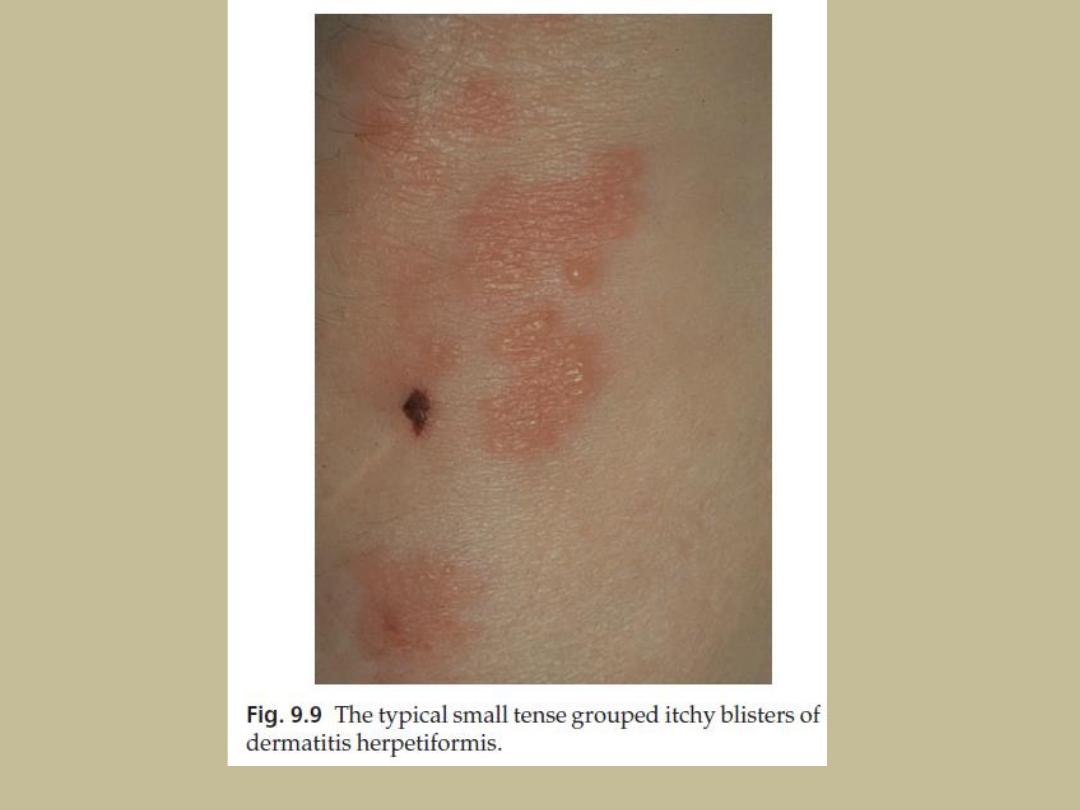
Dermatitis herpetiformis
• A very itchy chronic subepidermal vesicular disease, in
which the vesicles erupt in groups as in herpes simplex –
hence the name ‘herpetiformis’.
Cause
• Gluten-sensitive enteropathy (sprue, adult celiac disease is
always present, but most patients do not suffer
enteropathy as it mild, patchy and involves only the
proximal small intestine.
• A range of antibodies can be detected in serum, notably
directed against tissue transglutaminase, reticulin, gliadin
and endomysium
• The IgA deposits in skin clear slowly after the introduction
of a gluten-free diet.
• There is a strong association with certain human leucocyte
antigen (HLA) types, particularly HLA-DR3 and HLA-DQw2.
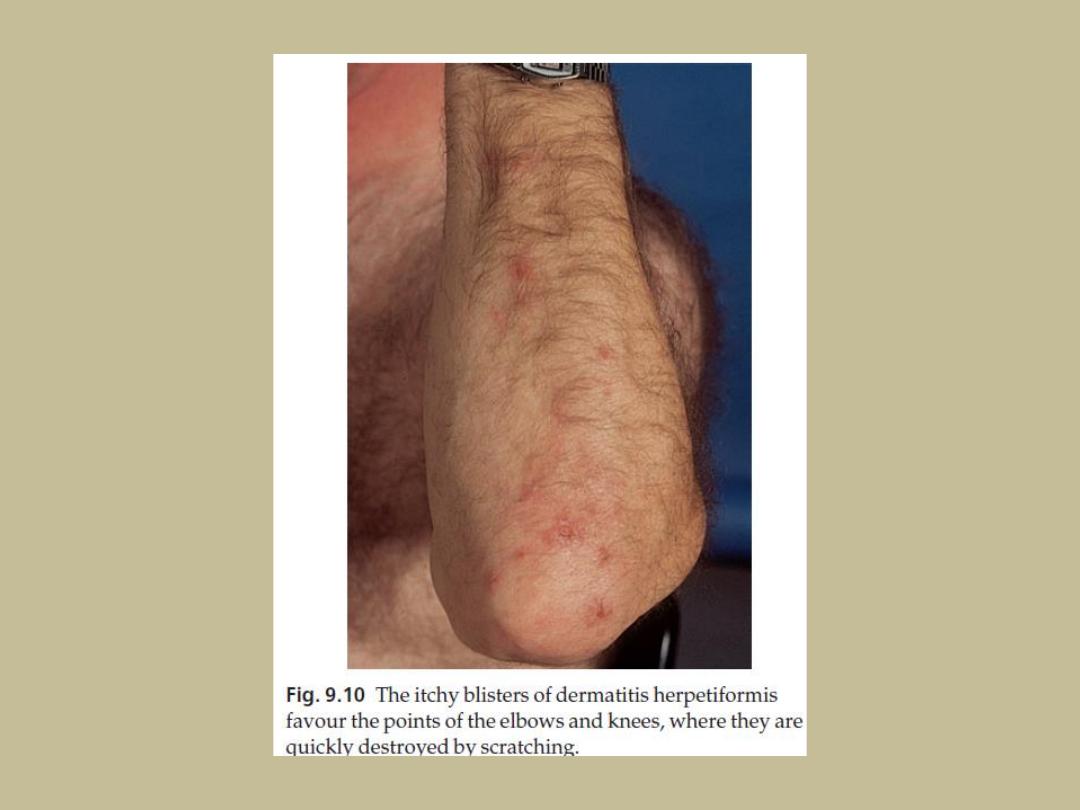
Presentation
• The extremely itchy, grouped vesicles and urticated
papules develop particularly over the elbows and
knees, buttocks and shoulders.
• They are often broken by scratching before they reach
any size. A typical patient therefore shows only
grouped excoriations.
• Sometimes a secondary eczematous dermatitis
develops from fierce scratching. Thus, the name
‘dermatitis’ comes from scratching, and ‘herpetiformis’
comes from grouping of vesicles and crusts.

