B
ACTERIAL INFECTIONS

R
ESIDENT FLORA OF THE SKIN
most numerous in moist hairy areas, rich in sebaceous
glands
found in irregularities in the stratum corneum and within
the hair follicles.
The resident flora is a mixture of harmless and poorly
classified staphylococci, micrococci and diphtheroid
Staphylococcus epidermidis and aerobic diphtheroids
predominate on the surface,and anaerobic diphtheroids
(Propionibacteria sp.) deep in the hair follicles.
helps to defend the skin against outside pathogens by
bacterial interference or antibiotic production.
Overgrowth of aerobic diphtheroids causes trichomycosis
axillaris, pitted keratolysis and erythrasma.
S
TAPHYLOCOCCAL INFECTIONS
Staphylococcus aureus is not part of the resident
flora of the skin other than in a minority who
carry it in their nostrils, perineum or armpits
Nasal carriage is almost invariable in babies born
in hospital, becomes less frequent during infancy
and rises again during the school years to the
adult level of roughly 30%.
Staphylococci can also multiply on areas of
diseased skin such as eczema, often without
causing obvious sepsis

I
MPETIGO
Impetigo may be caused by staphylococci, streptococci,
or by both together
As a useful rule of thumb, the bullous type is usually
caused by Staphylococcus aureus, whereas the crusted
ulcerated type is caused by beta-haemolytic strains of
streptococci
Both are highly contagious.
Exfoliative toxins produced by S. aureus cleave the cell
adhesion molecule desmoglein 1
If the toxin is localized this produces the blisters of
bullous impetigo, but if generalized leads to more
widespread blistering as in the staphylococcal scalded
skin syndrome.

I
MPETIGO
Presentation
A thin-walled flaccid clear blister forms, may
become pustular before rupturing to leave an
extending area of exudation and yellowish
varnish-like crusting
often multiple, particularly around the face.
The lesions may be more obviously bullous in
infants.
A follicular type of impetigo (superficial
folliculitis) is also common

I
MPETIGO
Course
The condition can spread rapidly through a family or
class. It tends to clear even without treatment
Complications
Streptococcal impetigo can trigger an acute
glomerulonephritis
Differential diagnosis
Always think of a possible underlying cause such as:
1.
Herpes simplex and eczema may become
impetiginized
2.
Recurrent impetigo of the head and neck, for
example, should prompt a search for scalp lice.

I
MPETIGO
Investigation and treatment
Gram stains or culture
Systemic antibiotics (such as flucloxacillin,
erythromycin or cefalexin) are needed for severe
cases or if a nephritogenic strain of streptococcus
is suspected (penicillin V).
For minor cases the removal of crusts by
compressing them
application of a topical antibiotic such as
neomycin, fusidic acid, mupirocin or bacitracin

E
CTHYMA
describes ulcers forming under a crusted surface
infection.
The site may have been that of an insect bite or
of neglected minor trauma.
The bacterial pathogens and their treatment are
similar to those of impetigo.
in impetigo the erosion is at the stratum
corneum, in ecthyma the ulcer is full thickness,
and thus heals with scarring.
F
URUNCULOSIS
(
BOILS
)
A furuncle is an acute pustular infection of a hair
follicle, usually with Staphylococcus aureus.
Adolescent boys are especially susceptible to them.
Presentation
tender red nodule enlarges, may discharge pus before
healing to leave a scar
Fever and enlarged draining nodes are rare.
The sudden appearance of many furuncles suggests a
virulent staphylococcus including strains of
community aquired MRSA.
Chronic furunculosis often because of susceptibility
of follicles or colonization of nares or groins to
pathogenic bacteria but rarely immunedeficiency

F
URUNCULOSIS
(
BOILS
)
Complications
Rarely Cavernous sinus thrombosis if central face
Septicaemia
Differential diagnosis
Hidradenitis suppurativa should be considered if
only the groin and axillae are involved

F
URUNCULOSIS
(
BOILS
)
Investigations in chronic furunculosis
1.
General examination: look for underlying skin
disease (e.g. scabies, pediculosis, eczema).
2.
Test the urine for sugar.
3.
Full blood count.
4.
Immunological evaluation only if the patient
has recurrent or unusual internal infections
too.
5.
Culture swabs from lesions and carrier sites
(nostrils, perineum) of the patient and
immediate family.
Test both to identify the organism and to
evaluate sensitivity to various antibiotics.
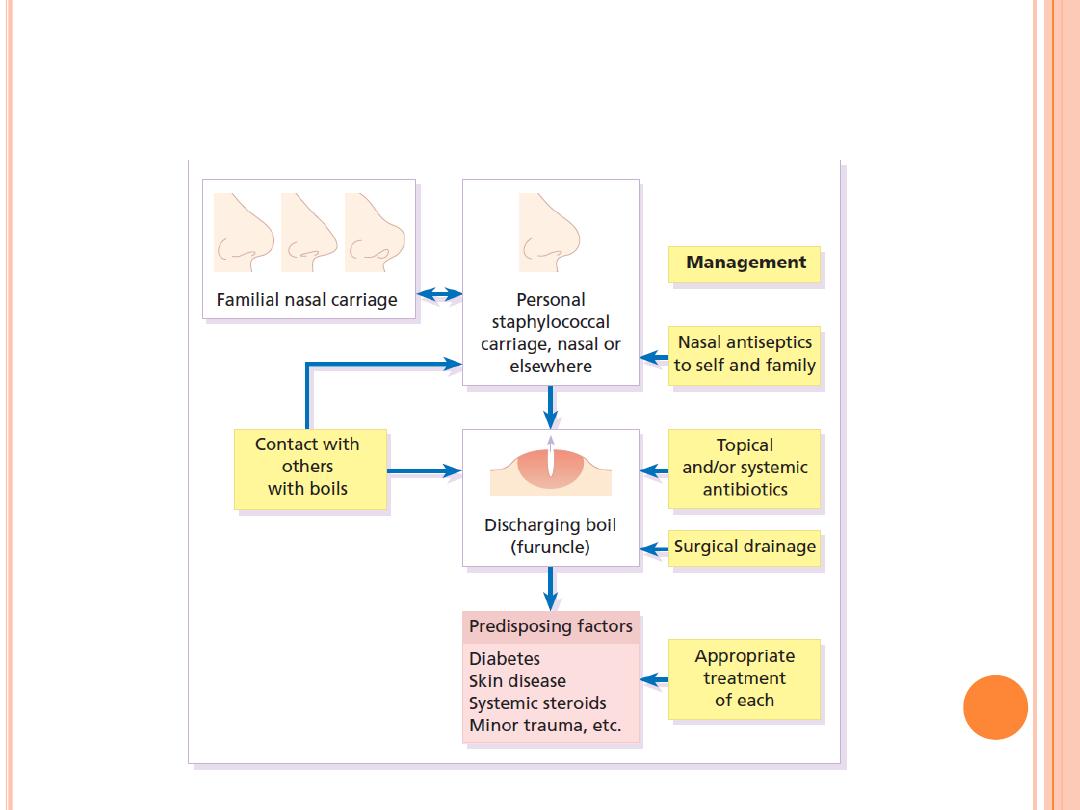
A
PPROCH TO CHRONIC FURNCULOSIS

F
URUNCULOSIS
(
BOILS
)
Treatment
Acute episodes
simple incision and drainage.
An appropriate systemic antibiotic is needed when:
1.
many furuncles
2.
fever is present
3.
the patient is immunosuppressed.
Chronic furunculosis
treat carrier sites such as the nose and groin twice daily for 6
weeks with an appropriate topical antiseptic or antibiotic (e.g.
chlorhexidine solution, mupirocin cream or clindamycin solution).
Treat family carriers in the same way.
Stubborn cases
add 6 weeks of a systemic antibiotic chosen to cover organism’s
proven sensitivities.
Daily bath using an antiseptic soap.
Improve hygiene and nutritional state

C
ARBUNCLE
A group of adjacent hair follicles becomes deeply
infected and discharging pus from several points
caused by Staphylococcus aureus
The pain and systemic upset are greater than those of
a boil
Diabetes must be excluded.
DDX
Consider the possibility of a fungal kerion in
unresponsive carbuncles
Treatment
topical and systemic antibiotics
Incision and drainage have been shown to speed up
healing, although it is not always easy when there are
multiple deep pus-filled pockets.

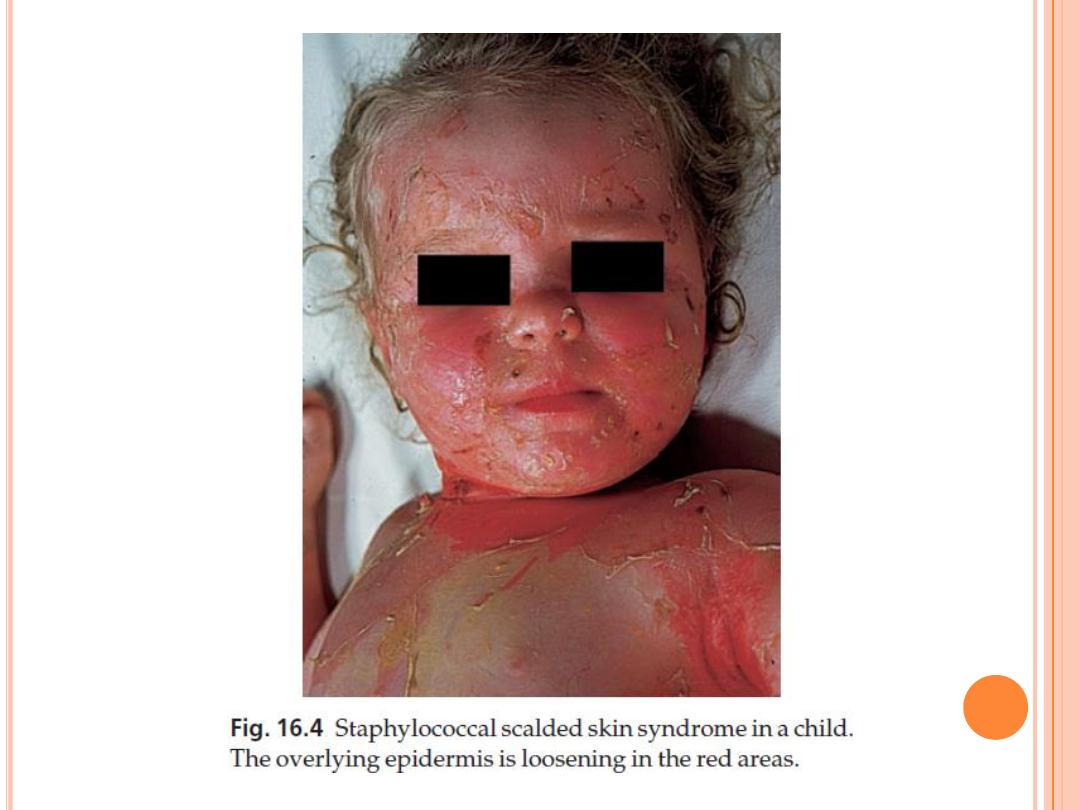
S
CALDED SKIN SYNDROME
Erythema and tenderness are followed by the loosening of
large areas of overlying epidermis
usually caused by a toxin produced by staphylococcal
infection elsewhere (e.g. impetigo or conjunctivitis).
The exfoliative toxins cleave desmoglein 1 to disrupt
adhesion high in the epidermis, causing the stratum
corneum to slough off.
With systemic antibiotics the outlook is good.
The disorder affects children and patients with renal failure
most adults have antibodies to the toxin, and therefore are
protected.
In adults with widespread exfoliation, consider toxic
epidermal necrolysis, which is usually drug induced.
The damage to the epidermis in toxic epidermal necrolysis
is full thickness, and a skin biopsy will distinguish it from
the scalded skin syndrome

T
OXIC SHOCK SYNDROME
Caused by staphylococcal toxin
Present as fever, a rash – usually a widespread
erythema – and sometimes circulatory collapse
are followed a week or two later by characteristic
desquamation, most marked on the fingers and
hands.
Many cases have followed staphylococcal
overgrowth in the vagina of women using
tampons.
Systemic antibiotics and irrigation of the
underlying infected site are needed.

