1
URINALYSIS
• The urinalysis is a fundamental test that should be performed in all
urologic patients
• A complete urinalysis includes both chemical and microscopic
analyses.
Reasons for inadequate urinalyses include
(1) Improper collection,
(2) Failure to examine the specimen immediately,
(3) Incomplete examination (eg, most laboratories do not perform a
microscopic analysis unless it is specifically requested by the
provider),
(4) Inexperience of the examiner, and
(5) Inadequate appreciation of the significance of the findings.
Collection of Urinary Specimens
• In the male patient, a midstream urine sample is obtained
• The four aliquots have been designated Voided Bladder 1, Voided
Bladder 2, Expressed Prostatic Secretions, and Voided Bladder 3 (VB1,
VB2, EPS, and VB3)
• To evaluate for a possible infection in a female, a catheterized urine
sample should always be obtained.
• All urine samples should be examined within 1 hour of collection and
plated for culture and sensitivity if indicated for Neonates and Infants
Physical Examination of Urine
• The physical examination of the urine includes an evaluation of color,
turbidity, specific gravity and osmolality, and pH.
Color
• The normal pale yellow color of urine is due to the presence of the
pigment urochrome
• Urine color varies most commonly because of concentration, but
many foods, medications, metabolic products, and infection may
produce abnormal urine color.
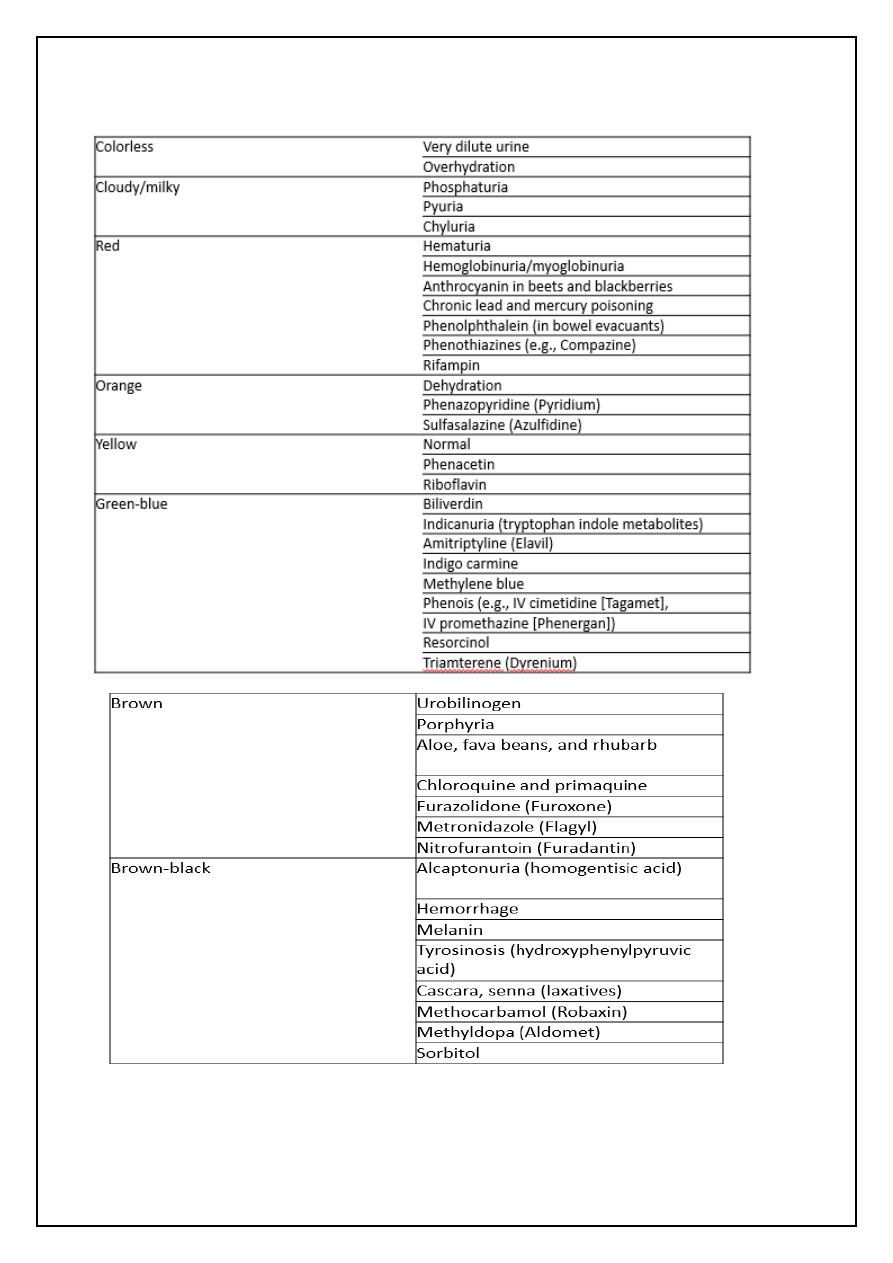
2
Common Causes of Abnormal Urine Color
3
Turbidity
• Cloudy urine is most commonly due to phosphaturia
• The large numbers of white blood cells cause the urine to become
turbid.
