
Renal Radiology
Dr. Mikdam Atia Khalaf
Radiology Department
Tikrit University – College of Medicine
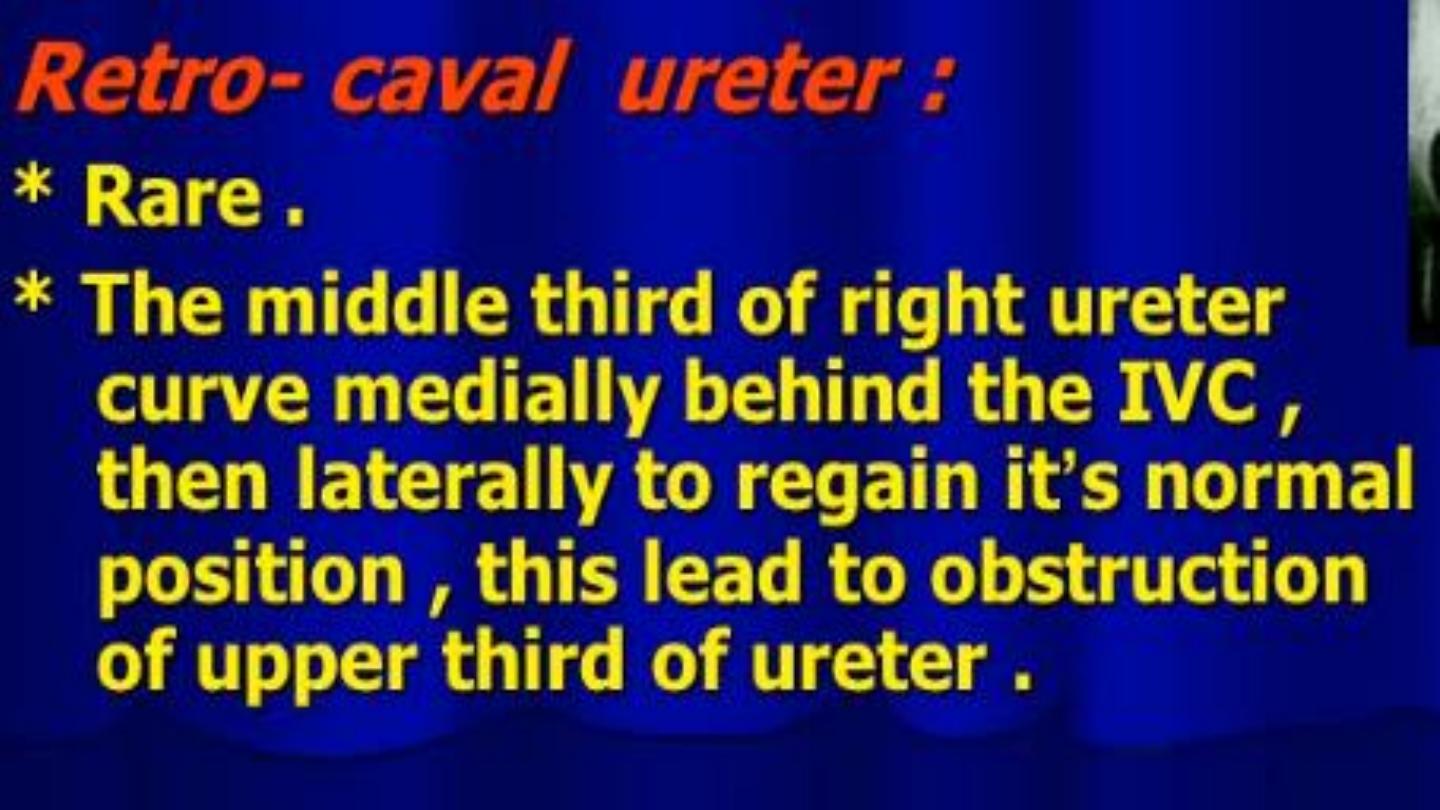
Coronal reformatted MIPS
image from a CT urogram
demonstrates medial
displacement of the right ureter
at the level of L3 (White arrow).
The ureter is medial to the
pedicle
of the vertebral body (blue
arrow)


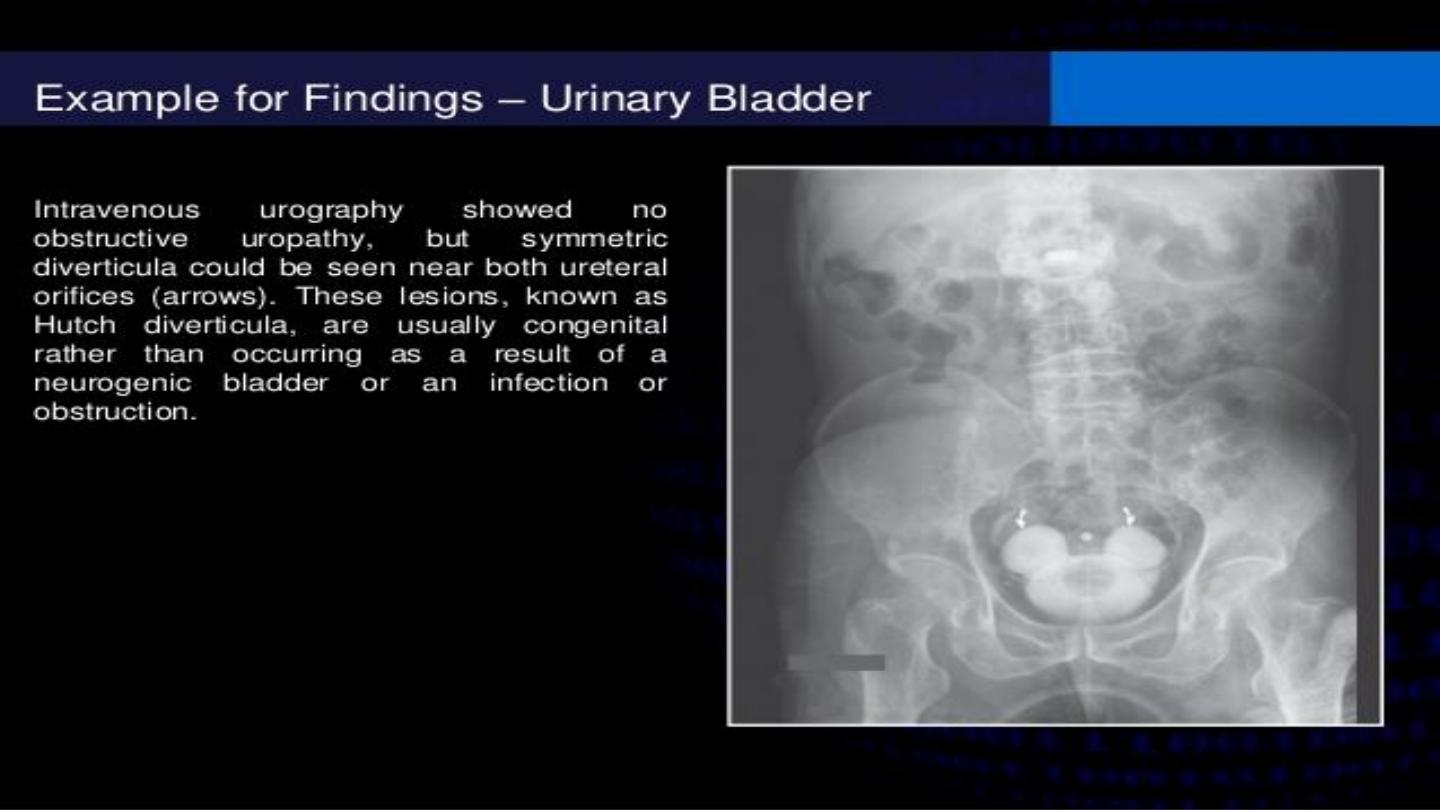
Intraveneous Urography

KUB



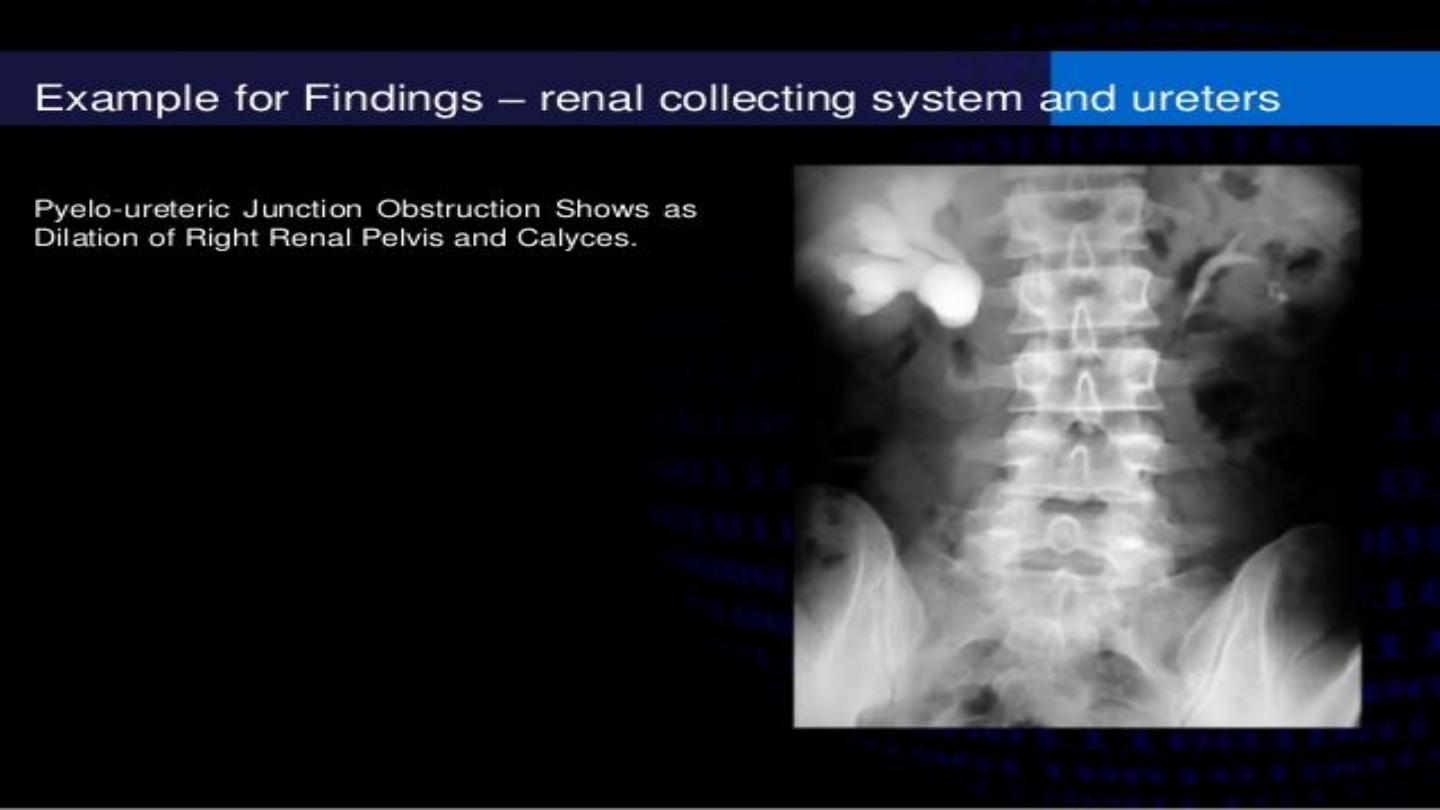

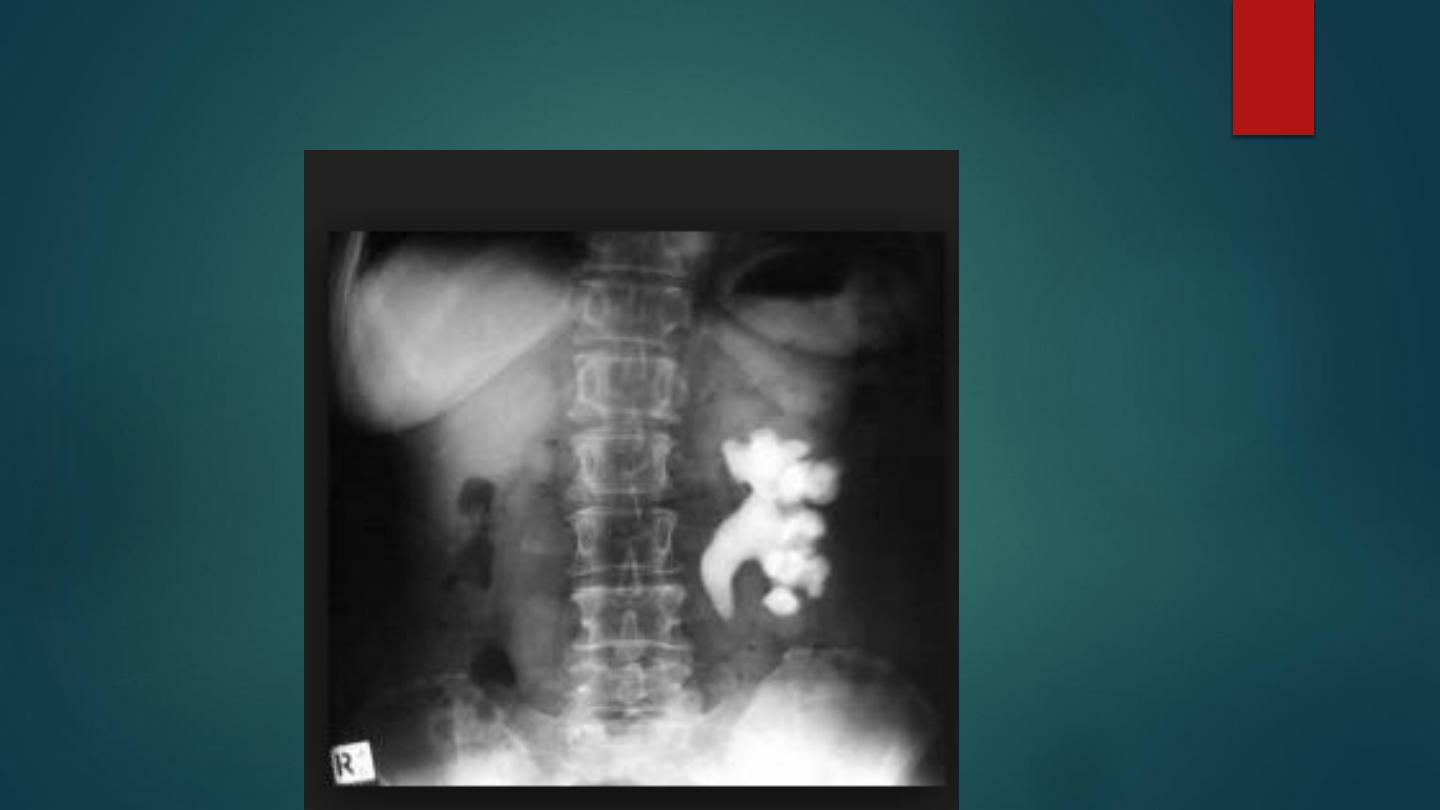
PUJ obstruction


NEPHROCALCINOSIS
Definition: Deposition of calcium within the renal parenchyma and outside of the pelvi-calyceal
system.
1- Medullary nephrocalcinosis: this is usually the product of a metabolic disorder resulting in a raised
serum calcium or a tubular defect resulting in hypercalciuria (usually bilateral and diffuse).
2- Cortical nephrocalcinosis: this is seen in acute cortical necrosis of any cause (classically with a
‘tramline’ appearance).
3- Focal nephrocalcinosis:
Linear or rim calcification
- Renal artery aneurysm and Real cyst.
Amorphous calcification
- Calcified haematoma
- Tuberculosis
- Renal cell carcinoma
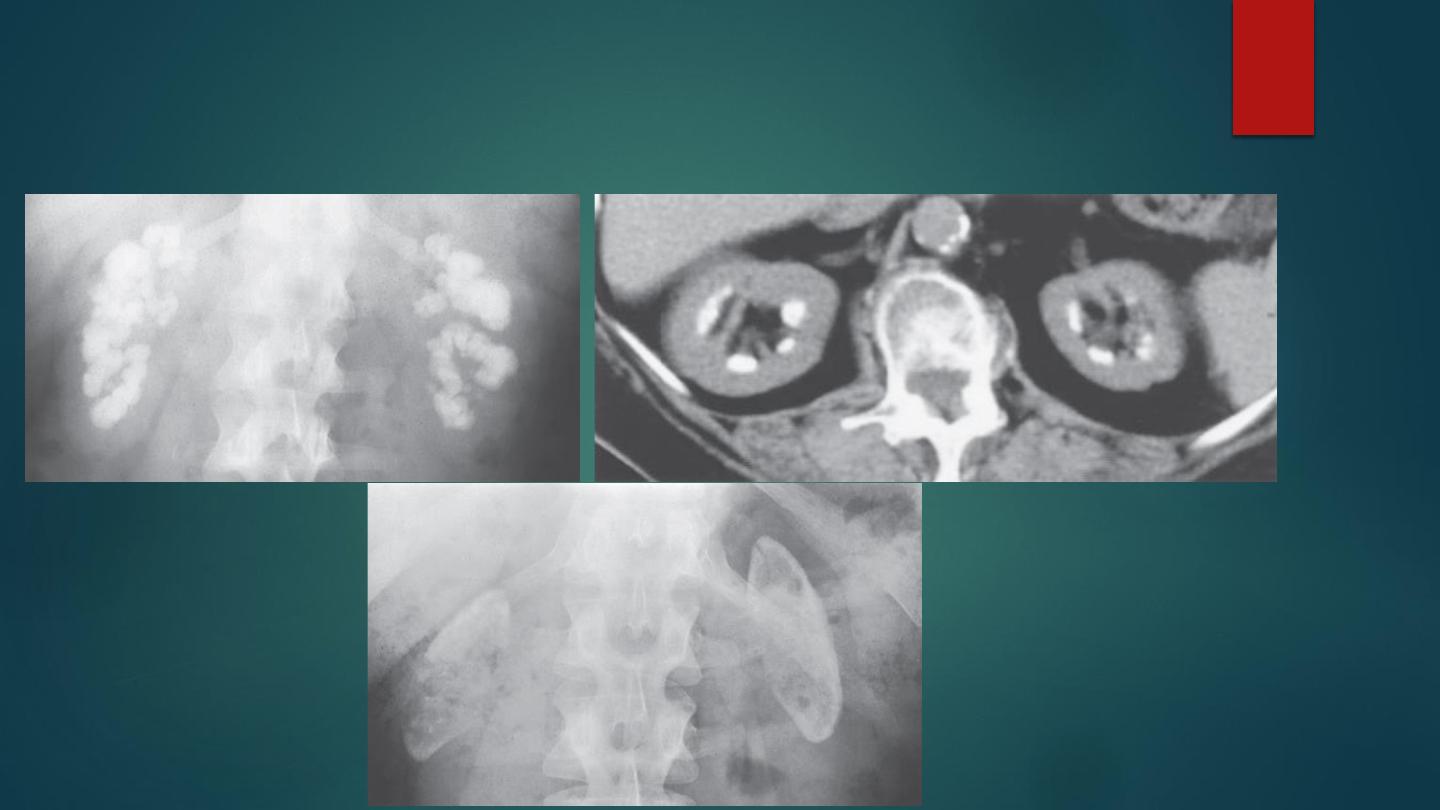
Medullary nephrocalcinosis with the corresponding CT appearances
Cortical nephrocalcinosis

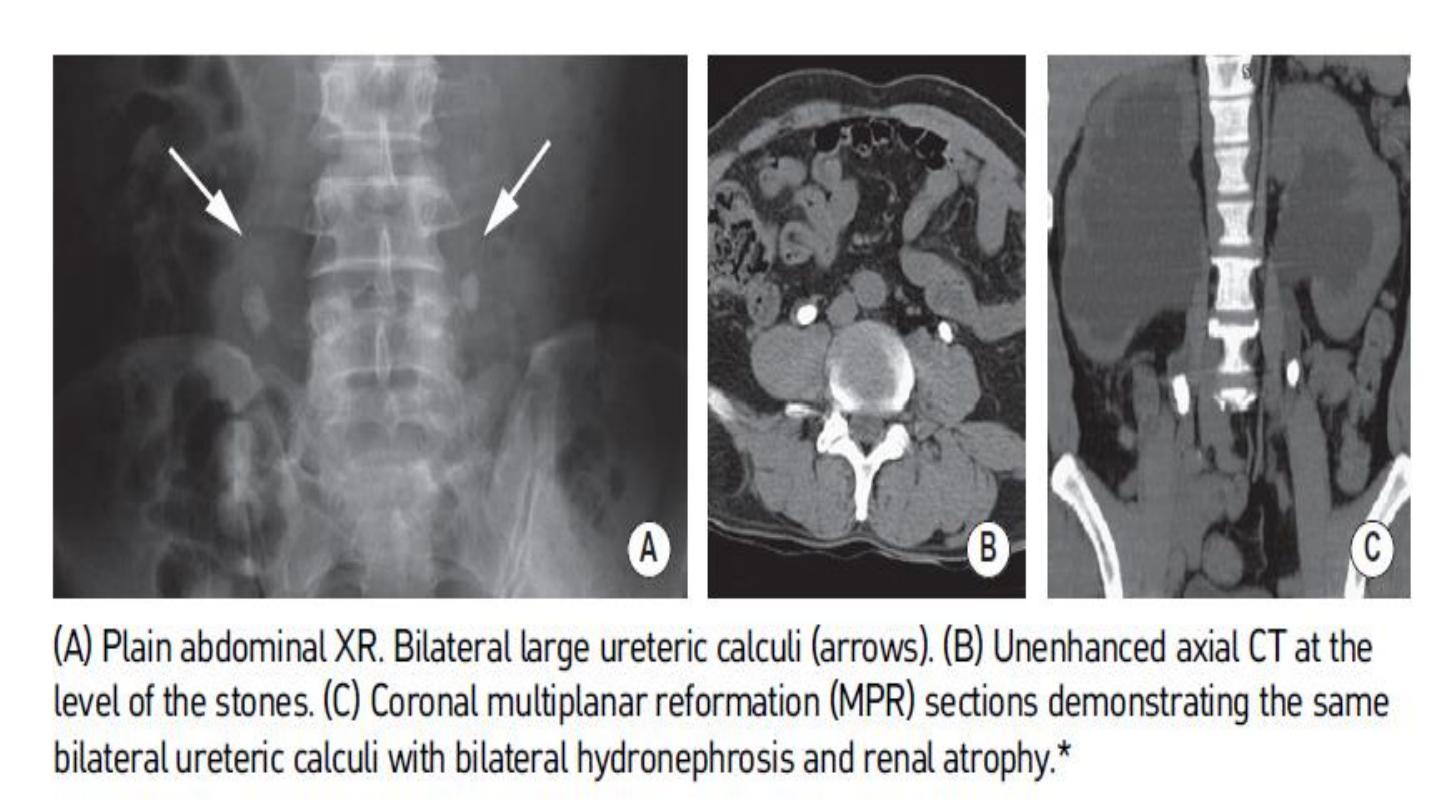
UROLITHIASIS
Stones form when the concentration of two ions in solution exceeds the saturation
point
•CLINICAL PRESENTATION
- Classically there is acute severe ipsilateral loin-to groin pain ( nausea and
vomiting).
- haematuria
- There is a peak age of onset between 20 and 30 years (2M:F).