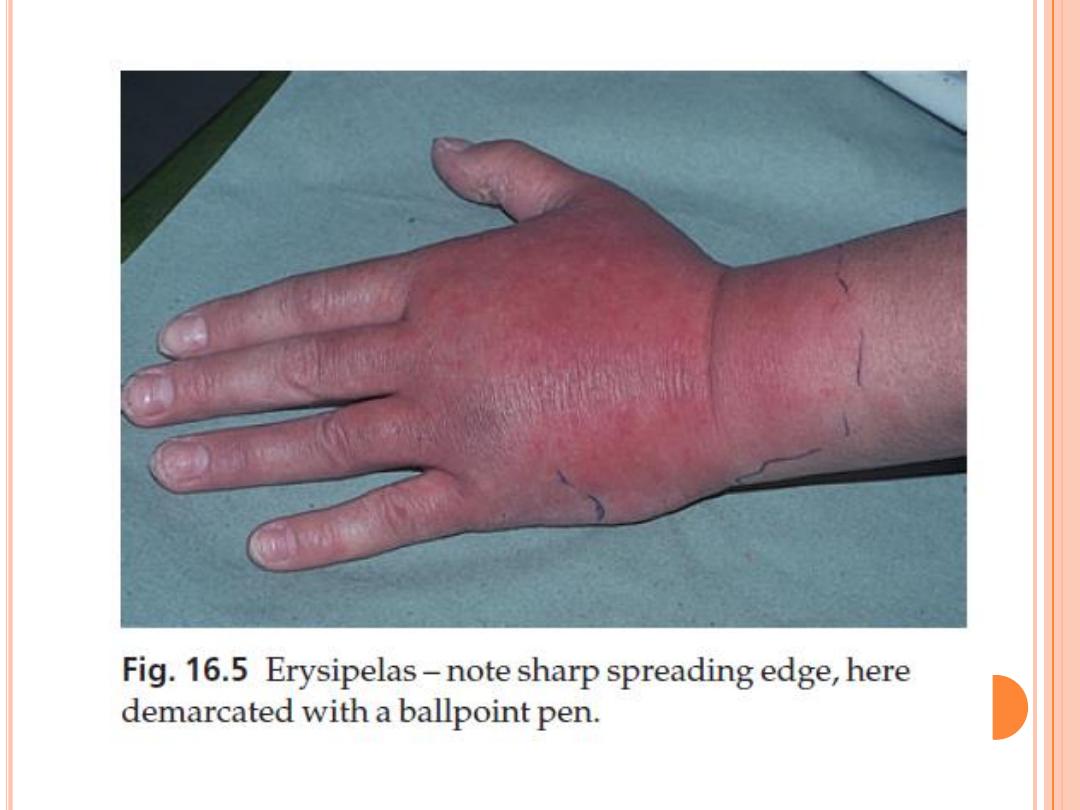
S
TREPTOCOCCAL INFECTIONS

E
RYSIPELAS
malaise, shivering and a fever.
red area of skin, with a well-defined advancing edge
with or without blisters
Untreated, the condition can even be fatal, but it responds
rapidly to systemic penicillin, sometimes given
intravenously.
The causative streptococci usually gain their entry through
a split in the skin (e.g. between the toes or under an ear
lobe).
Episodes can affect the same area repeatedly and so lead to
persistent lymphoedema.
Low dosage long-term oral penicillin V will usually cut
down the frequency of recurrences.
The cause of the original skin split, perhaps a minor tinea
pedis, should be treated.

C
ELLULITIS
This inflammation of the skin occurs at a deeper
level than erysipelas involving the subcutaneous
tissues
the area is more raised and swollen, and the
erythema less marginated than in erysipelas.
Cellulitis often follows an injury and favours
areas of hypostatic oedema.
Streptococci, staphylococci or other organisms
may be the cause.
Treatment is elevation, rest – sometimes in
hospital – and systemic antibiotics, sometimes
given intravenously.

N
ECROTIZING FASCIITIS
A mixture of pathogens, usually including streptococci
and anaerobes
It is a surgical emergency.
Diabetics and post-surgical patients are predisposed.
At first the infection resembles a dusky, often painful,
cellulitis, but it quickly turns into an extending necrosis of
the skin and subcutaneous tissues.
Classically, the central area of skin involvement becomes
anaesthetic because of cutaneous nerve damage.
A deep ‘stab’ incision biopsy through the skin into the fascia
may be necessary to establish the diagnosis
A magnetic resonance imaging (MRI) scan may help to
establish how far the infection has spread.
The prognosis is often poor despite early wide surgical
débridement and prompt intravenous antibiotic
administration.

V
IRAL DIEASES

V
IRAL WARTS
Their prevalence is highest in childhood
Cause
human papilloma virus (HPV):
1.
HPV-1, 2 and 4, are found in common warts
2.
HPV-3 is found in plane warts
3.
HPV-6, 11, 16 and 18 are most common in
genital warts
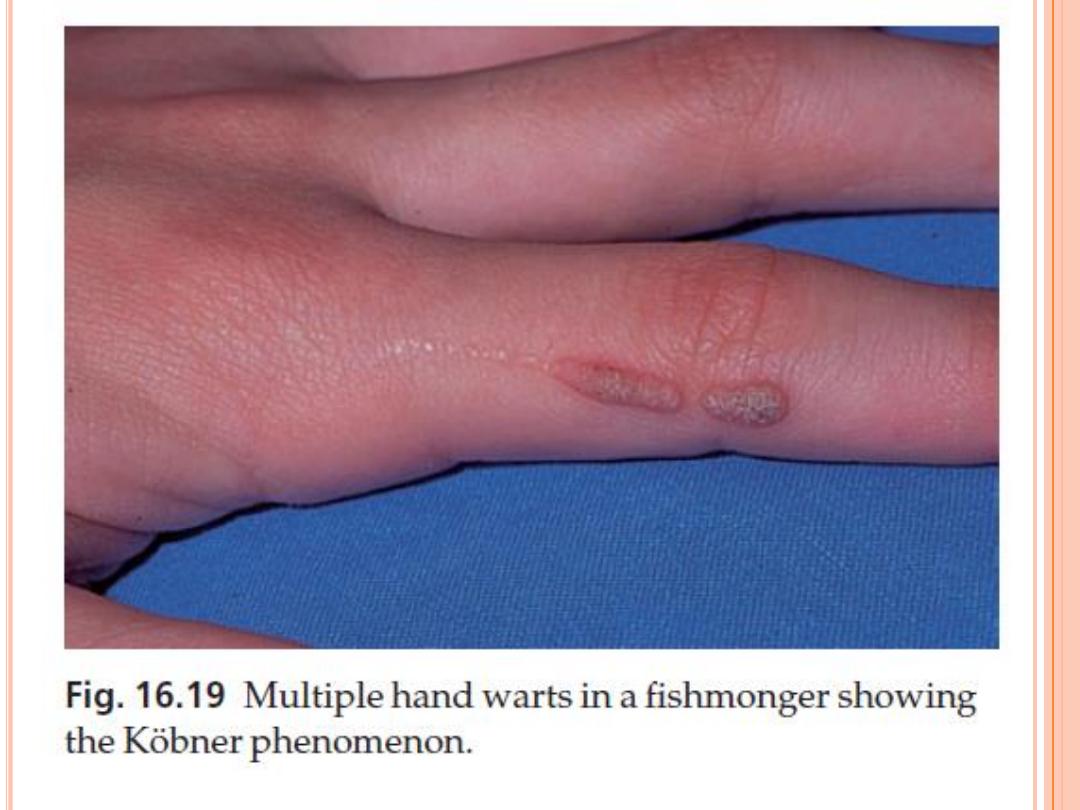
Infections occur when wart virus in skin scales
comes into contact with breaches in the skin or
mucous membranes or when immunity is
suppressed and dormant viruses escape from
their resting place in the outer root sheaths of
hairs.
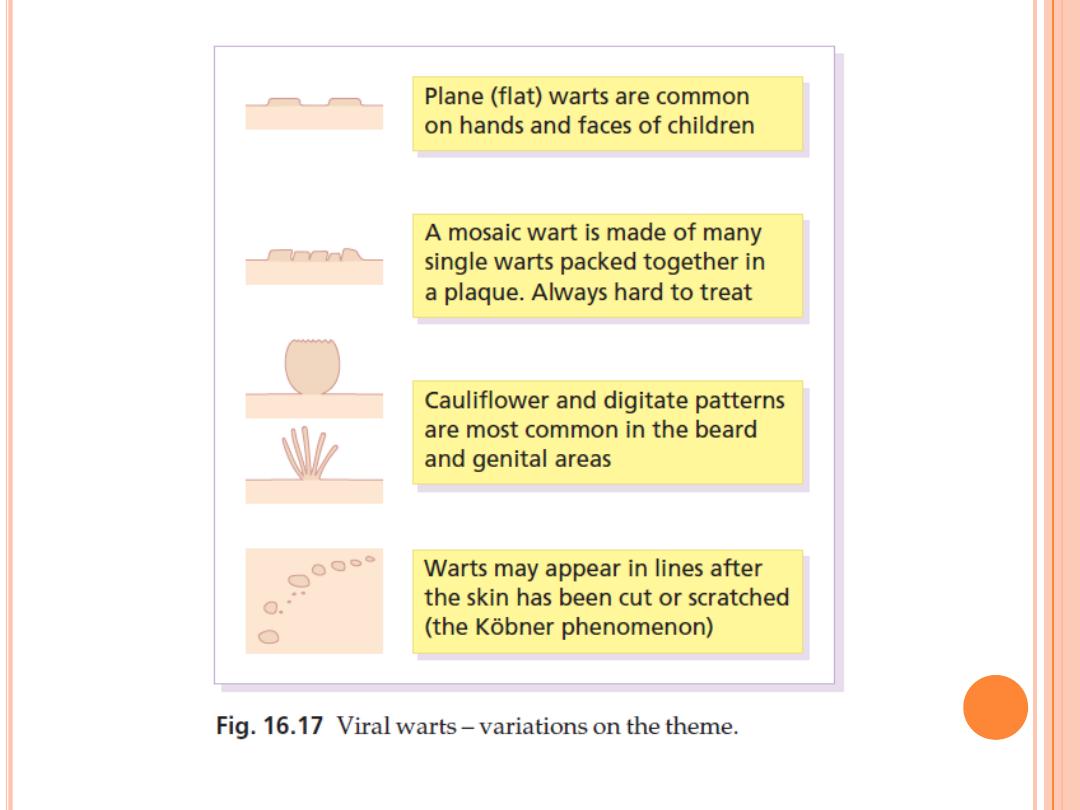

