RHEUMATOID ARTHRITIS
Dr. Nizar AbdulateefAssistant Professor & Consultant Rheumatologist
Learning objectives
1. To understand proposed pathophysiologic mechanisms that result in the inflammation and pathology of rheumatoid arthritis (RA).2. To define the clinical features, laboratory & radiologic findings of RA.
3. To understand the principles behind current and future therapy of RA.Case History
Ms. JA, 47-year-old woman gradually developed painful wrists over 3 months; she consulted her doctor only when the pain and early morning stiffness stopped her from gardening.On examination, both wrists and the metacarpophalangeal joints of both hands were swollen and tender but not deformed. There were no nodules or vasculitic lesions.
On investigation, she was found to have a raised C-reactive protein (CRP) level (27mg/l) (NR <10) but a normal haemoglobin and white-cell count. A latex test for rheumatoid factor was positive and antinuclear antibodies were not detected.
What is the most likely diagnosis?
What is RA?Chronic, Systemic
InflammatoryDiarthoroidal joints (meet at point where cartilage attach to cartilage)
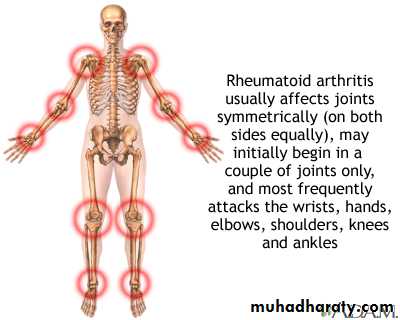
Usually a polyarthritis with symmetrical joints affected
Extra-articular features = affects organs outside the joint (skin, blood vessels, nerves, heart, lungs, muscles, etc...)
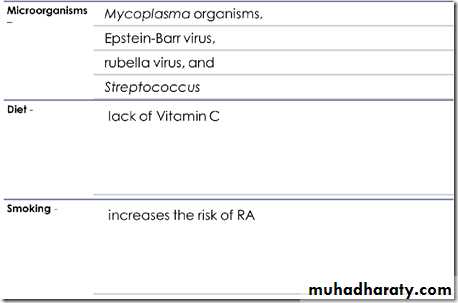
Etiology
Genetic susceptibility: strong association withHLA DR4
- Environmental factors
- Hormonal factors
oestrogen & progesterone
symptoms improve during pregnancy
Pathogenesis
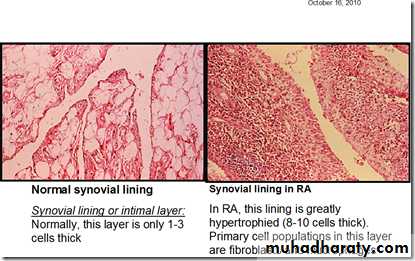
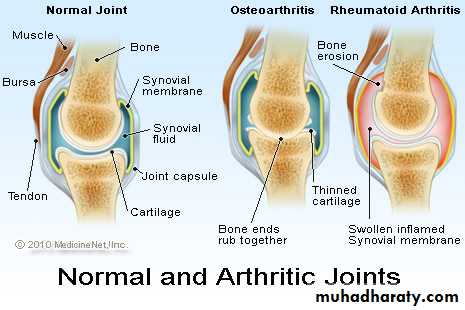
Synovium and Synovitis1-3 cell layers thick; secretes fluid for lubrication -important since cartilage is avascular
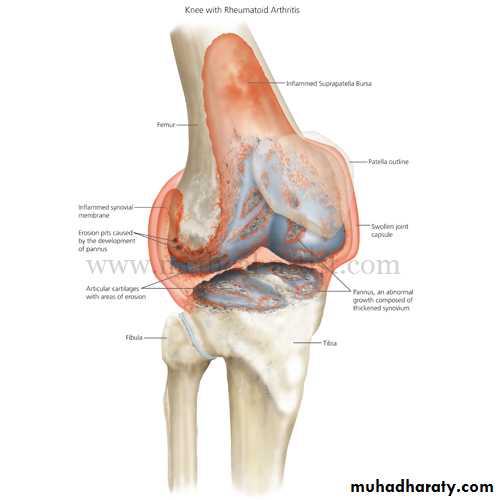
In RA, synovium become inflamed and overgrows over cartilagePannus forms = chronic hypertrophic synovial tissue
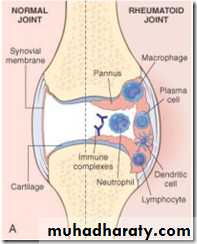
Immunogenesis of RA
Involves Rhuematoid factors, complement systemRA = represents a localized immune complex disease
Pathologic changes begin in synovium --> infilration with leukocytes + macrophages --> pannus forms
Most likely inciting incident = activation of T cells by putative antigen in a genetically susceptible individual --> this stim B cells which produce autoantibodies and secret pro-inflamm cytokines --> inflammation process has begun
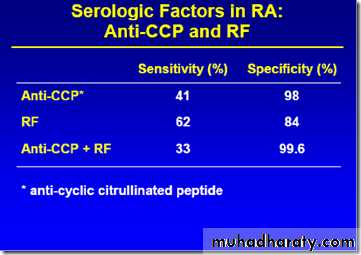
Antibody that has some predictive value of people getting RA is
* Anti-cyclic citrullinated peptide antibody (ACPA)Cytokines involved in RA
*Pro-inflamm cytokines:-TNF-alpha-IL-1*Anti-inflamm cytokines:-IL-IRa (receptor antagonist = can regulate pro-inflamm cytokines but in RA this ability to down regulate pro-inflamm cytokines is lost).