RADIOLOGICAL FEATURES
KUB
The majority of calcium-containing stones are radio-opaque
Oxalate stones: these are denser than bone
Cysteine stones: these are less dense than bone
Uric acid stones: these are radiolucent
It has a poor sensitivity due to overlying bowel gas and extrarenal calcification
IVU
A dense nephrogram with delayed excretion.
A column of contrast may be seen down to the point of obstruction
The degree of ureteric dilatation is not related to the stone size
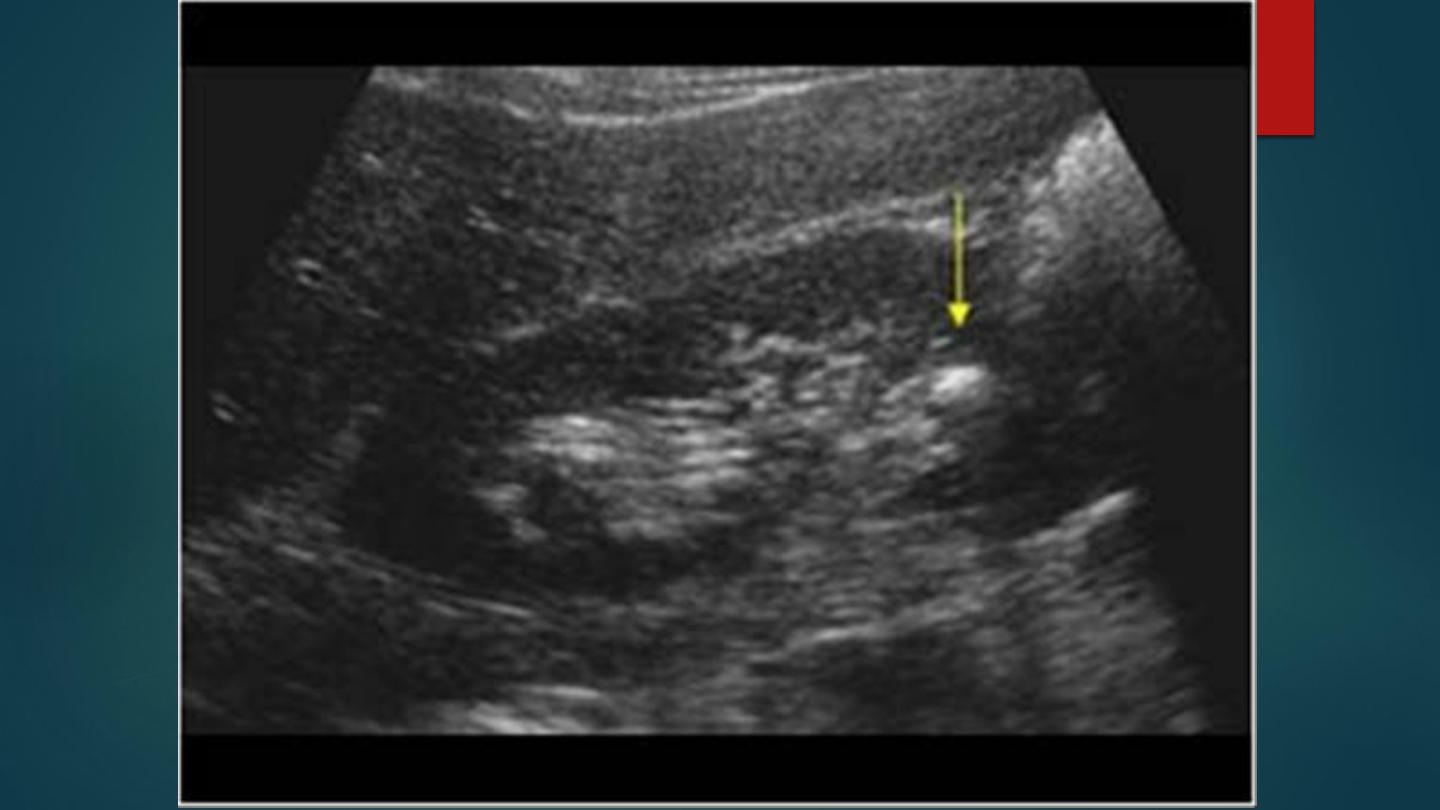
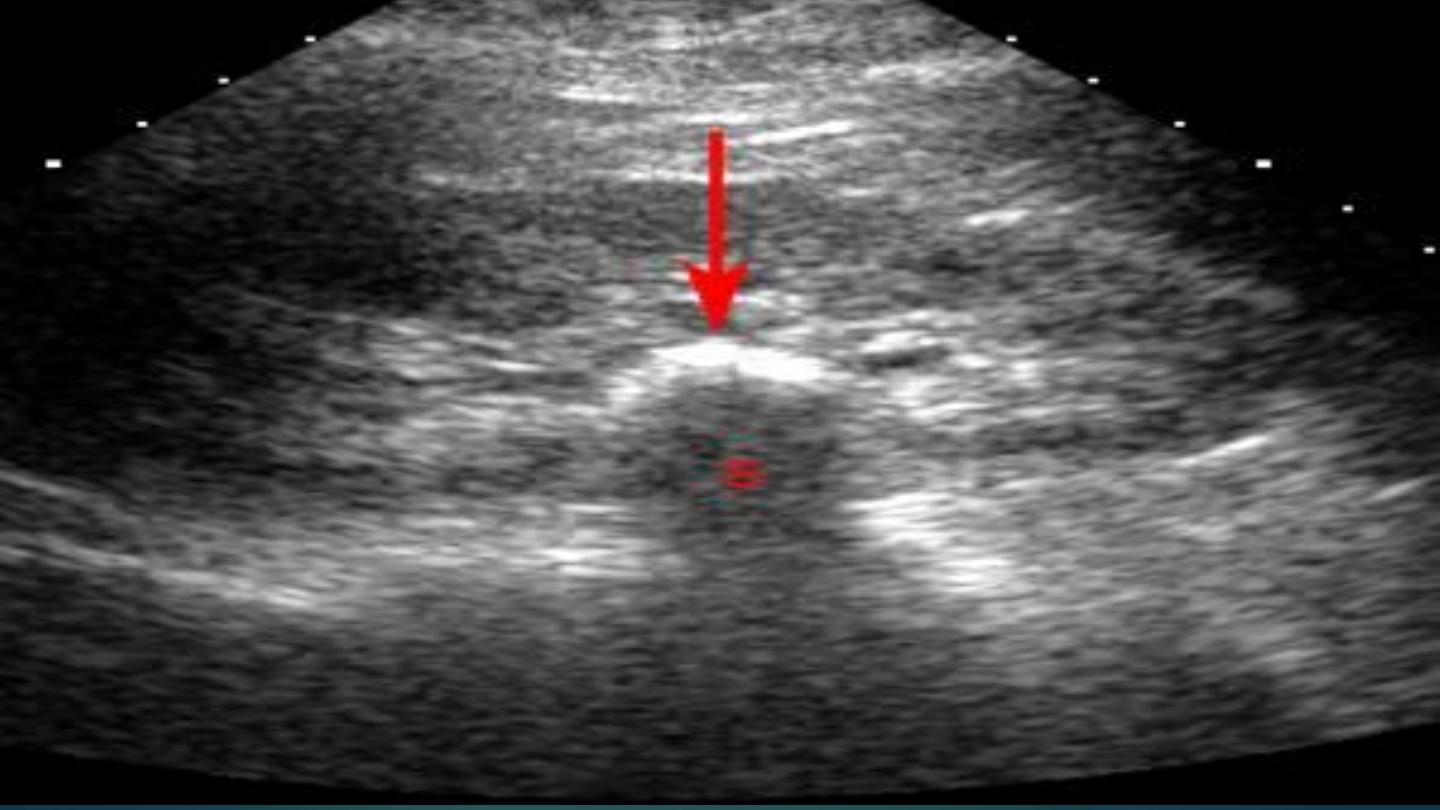
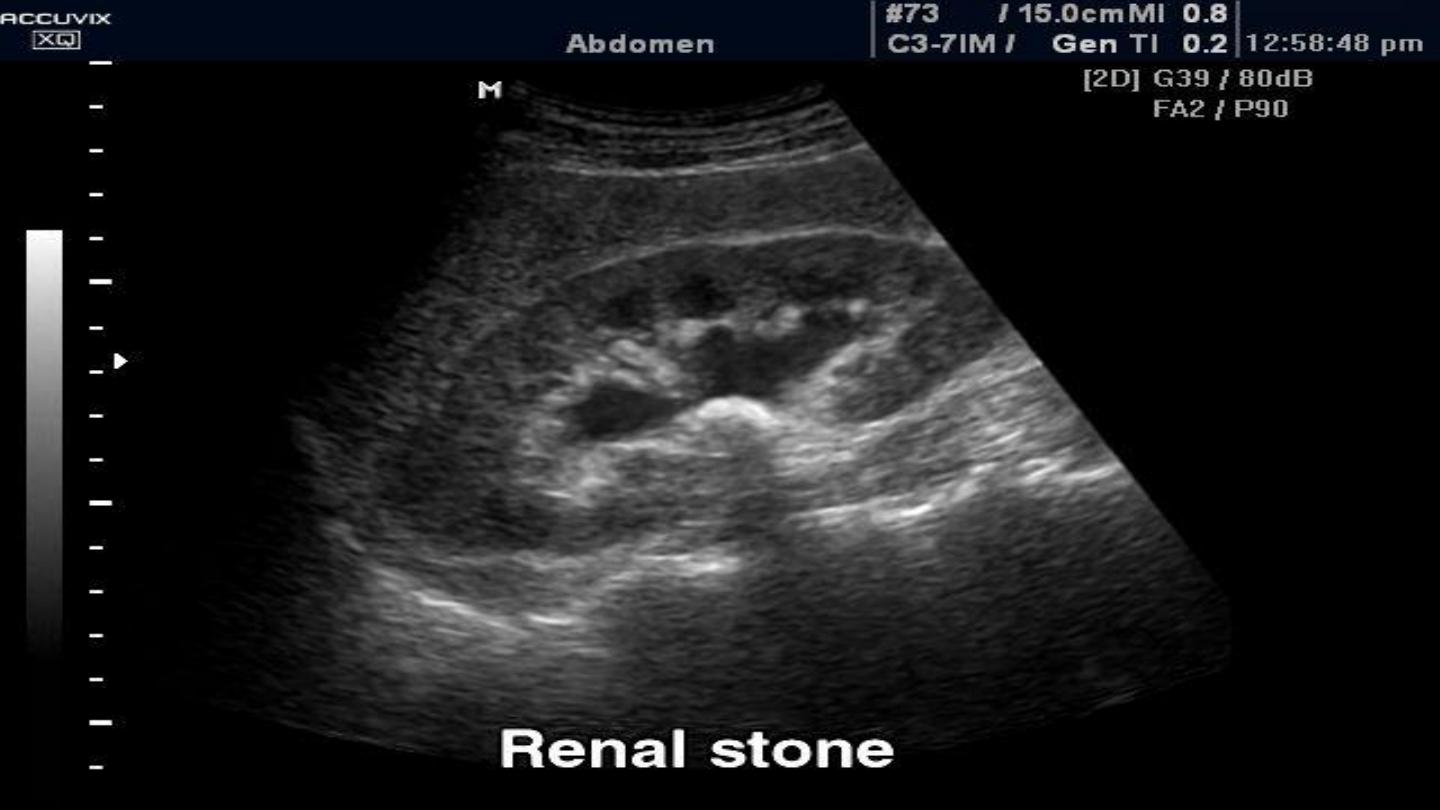
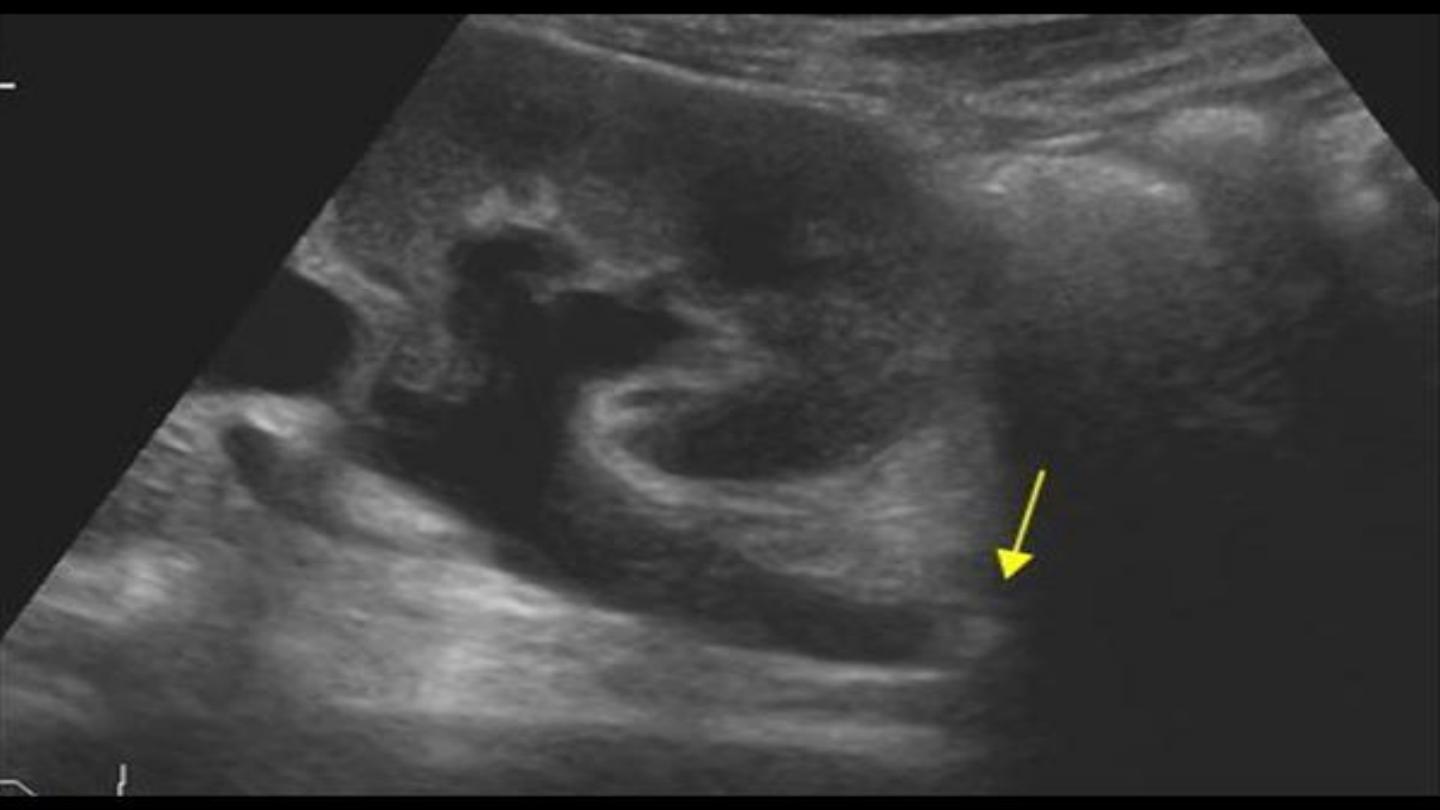
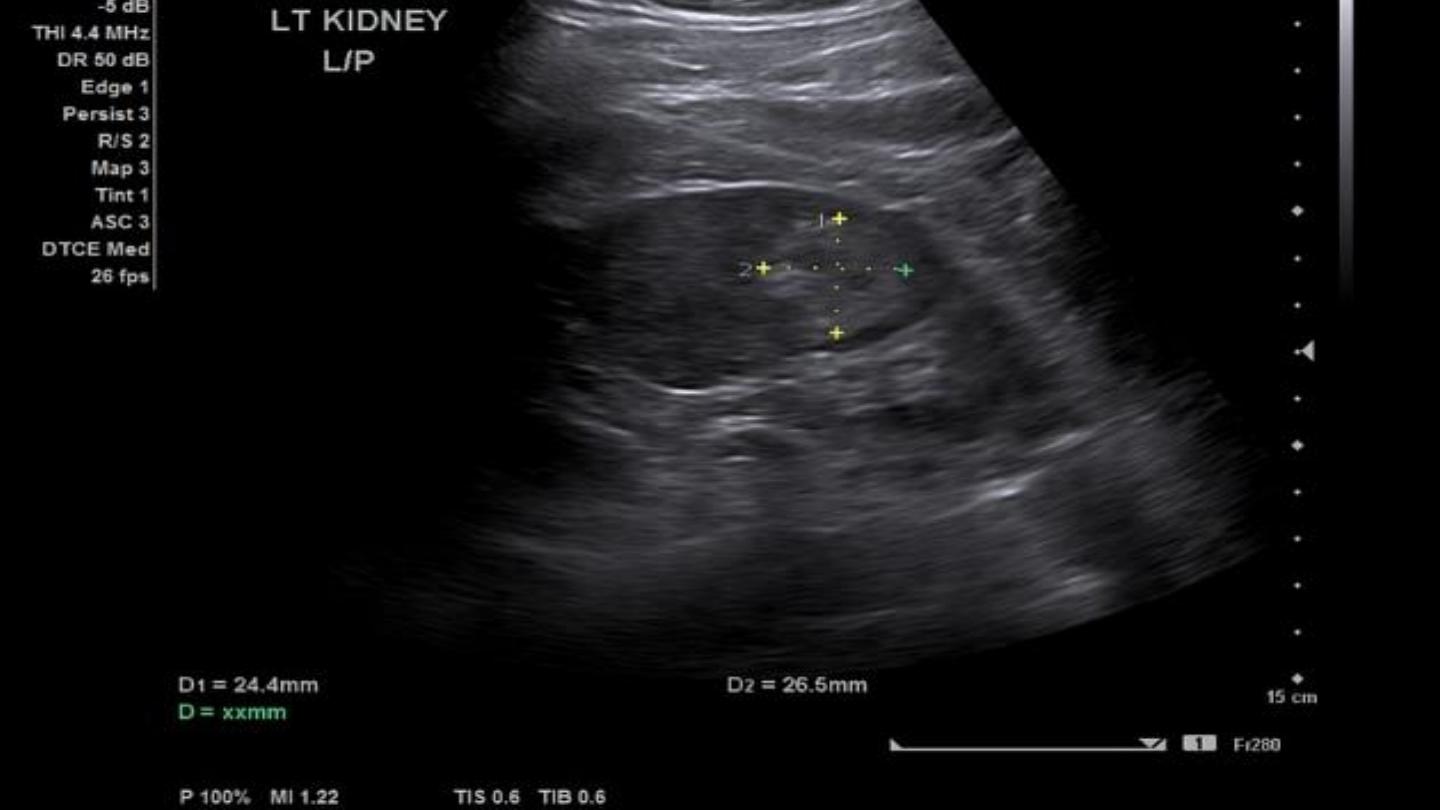
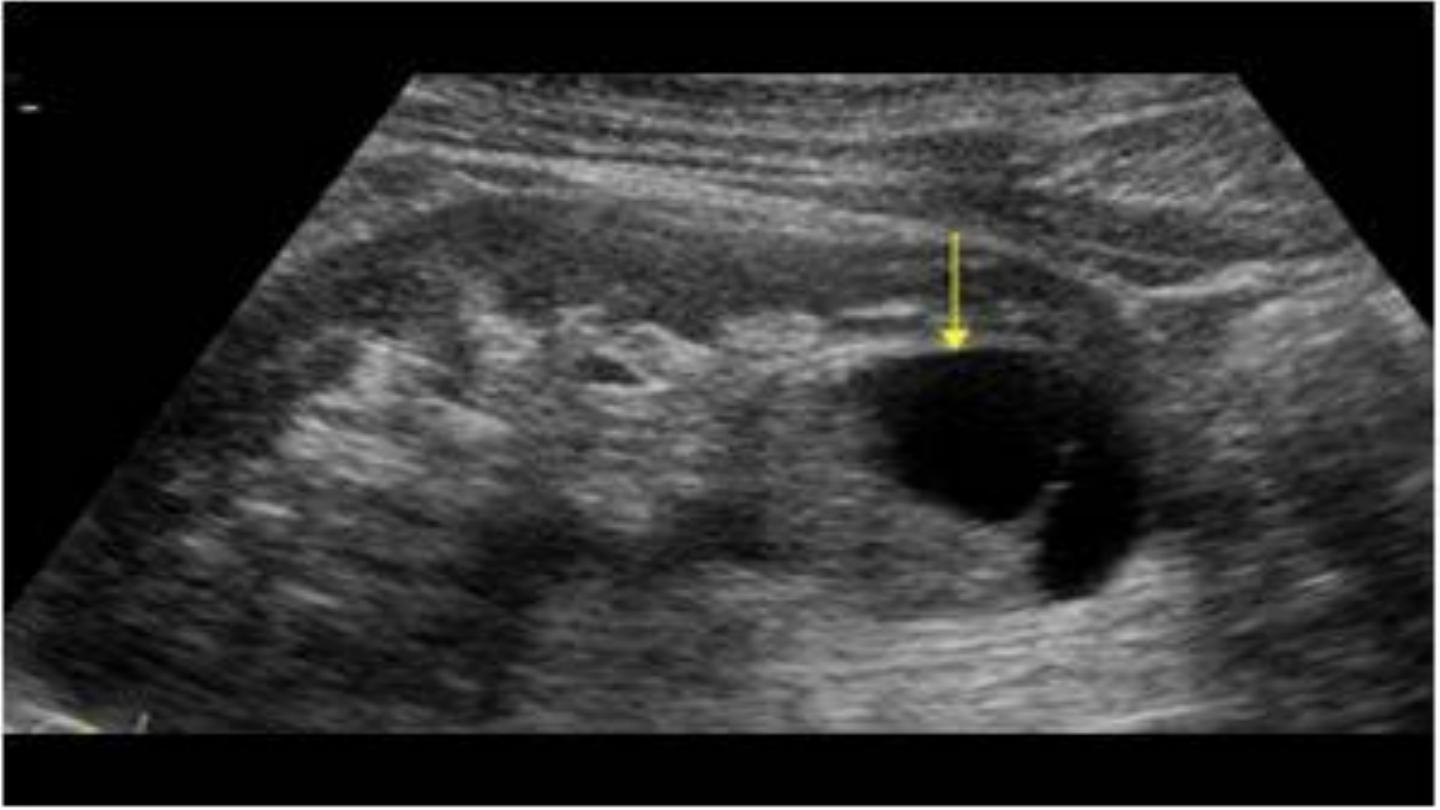
US
An echogenic focus ( acoustic shadowing).
There can be pelvicalyceal or ureteric dilatation
Stones within the pelvicalyceal system can only be reliably identified if they are greater than 5mm in size (as small stones are less likely to cast an
acousticshadow).
Ureteric stones are poorly visualized unless they are located within the proximal ureter or VUJ
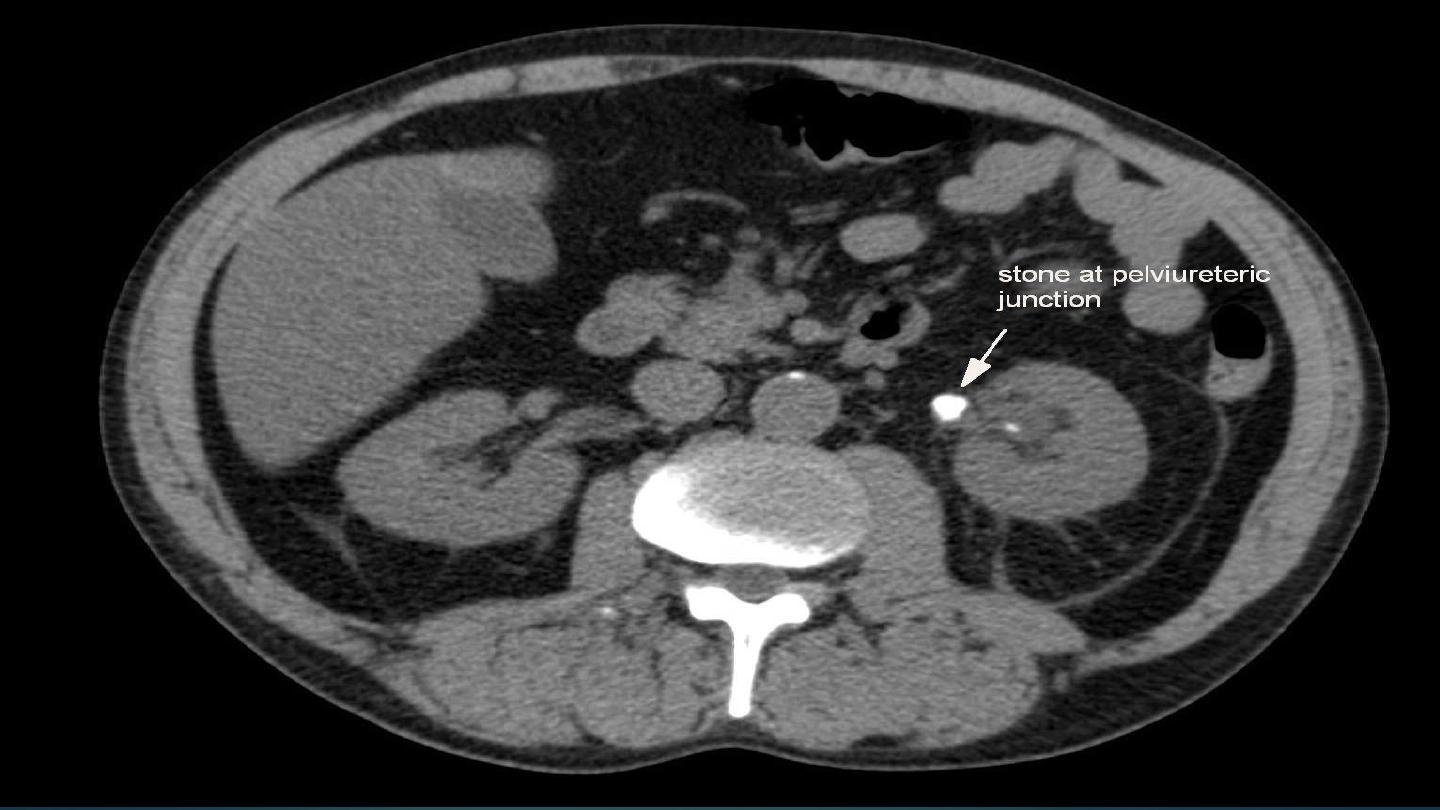
NECT
This is the investigation of choice
It detects greater than 99% of stones (including thosethat are radiolucent on AXR).
Secondary CT signs: ureteric and collecting system dilatation ▶ nephromegaly ▶ perinephric and periureteric stranding.
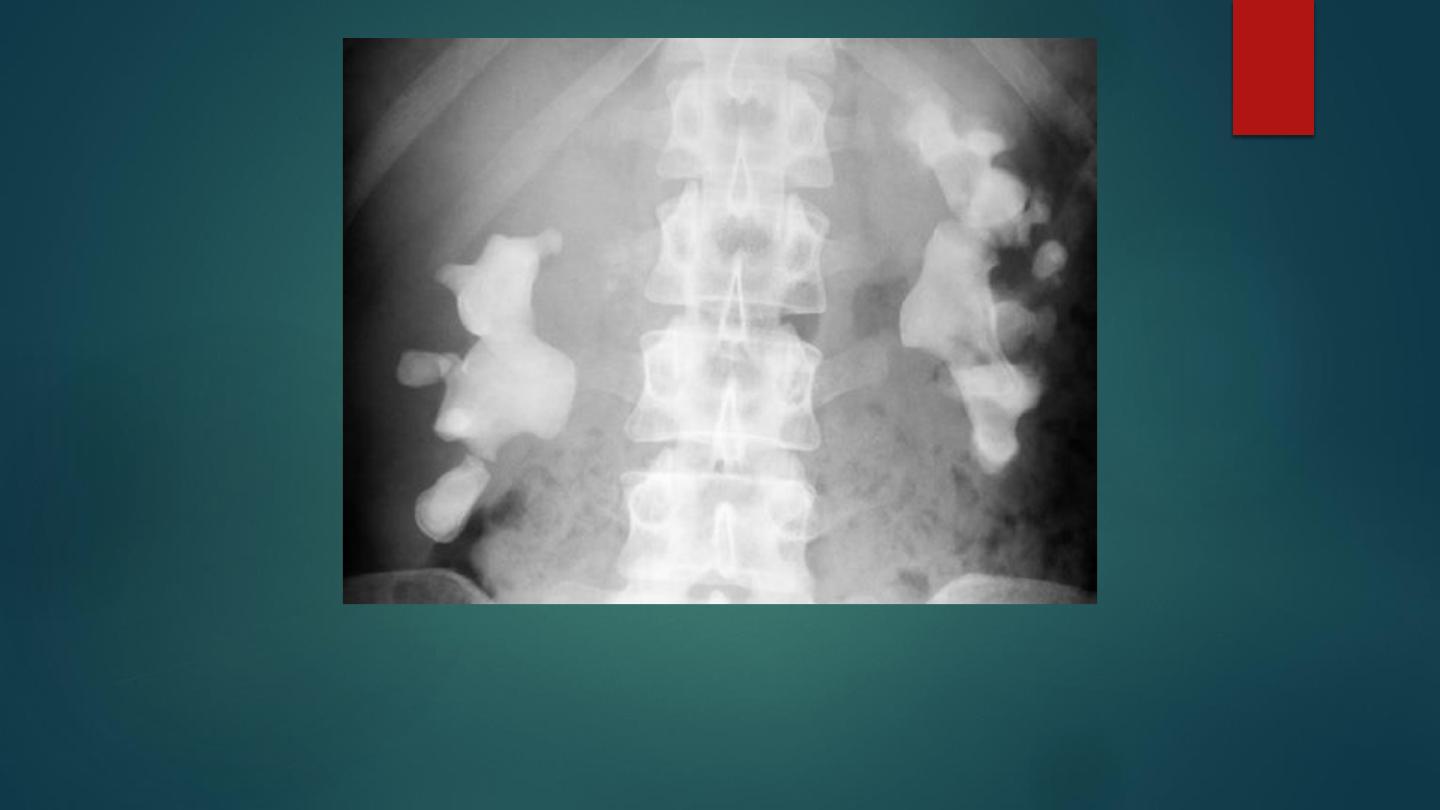
Bilateral staghorn calculi are seen on the control image of an IVU series.

US demonstrating a small solitary renal calculus which is seen as an echogenic
focus with marked posterior acoustic shadowing.

Ureteric stones on CT


RENAL CELL CARCINOMA
• THIS ACCOUNTS FOR 85% OF ALL MALIGNANT RENAL TUMOURS.
• THE CLASSIC CLINICAL TRIAD OF A PALPABLE MASS, FLANK PAIN, HAEMATURIA, AND WEIGHT LOSS.
• IT USUALLY PRESENTS DURING THE 5TH–7TH DECADES (2M:1F)

RADIOLOGICAL FEATURES
X-ray
:
Renal calcification may be visible
IVU:
- Distortion of the pelvicalyceal system.
- A demonstrable mass.
US:
- Small tumours are usually hyperechoic.
- Larger tumours can be isoechoic ( central necrosis).
- Cystic tumours have thick or irregular walls with variably sized intracystic tumour nodules
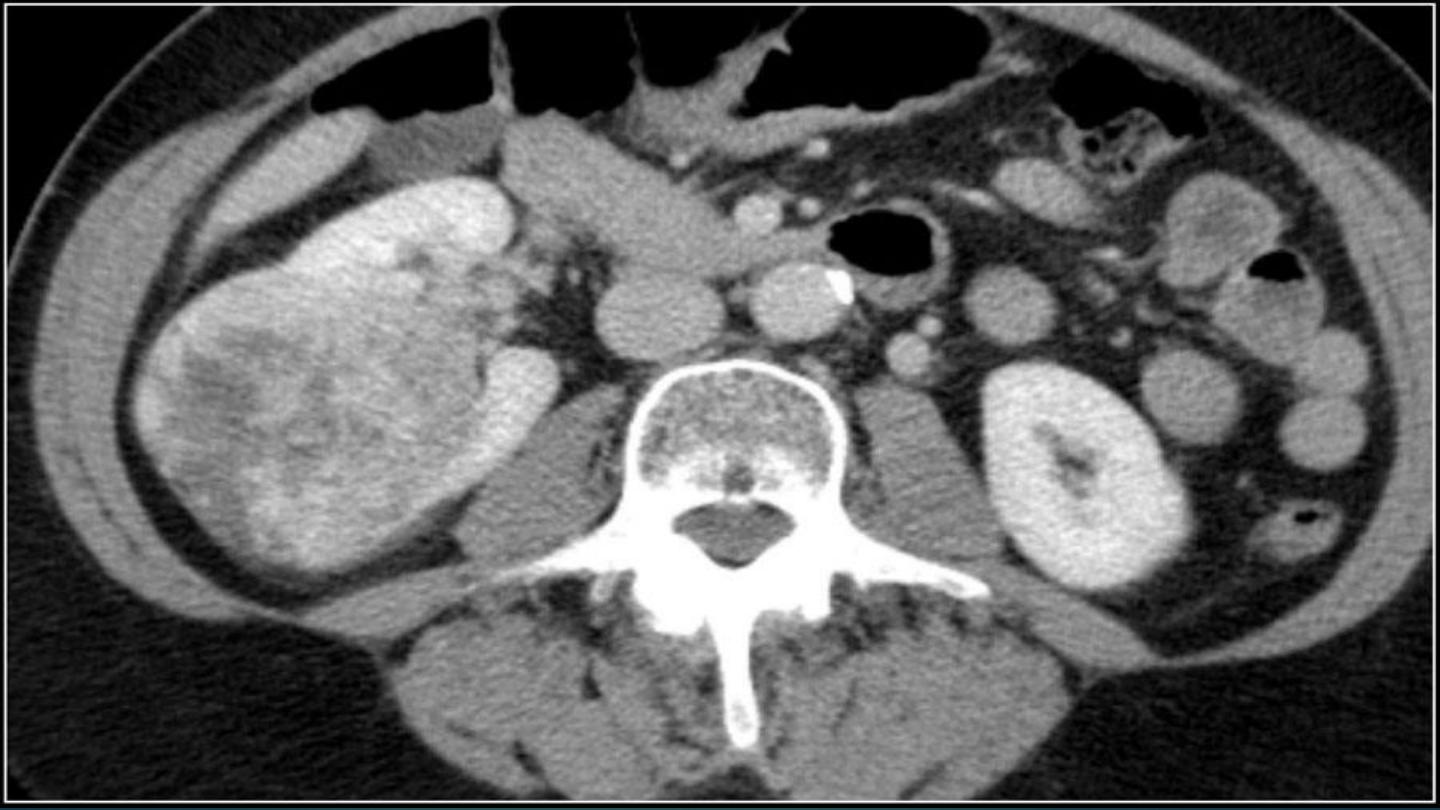
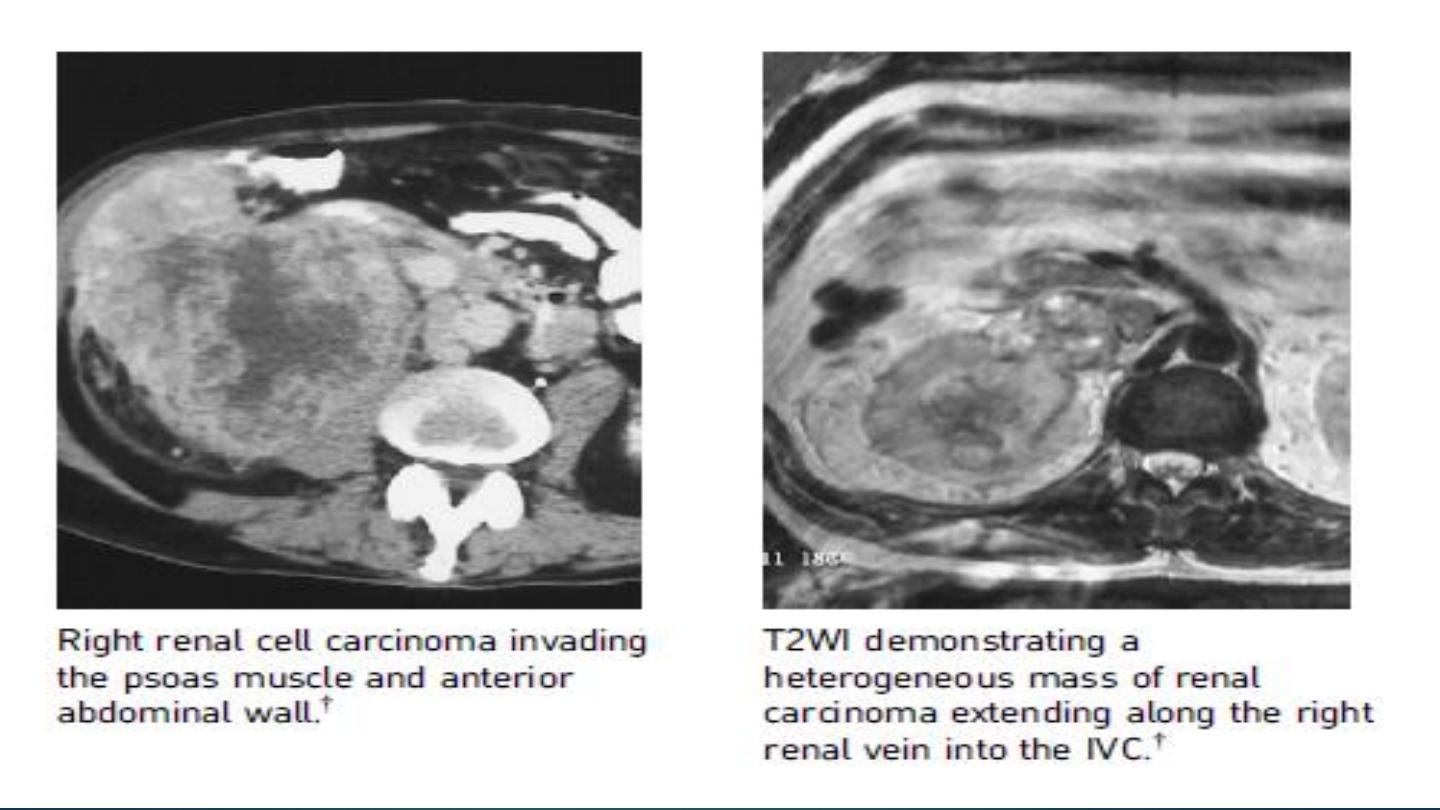
CT:
- The preferred method for staging
- NECT: a solid mass of heterogeneous attenuation (>20HU) with low-density central areas.
- calcif`ication can be present (5–10%)
- CECT: increased attenuation (>10HU) suggests a solid mass ▶ increased attenuation > 20HU is consistent with malignancy.
MRI:
This is used for staging if a CECT is contraindicated or if frequent follow-up is required in high-risk patients
- T1WI: low-to-intermediate SI.
- T2WI: slightly high SI .
- T1WI Gad: immediate heterogeneous enhancement which decreases on delayed images.
- homogeneous enhancement is more likely in small, low-grade tumours.
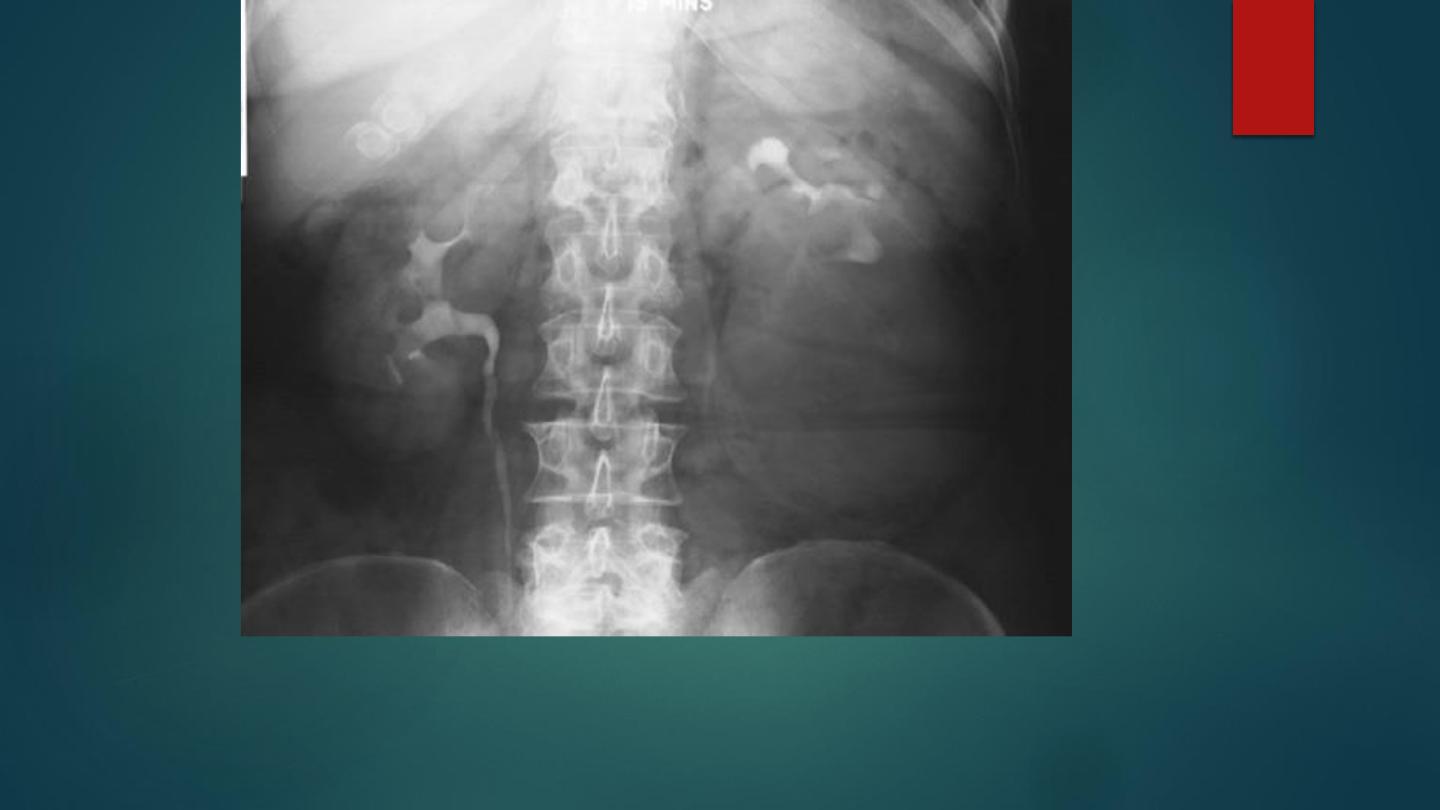
Renal cell carcinoma on IVU appears as a large left lower pole mass distorting the adjacent pelvicalyceal system.
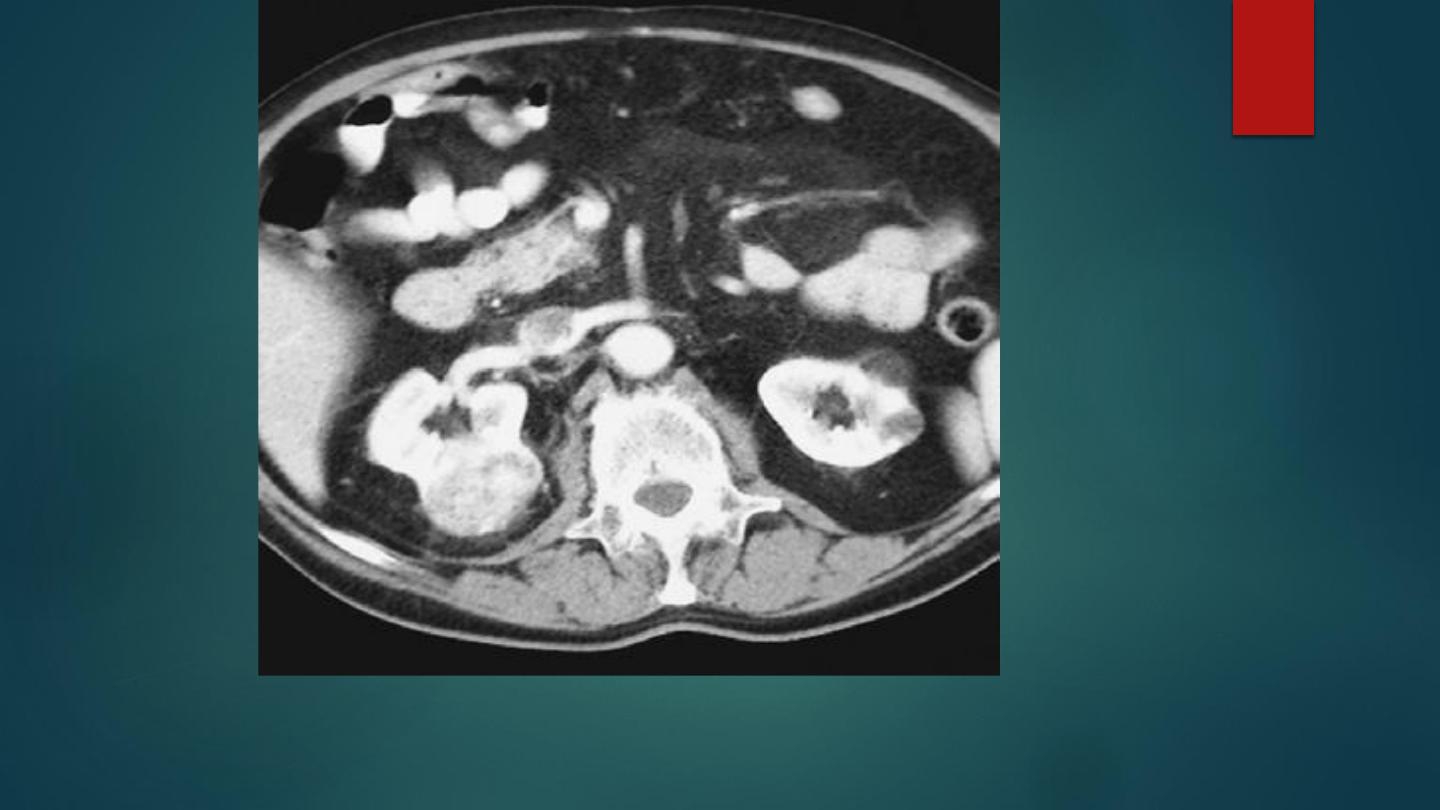
CECT demonstrating a renal cell carcinoma extending to the kidney margin with some local nodular
extension through the capsule