V
IRAL WARTS
Presentation
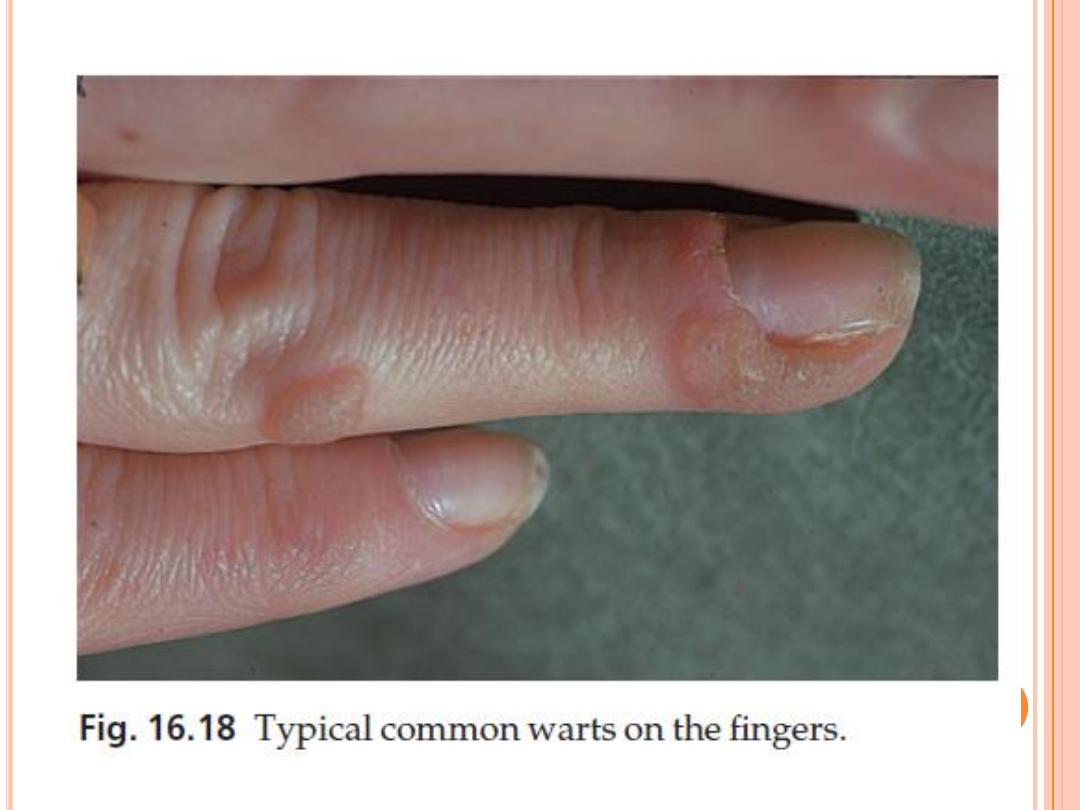
Common warts
is a smooth skin-coloured papule, often more
easily felt than seen
As the lesion enlarges, its irregular
hyperkeratotic surface give it the classic ‘warty’
appearance.
usually occur on the hands but are also often on
the face and genitals.
more often multiple than single.
Pain is rare.

V
IRAL WARTS
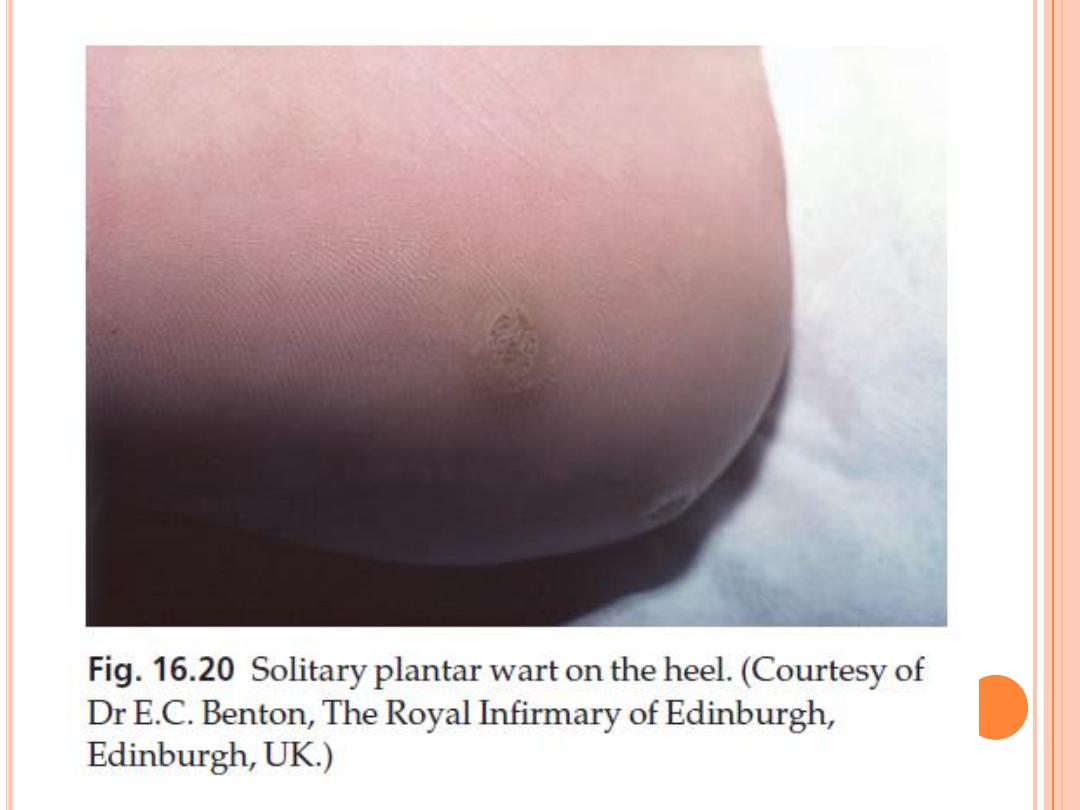
Plantar warts
have a rough surface, which protrudes only slightly from
the skin and is surrounded by a horny collar
On paring, the presence of bleeding capillary loops allows
plantar warts to be distinguished from corns.
Often multiple
plantar warts can be painful.
Mosaic warts
rough marginated plaques are made up of many small,
tightly packed but discrete individual warts.
They are most common on the soles but are also seen on
palms and around finger nails.
Usually they are not painful.


V
IRAL WARTS
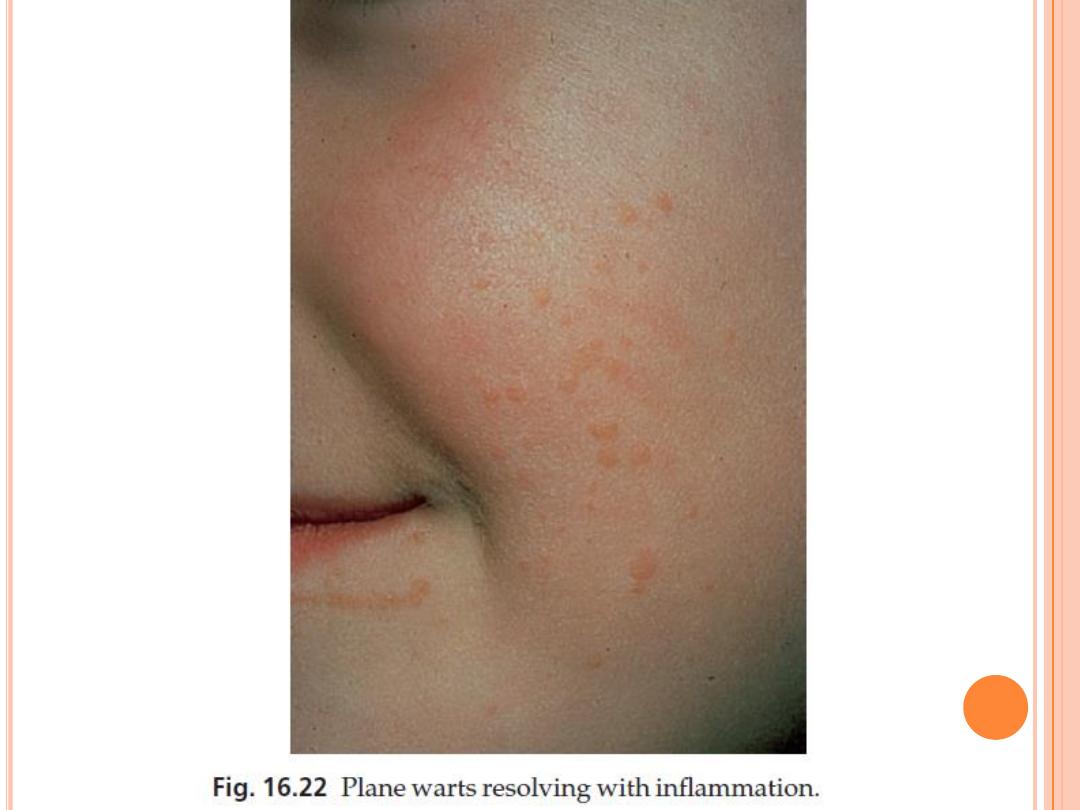
Plane warts
Are multiple, painless, smooth flat-topped papules
most common on the face and brow, on the backs of
the hands and on the shaven legs of women
they become inflamed as a result of an immunological
reaction, just before they resolve spontaneously
Facial warts
most common in the beard area of adult males and
are spread by shaving.
A digitate appearance is common.
Lesions are often ugly but are painless

V
IRAL WARTS
Anogenital warts (condyloma acuminata)
Papillomatous cauliflower-like lesions, with a moist
macerated vascular surface, can appear anywhere in
this area. They may coalesce to form huge fungating
plagues causing discomfort and irritation.
The vaginal and anorectal mucosae may be affected.
The presence of anogenital warts in children raises the
spectre of sexual abuse, but is usually caused by
autoinoculation from common warts elsewhere.