• Pyuria is readily distinguished from phosphaturia either by smelling
the urine (infected urine has a characteristic pungent odor)
• Rare causes of cloudy urine include chyluria (in which there is an
abnormal communication between the lymphatic system and the
urinary tract resulting in lymph fluid being mixed with urine),
lipiduria, hyperoxaluria, and hyperuricosuria.
Specific Gravity and Osmolality
• Specific gravity of urine is easily determined from a urinary dipstick
and usually varies from 1.001 to 1.035.
• A specific gravity less than 1.008 is regarded as dilute, and a specific
gravity greater than 1.020 is considered concentrated
• Conditions that decrease specific gravity include --
(1) increased fluid intake,
(2) diuretics,
(3) decreased renal concentrating ability, and
(4) diabetes insipidus.
• Conditions that increase specific gravity include--
(1) decreased fluid intake;
(2) dehydration owing to fever, sweating, vomiting, and diarrhea;
(3) diabetes mellitus (glucosuria); and
(4) inappropriate secretion of antidiuretic hormone.
• Osmolality is a measure of the amount of material dissolved in the
urine and usually varies between 50 and 1200 mOsm/L.
4
pH
• Urinary pH is measured with a dipstick test strip( methyl red and
bromothymol blue), which yield clearly distinguishable colors over
the pH range from 5 to 9.
• Urinary pH may vary from 4.5 to 8;
• The average pH varies between 5.5 and 6.5.
• A urinary pH between 4.5 and 5.5 is considered acidic, whereas a pH
between 6.5 and 8 is considered alkaline.
• In patients with a presumed UTI, an alkaline urine with a pH greater
than 7.5 suggests infection with a urea-splitting organism, most
commonly Proteus.
• Urinary pH is usually acidic in patients with uric acid and cystine
lithiasis.
• Alkalinization of the urine is an important feature of therapy in both
of these conditions
Chemical Examination of Urine
• Urine dipsticks provide a quick and inexpensive method for detecting
abnormal substances within the urine
• The abnormal substances commonly tested for with a dipstick include
(1) blood,
(2) protein,
(3) glucose,
(4) ketones,
(5) urobilinogen and bilirubin, and
(6) white blood cells.
Hematuria
• Normal urine should contain less than three red blood cells per HPF.
• A positive dipstick for blood in the urine indicates either hematuria,
hemoglobinuria, or myoglobinuria.
• The chemical detection of blood in the urine is based on the
peroxidase-like activity of hemoglobin
5
• Hematuria can be distinguished from hemoglobinuria and
myoglobinuria by microscopic examination of the centrifuged urine;
• The presence of a large number of erythrocytes establishes the
diagnosis of hematuria.
• If erythrocytes are absent, examination of the serum will distinguish
hemoglobinuria and myoglobinuria
Differential Diagnosis and Evaluation of Hematuria.
• Hematuria may reflect either significant nephrologic or urologic
disease
• Hematuria of nephrologic origin is frequently associated with casts in
the urine and almost always associated with significant proteinuria.