WILMS’TUMOUR(NEPHROBLASTOMA)
DEFINITION
• A renal tumour arising from metanephric blastema cells (the primitive embryonic renal
parenchyma).
CLINICAL PRESENTATION:
• It most commonly presents as an asymptomatic abdominal mass, haematuria, less
commonly pain, fever or hypertension.
• Peak incidence at 3 years (M ¼ F)
• It is the 3rd most common childhood malignancy after leukaemia and brain tumours.
•

RADIOLOGICAL FEATURES:
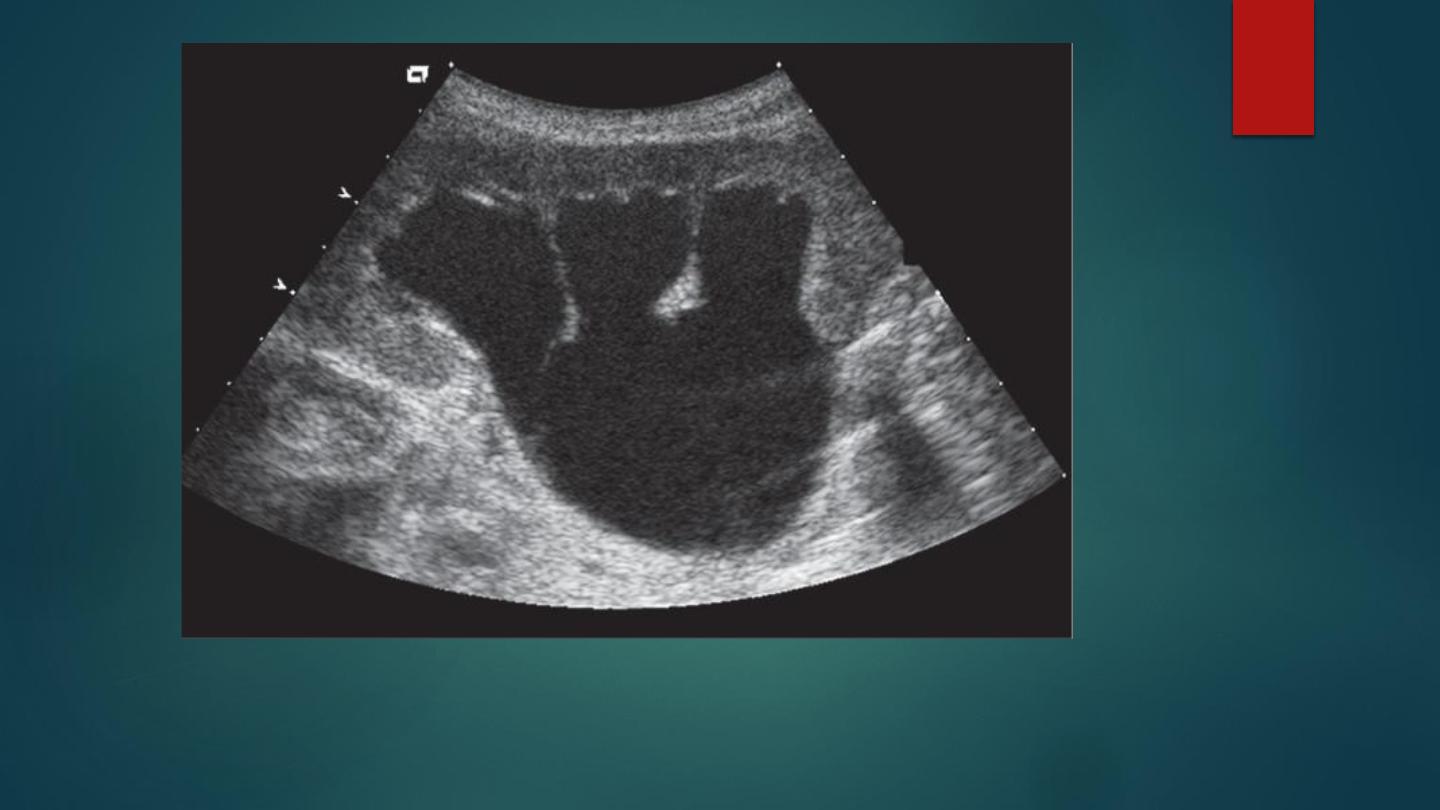
Ultrasound:
-
A solid hyperechoic mass ( cystic areas).
CT:
-
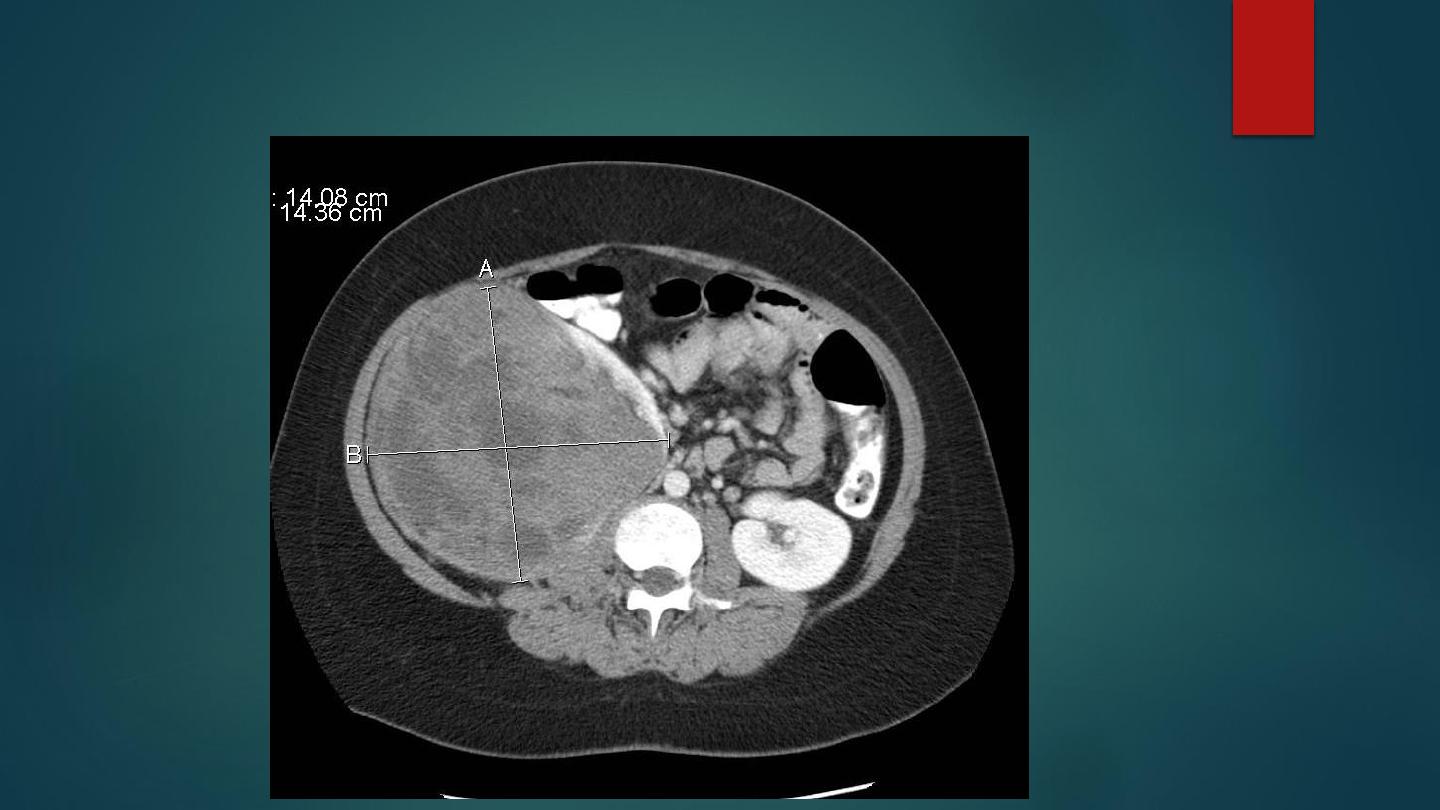
Typically a large heterogeneously enhancing renal mass (enhancing less than normal kidney).
-
‘Claw’ sign: normal renal tissue is typically stretched at the periphery of the lesion.
-
Tumour spread: typically by direct extension with displacement of any adjacent structures.
-
Vascular invasion: this is seen in 5–10% (involving the renal vein, IVC and right atrium) ▶ it can
also invade the renal pelvis and ureter
MRI:
-
T1WI: low SI.
-
T2WI: high SI.
-
T1WI, Gad: heterogeneous enhancement.
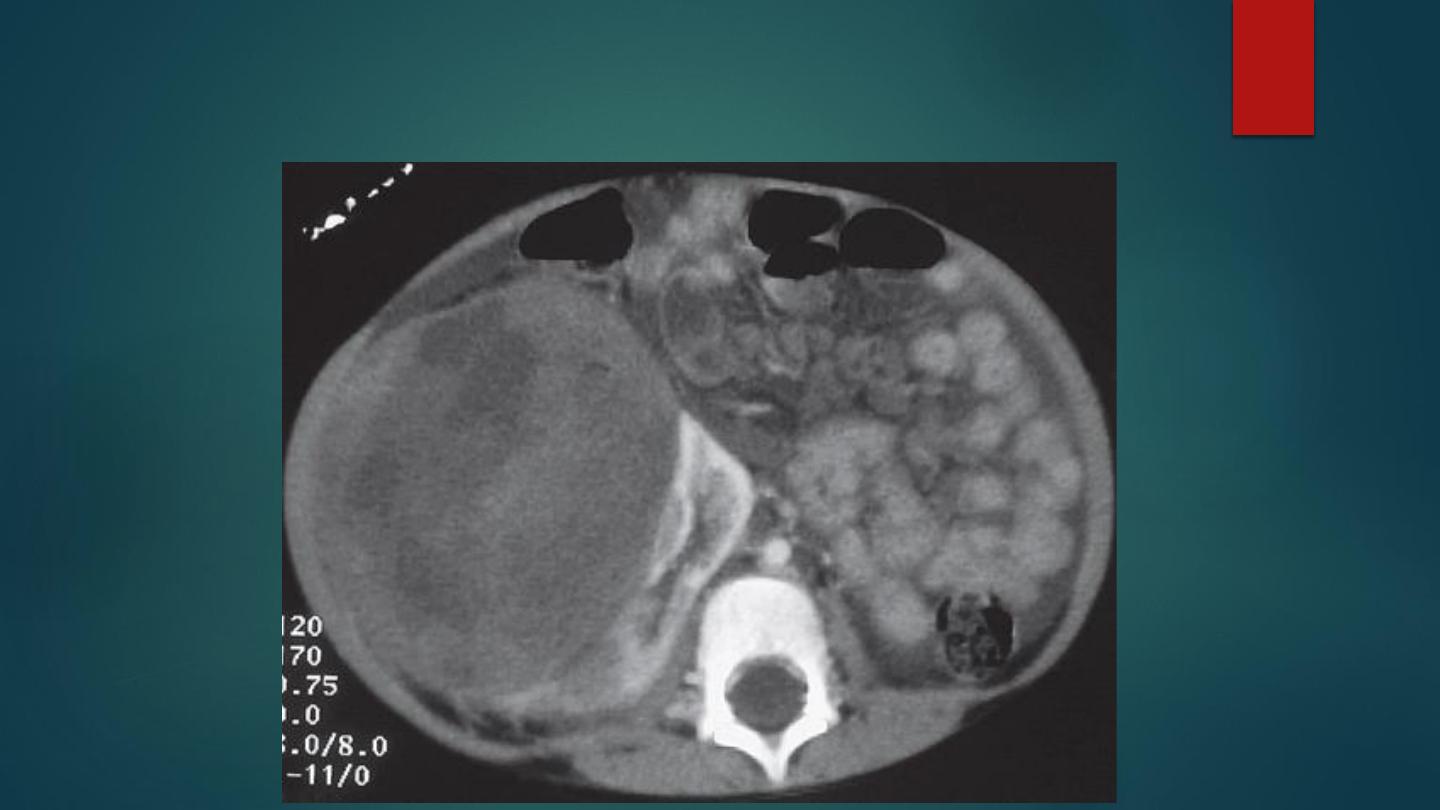
Wilms’ tumour. (A) Axial CECT of the abdomen showing a large mass arising from the right
kidney which is of heterogeneous attenuation. The mass is seen to displace the normal
enhancing renal parenchyma to the left.
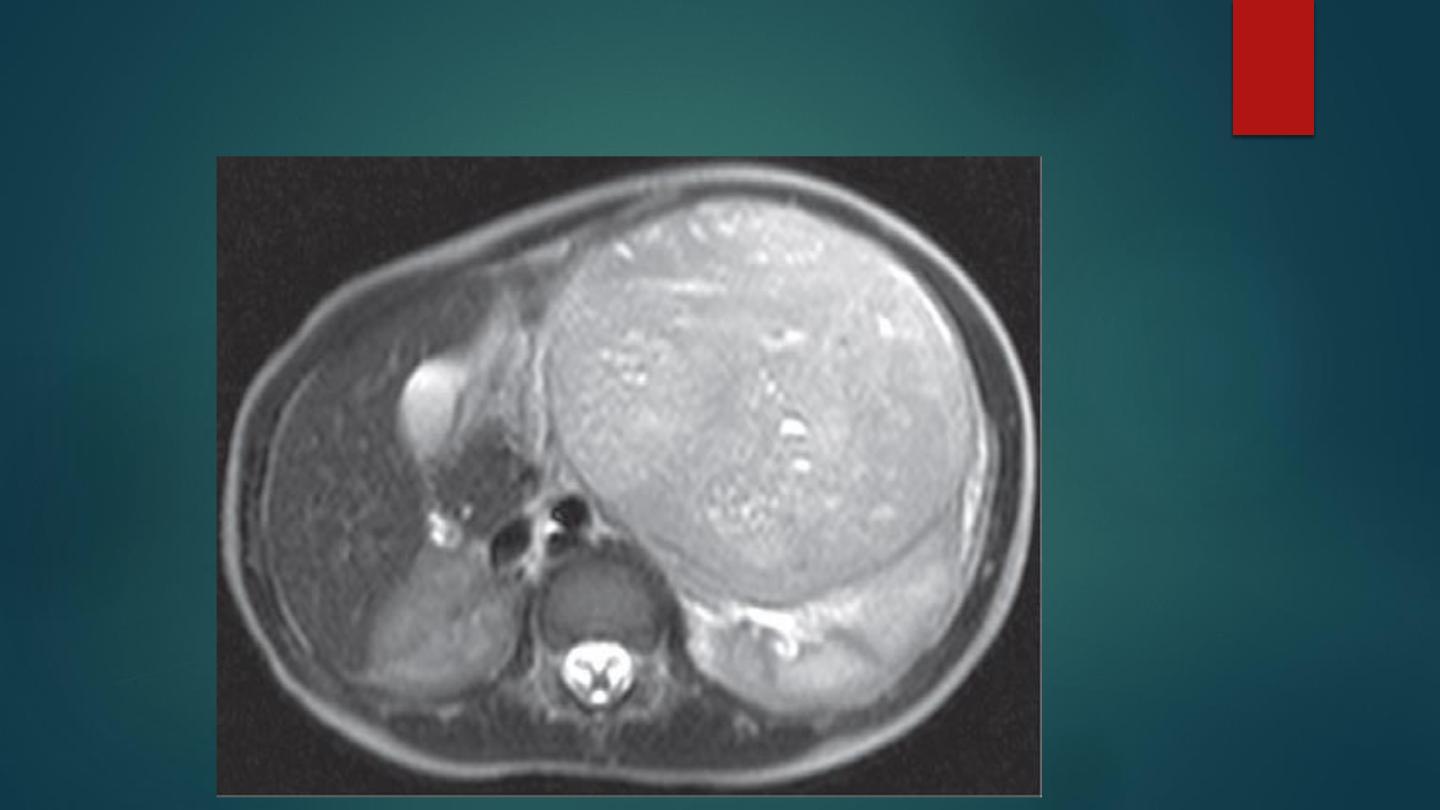
Wilms’ tumour MRI Axial T2WI
Contrast enhanced CT of abdomen

) outlined by red line with
seen in association with
a displaced right kidney (yellow arrow) confirming the renal origin of the mass.

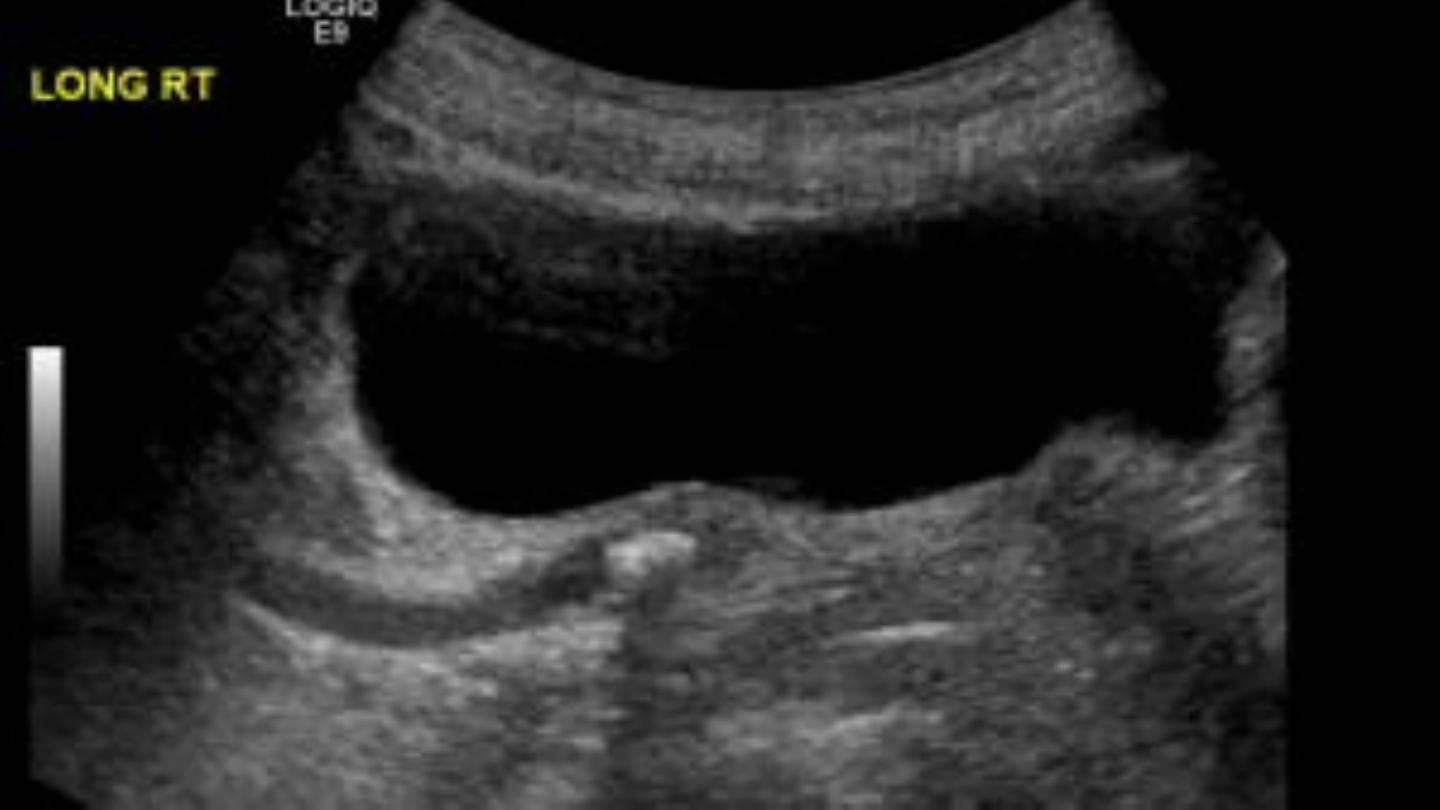
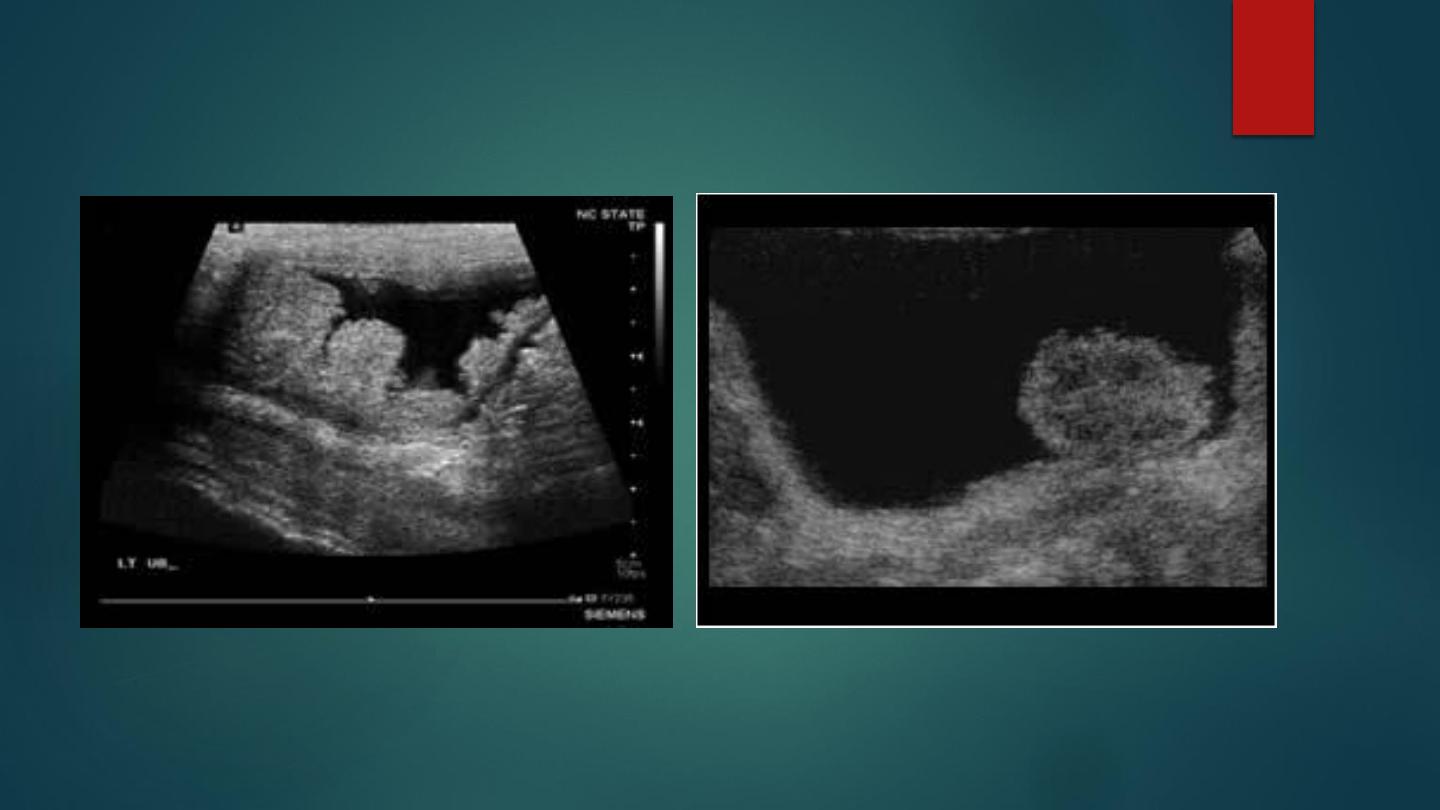
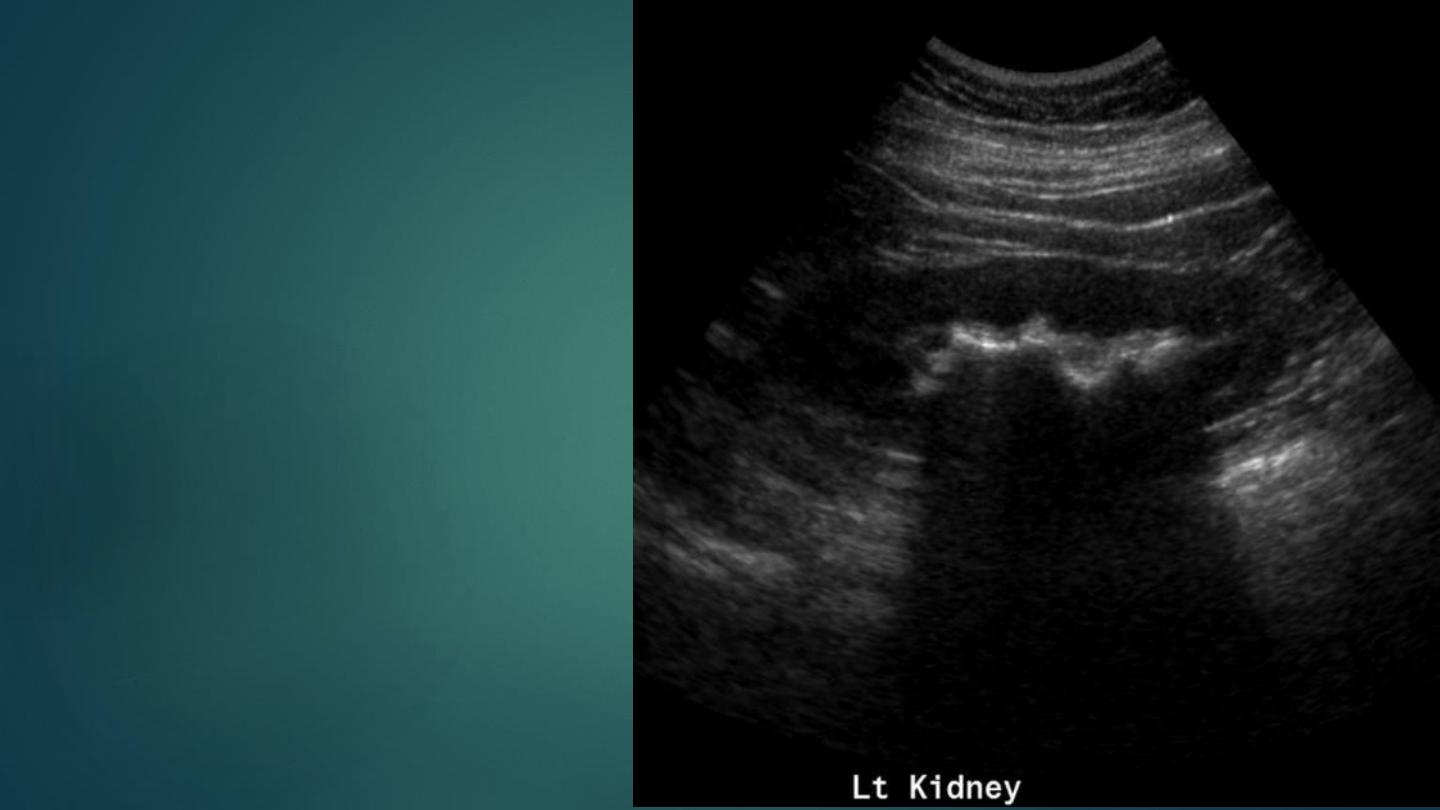
METHODS OF IMAGING IN OBSTRUCTION
RADIOLOGICAL FEATURES
US
- This is an excellent method of detecting obstruction – however is
does not provide functional information and it can be difficult to
distinguish a prominent extra renal pelvis from mild hydronephrosis.
- False negative results may arise if there is a large staghorn calculus
- Dilatation of the pelvicalyceal system is a poor indicator of the
severity of obstruction (the absence of dilatation does not exclude
obstruction)
§ Grade I: minimal calyceal dilatation
§ Grade II: mild hydronephrosis
§ Grade III: moderate hydronephrosis
§ Grade IV: severe hydronephrosis

IVU
- Obstructive nephrogram: an increasingly dense nephrogram (lasting up to 24 h with a peak
density at 6 h) ▶ this is seen with acute obstruction and only in kidneys with normal renal
blood flow, GFR and tubular function (i.e. not with pre-existing parenchymal disease)
- Delayed contrast excretion: the delay in contrast excretion depends on the degree of
obstruction.
- Ureteric or pelvicalyceal dilatation: this may be minimal during the first few days
-
Urinoma: a persistent encapsulated collection of urine
CT
NECT: hydronephrosis and hydroureter to the level of the obstruction
CECT:
Acute obstruction:
There is prolongation of the usually transient, early corticomedullary nephrogram.
Chronic obstruction:
-
hydronephrosis.
-
Parenchymal thinning ( a shell or rim nephrogram)
Ultrasound of the kidneys showing hydronephrosis and cortical
atrophy.