V
IRAL WARTS
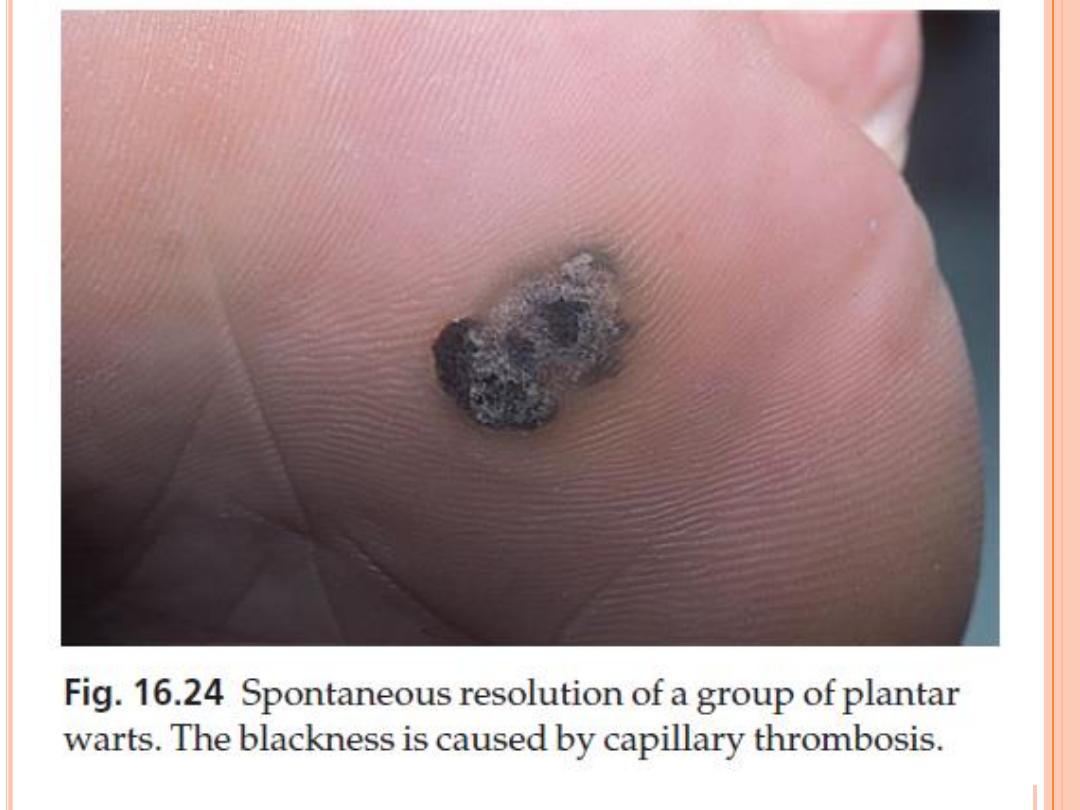
Course
Warts resolve spontaneously in the healthy as
the immune response overcomes the infection.
This happens within 6 months in some 30% of
patients, and within 2 years in 65%.
Such spontaneous resolution, sometimes
heralded by a punctate blackening caused by
capillary thrombosis leaves no trace.
Mosaic warts are notoriously slow to resolve and
often resist all treatments.
70% of renal allograft recipients will have warts
5 years after transplantation
V
IRAL WARTS
Complications
1.
Some plantar warts are very painful.
2.
Epidermodysplasia verruciformis
3.
Malignant change, rare
4.
infection with HPV types 16 and 18 predisposes
to cervical carcinoma.
HPV infections in immunocompromised patients
(e.g. renal allograft recipients) have also been
linked with skin cancer, especially on light-
exposed areas.

V
IRAL WARTS
T
REATMENT
Differential diagnosis
1.
Molluscum contagiosum
2.
Plantar corns
are found on pressure areas
there is no capillary bleeding on paring
They have a central keratotic core and are painful.
3.
Granuloma annulare
4.
Condyloma lata
5.
Amelanotic melanomas, squamous cell carcinomas and
other epithelial malignancies can present as verrucose
nodules – those in patients over the age of 40 years
should be examined with special care. Mistakes have been
made in the past.

V
IRAL WARTS
T
REATMENT
Palmoplantar warts
Regression of warts and prevention of their
recurrence depends on establishment of cell-mediated
immunity.
Salicylic acid (12–20%) paints or plasters
home treatment is best
Paints should be applied once daily, after moistening
the warts in hot water for at least 5 min.
Enough paint to cover the surface of the wart, is
applied and allowed to dry.
Warts on the plantar surface should be covered with
plasters although this is not necessary elsewhere.
Wart paints should not be applied to facial or
anogenital skin, or to patients with adjacent eczema.

V
IRAL WARTS
T
REATMENT
If no progress after 12 weeks, then a paint containing
formaldehyde or glutaraldehyde.
A useful way of dealing with multiple small plantar warts
is for the area to be soaked for 10 min each night in a 4%
formalin solution, although a few patients become allergic
to this.
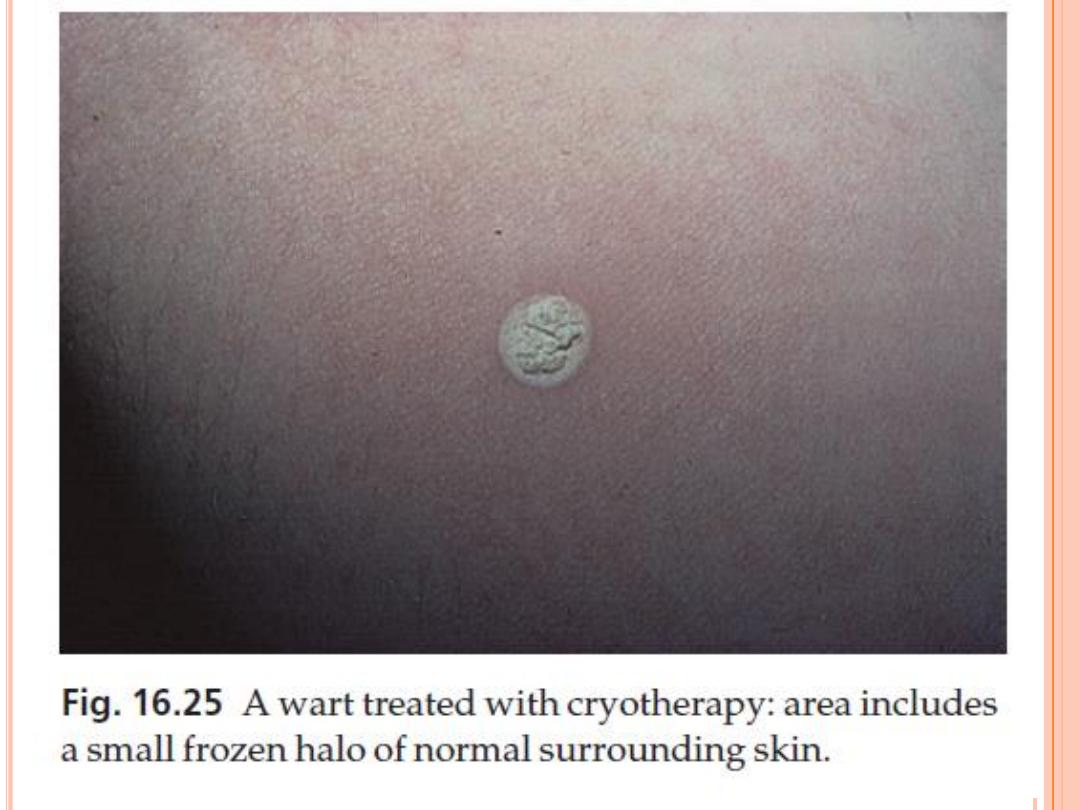
Cryotherapy
with liquid nitrogen (at −196°C) is more effective than the
less cold dry ice or dimethyl ether or propane techniques
it is painful
use of two freeze–thaw cycles increases the clearance rate of
plantar warts but not of hand warts.
If further treatments are necessary, the optimal interval is
3 weeks.

V
IRAL WARTS
T
REATMENT
Anogenital warts
Women with anogenital warts should have their cervical cytology
checked regularly as the wart virus can cause cervical cancer.
Podophyllotoxin (0.5% solution or 0.15% cream) or
imiquimod (5% cream)
Is self-treatment
Both are irritants and should be used carefully
Imiquimod is an immune modifier
It is applied three times weekly and washed off with a mild soap
6–10 h after application
Podophyllin paint (15%)
On the first occasion it should be washed off with soap and water
after 2 h but, if there has been little discomfort, this can be
increased stepwise to 6 h.
Treatment is best carried out weekly by a doctor or nurse, but not
by the patient.
Podophyllin must not be used in pregnancy.

V
IRAL WARTS
T
REATMENT
Anogenital warts
Cryotherapy, electrosurgery and laser treatment
are all effective treatments in the clinic.
Prevention of anogenital warts
By vaccine against the relevant HPV subtypes.
This appears to be highly effective at preventing
HPV infection, and subsequent cervical dysplasia
and cancer.

V
IRAL WARTS
T
REATMENT
Facial common warts
best treated with electrocautery or careful cryotherapy.
Scarring is an unwanted complication.
Shaving, if essential, should be with a brushless foam and a
disposable razor.
Plane warts
On the face these are best left untreated and the patient or
parent can be reasonably assured that spontaneous
resolution will occur.
When treatment is demanded, the use of a wart paint,
tretinoin gel or imiquimod cream is reasonable.

V
IRAL WARTS
T
REATMENT
Solitary, stubborn or painful warts
removed under local anaesthetic with a curette, a
scar often follows.
Surgical excision is never justifiable
Bleomycin can also be injected into such warts
but only be undertaken by a specialist

V
ARICELLA
(
CHICKENPOX
)
Cause
virus varicella-zoster is spread by the respiratory route
its incubation period is about 14 days.
Presentation and course
Slight malaise is followed by the development of papules, which
turn rapidly into clear vesicles on a pink base (dewdrops on a rose
petal).
Vesicles soon become pustules and then umbilicate.
Over the next few days the lesions crust and then clear,
sometimes leaving white depressed scars.
Lesions appear in crops, are often itchy, and are most profuse on
the trunk and least profuse on the periphery of the limbs
(centripetal).
Second attacks are rare.
Varicella can be fatal in those who are immunologically
compromised.

V
ARICELLA
(
CHICKENPOX
)
Complications
Pneumonitis, with pulmonary opacities on X-ray.
Secondary infection of skin lesions.
Haemorrhagic or lethal chickenpox in leukaemics and other
immunocompromised children and adults.
Scarring.
Investigations
None are usually needed.
The Tzanck smear is positive.
Treatment
In mild attacks, calamine lotion topically is all that is required
Aciclovir, famciclovir and valaciclovir should be reserved for severe
attacks and for immunocompromised patients
Prevention
A live attenuated vaccine is now available
should not be given to patients with immunodeficiencies, therapeutic
immunosuppression or blood dyscrasias who might not be able to
resist even the attenuated organism

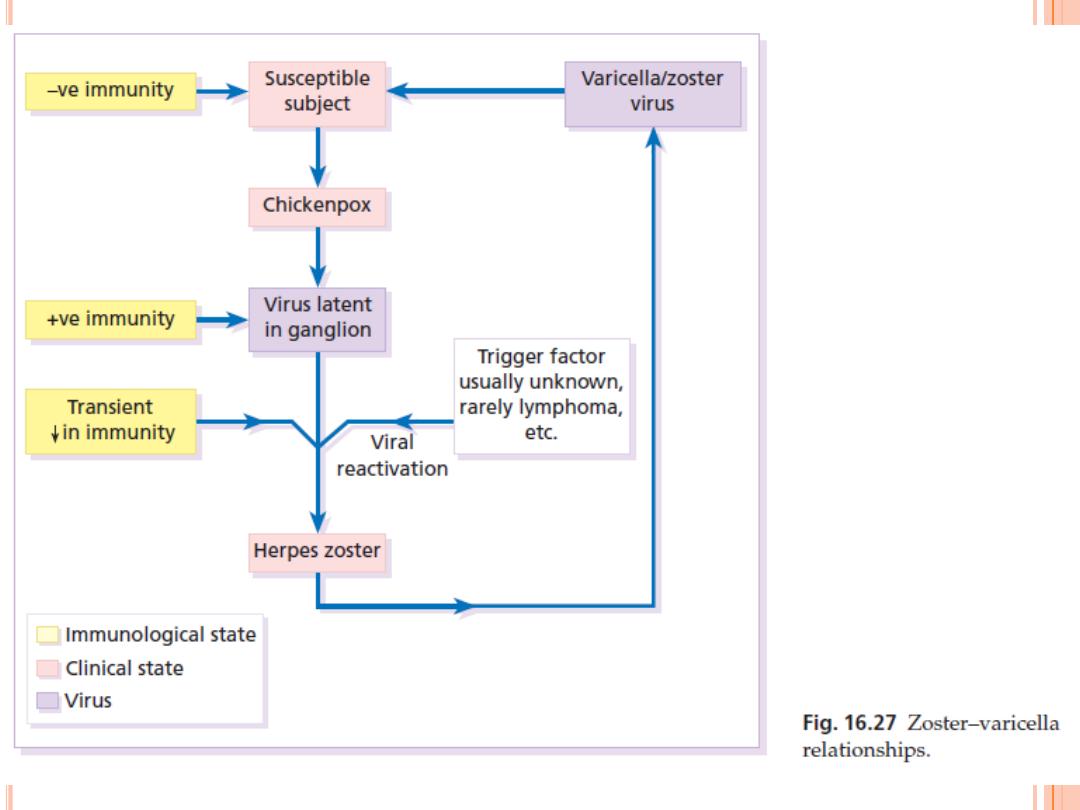
H
ERPES ZOSTER
(S
HINGLES
)
Cause
caused by the virus varicella-zoster
result of the reactivation of virus that has
remained dormant in a sensory root ganglion
since an earlier episode of chickenpox (varicella).
The incidence of shingles is highest in old age,
and in conditions such as Hodgkin’s disease,
AIDS and leukaemia, which weaken normal
defence mechanisms.
Shingles does not occur in epidemics
patients with zoster can transmit the virus to
others in whom it will cause chickenpox