• Even significant hematuria of urologic origin will not elevate the
protein concentration in the urine into the 100 to 300 mg/dL or 2+ to
3+ range on dipstick.
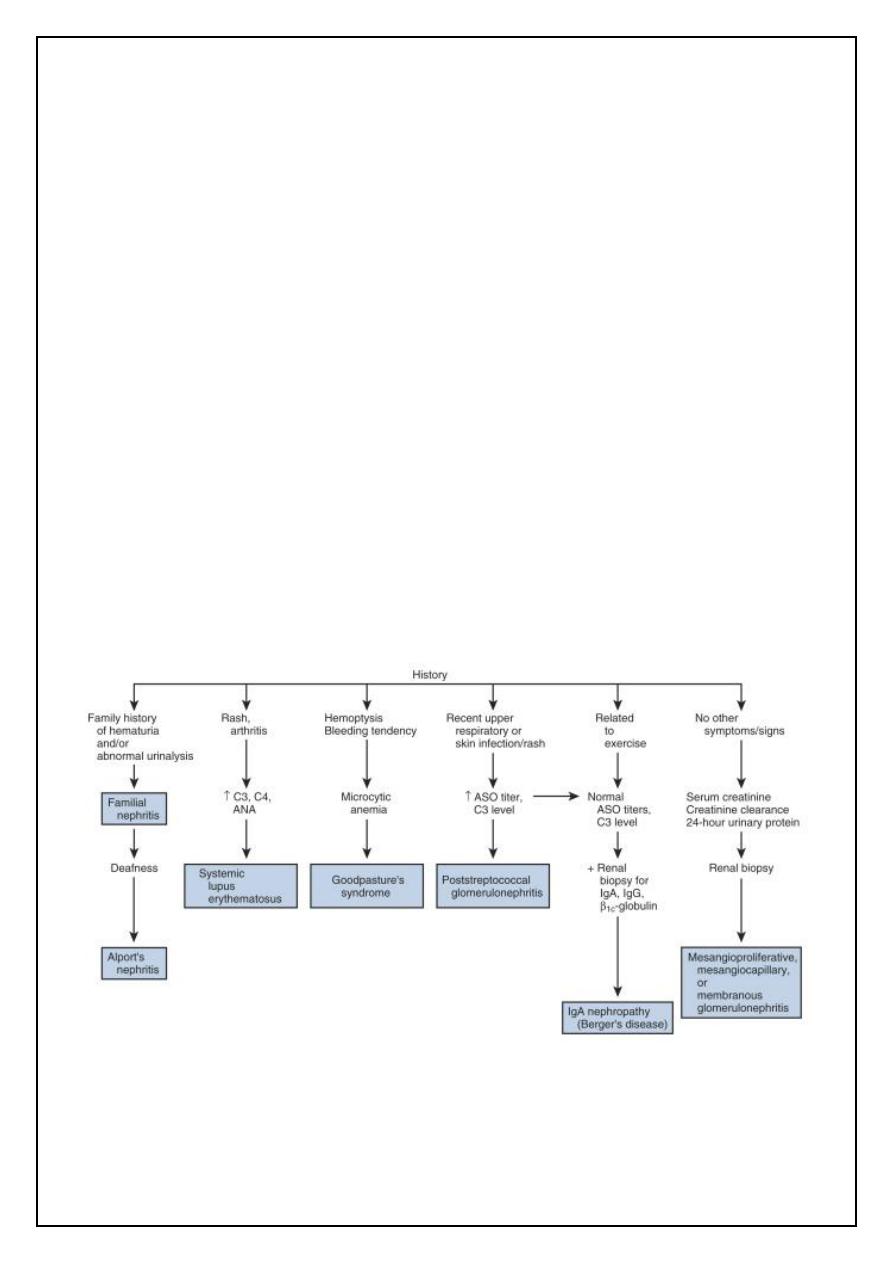
Evaluation of glomerular hematuria (dysmorphic erythrocytes, erythrocyte casts, and
proteinuria). ANA, antinuclear antibody; ASO, antistreptolysin O; Ig, immunoglobulin.