Course
• Typically lasts for decades unless patients avoid gluten entirely.
Complications
• The complications of gluten-sensitive enteropathy include
diarrhoea, abdominal pain, anaemia and, rarely, malabsorption.
• Small bowel lymphomas have been reported
• proven association with other autoimmune diseases, most
commonly of the thyroid.
Differential diagnosis
• Scabies
• an excoriated eczema
• insect bites
• neurodermatitis.

Investigations
• Histology will be that of a subepidermal blister, with
neutrophils packing the adjacent dermal papillae.
• Direct immunofluorescence of uninvolved skin shows
granular deposits of IgA, and usually C3, in the dermal
papillae and superficial dermis
• Serum antibody tests for anti-endomysial antibodies or
tissue transglutaminase can help diagnose the
enteropathy.
• Small bowel biopsy is no longer recommended as
routine because the changes are often patchy and
serum tests are more sensitive.

Treatment
• A gluten-free diet, Adherence can be monitored
using the titre of antibodies to anti-endomysial
antigens or to tissue transglutaminase, which fall
if gluten is strictly avoided.
• Dapsone or sulfapyridine, although both can
cause severe rashes, haemolytic anaemia
(especially in those with glucose- 6-phosphate
dehydrogenase deficiency), leucopenia,
thrombocytopenia, methaemoglobinaemia and
peripheral neuropathy. Regular blood checks are
therefore necessary.