H
ERPES ZOSTER
(S
HINGLES
)
Presentation and course
Attacks usually start with a burning pain, soon followed by
erythema and grouped, sometimes blood-filled, vesicles
scattered over a dermatome
The clear vesicles quickly become purulent, and over the
space of a few days burst and crust.
Scabs usually separate in 2–3 weeks, sometimes leaving
depressed depigmented scars.
Zoster is characteristically unilateral but may affect more
than one adjacent dermatome.
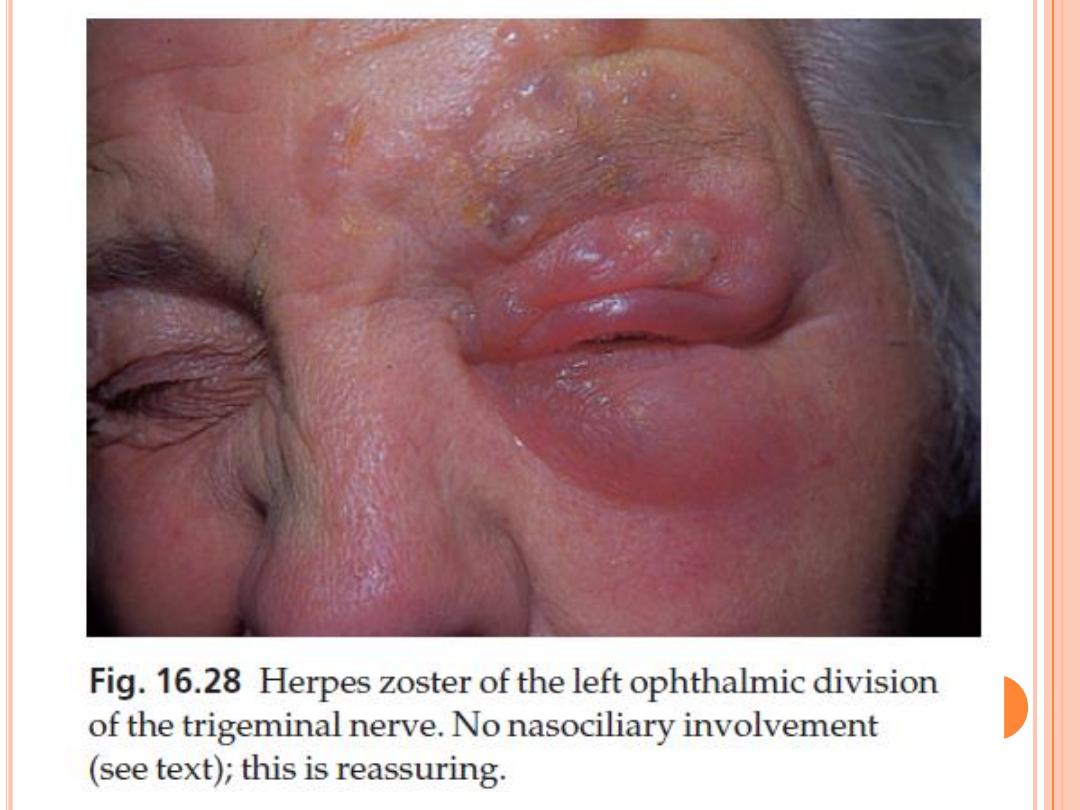
The thoracic segments and the ophthalmic division of the
trigeminal nerve are involved disproportionately often.
a generalized chickenpox-like eruption accompanying
segmental zoster should raise suspicions of an underlying
immunocompromised state or malignancy, particularly if
the lesions are unusually haemorrhagic or necrotic.

H
ERPES ZOSTER
(S
HINGLES
)
Complications
1.
Secondary bacterial infection is common.
2.
Motor nerve involvement is uncommon, but has
led to paralysis of ocular muscles, the facial
muscles, the diaphragm and the bladder.
3.
Zoster of the ophthalmic division of the
trigeminal nerve can lead to corneal ulcers and
scarring.
Persistent neuralgic pain, after the acute
episode is over, is most common in the elderly. A
good clinical clue here is involvement of the
nasociliary branch (vesicles grouped on the side
of the nose).

C
OMPLICATIONS
Investigations
Cultures are of little help as they take 5–7 days,
andare only positive in 70% of cases.
Biopsy or Tzanck smears
Any clinical suspicions about underlying
conditions, such as Hodgkin’s disease, chronic
lymphatic leukaemia or AIDS, require further
investigation.

C
OMPLICATIONS
Treatment
1.
Antivirals
Systemic treatment should be given to all patients within the first
5 days of an attack.
Famciclovir and valaciclovir are as effective as aciclovir
All three drugs are safe, and reduce the chance of post-herpetic
neuralgia, particularly in the elderly.
If diagnosed late in the course of the disease, systemic treatment
is not likely to be effective and treatment should be supportive
with rest, analgesics and bland applications such as calamine.
2.
Secondary bacterial infection should be treated appropriately.
3.
A trial of systemic carbamazepine, gabapentin or Amitriptyline
may be worthwhile for established post-herpetic neuralgia.
Prevention
Vaccination of elderly patients with a live attenuated vaccine to
the varicella-zoster virus has been shown to reduce the incidence
of both herpes zoster and postherpetic neuralgia.

H
ERPES SIMPLEX
Cause
Herpesvirus hominis is the cause of herpes simplex.
carriers continue to shed virus particles in their saliva or
tears.
two types
1.
lesions caused by type II virus occur mainly on the
genitals
2.
while those of type I are usually extragenital
however, this distinction is not absolute.
The route of infection is through mucous membranes or
abraded skin.
After the primary infection, the virus may become latent,
possibly within nerve ganglia, but still capable of giving rise
to recurrent bouts of vesication.

H
ERPES SIMPLEX
Presentation
Primary infection
Acute gingivostomatitis accompanied by malaise,
headache, fever and enlarged cervical nodes.
Vesicles, soon turning into ulcers, can be seen
scattered over the lips and mucous membranes.
The illness lasts about 2 weeks.
The virus can also be inoculated directly into the skin
(e.g. during wrestling), herpetic whitlow is one
example of this direct inoculation.
Primary type II virus infections, usually transmitted
sexually, cause multiple and painful genital or
perianal blisters which rapidly ulcerate.
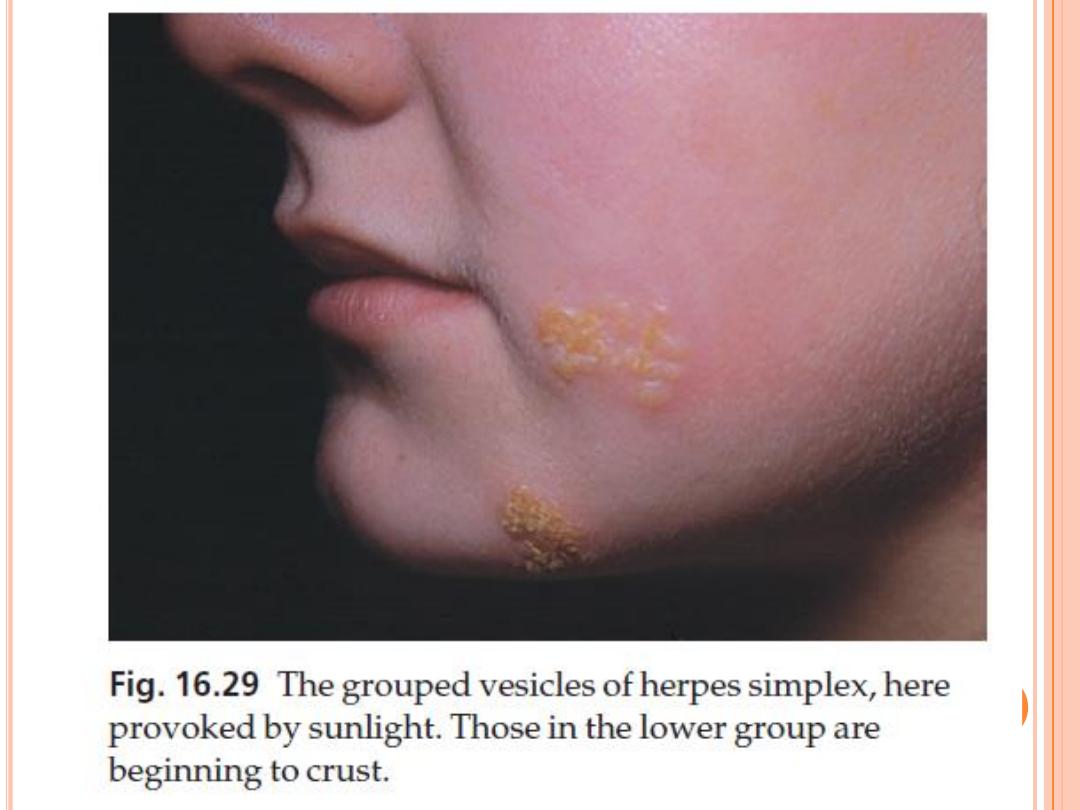

H
ERPES SIMPLEX
Recurrent (recrudescent) infections
These strike in roughly the same place each time.
They may be precipitated by respiratory tract
infections (cold sores), ultraviolet radiation,
menstruation or even stress.
Common sites include the face, the lips (type I)
and the genitals (type II), but lesions can occur
anywhere.
Tingling, burning or even pain is followed within
a few hours by the development of erythema and
clusters of tense vesicles
The whole episode lasts about 12 days.