Epidemiology of RA
Affects 1% of population
Affects more women than men (3:1)
Peak age= 25-45Disease often improves during pregnancy and flares 4-6 weeks postpartum
Why is RA important?It causes significant morbidity.
Mortality is similar to Stage III Hodgkins lymphoma (so this is not a benign disease).
Economic costs are high.Patients frequently disabled.
Mortality associated with RA#1 = heart disease
Others = malignancy and infection, renal and GI
Clinical features
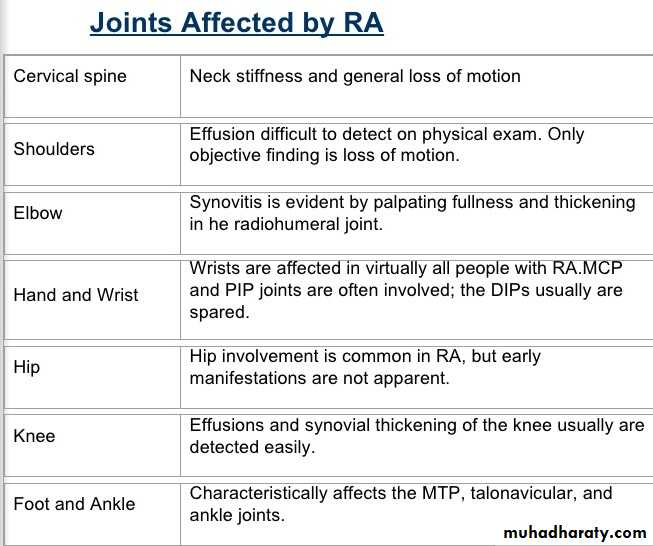
The hallmark feature of the disease is persistent symmetric polyarthritis (synovitis) that affects the hands and feet, although any joint lined by a synovial membrane may be involved.Other symptoms:
- Fatigue
- Stiffness
- Weakness
- Flu-like symptoms
- Muscle pain
- Loss of appetite
- Depression
Physical abnormalities in RA
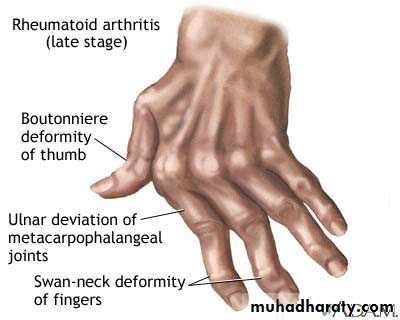
Synovitis = feels like doughy - Spindyling of the fingers- Wrist expansion - Hand deformities (boutonniere and Swan-neck)
Boutonniere vs Swan-neck deformity
- Boutonniere = hyperextension DIP, flexion of PIP- Swan-neck = hyperflexion DIP, extension of PIP
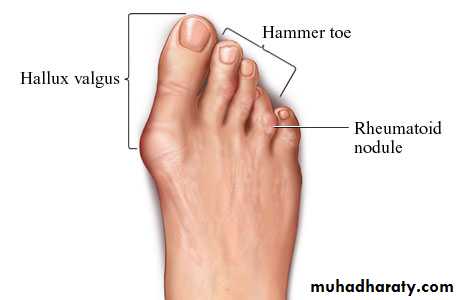
Extra-articular manifestation of RA
Rheumatoid Nodules = granulomas - implies severe diseaseSjogren's Syndrome = autoimmune exocrinopathy
Felty's Syndrome = leukopenia, splenomegaly
Vasculitis = purpura, cutaneous ulcers, and nail bed infarction
Interstitial lung disease
Cardiac Disease (pericardial effusion usually asymptomatic, valvular HD)
Neuoromyopathy = cervical spine instability, peripheral n. entrapment & mononeuritis multiplex
Eye = episcleritis, scleritis & scleromalacia perforance
Osteoporosis
Lymphadenopathy
Amyloidosis
Rheumatoid nodules
• Firm, non-tender, and round to oval; in the skin, they arise in the subcutaneous tissue.
Often found on elbow.