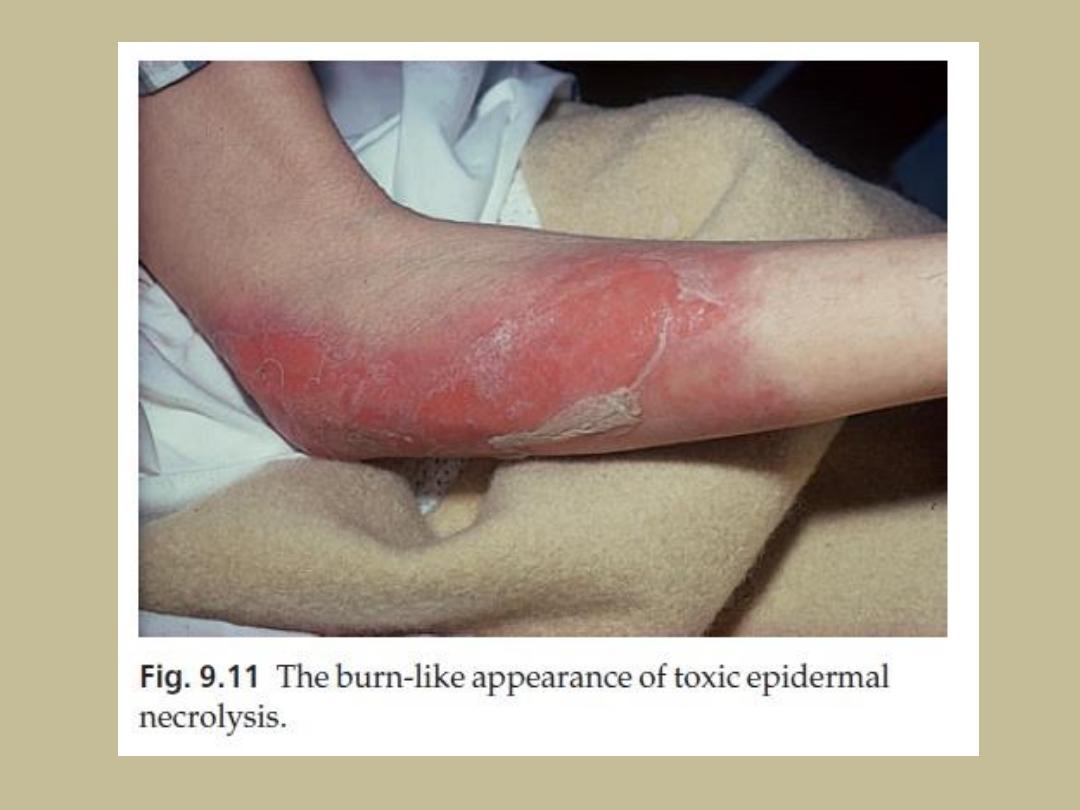
Toxic epidermal necrolysis (Lyell’s
disease)
Cause
• usually a drug reaction, most commonly to sulphonamides,
lamotrigine, barbiturates, carbamazepine or allopurinol
• graft-vs.-host disease
• AIDs
Presentation
• The skin becomes red and intensely painful, and then
begins to come off in sheets like a scald leaving an eroded
painful glistening surface
• Nikolsky’s sign is positive.
• The mucous membranes may be affected, including the
mouth, eyes, and even the bronchial tree.

Course
• The condition usually clears if the offending drug is
stopped.
• New epidermis grows out from hair follicles so that skin
grafts are not usually needed.
• The disorder may come back if the drug is taken again.
Complications
• It is a skin emergency and can be fatal.
• Infection, and the loss of fluids and electrolytes, are life-
threatening
• Corneal scarring may remain when the acute episode has
settled.

Differential diagnosis
• Staphylococcal scalded skin syndrome but only the
stratum corneum is lost and is seen in infancy or early
childhood.
• Some believe that toxic epidermal necrolysis can
evolve from Stevens–Johnson syndrome because some
patients have the clinical features of both.
Investigations
• Biopsy helps to confirm the diagnosis. The split is
subepidermal in toxic epidermal necrolysis, in scalded
skin syndrome where the split is subcorneal.

Treatment
• The drug must be stopped
• treatment relies mainly on symptomatic management with
intensive nursing care and medical support including the
use of central venous lines, intravenous fluids and
electrolytes.
• Many patients are treated in units designed to deal with
extensive thermal burns
• The weight of opinion has turned against the use of
systemic corticosteroids.
• Intravenous IgG seems more promising and ciclosporin
treatment has been associated with a decreased mortality
rates.
• Plasmapheresis may remove triggering drugs, or
inflammatory mediators.

The END
THANKS