H
ERPES SIMPLEX
Complications
1.
Herpes encephalitis or meningitis can occur
without any cutaneous clues.
2.
Disseminated herpes simplex: widespread
vesicles may be part of a severe illness in
newborns, debilitated children or
immunosuppressed adults.
3.
Eczema herpeticum: patients with atopic
eczema are particularly susceptible to
widespread cutaneous herpes simplex infections
4.
Recurrent dendritic ulcers leading to corneal
scarring.
5.
Erythema multiforme
H
ERPES SIMPLEX
Treatment
‘Old-fashioned’ remedies suffice for occasional mild
recurrent attacks
sunblock may cut down their frequency.
secondary bacterial infection can be reduced by topical
bacitracin, mupirocin, framycetin or fusidic acid.
Aciclovir cream, applied five or six times a day for the first
4 days of the episode, may cut down the length of attacks.
More effective still is oral aciclovir 200 mg five times daily
for 5 days, although this is usually reserved for those with
widespread or systemic involvement.
Famciclovir and valaciclovir are as effective as aciclovir,
having the additional advantage of better absorbtion and
fewer doses per day.
Recurrences in the immunocompromised can usually be
prevented by long-term treatment at a lower dosage.
M
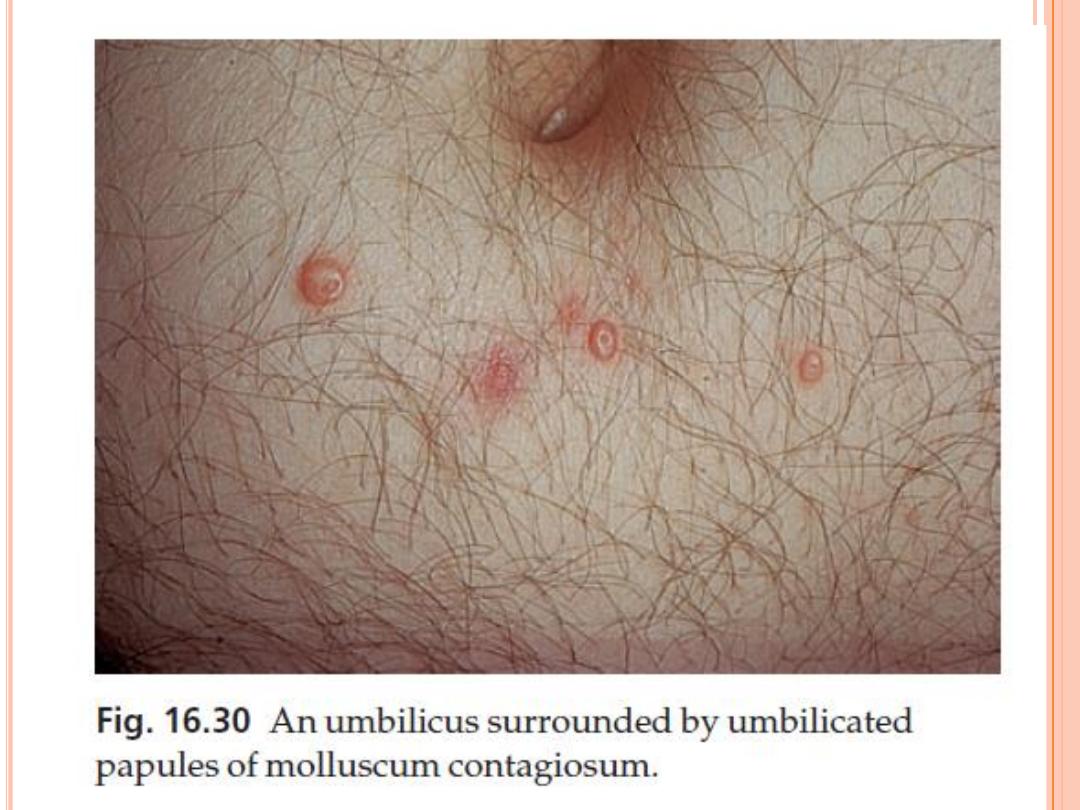
OLLUSCUM CONTAGIOSUM
pox virus infection
spread by direct contact (e.g. sexually or by sharing a towel
at the swimming bath).
Presentation and course
The incubation period ranges from 2 to 6 weeks Often
several members of one family are affected.
Individual lesions are shiny, white or pink, and
hemispherical; they grow slowly up to 0.5 cm in diameter.
A central punctum, which may contain a cheesy core, gives
the lesions their characteristic umbilicated look.
Multiple lesions are common
Atopic individuals and the immunocompromised are prone
to especially extensive infections, spread by scratching and
the use of topical steroids.
Untreated lesions usually clear in 6–9 months
Some leave depressed scars.
M
OLLUSCUM CONTAGIOSUM
Complications
Eczematous patches often appear around
mollusca.
Traumatized or overtreated lesions may become
secondarily infected.
Differential diagnosis
Inflamed lesions can simulate a boil.
Large solitary lesions in adults can be confused
with a keratocanthoma
Intradermal naevus
cystic basal cell carcinoma

M
OLLUSCUM CONTAGIOSUM
Treatment
Many simple destructive measures cause
inflammation and then resolution.
They include squeezing out the lesions with
forceps, piercing them with an orange stick
(preferably without phenol) and curettage
Liquid nitrogen, wart paints and topical
imiquimod may also be helpful.
These measures are fine for adults, but young
children dislike them and as mollusca are
selflimiting, doing nothing is often the best
option.

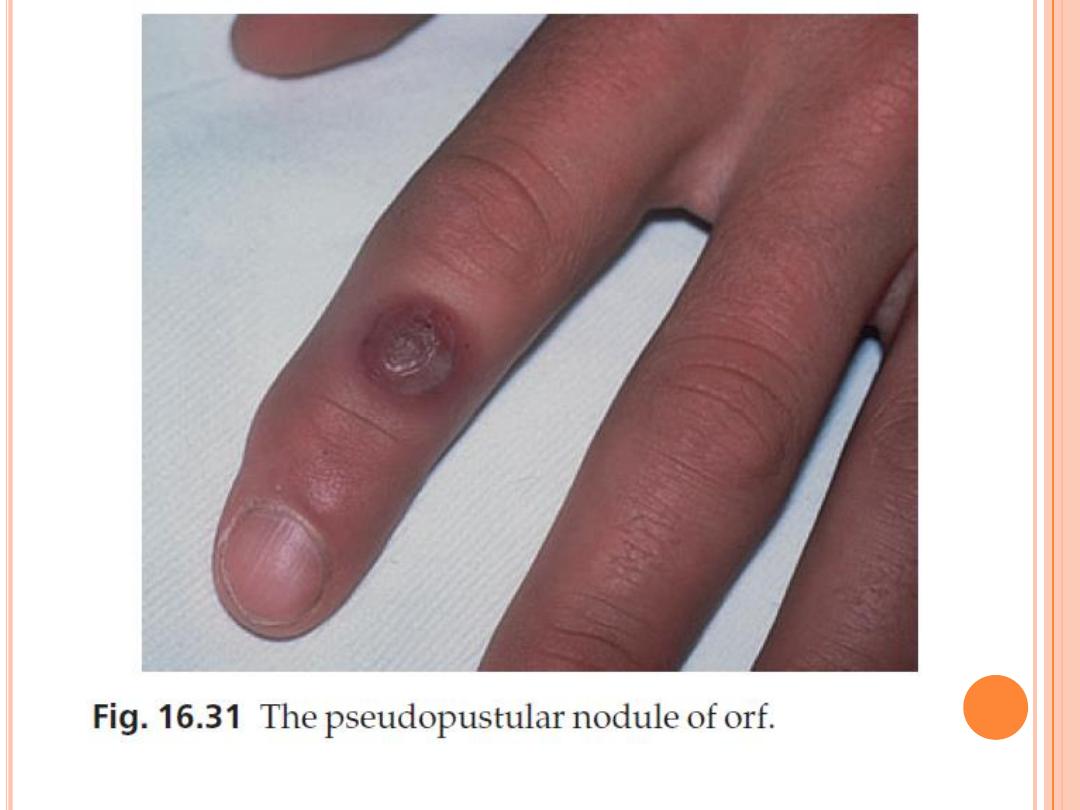
O
RF
Cause
Its cause is a parapox virus that can be transmitted to
those handling infected animals.
most commonly seen on the hands of shepherds, of
their wives who bottle-feed lambs and of butchers,
vets and meat porters.
Presentation and course
The incubation period is 5–6 days.
Lesions, which may be single or multiple, start as
small firm papules that change into flat-topped,
apparently pustular nodules with a violaceous and
erythematous rim
The condition clears up spontaneously in about a
month.

O
RF
Complications
Lymphadenitis and malaise are common.
Erythema multiforme.
‘Giant’ lesions can appear in the
immunosuppressed.
Treatment
A topical antibiotic helps to prevent secondary
infection; otherwise no active therapy is needed

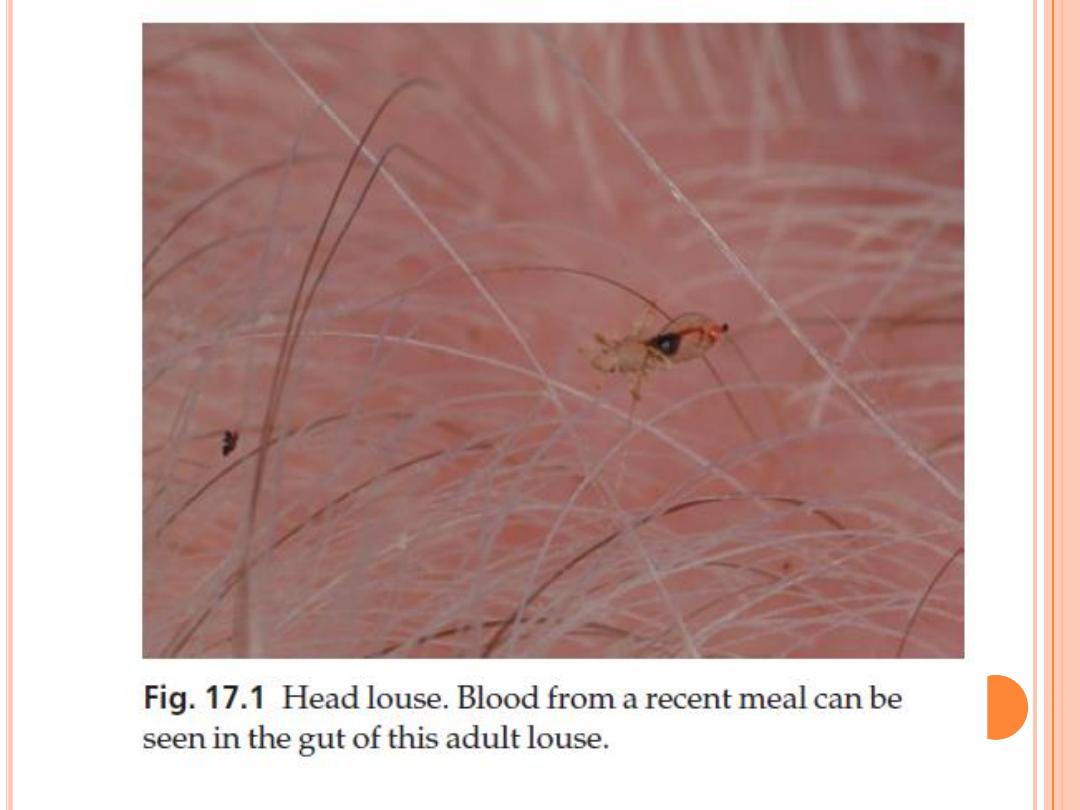
I
NFESTATIONS

L
ICE INFESTATIONS
(
PEDICULOSIS
)
Lice are flattened wingless insects that suck blood.
Their eggs, attached to hairs or clothing, are known as
nits.
The main feature of all lice infestations is severe
itching, followed by scratching and secondary
infection.
Two species are obligate parasites in humans:
1.
Pediculus humanus (with its two varieties: P.
humanus capitis, the head louse, and P. humanus
corporis, the body louse)
2.
Phthirus pubis (the pubic louse).

H
EAD LICE
Cause
still common: up to 10% of children have them,
even in the smartest schools.
Many of these children have few or no symptoms.
Infestations peak between the ages of 4 and 11
years, and are more common in girls than boys.
A typical infested scalp will carry about 10 adult
lice
Egg cases (nits) can be seen easily enough,
firmly stuck to the hair shafts.
Spread from person to person is achieved by
head-to-head contact, and perhaps by shared
combs or hats.