Always associated with sero-positive (RF +ve).Skin
Myelopathy in RA
spinal involvement rare except cervical!!!C1/C2 subluxation common
Severe neck pain often radiating to the occiput
Weakness in arms & legs
Dysesthesias of the fingers & feet
Jumping legs, due to spinal automatism
Disturbed bladder function
Sjogrens syndrome
Symptoms include dry eyes, dry mouth, vaginal dryness & tracheo-bronchial dryness (chornic cough)Primary Sjogren's syndrome is assoc iated with SS-A (Ro) & SS-B (La) antibodies
Treated with antiinflammatory & Immunosuppressive
Antibodies against exocrine glands
Can also affect liver, lung, many other organs
Test done to diagnose Sjogrens
- Schirmer's test = <5mm wetness = dry eyes
Lab findings in RA
*Most imp =Rheumatoid Factor
Anti - CCP AntibodyElevated ESR or CRP
*Non-specific findings =Anemia
Leukocytosis / thrombocytosisHyperglobulinemia
Positive ANA
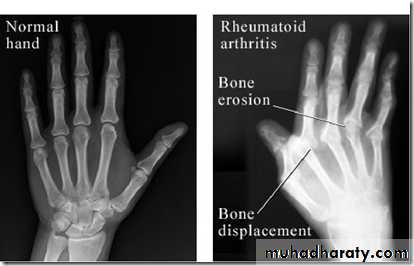
Radiological findings
ACR 1987 Classification Criteria
StiffnessInflammatory arthritis
3 or more joints
wrist (MCP PIP)
Symmetric arthritis
Rheumatoid nodules
Serum rheumatoid factor
Radiographic changes typical of RA
Criteria 1-4 of these present for 6 weeks or more.
Any 4 = RA
2010 RA Classification Criteria
Class criteria for RA (score based algorithm: add A-D): *A score > 6/10 = definite RA**A) Joint involvement1 large joint = 12-10 large joints = 21-3 small joints = 24-10 small joints = 3> 10 joints (at least 1 sm) = 5B) 3 points can come from lab values = Serology-low pos RF or low pos aCCP = 2-high pos RF or high pos aCCP = 3C) Acute phase reactantsabn CRP or ESR = 1 D) Duration of symptoms>6 weeks = 1
Case History, Cont…
Ms. JA, 47-yr-oldSymmetrical polyarthritis
Arthritis of small joints of the hand
- Morning stiffness
- High CRP
- Positive RF
The clinical diagnosis was early rheumatoid arthritis
Treatment of RA
Disease activityDisability
Structural damage
Reduce
DecreasePrevent
Traditional objectives of treatment in RAAdapted from: van der Heijde D. Ann Rheum Dis. 2001;60:iii47-iii50
Rationale for Early Treatment of RA
• Diagnose and treat early in the course of RA• Apply tight control = regular, protocol-driven review
• Initiate aggressive treatment in patients with poor prognosis
EARLY remission =
less disease progression
less disability
less comorbidity
increased productivity
Non-pharmacologic Treatment for RA
Patient education = most important
Rest, exercise, heat and cold, splints, weight lossPharmacologic Treatment for RA
NSAIDs = used for pain but do NOT halt disease progression- efficacy/toxicity leads to frequent switchingCorticosteroids
- symptomatic relief, and slows progress- adverse effects on long term use
- only used for short time; doesn't halt disease progression
DMARDs = major drugs
- reduce or prevent joint damage and preserve joint integrity - delayed onset of action- need cont monitoring
Analgesics- absolutely necessary to control pain.
Disease modifying anti-rheumatic drugs
Conventional DMARDS:Gold standard = Methotrexate
Others = Lefluonomide, Sulphasalazine, Hydroxychloroquine
Pros of methotrexate
Once a wk dosingLong-term clinical experience
Favorable rate of continuing therapy
Proven efficacy in moderate – severe RA
Cons of methotrexate
Lab monitoring every 4-8 wks CBC, LFTs, CreatinineToxicities: hepatic, myelosuppression, pulmonary
SE = nausea
C/I in pregnancy
Methotrexate (7.5 – 25 mg / wk) is given with...
FOLIC ACID (helps with SEs)Central role of TNF in the pathogenesis of RA
Brennan FM & McInnes IB. J. Clin Invest 2008;118: 3537-45.Biologic Therapies in RA
Made a big difference in treatment of RA
TNF-alpha inhibitors:
Soluble TNF receptor (etanercept)
Monoclonal TNF-alpha (infliximab)
Human monoclonal anti TNF (adalimumab)
Toxicities of anti-TNF:
Increased risk of infectionReactivating latent TB
Neoplasia
Multiple sclerosis
Autoimmune Disease
**Must check TB and Hep B first before prescribing.
Other biologics:Interleukin1 Ra (anakinra)
B cell depleting (rituximab)T cell inhibitors (abatacept)
Anti Interleukin-6 receptor Ab (Tocilizumab)
Other Treatments
Small molecule synthetic DMARDs = JAK 3 inhibitor (Tofacitinib)
Inhibits intracellulr signaling
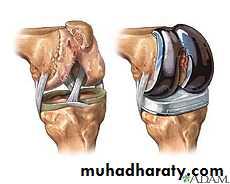
Surgical TreatmentSurgical procedures:
Arthrodesis
Total joints replacementCase History, Cont…
Ms. JA, 47-yr-oldThe clinical diagnosis was early rheumatoid arthritis.
What are the lines of treatment?
Managing RA in 2015: reviewConfirm the diagnosis
Define extent of joint involvement
Define extra-articular involvement
Consider co-morbid disease
Full dose NSAID
Early use of a DMARD
Add a Biologic Agent
Low dose steroids - flares/bridge
Adequate pain management
Frequently monitor progress & toxicity