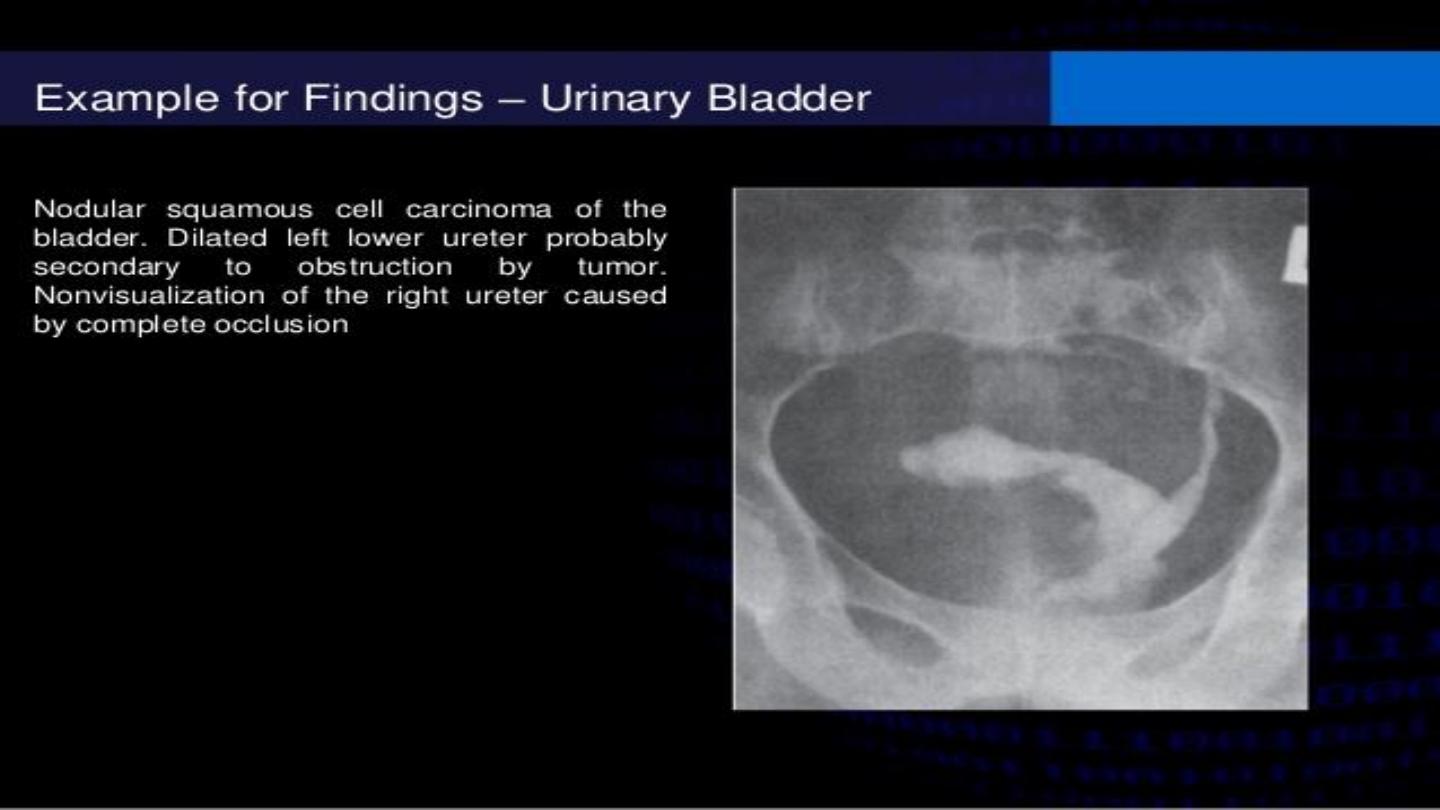
BLADDER TUMOURS
Transitional cell carcinoma (TCC): 90% of all epithelial tumours.
Squamous cell carcinoma (SCC): 1.5–10% of all epithelial tumours.
Adenocarcinoma: 1% of all epithelial tumours.
CLINICAL PRESENTATION
-
Haematuria.
-
Dysuria.
-
pelvic pain (due to side wall invasion)

RADIOLOGICAL FEATURES
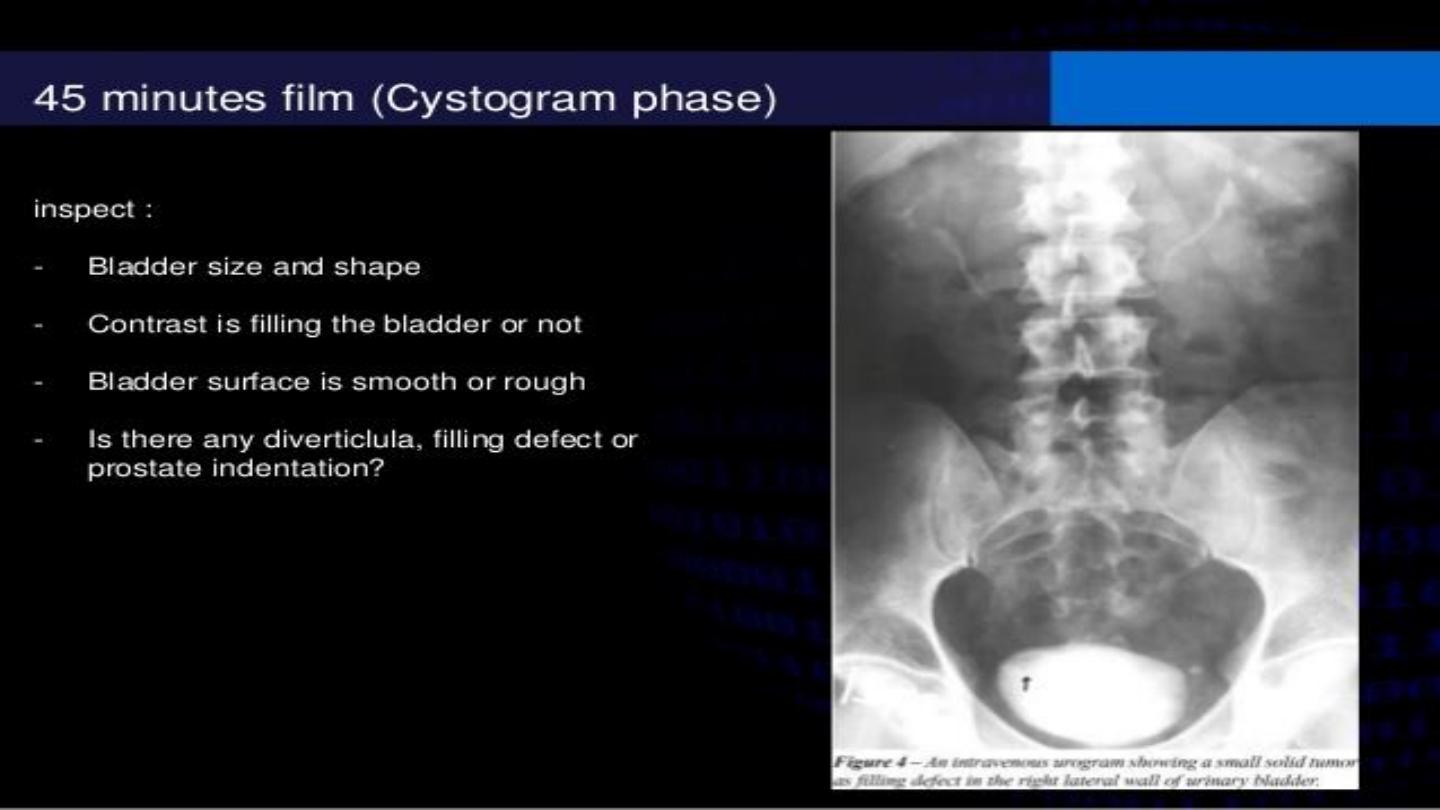
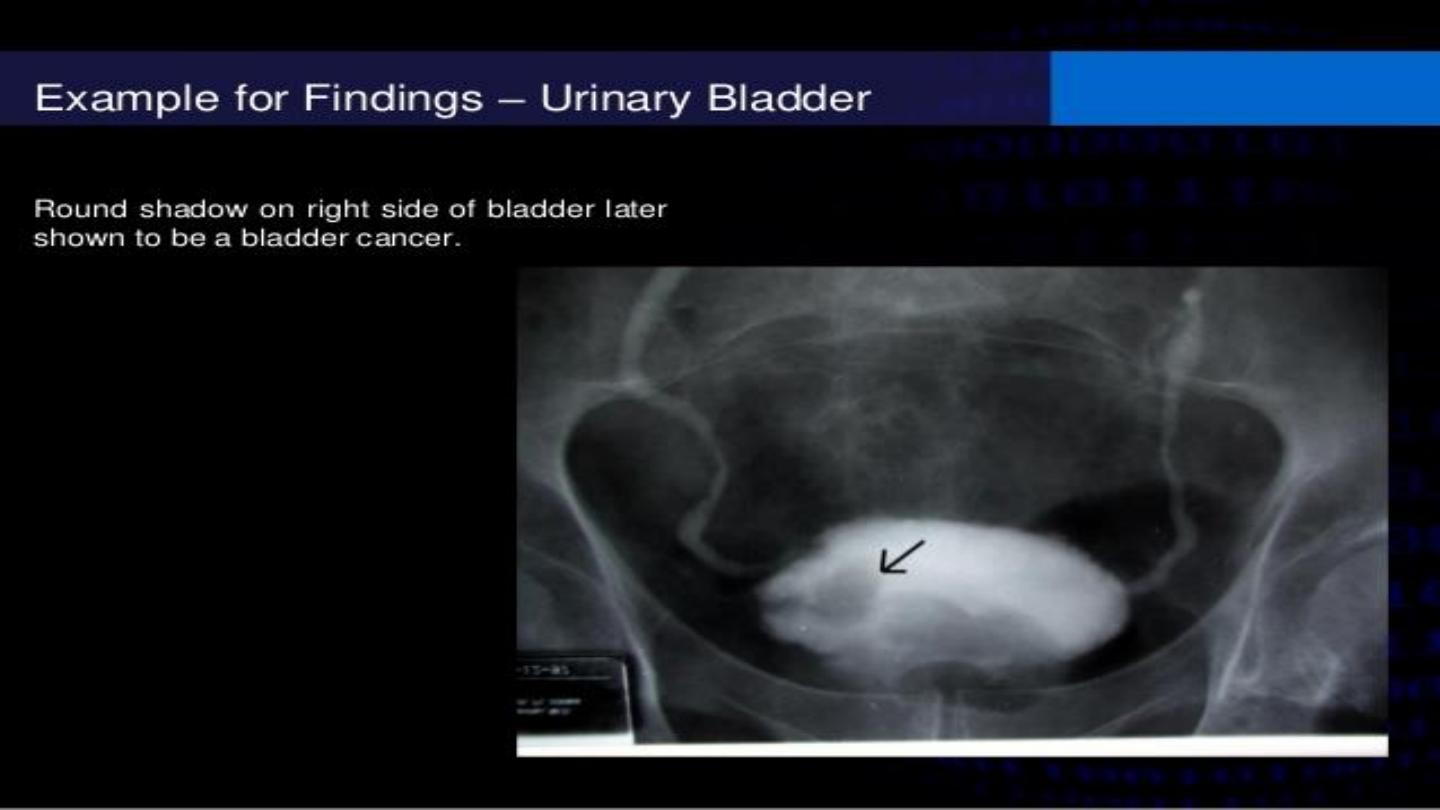
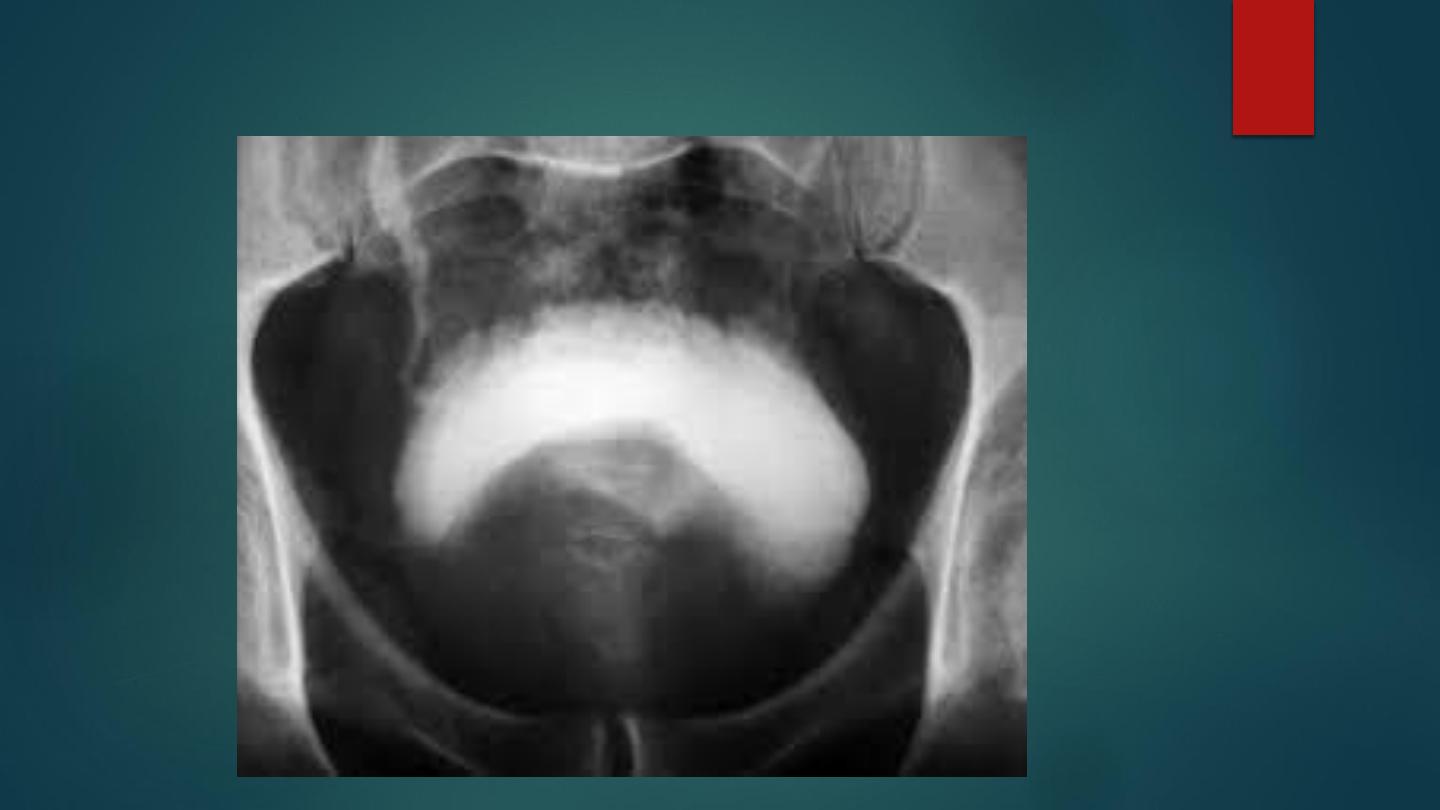
IVU/cystogram:
A lobulated filling defect within the bladder ( it may miss infiltrative
tumour types).
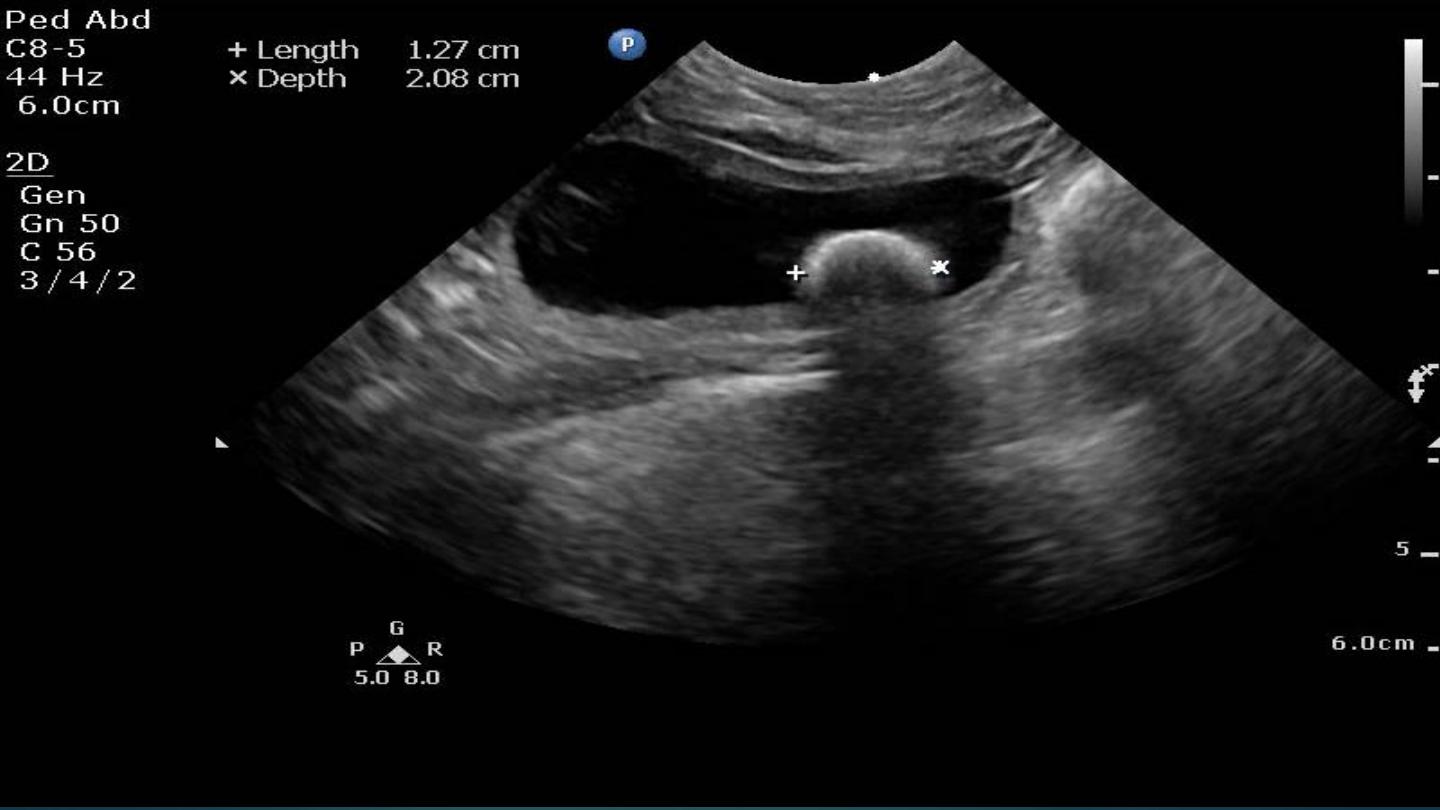
US:
A sessile or pedunculated mixed echogenicity mass projecting into
the bladder lumen ( vascularity)

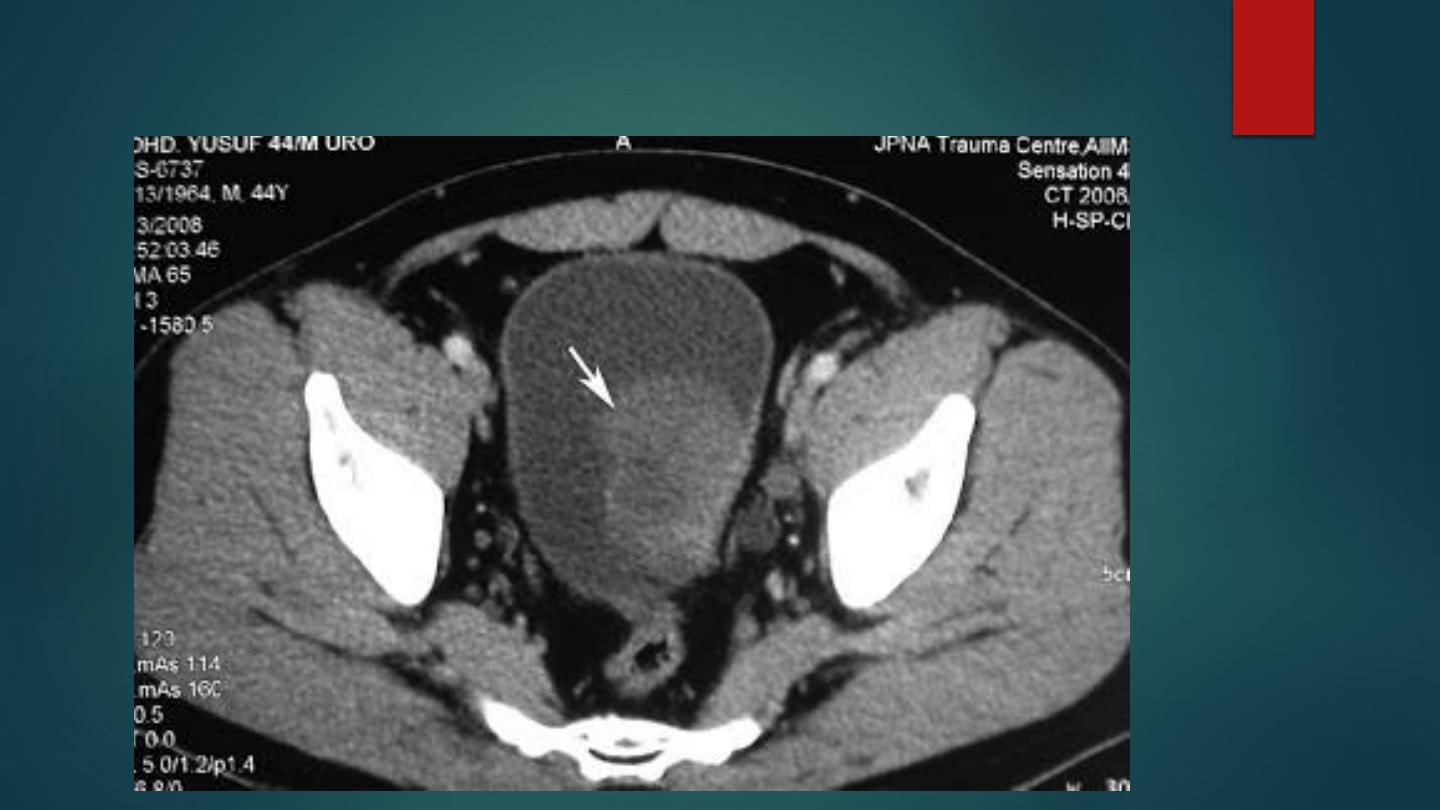
CT:
-
A SESSILE OR PEDUNCULATED SOFT TISSUE MASS PROJECTINGINTO THE
BLADDER LUMEN ( OVERLYING CALCIFICATION
-
LOCALIZED BLADDER WALL THICKENING
- PERIVESICAL FAT INVASION WITH INCREASED PERIVESICAL FAT DENSITY
-
ADJACENT VISCERAL INVASION (RECTUM, UTERUS, PROSTATE OR
VAGINA).
MRI:
- T1WI: SIMILAR SI TO NORMAL WALL ▶ HIGHER SI TO URINE
- T2WI: HIGHER SI TO NORMAL WALL ▶ LOWER SI TO URINE
- T1WI GAD: A HIGHER SI RELATIVE TO NORMAL BLADDER WALL (WITH
SIMILAR ENHANCEMENT CHARACTERISTICS WITH CT)

Noncontrast CT image through the pelvis shows a polypoid lesion
(arrow) arising from the left posterior wall of the bladder
TCC by Ultrasound
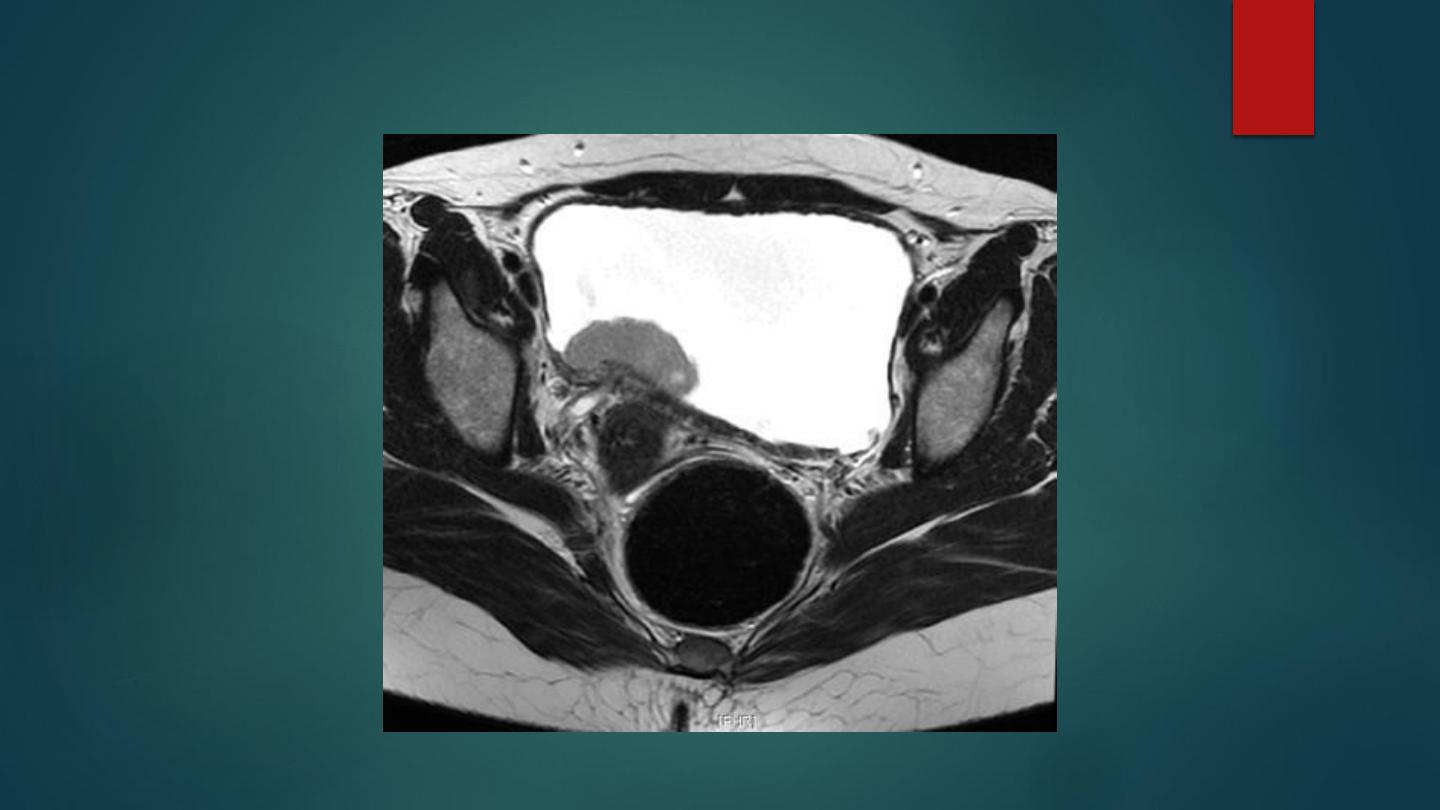
T2WI MRI for posterior wall TCC of Bladder
Anteroposterior view from an IVU demonstrates a filling defect within a right base of
a contrast-filled bladder. Cystoscopic evaluation and eventual biopsy confirmed
the diagnosis of TCC.