H
EAD LICE
Presentation and course
The main symptom is itching, although this may
take several months to develop.
At first the itching is mainly around the sides
and back of the scalp: later it spreads generally
over the scalp. Scratching and secondary
infection soon follow
in heavy infestations, the hair becomes matted
and smelly.
Draining lymph nodes often enlarge

H
EAD LICE
Complications
Secondary bacterial infection may be severe enough to
make the child listless and feverish.
Differential diagnosis
All patients with recurrent impetigo or crusted
eczema on their scalps should be carefully examined
for the presence of nits.
Diagnosis
The finding of living moving lice means that the
infestation is current and active, and needs
treatment.
Empty egg cases signify only that there has been an
infestation in the past, but suggest the need for
periodic re-inspection.
H
EAD LICE
Treatment
Malathion, carbaryl and synthetic pyrethroids
(phenothrin and permethrin) are the
treatments of choice now.
They are equally effective at killing lice and eggs
malathion has the extra virtue of sticking to the
hair and so protecting against re-infection for 6
weeks.
Lotions should remain on the scalp for at least 12
h, and are more effective than shampoos.
The application should be repeated after 1 week
so that any lice that survive the first application
and hatch out in that interval can be killed

H
EAD LICE
systemic antibiotic may be needed to deal with
severe secondary infection.
If live lice are found on follow-up, a pediculicide
from another chemical class should be used.
Pillow cases, towels, hats and scarves should be
laundered or dry cleaned.
Other members of the family and school mates
should be checked.
Systemic ivermectin therapy is reserved for
infestations resisting the treatments listed above
B
ODY LICE
are now uncommon except in the unhygienic and
socially deprived.
Morphologically, the body louse looks just like the
head louse, but lays its eggs in the seams of
clothing in contact with the skin.
Transmission is via infested bedding or clothing.

B
ODY LICE
Presentation and course
Self-neglect is usually obvious
severe and widespread itching especially on the
trunk.
The bites themselves are soon obscured by
excoriations and crusts of dried blood or serum.
In chronic untreated cases (‘vagabond’s disease’),
the skin becomes generally thickened,
eczematized and pigmented; lymphadenopathy is
common.

B
ODY LICE
Differential diagnosis
In scabies, characteristic burrows are seen
eczema and lymphomas, but these are ruled out
by the finding of lice and nits.

T
REATMENT
First and foremost, treat the infested clothing
and bedding.
Lice and their eggs can be killed by high
temperature laundering, dry cleaning and
tumbledrying.
5% permethrin cream or 1% lindane lotion can be
used on the patient’s skin

P
UBIC LICE
Pubic lice (crabs) are broader than scalp and body
lice, and their second and third pairs of legs are
well adapted to cling on to hair.
usually spread by sexual contact, and most
commonly infest young adults.
Severe itching in the pubic area is followed by
eczematization and secondary infection.
small blue–grey macules of altered blood at the
site of bites.
Pubic lice spread most extensively in hairy males
and may even affect the eyelashes.

Investigations
The possibility of coexisting sexually transmitted
diseases should be kept in mind.

Treatment
Carbaryl, permethrin and malathion are all
effective treatments.
Aqueous solutions are less irritant than alcoholic
ones.
They should be applied for 12 h or overnight –
and not just to the pubic area, but to all
surfaces of the body, including the perianal
area, limbs, scalp, neck, ears and face (especially
the eyebrows and the beard, if present).
Treatment should be repeated after 1 week
infected sexual partners should also be treated.
Shaving the area is not necessary.
S
CABIES

S
CABIES
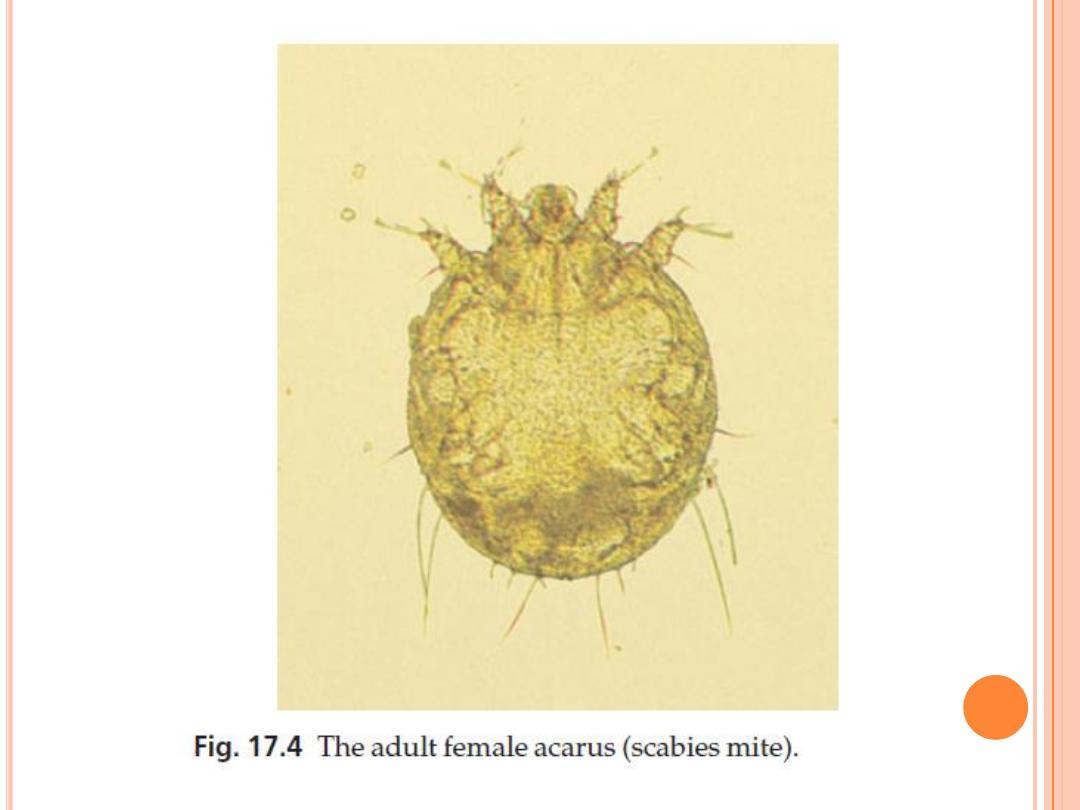
Cause
Scabies is caused by the mite Sarcoptes scabiei var.
hominis
mites are transferred from person to person by close
bodily contact and not via inanimate objects.
Once on the skin, fertilized female mites can move
over the surface at up to 2 cm/min, but can burrow
through the stratum corneum at only about 2
mm/day.
They produce two or three oval eggs each day, which
turn into sexually mature mites in 2–3 weeks.
The generalized eruption of scabies, and its itchiness,
are thought to be caused by a sensitization to the
mites or their products.

S
CABIES
Epidemiology
Scabies is endemic in many developing countries,
and high levels of prevalence go with poverty,
overcrowding and poor hygiene.
Scabies is most common in the autumn and
winter

S
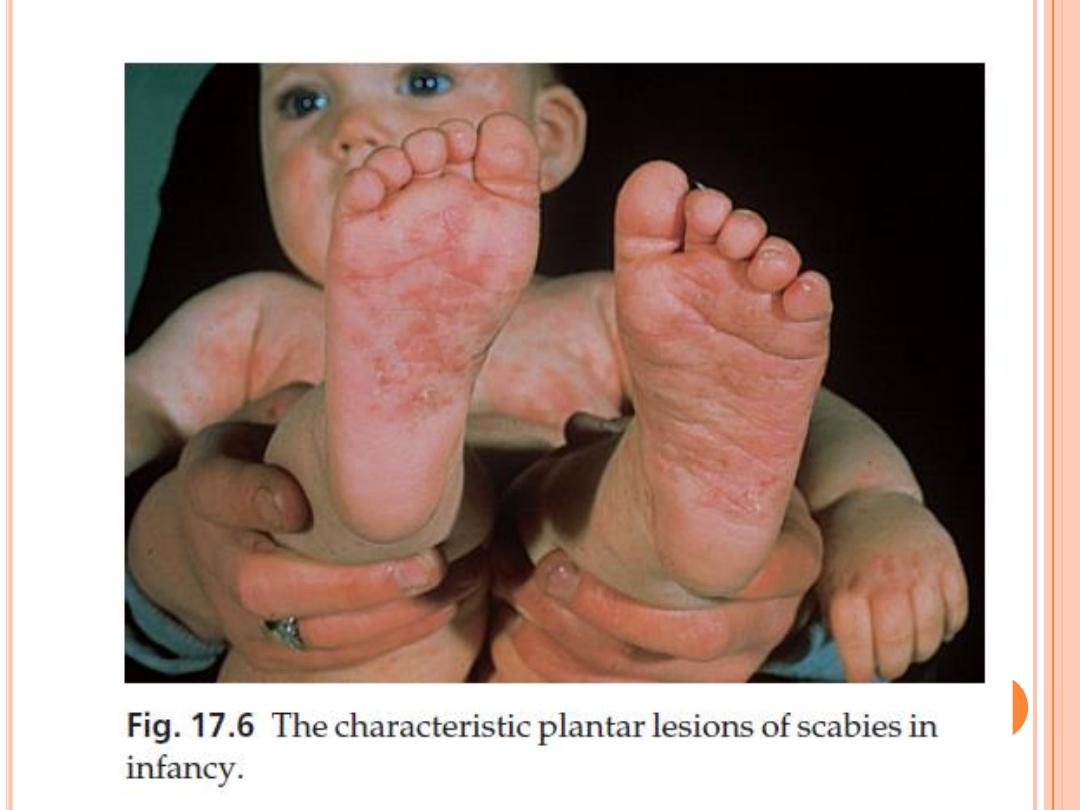
CABIES
Presentation
1.
Itching often being 4–6 weeks after a first infestation,
particularly bad at night and affecting several people.
In contrast, in a second attack of scabies, itching starts
within a day or two, because these victims already have
immunity to produce the itchy allergic reactions
2.
excoriated, eczematized or urticarial papules
3.
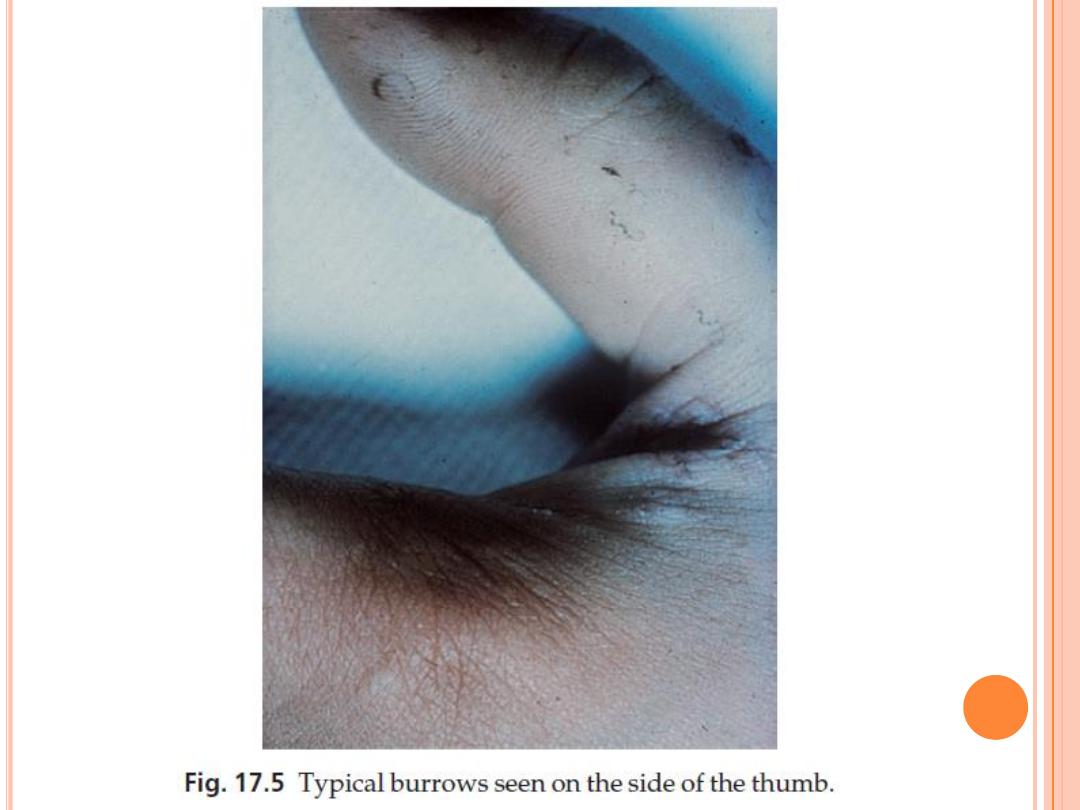
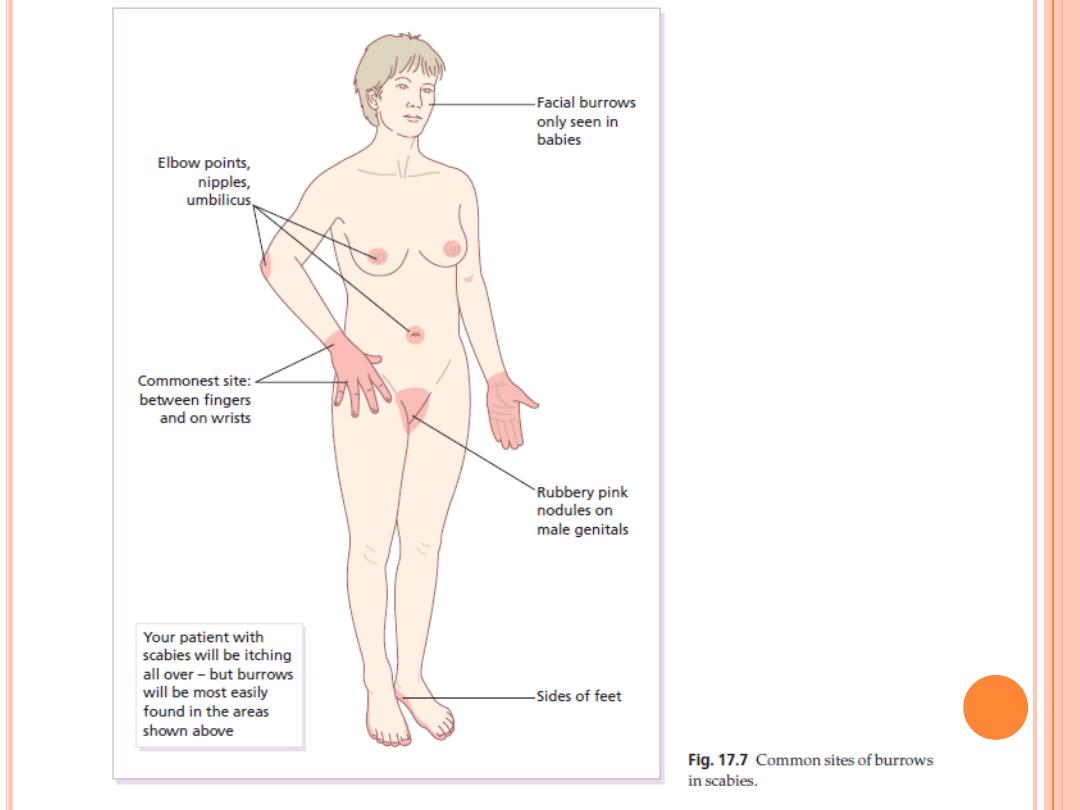
Burrows
Most burrows lie on the sides of the fingers, finger webs,
sides of the hand and on the flexural aspects of the wrists.
Other favourite sites include the elbows, ankles and feet,
nipples and genitals
Animal scabies from pets induces an itchy rash in humans
but this lacks burrows.
Only in infancy does scabies affect the face
S

S
CABIES
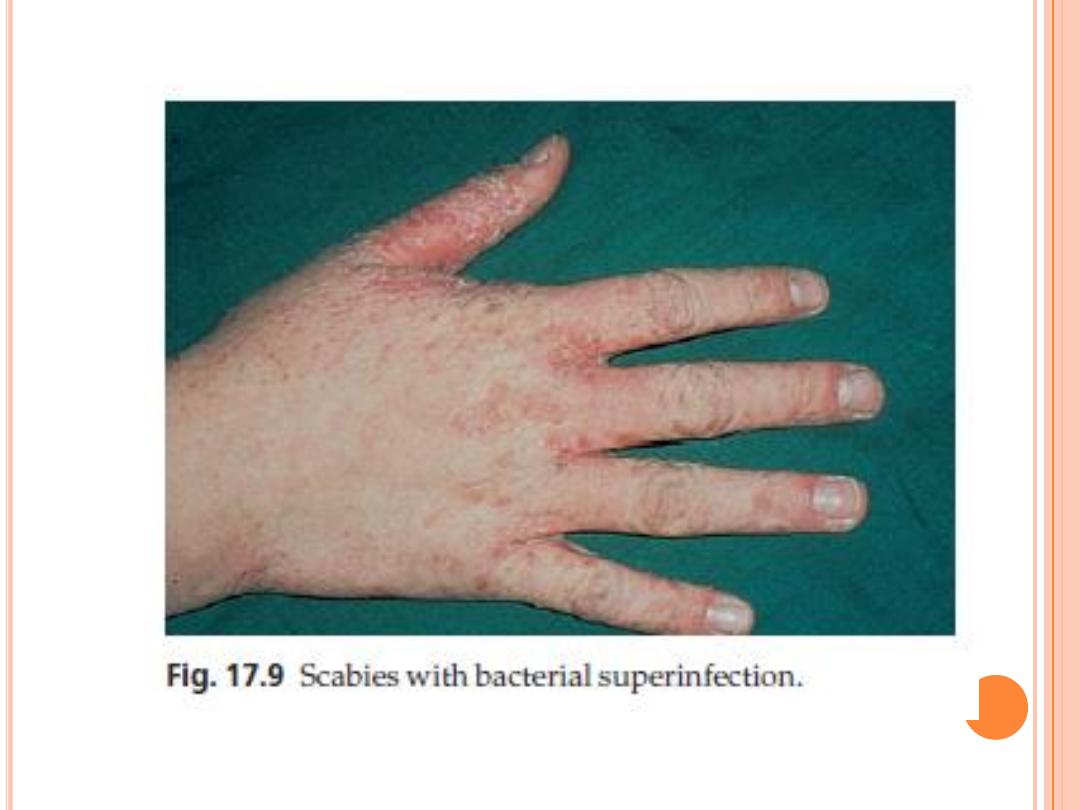
Complications
1.
Secondary infection, with pustulation, is common
2.
Repeated applications of scabicides can cause skin
irritation and eczema.
3.
Persistent itchy red nodules may remain on the
genitals or armpits of children for some months after
adequate treatment.
4.
Venereal disease may be acquired at the same time
as scabies.
5.
Crusted (Norwegian) scabies
may not be itchy
is a widespread crusted eruption in which vast numbers of mites are found
It affects people with mental retardation or immunosuppression, and can be the unsuspected
source of epidemics of ordinary scabies (e.g. in nursing homes).

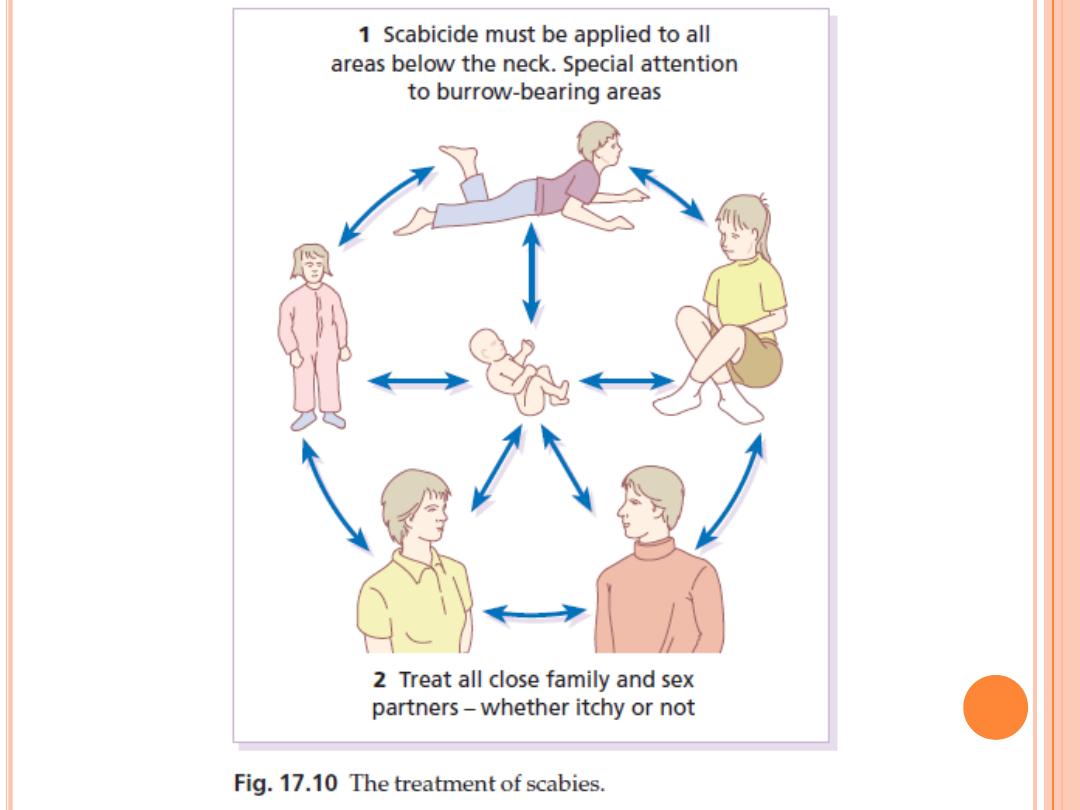
S
CABIES
Treatment
Do not treat just the patient; treat all members of the
family and sexual contacts too, whether they are itching or
not
Permethrin as first choice, with malathion as the second
choice
A second application, a week after the first
ivermectin in a single dose of 200 μg/kg by mouth, is
effective for Norwegian scabies and scabies that does not
respond to topical measures alone
Permethrin is probably safe in pregnancy and in nursing
mothers as little is absorbed
Permethrin is licensed for infants over the age of 2 months
Should be applied to the entire body except the face and
scalp in adults, in children apply to scalp also

S
CABIES
6% Precipitated sulphur in petrolatum is also
effective in children
Ordinary laundering deals satisfactorily with clothing
and sheets. Mites die in clothing unworn for 1 week.
Residual itching may last for several days, or even a
few weeks, but this does not need further applications
of the scabicide. Rely instead on calamine lotion or
crotamiton.

T
HIANKS