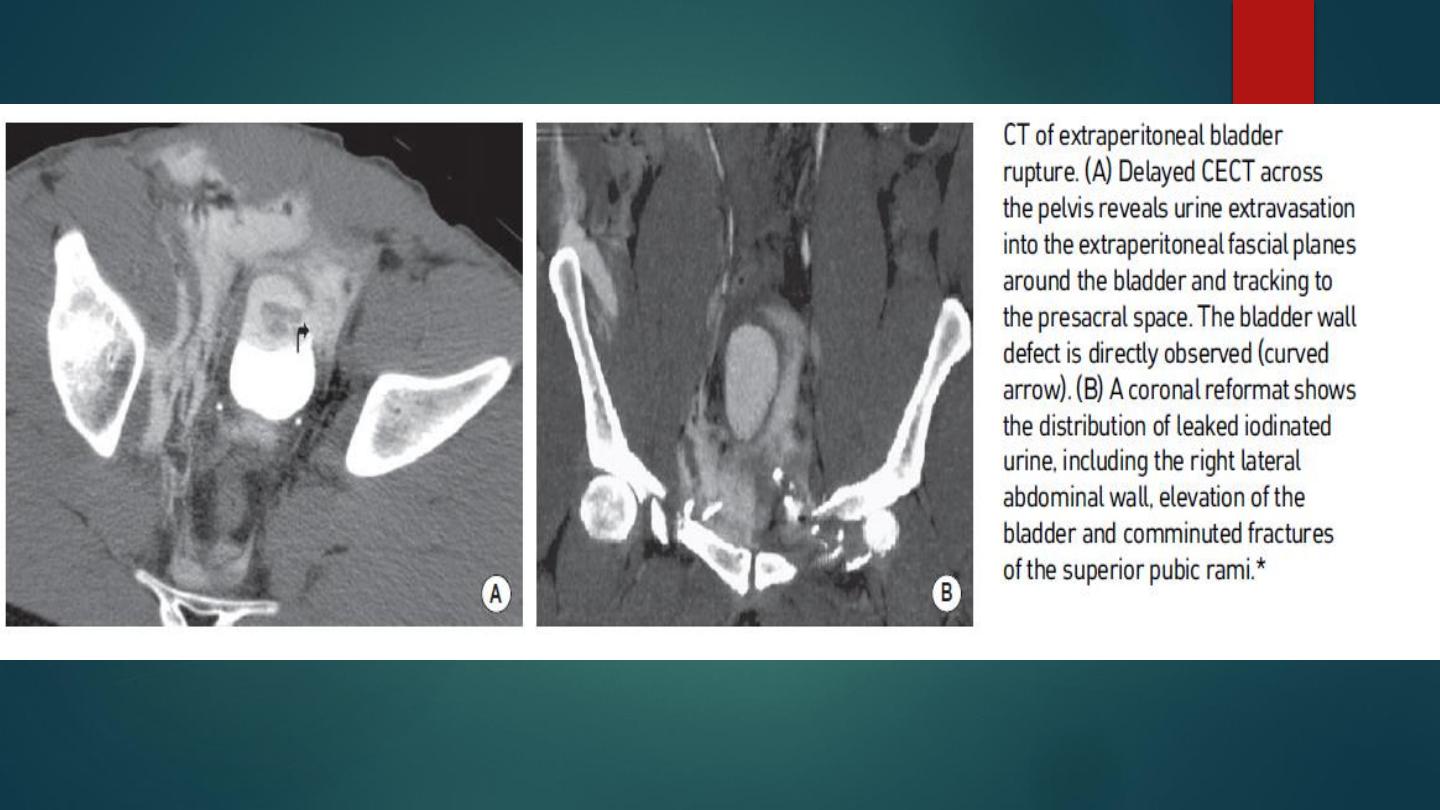
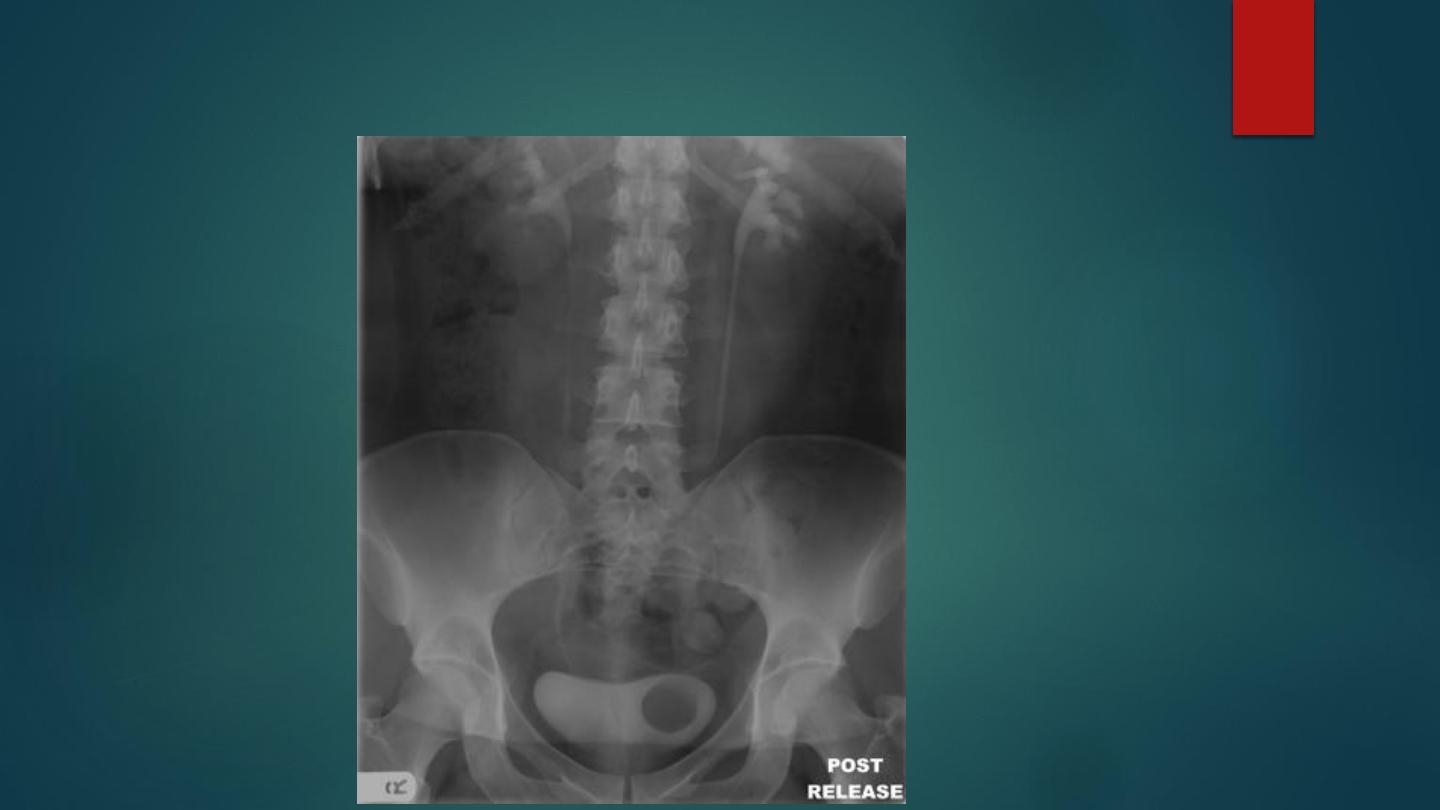
BLADDER INJURY
Trauma to the bladder can be due to:
Blunt abdominal trauma: the most common cause (90% follow a motor vehicle
accident).
External penetrating agents: stab wounds or bone fragments.
Internal penetrating agents: cystoscopes.
Classification of traumatic bladder injuries:
-
Bladder contusion.
-
Intramural (partial-thickness) laceration.
-
Full-thickness laceration with intra- or extraperitoneal rupture
Clinical presentation:
-
Gross haematuria, suprapubic pain and Inability to void.

-
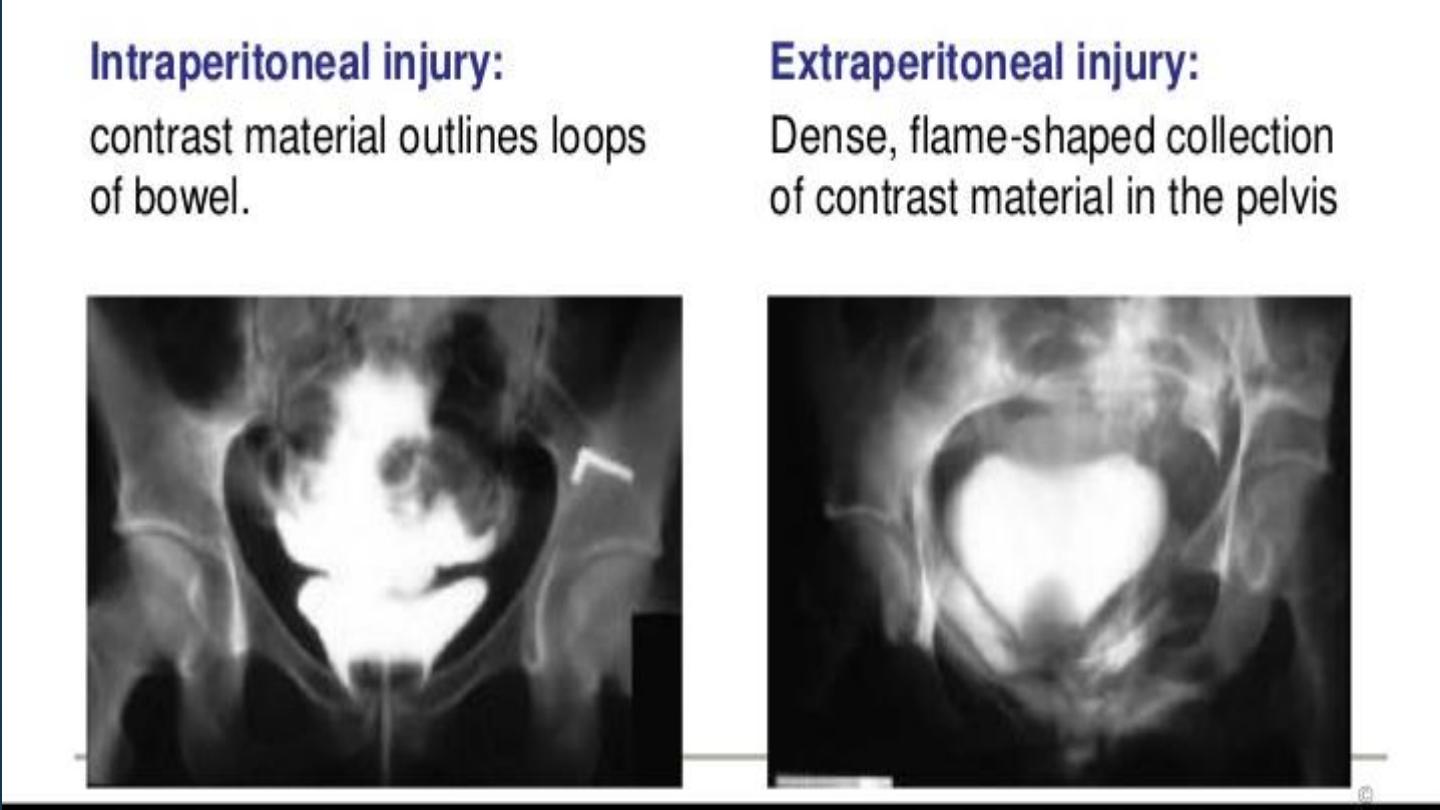
CT cystography This is more accurate than standard cystography for the
detection of bladder injuries
- Intraperitoneal bladder rupture: free intraperitoneal contrast medium is
seen outlining the peritoneal recesses and bowel loops
- Extraperitoneal bladder rupture: contrast extravasates into the surrounding
extraperitoneal space, often spreading in an irregular and often streaky
manner along the fascial planes (with a‘flame-shaped’ appearance)
Urine can dissect into the following:
- The anterior prevesical space.
-
The anterior abdominal wall.
-
The inguinal region and upper thigh.
-
The lateral paravesical and presacral spaces.
-
The perineum, scrotum, and rarely the retoperitoneum

Conventional cystogram demonstrating an intraperitoneal bladder rupture.

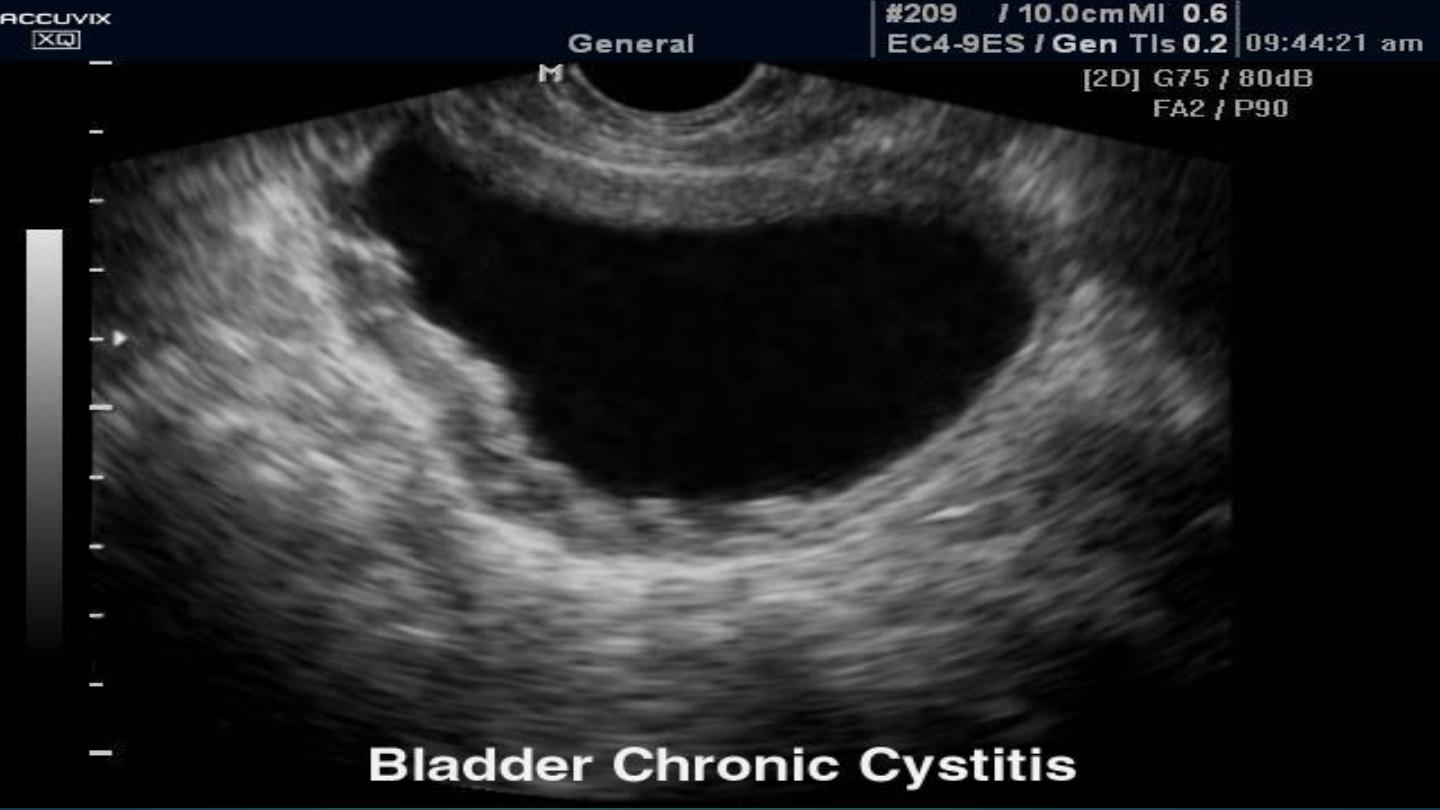
Chronic cystitis
This follows repeated bacterial infections (Usually with E. coli)
Predisposing factors: Reflux, bladder outlet obstruction, bladder diverticulae.
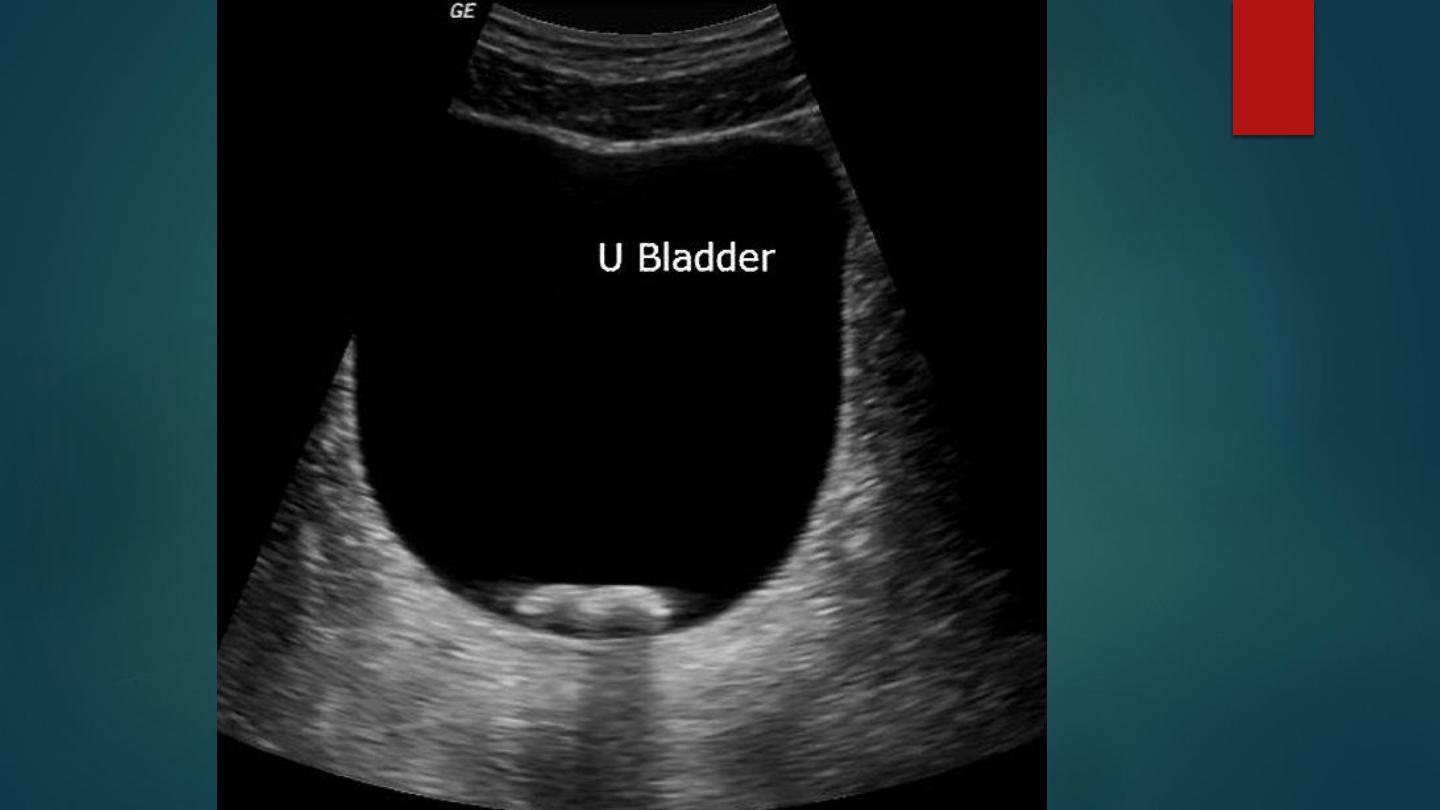
Diffuse bladder wall thickening by Ultrasound
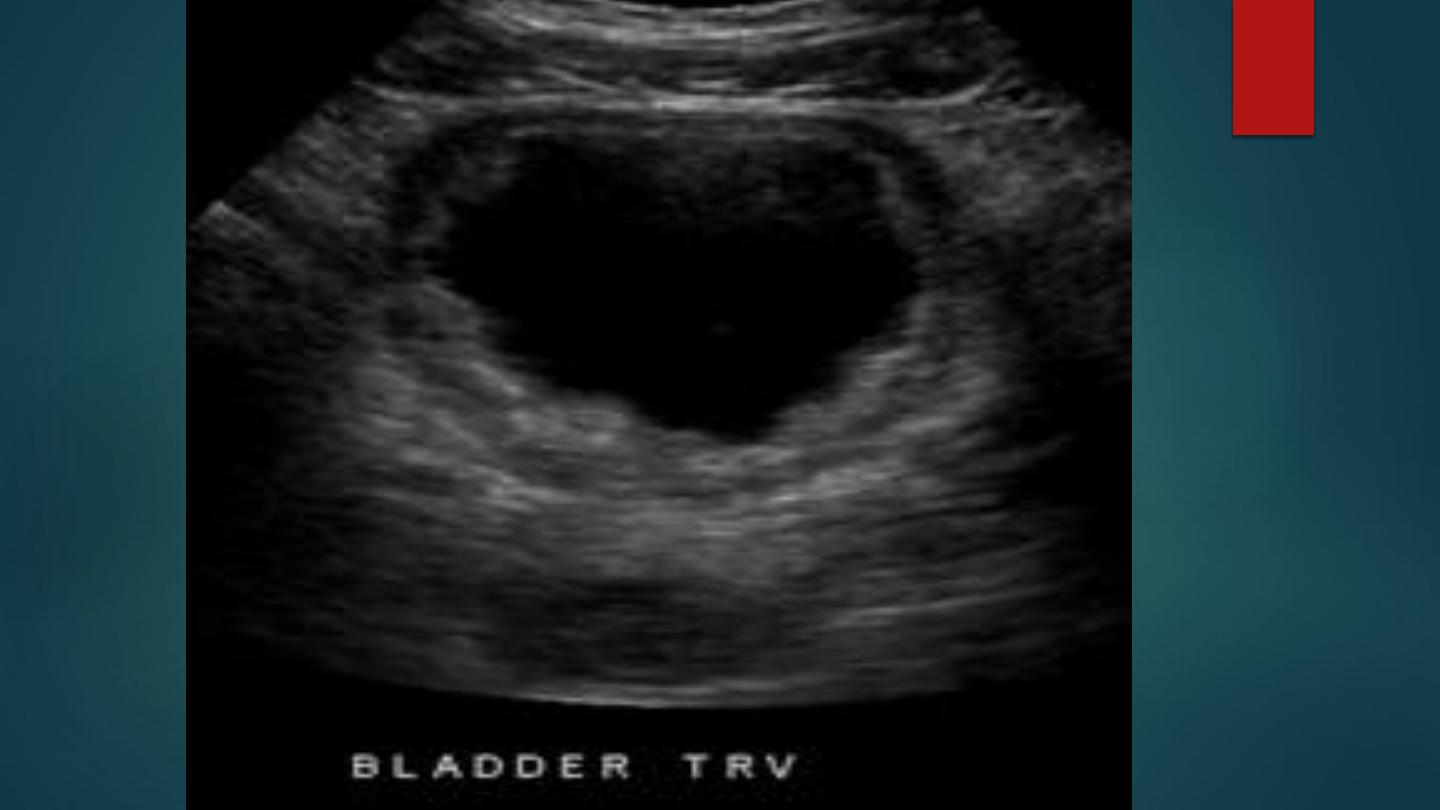
Normal Bladder wall thickening

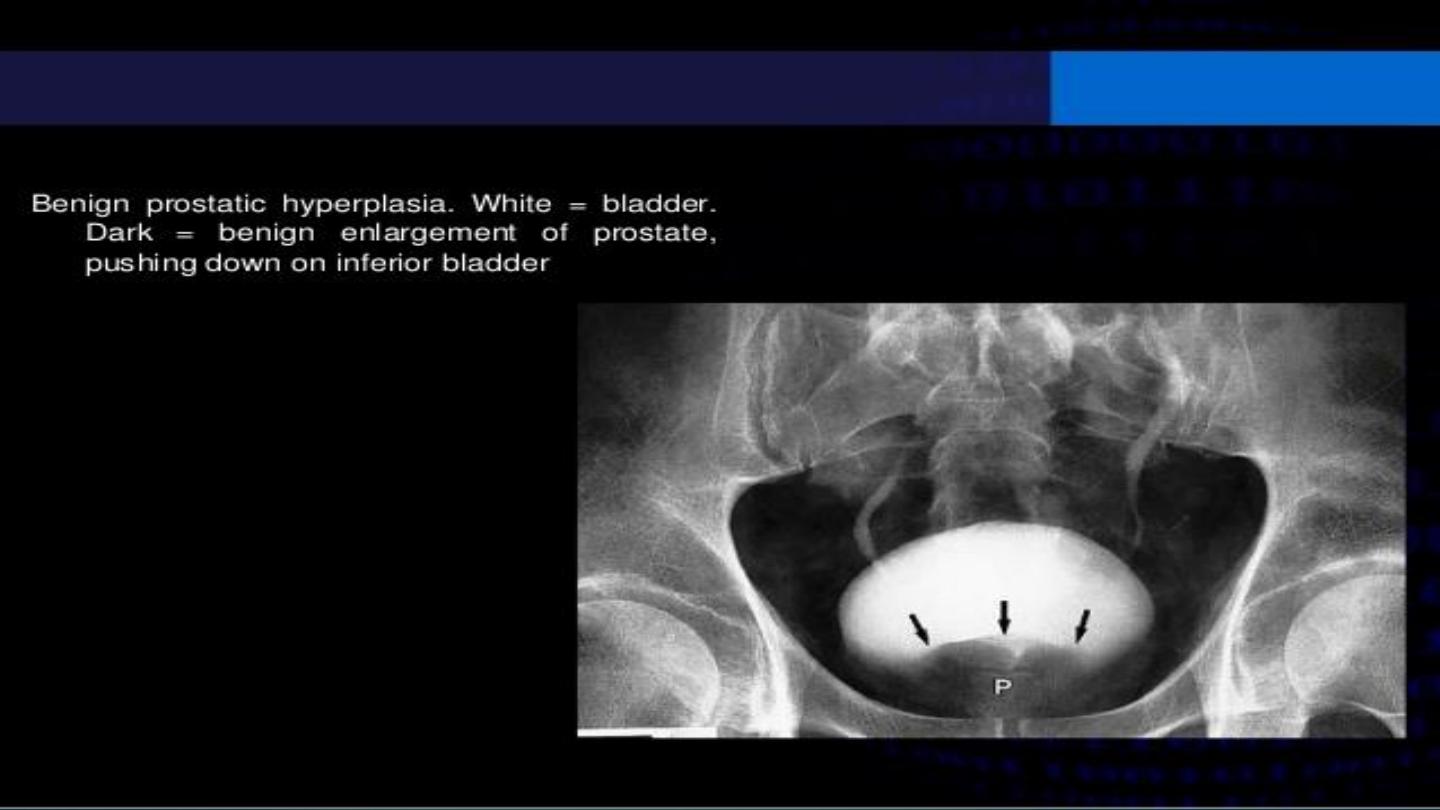
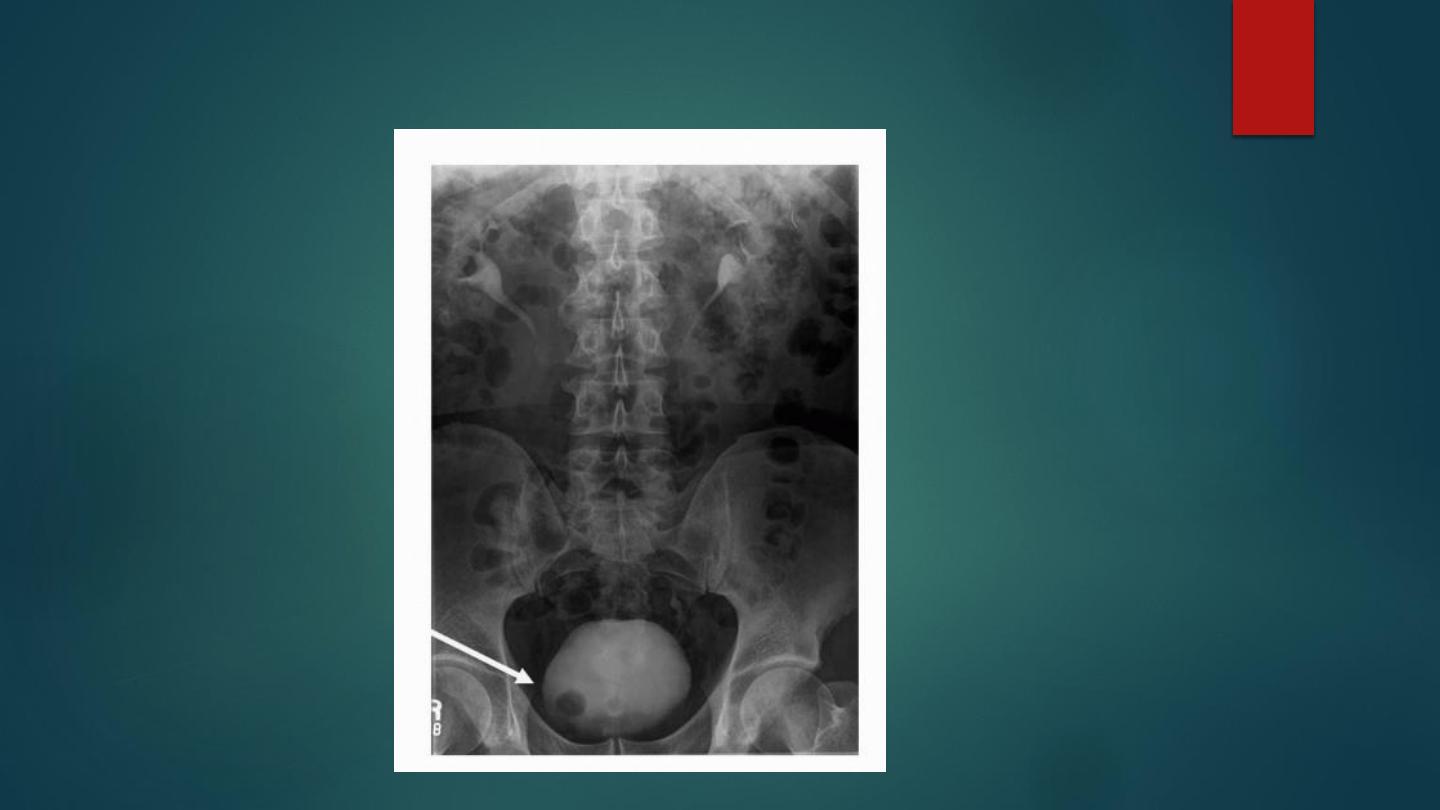
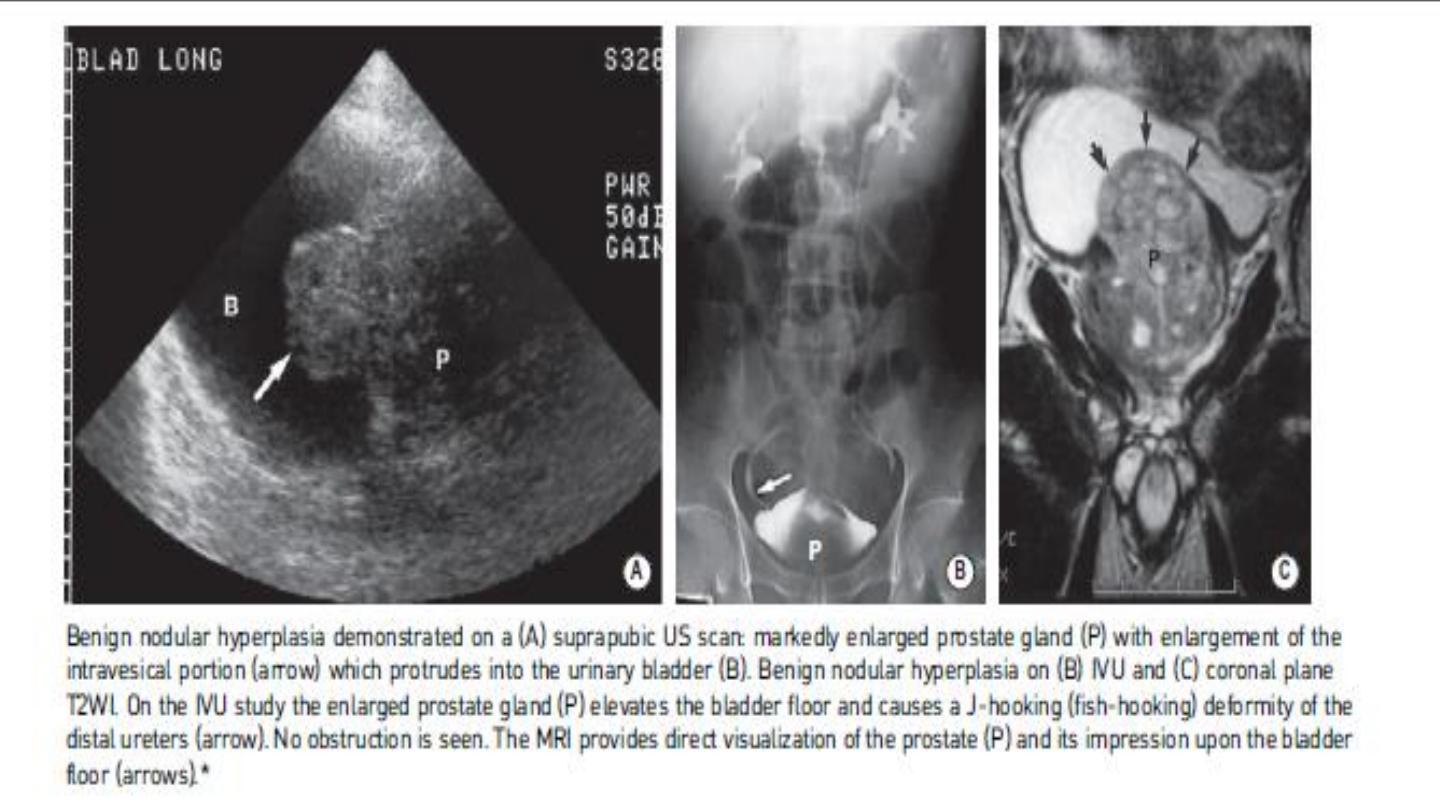
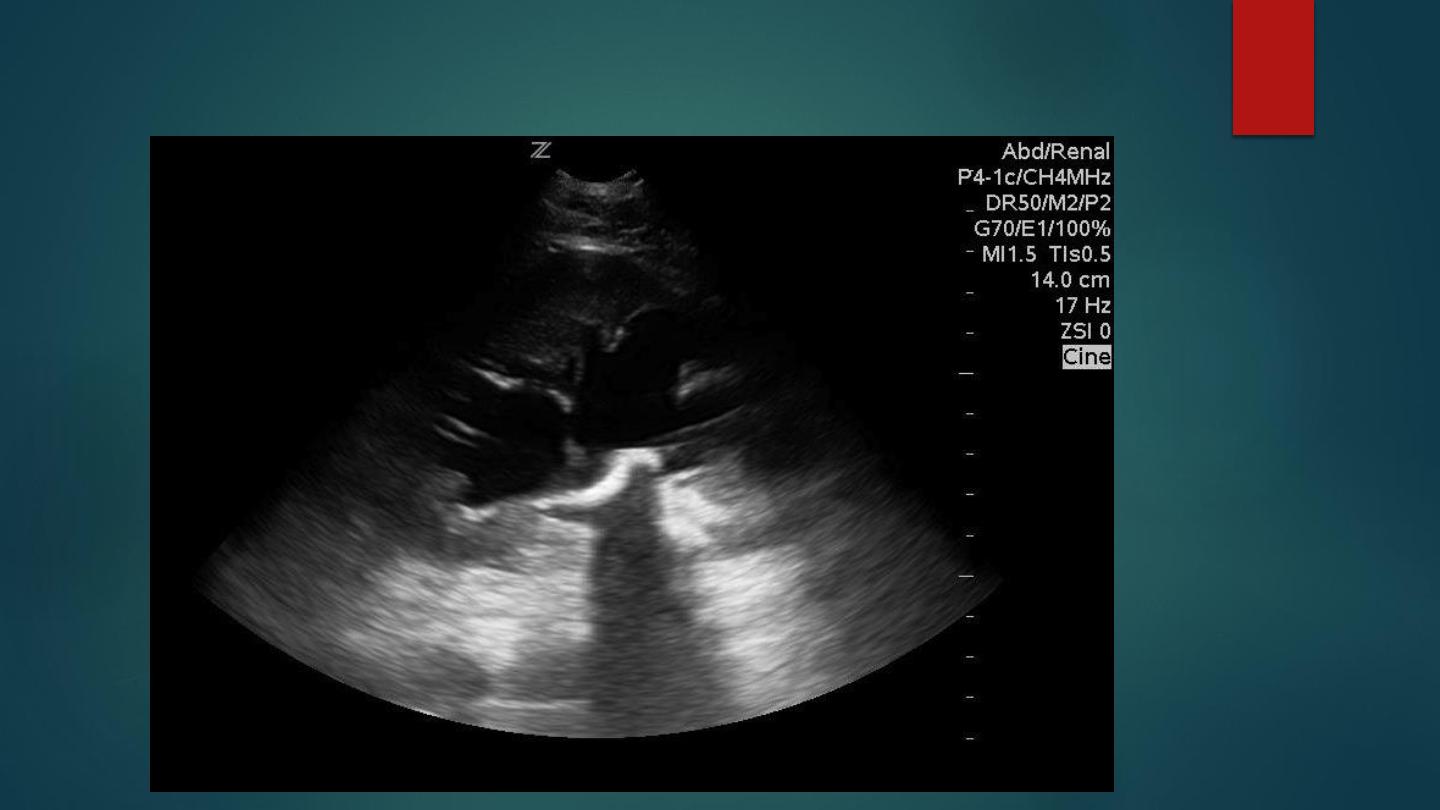
BENIGN PROSTATIC HYPERTROPHY (BPH)
Benign nodular enlargement of the prostate gland involving the transitional and periurethral zones
(carcinoma typically affects the peripheral zone)
Cystourethrography:
An elongated and compressed urethra.
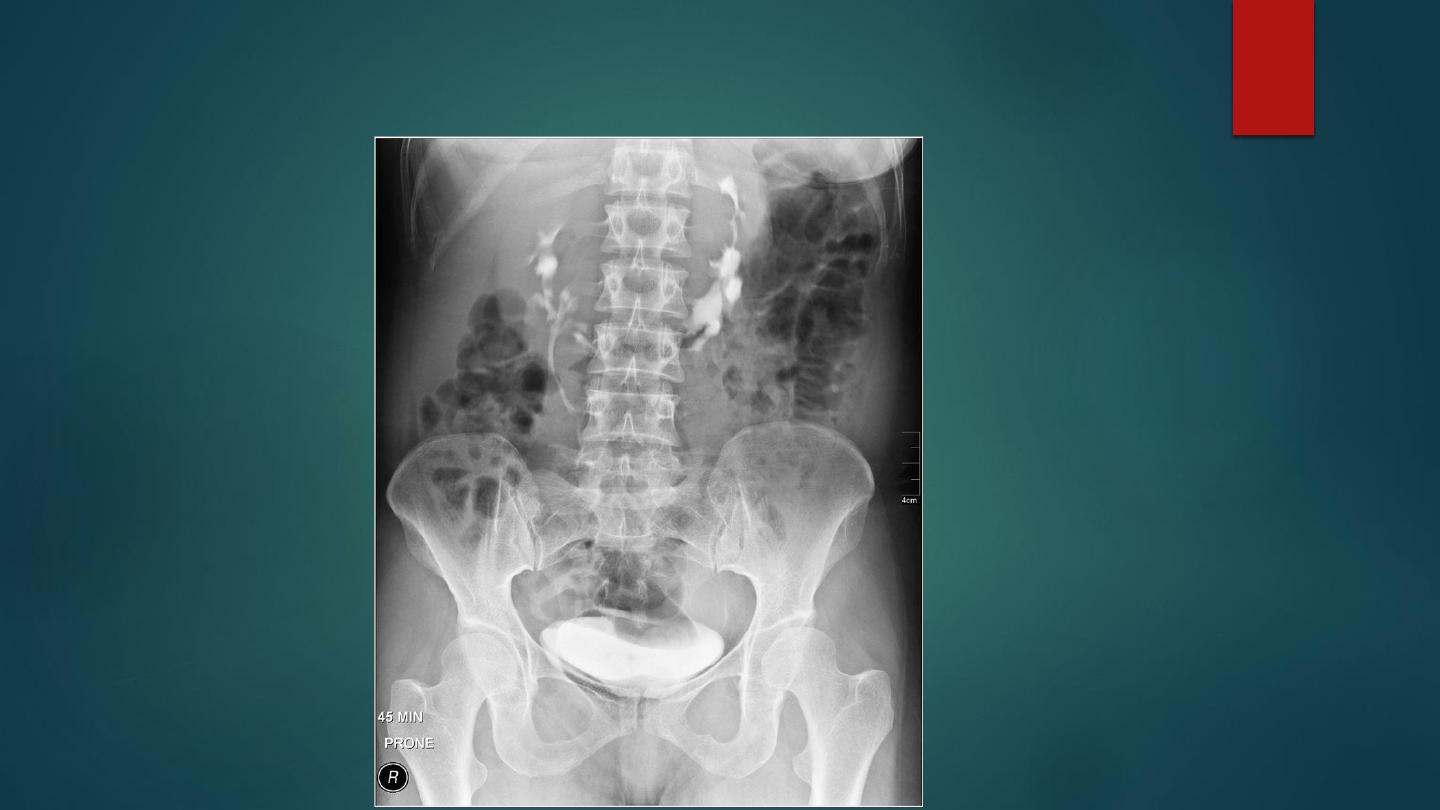
IVU/retrograde cystogram:
- Bladder outlet obstruction producing bladder trabeculation, diverticulae or calculi formation ( hydroureters
and hydronephrosis)
-
J-shaped or ‘fish-hook’ ureters: as the prostate enlarges, the bladder floor is elevated and the trigone
pushed upwards.
TRUS:
-
A prostate volume > 30ml.
-
Enlarged central gland with well-defined or poorly demarcated hypoechoic or mixed echogenicity
nodules ( hyperechoic foci).
CT:
- A prostate gland seen 2–3cm above the symphysis pubis is unequivocal evidence of enlargement

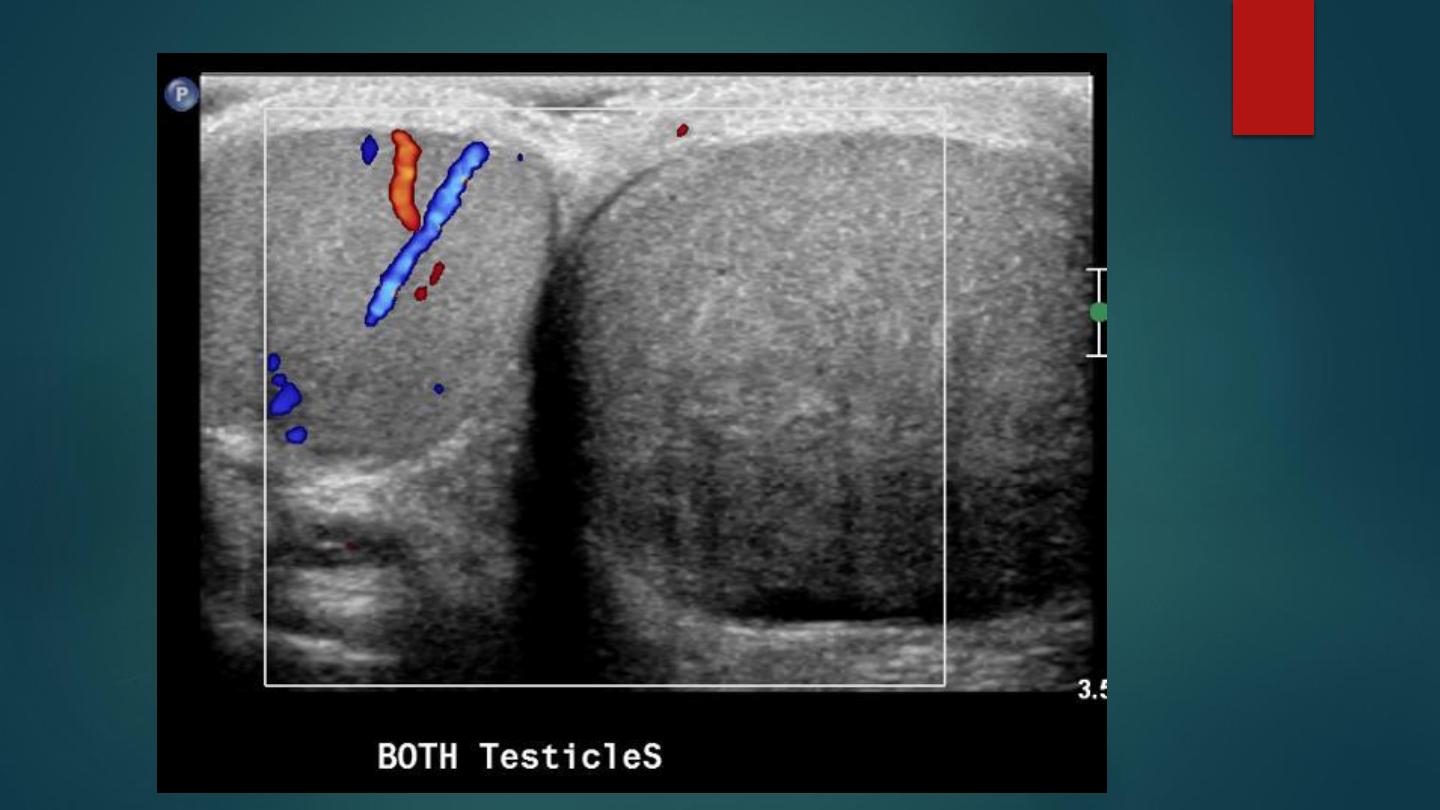
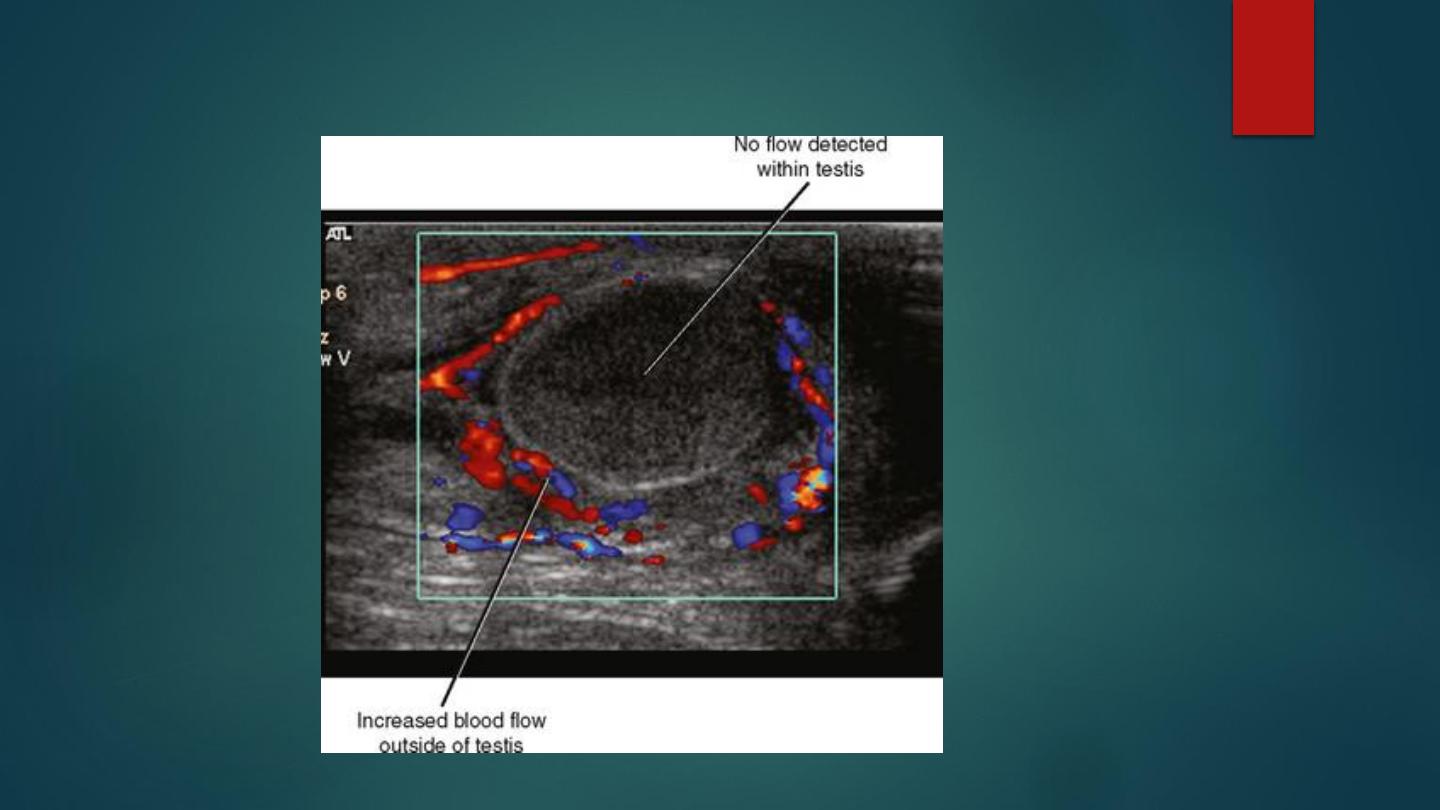
TESTICULAR TORSION
An abnormal twist of the spermatic cord as a result of testicular rotation.
It can be complete (at least 360 of rotation) or incomplete .
The degree of torsion determines the severity of testicular ischaemia and the rapidity of
any irreversible changes.
Acute: lasting between 24 h and 10 days ▶ subacute or chronic: > 10 days.
It is commonly seen during the 1st year of life or during adolescence (when the testicle is
rapidly enlarging).
Intravaginal: this affects an older age group and is common.
Extravaginal: this affects infants and is rare.

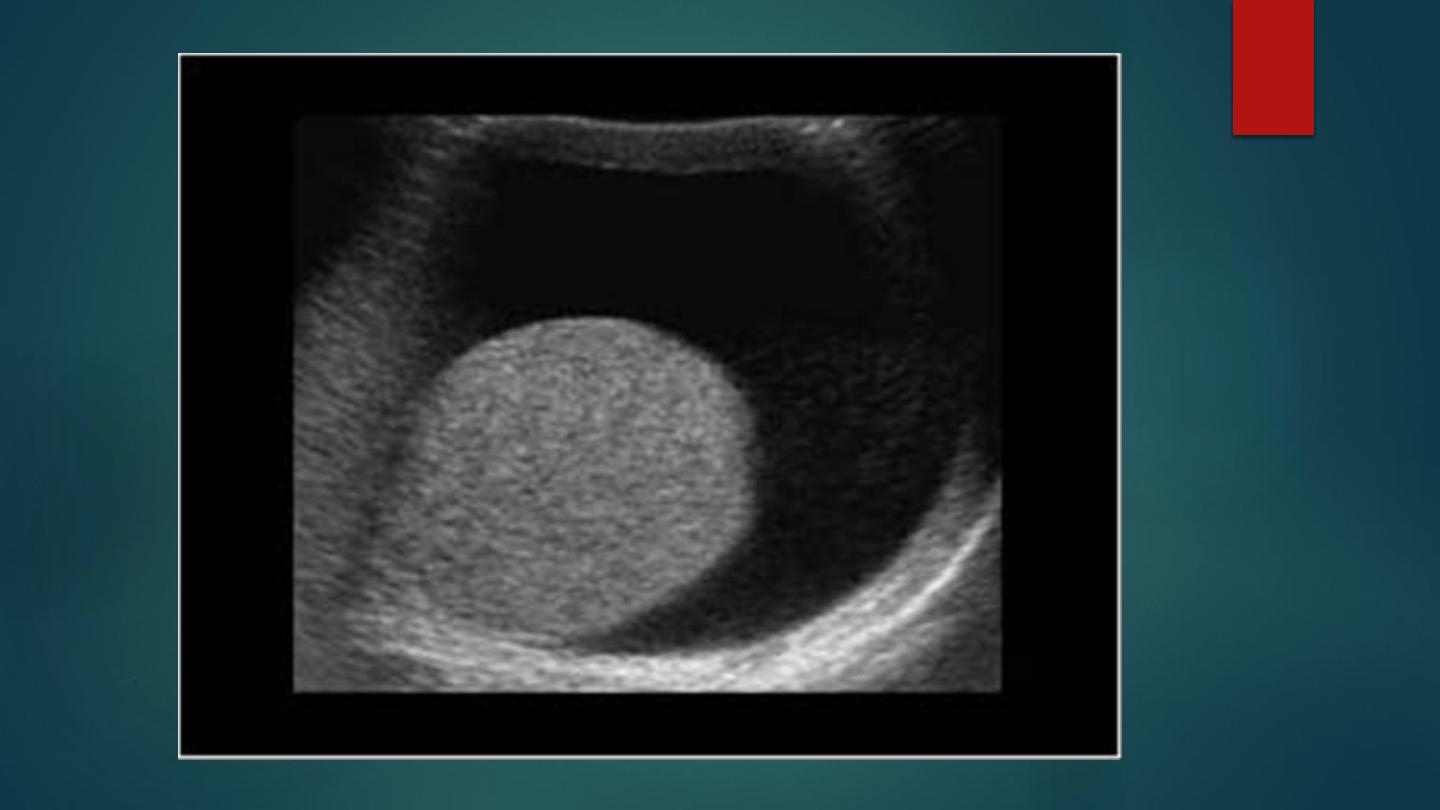
Radiological features
Ultrasound:
• Acute: an enlarged heterogeneous testis and epididymis.
• Chronic: a reactive hydrocele.
Color Doppler Ultrasound:
• Absent or markedly reduced testicular blood flow.
• The demonstration of normal blood flow does not exclude torsion
(which can be intermittent)
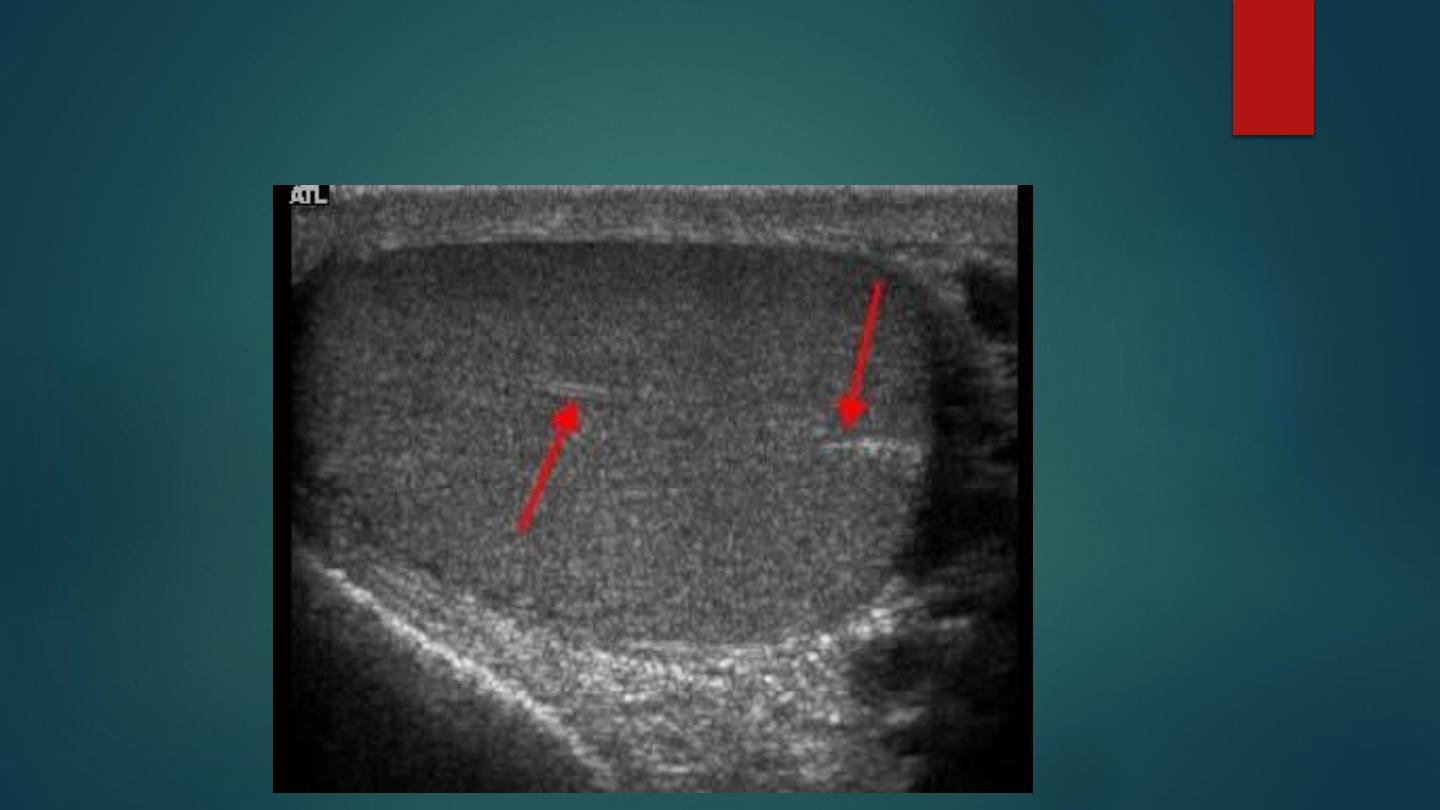
Gray scale ultrasound of testis. Normal homogeneous echogenicity is finding
that characterizes normal testicle. The linear echogenic band running
through the testis is a normal structure called the mediastinum testis (arrow).
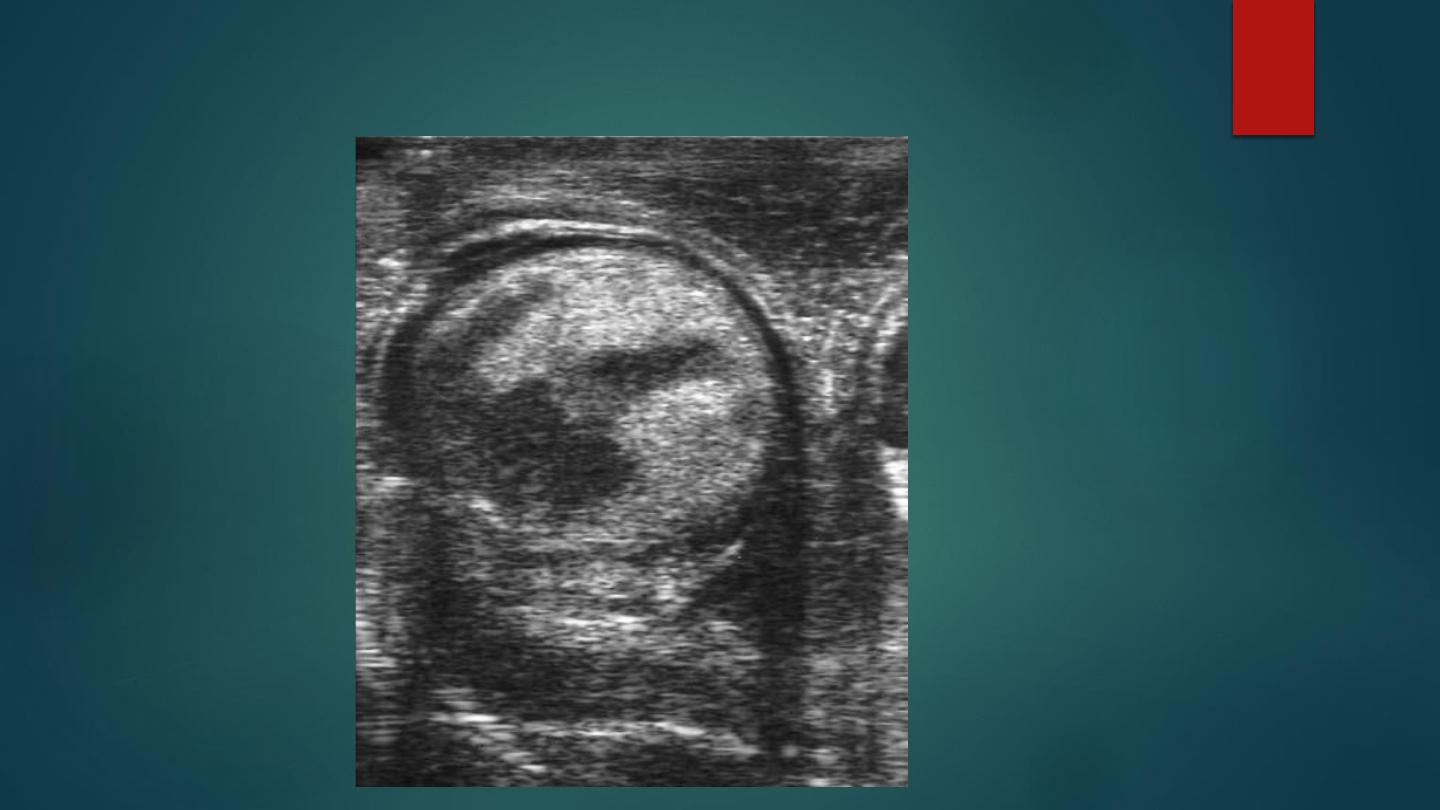
Infarcted testicle. There are extensive areas of reduced echogenicity within the testicle and
the adjacent epididymis is also markedly swollen
Doppler of an enlarged testis showing no Doppler flow within the infarcted
testis and only in the surrounding epididymis

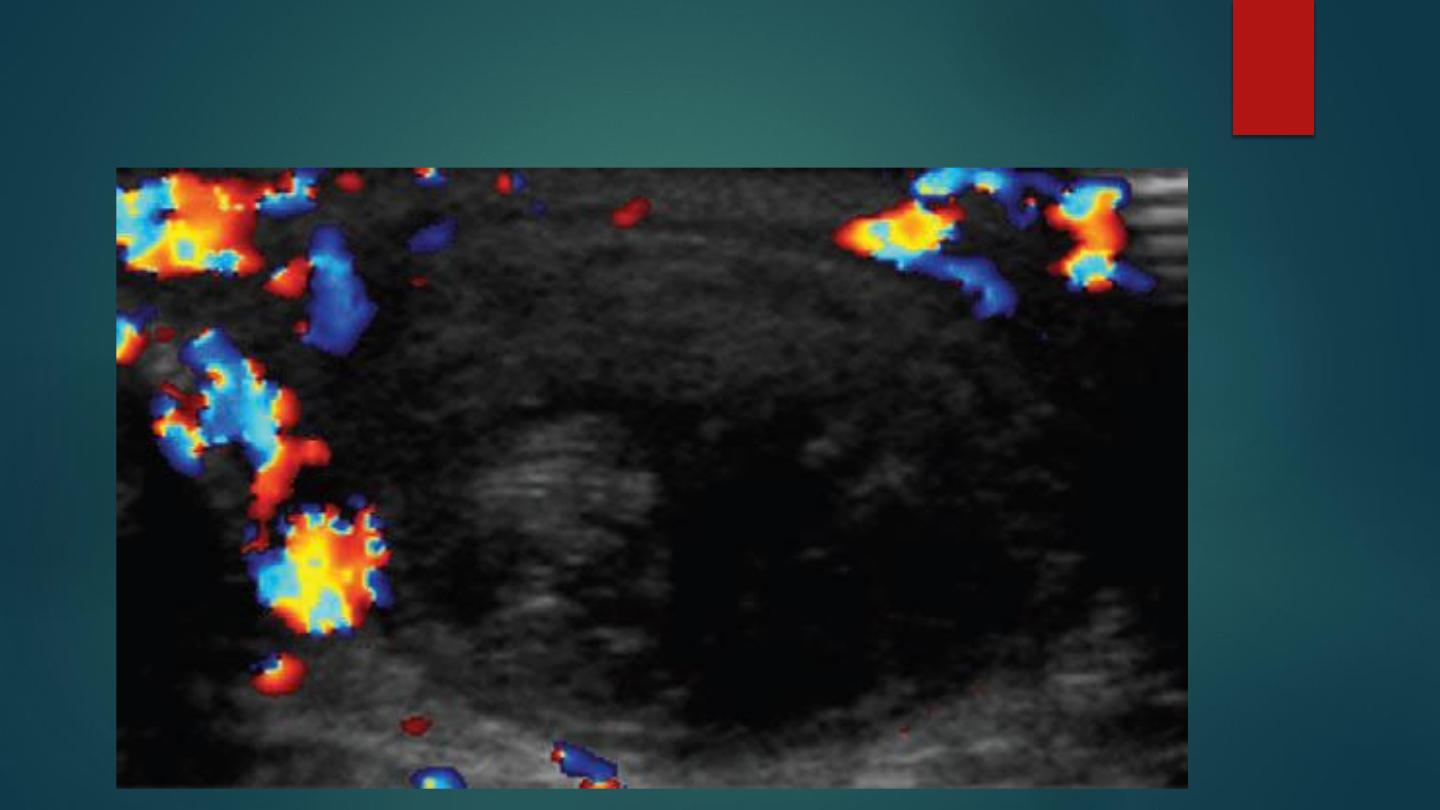
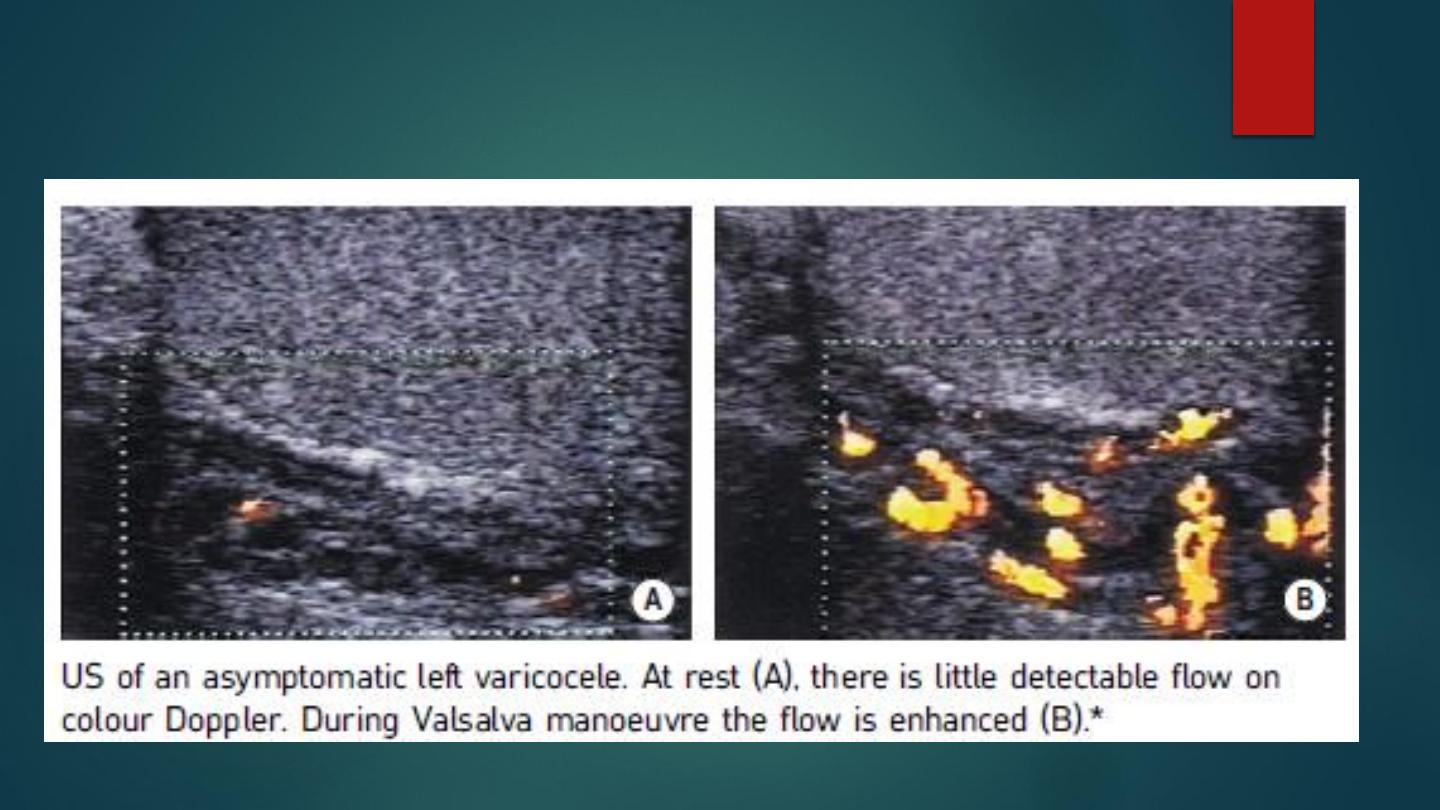
VARICOCELE
Dilated tortuous veins of the pampiniform plexus, it is associated with
male infertility
Causes: idiopathic (invariably left sided due to more indirect drainage of
left testis into left renal vein). secondary to incompetent valves within the
spermatic vein.
Ultrasound:
- Multiple serpiginous tubules > 2mm in diameter superior and posterior to
the testis (they may extend to the inferior pole of the testis).
- Spontaneous flow may not be seen – flow may be demonstrated with
coughing, rapid inspiration or the Valsalva manoeuvre.
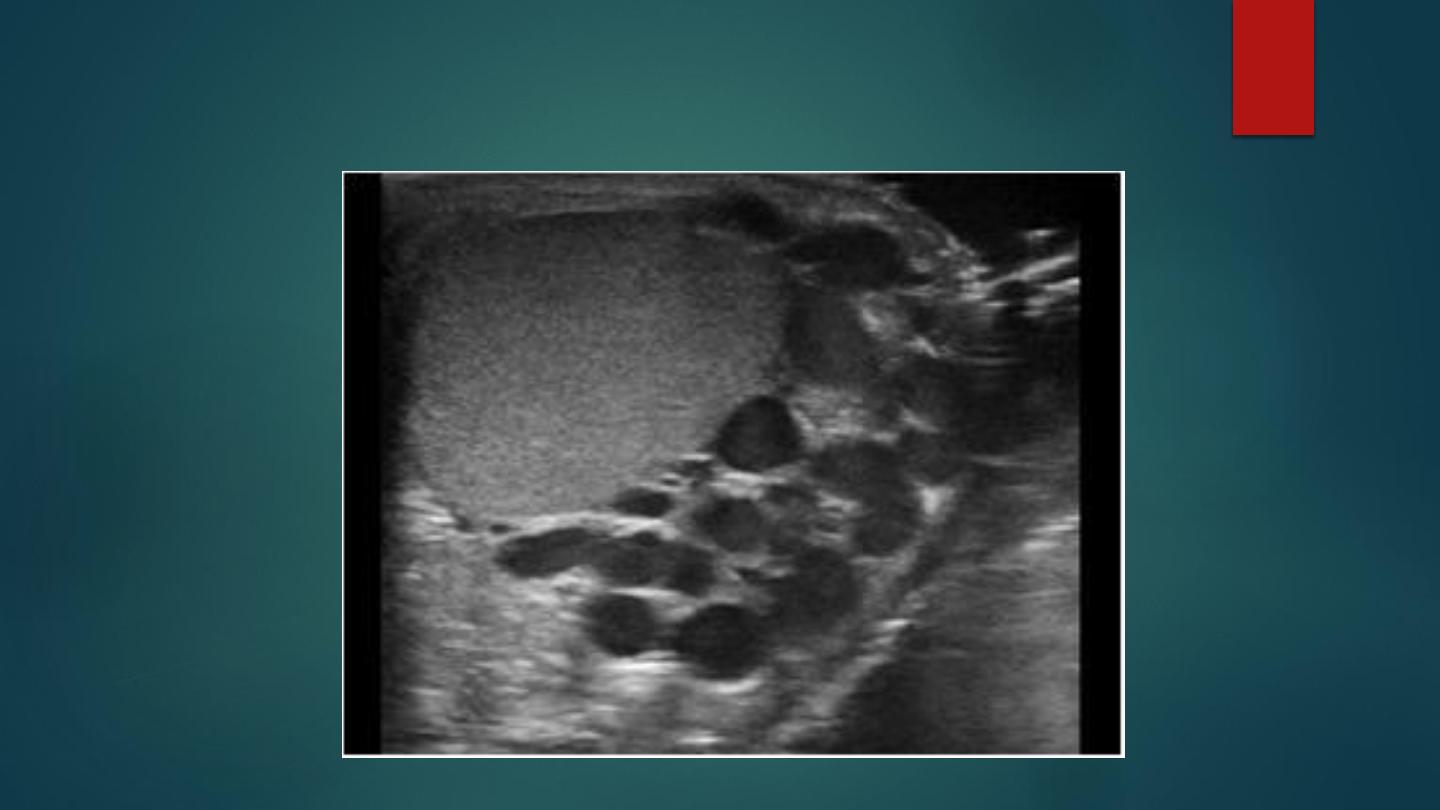
VARICOCELE
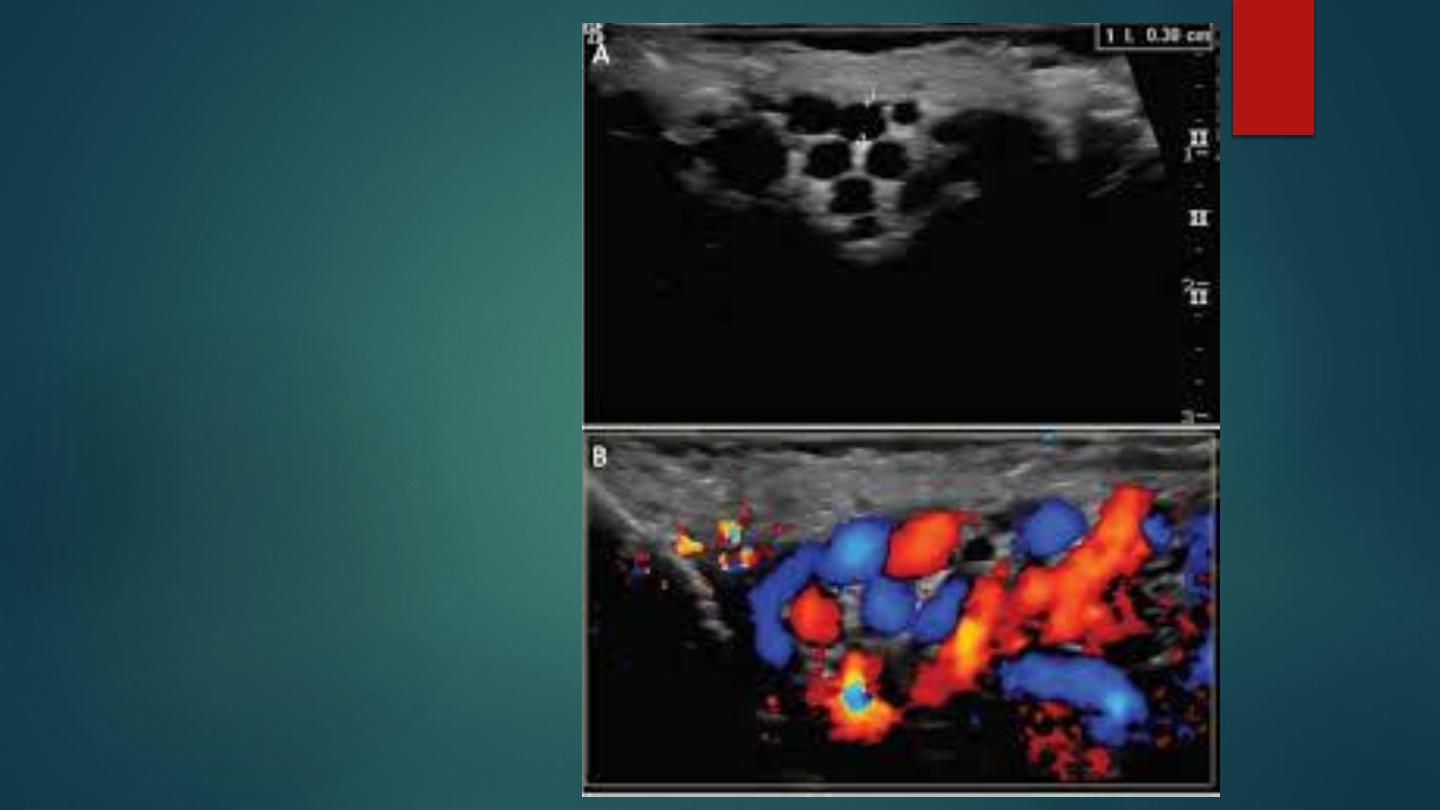
VARICOCELE

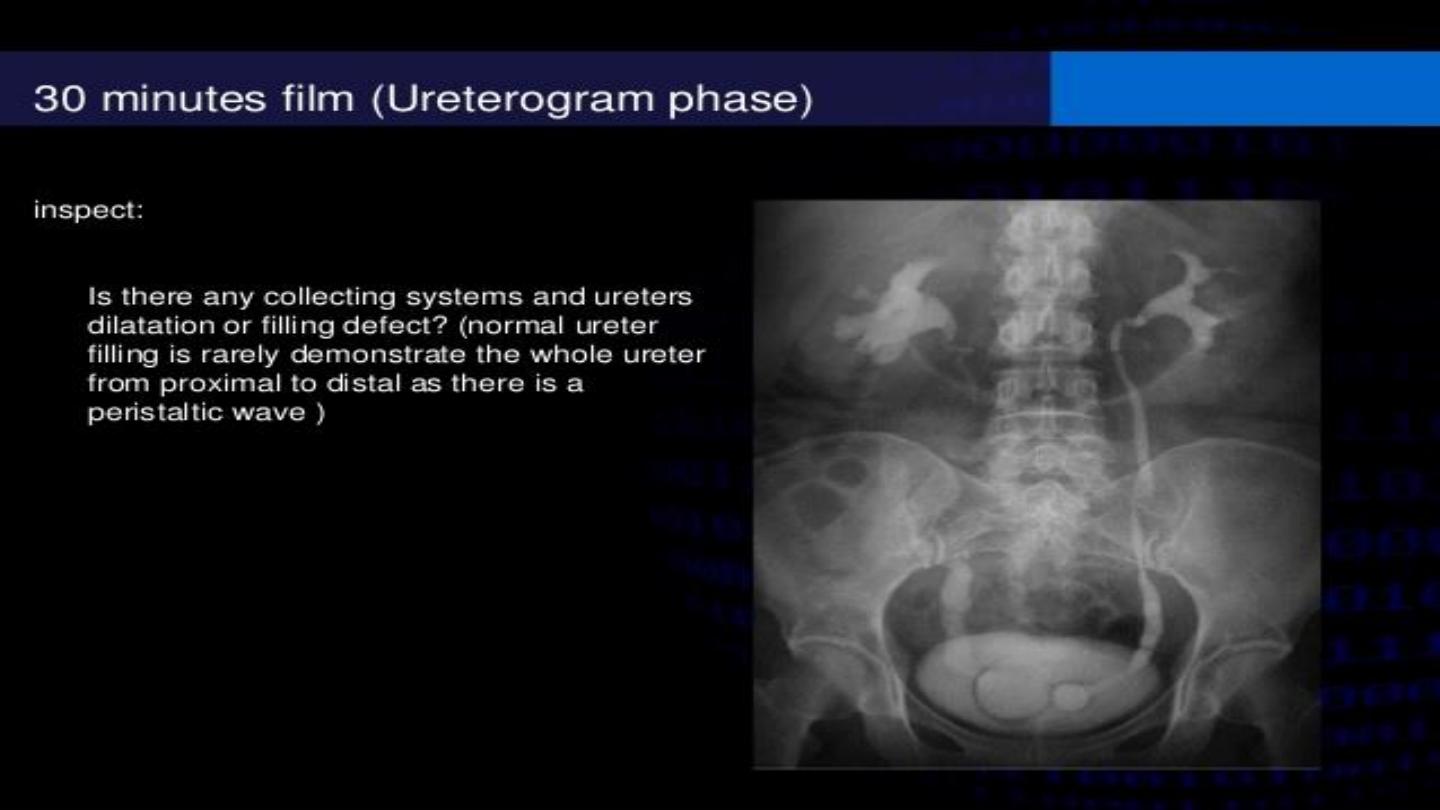
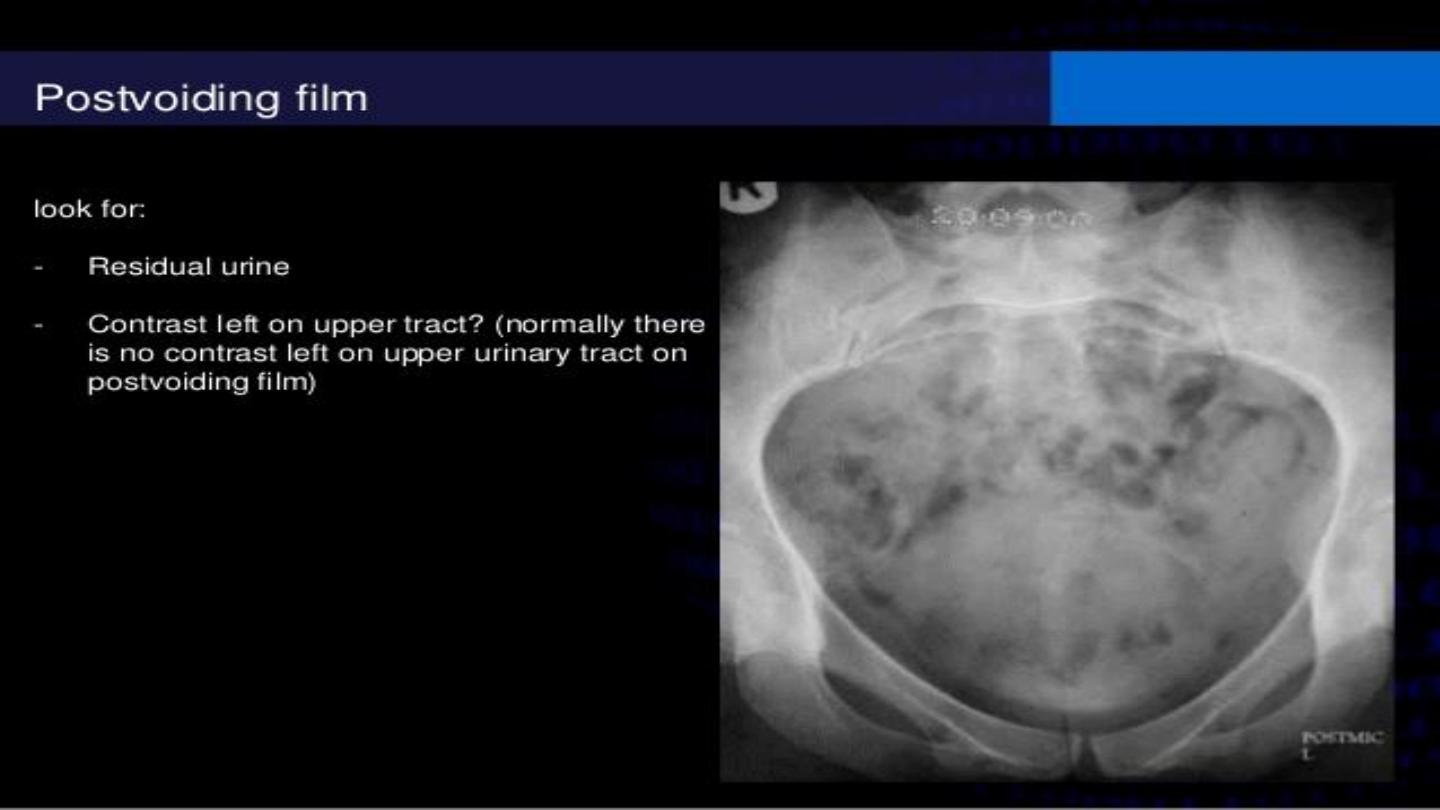
Film Reading
Staghorn Calculus
Staghorn PUJ Calculus
Staghorn Calculus X-ray

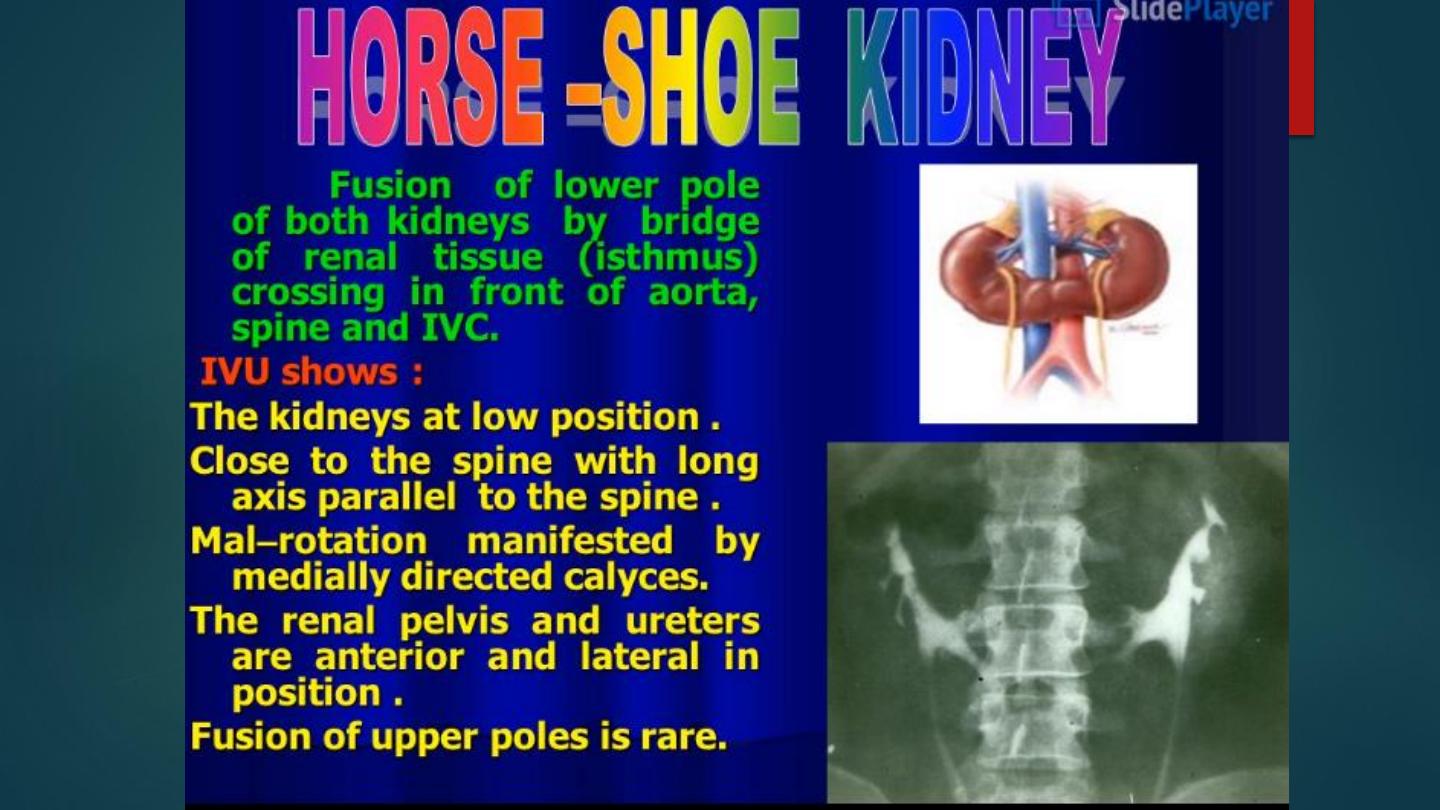
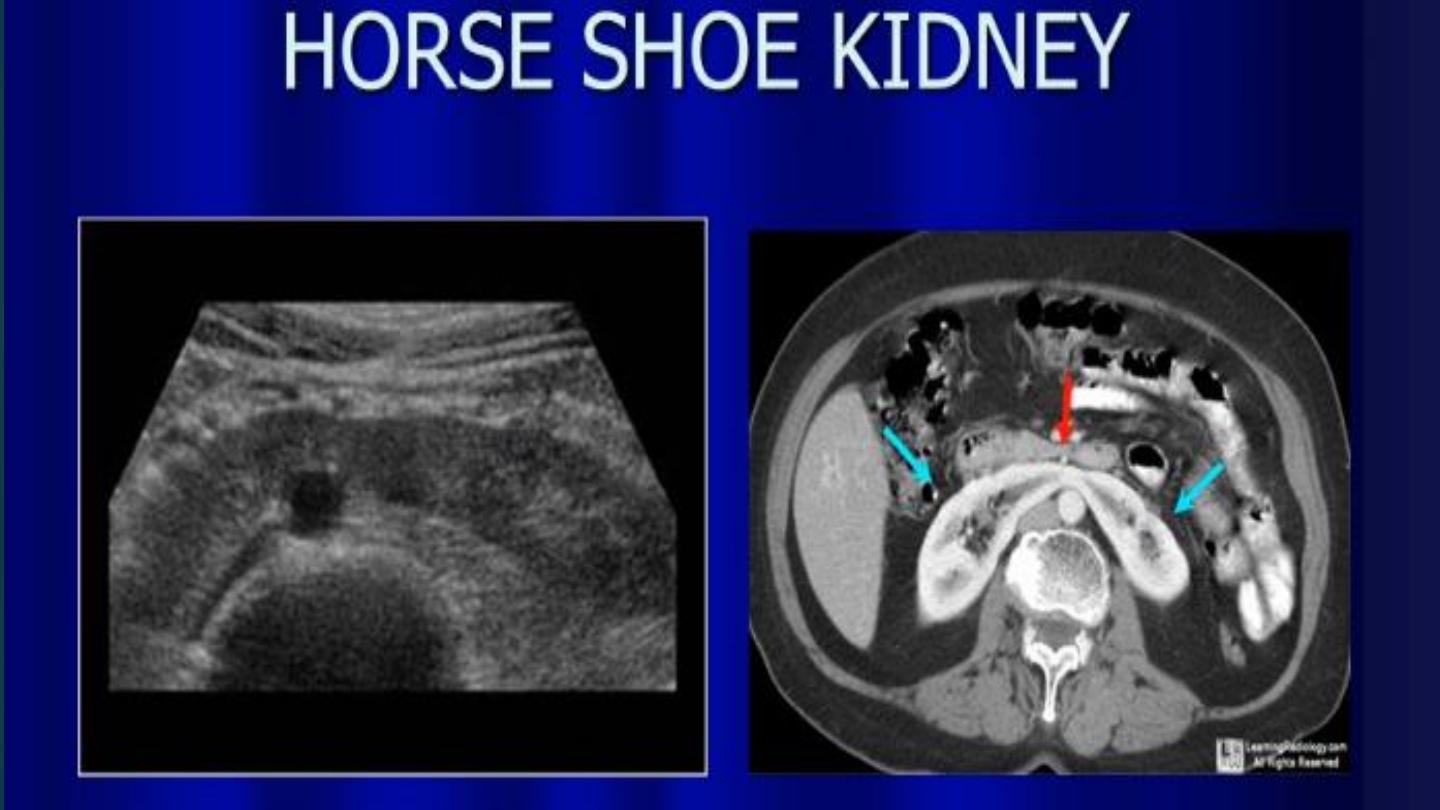
CT scan – Horseshoe Kidneys

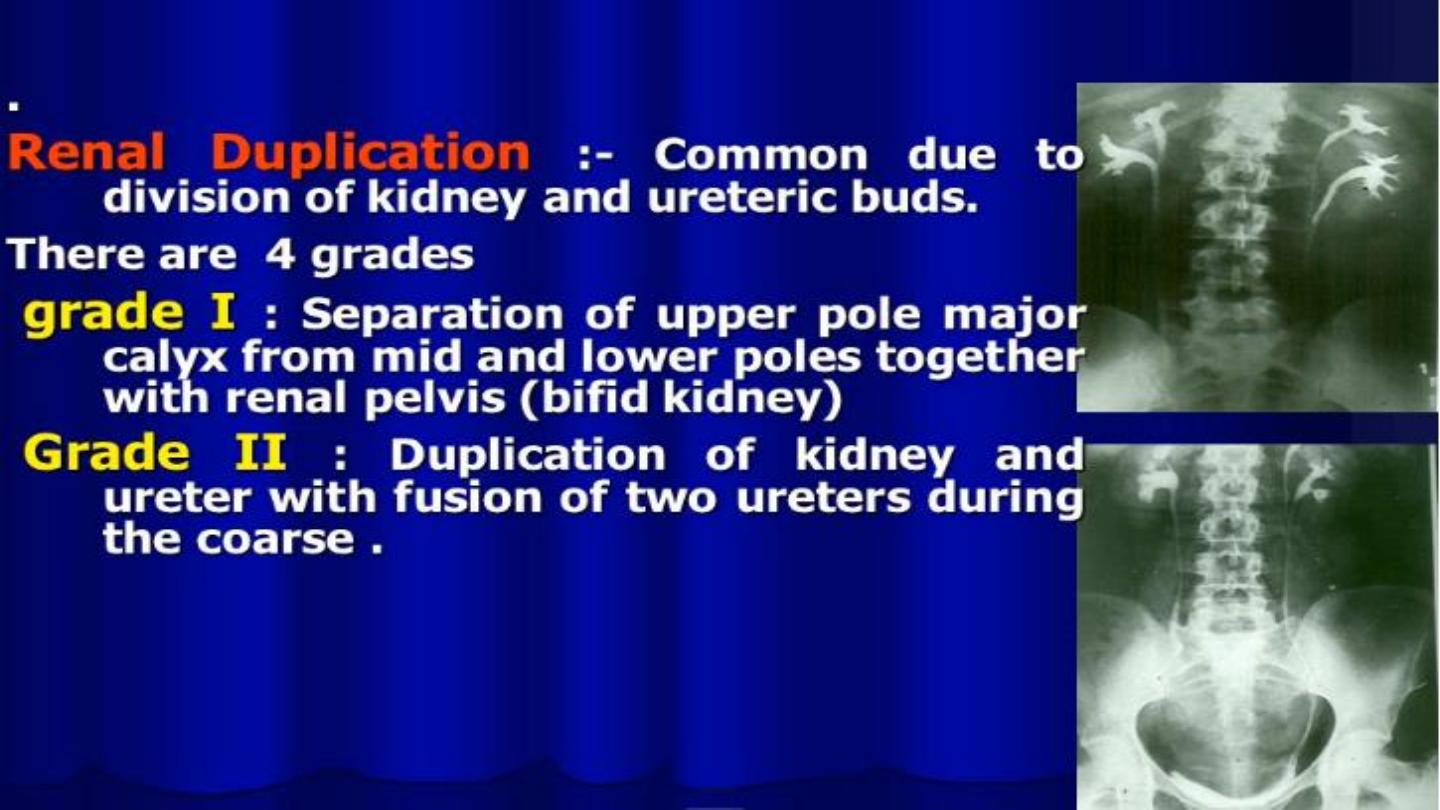
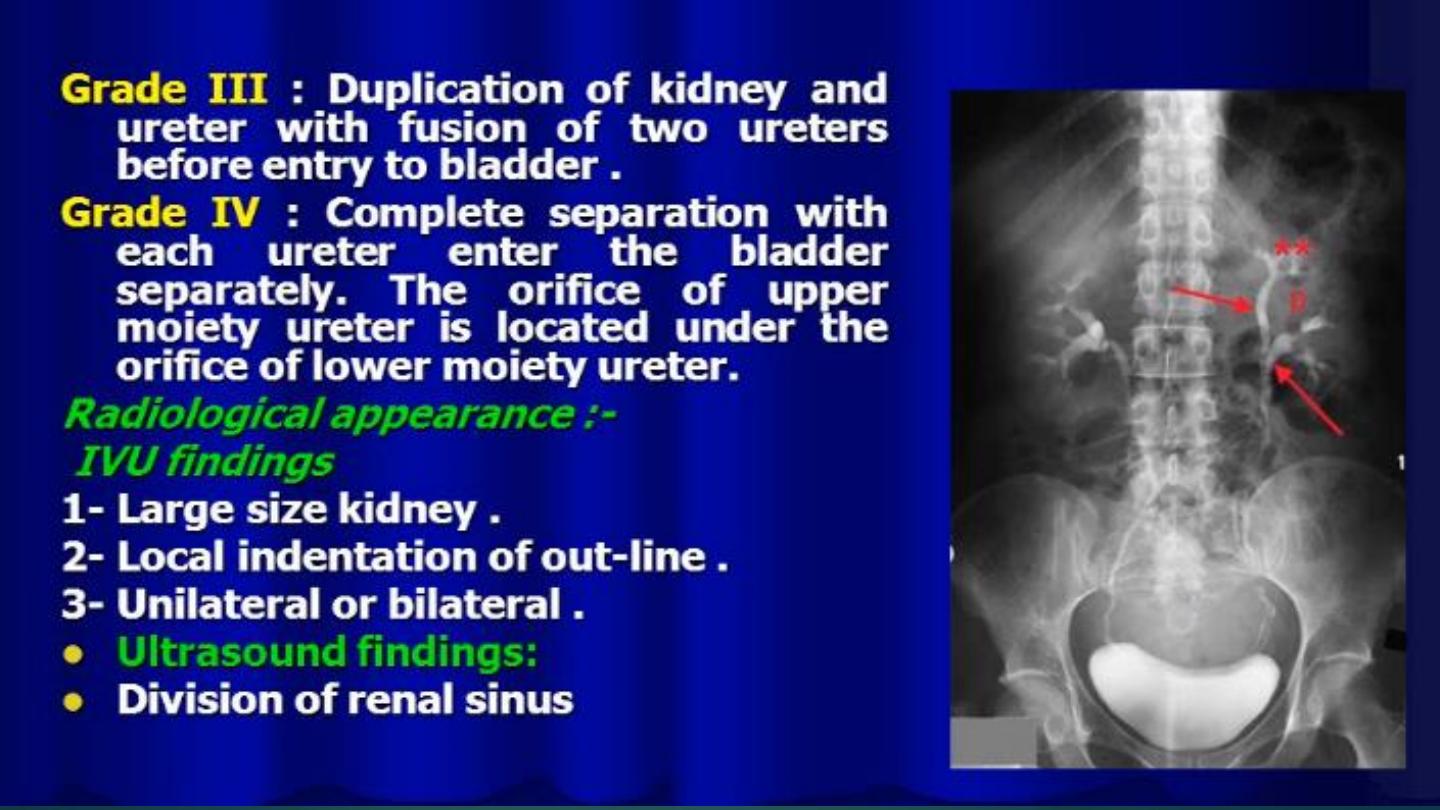
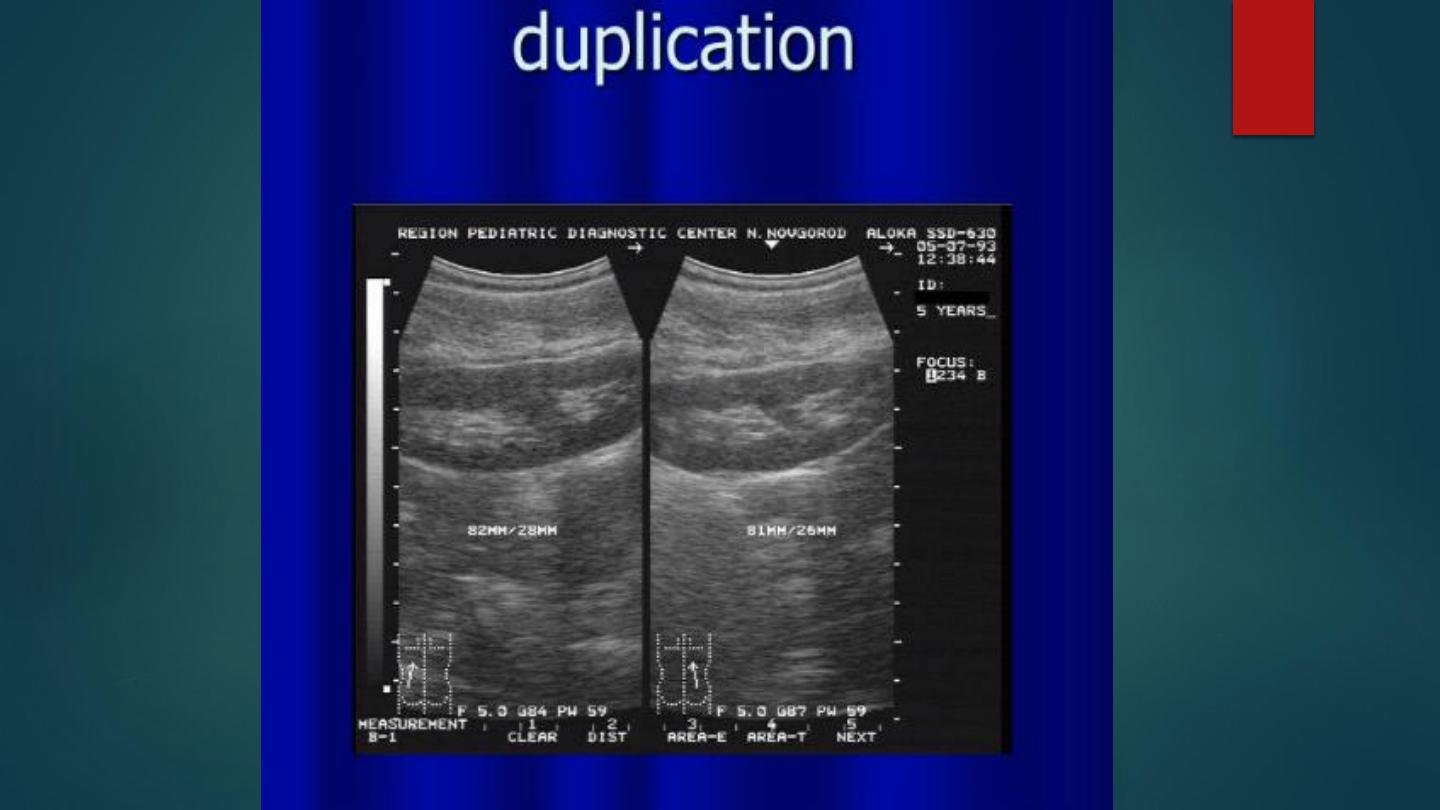
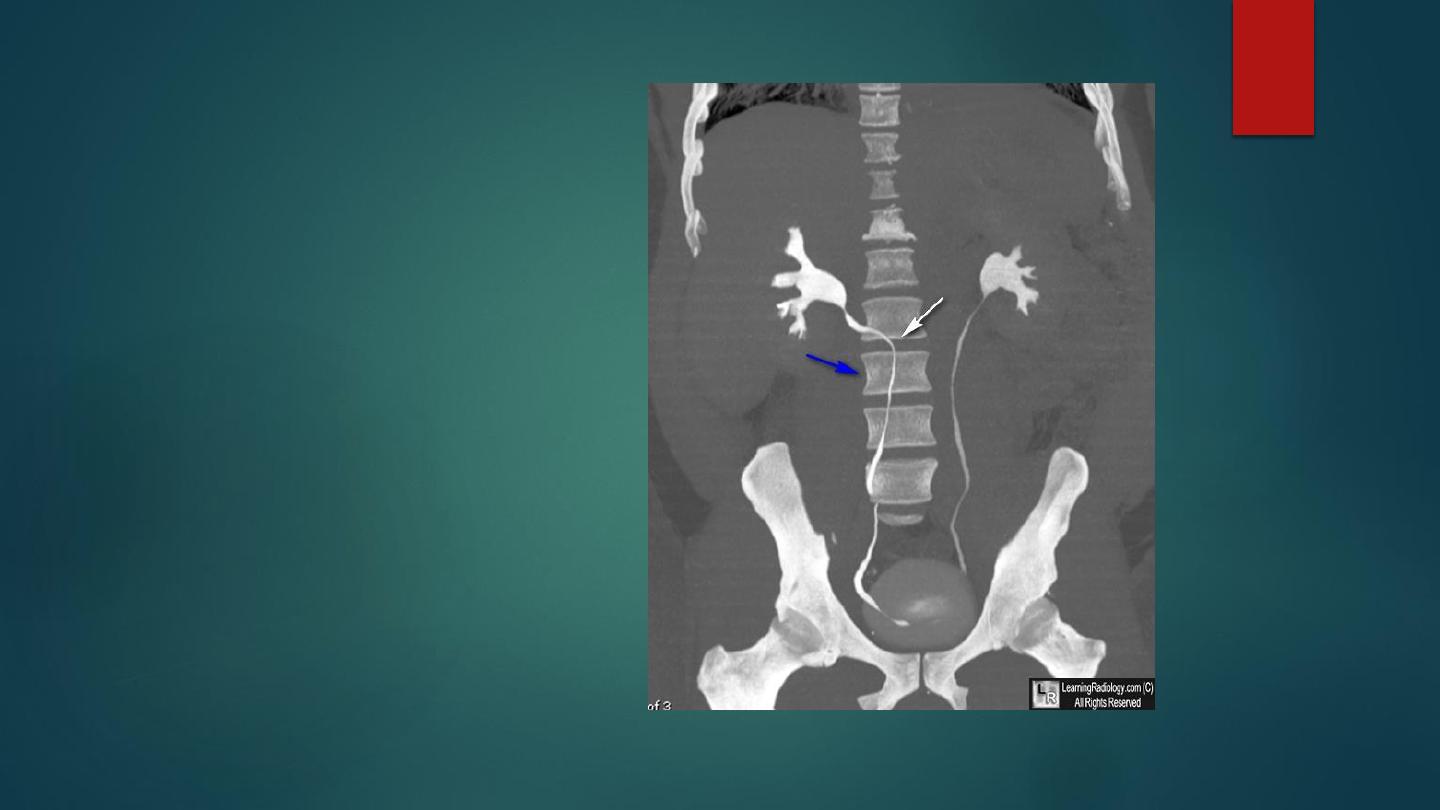
Intravenous urography film showing
incomplete duplication (white
arrow) on right side and complete
duplication (black arrow) left side
with ureterocele (curved arrow) of
upper moiety ureter.
IVP showing Horseshoe kidney
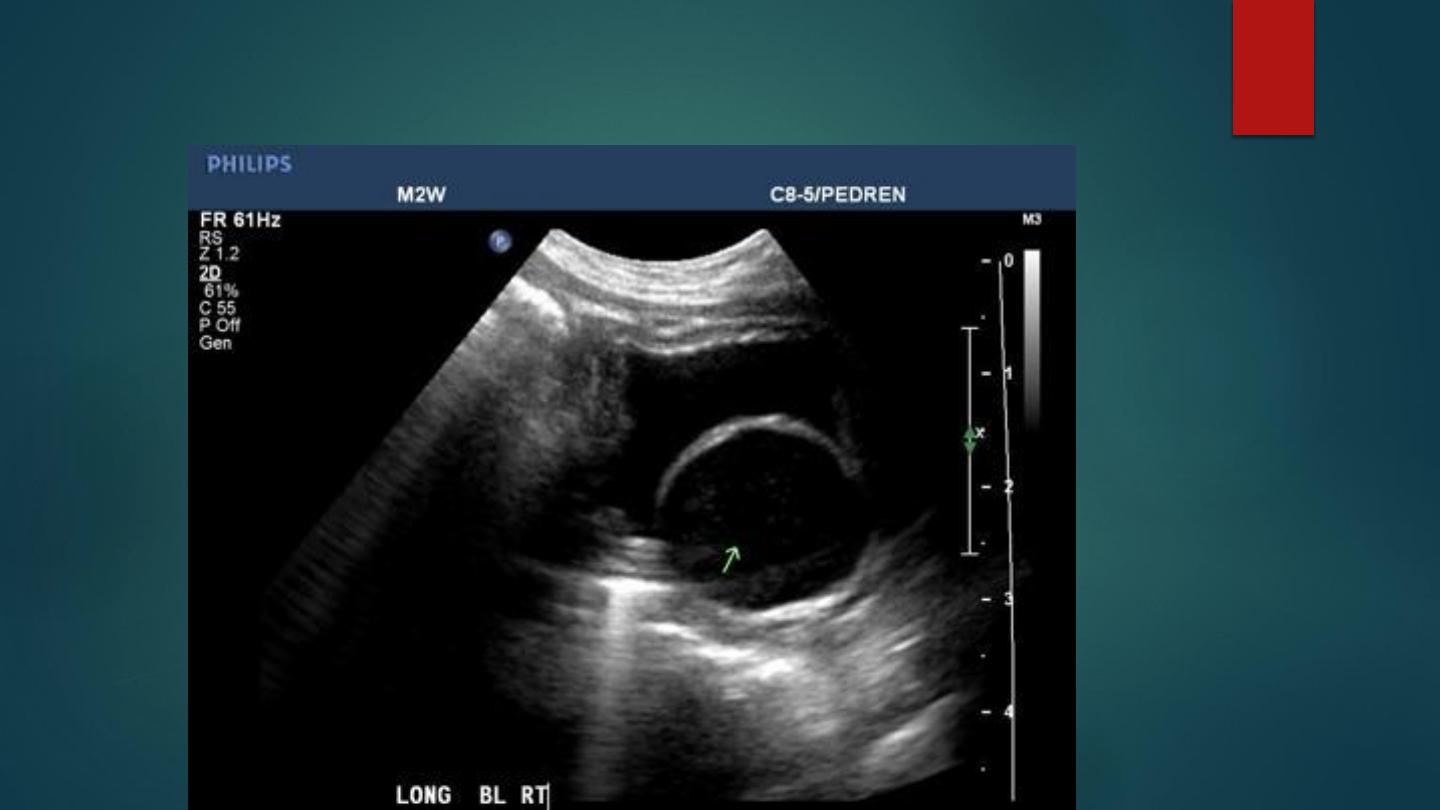
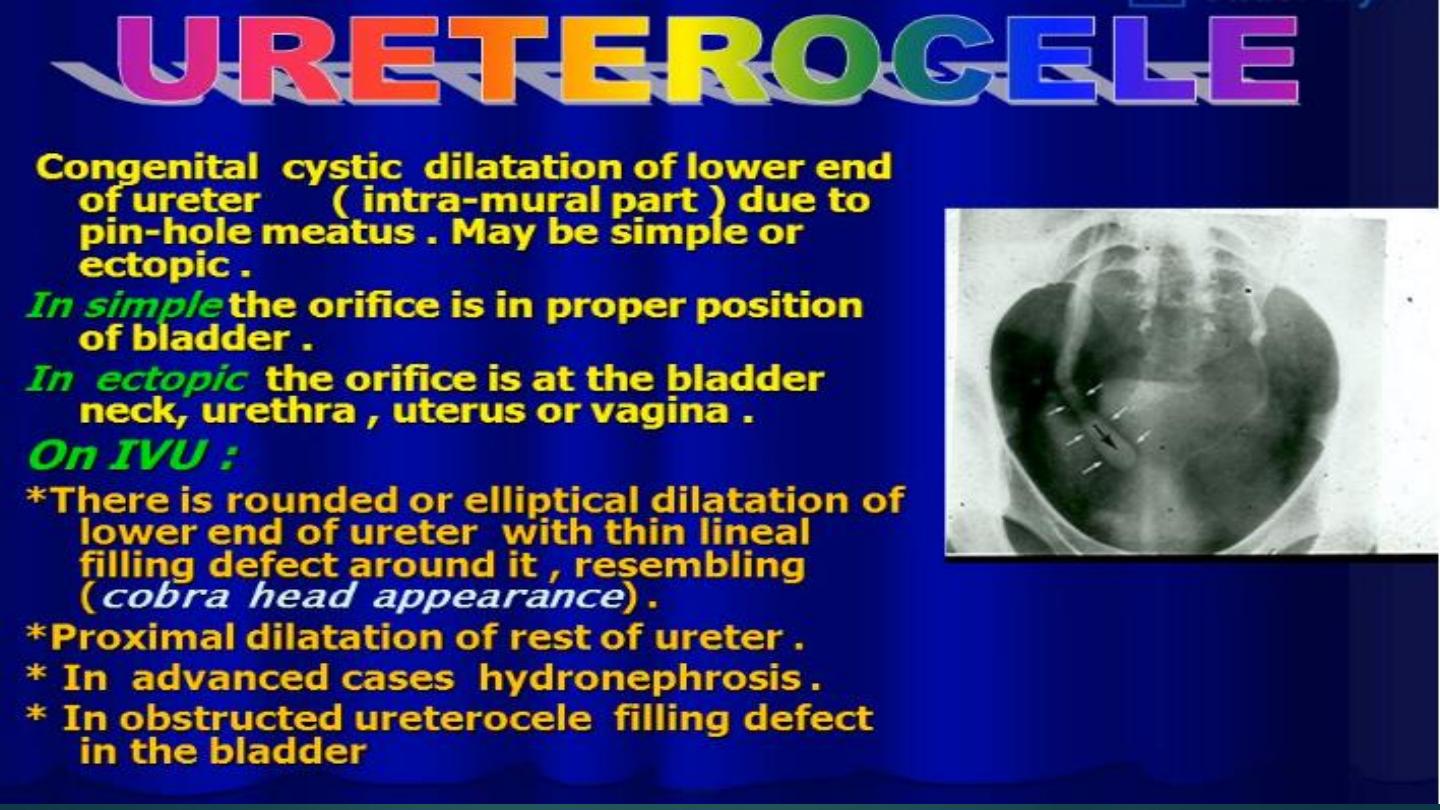
Ultrasound of Ureterocele
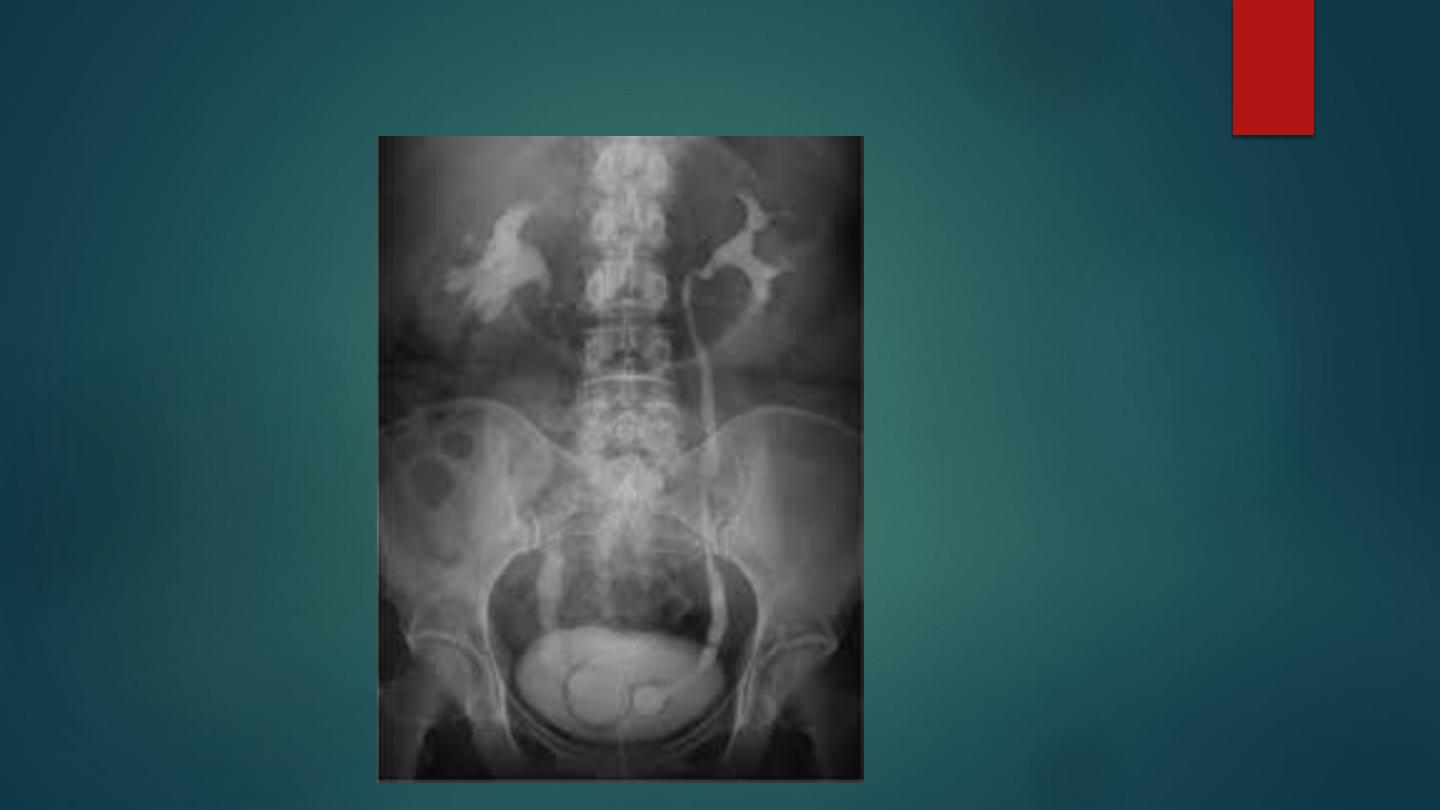
IVU of bilateral Ureterocele
IVU of obstructed Ureterocele

Sagital CT of Renal Cell Carcinoma

CT scan of Renal Cell Carcinoma
CT scan of Bladder TCC

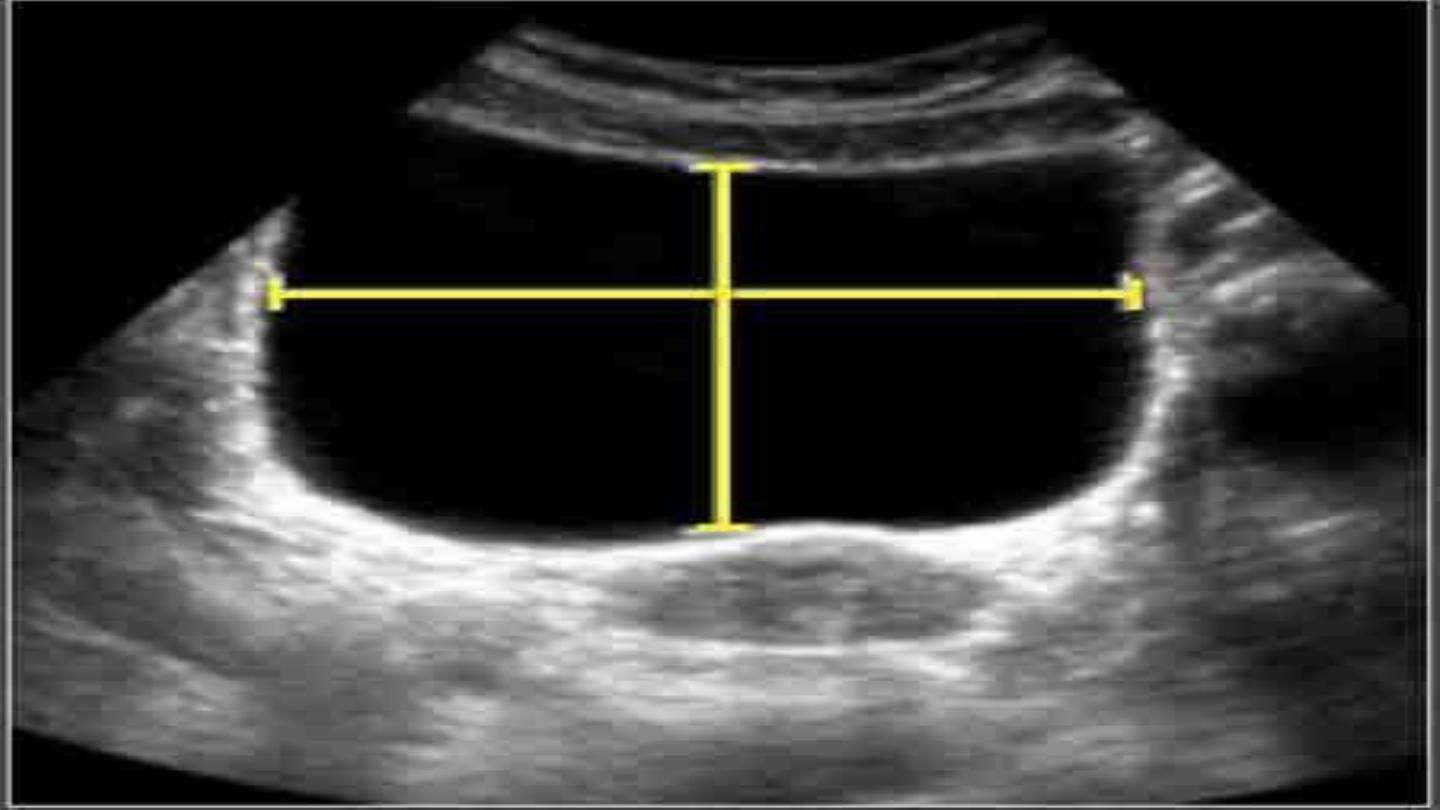
Ultrasound of BPH
IVU image demonstrating BPH

Ultrasound of Bilateral Hydrocele
Testicular Torsion
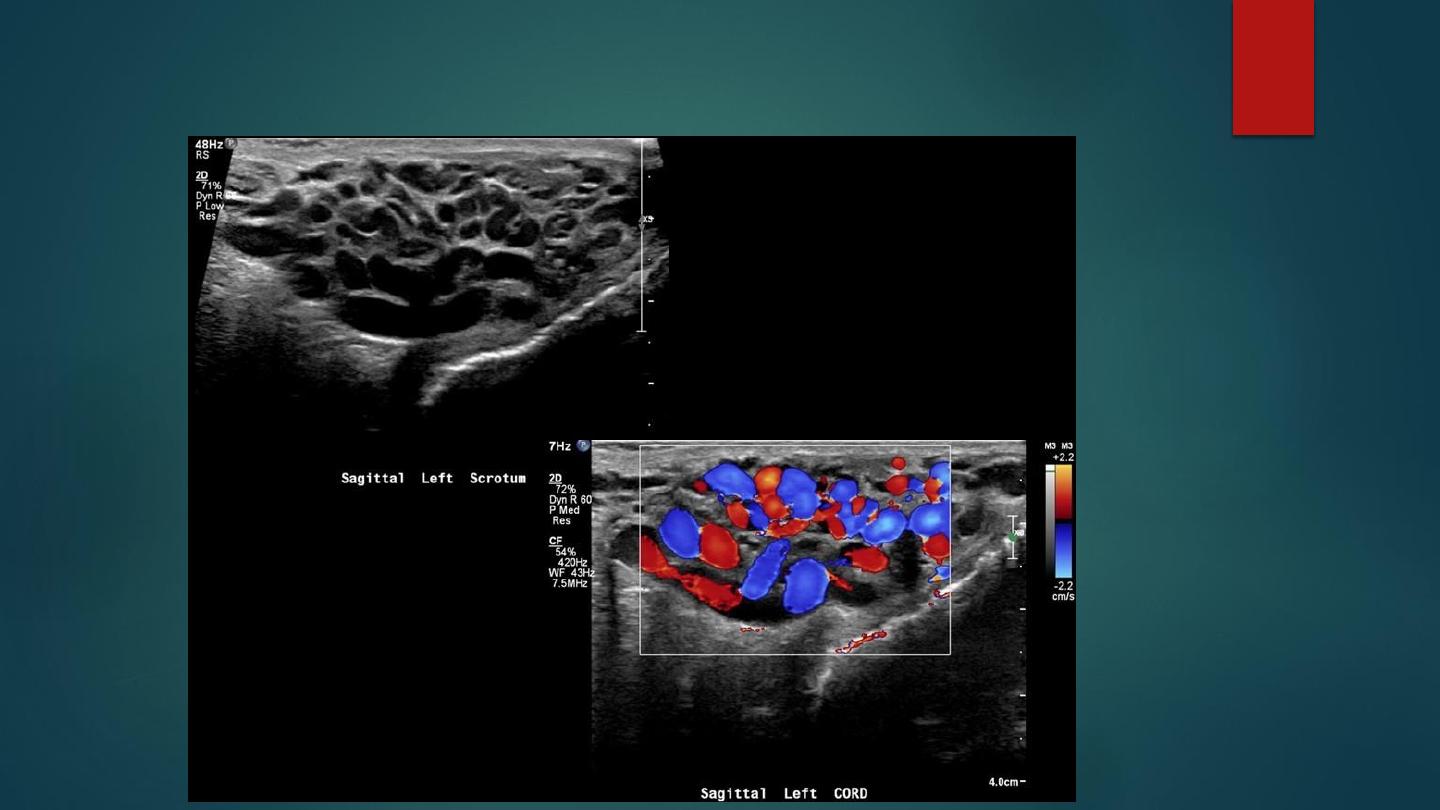
Varicocele

CT Scan of left ureteric stone

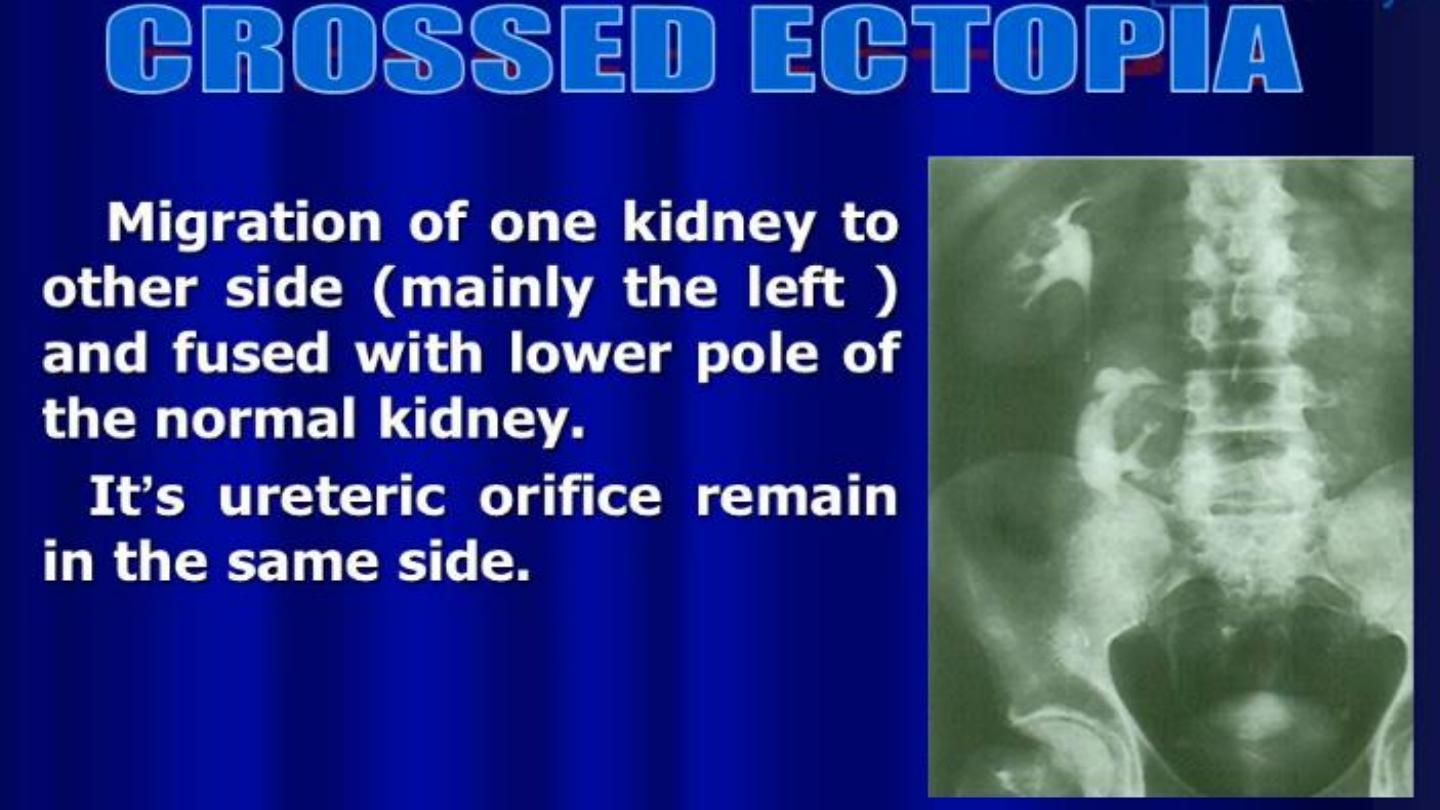
Crossed Fused Ectopia

THANK YOU