6
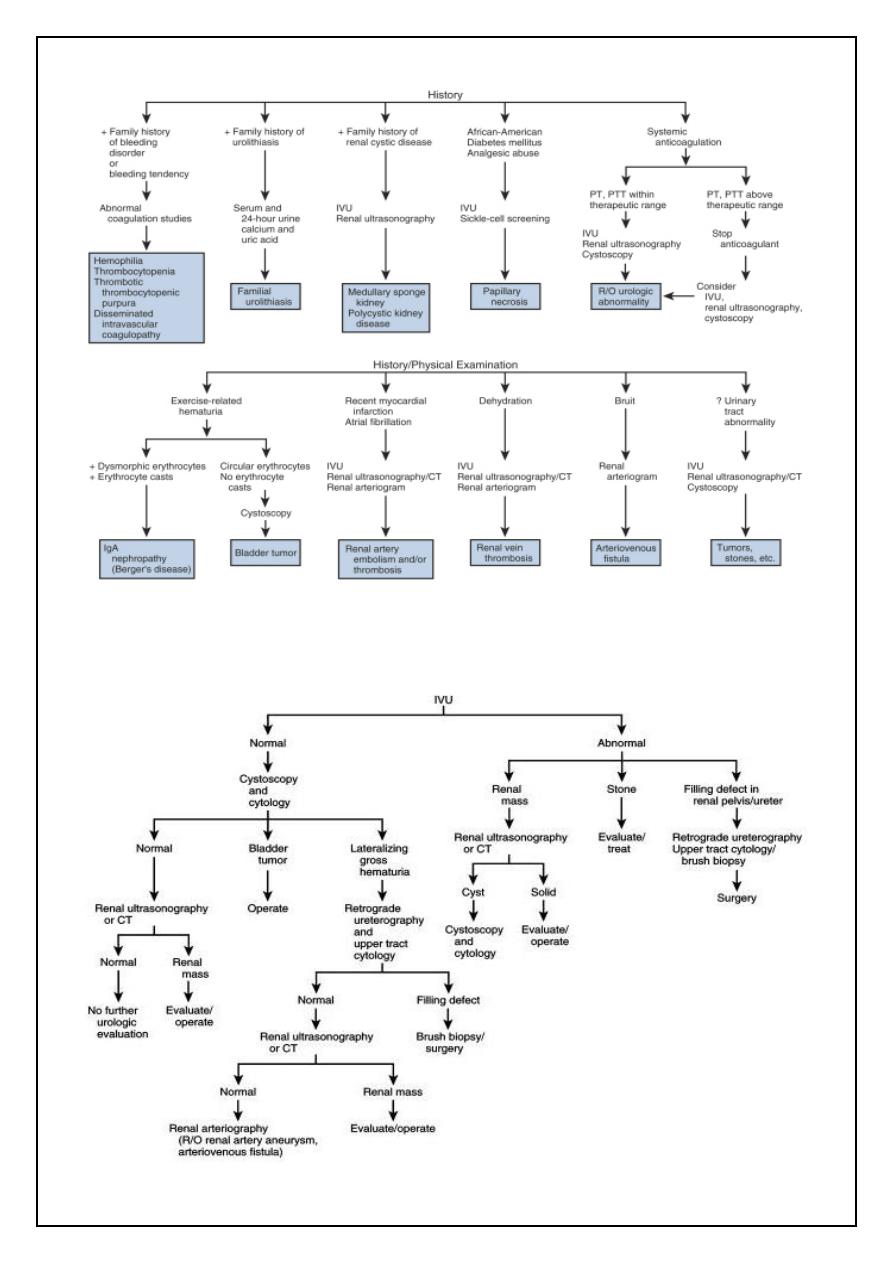
Evaluation of nonglomerular renal hematuria (circular erythrocytes, no erythrocyte
casts, and proteinuria). CT, computed tomography; IgA, immunoglobulin A; IVU,
intravenous urography; PT, prothrombin time; PTT, partial thromboplastin time;
Evaluation of essential hematuria (circular erythrocytes, no erythrocyte casts, no significant
proteinuria). CT, computed tomography; IVU, intravenous urography
7
Proteinuria
• Healthy adults excrete 80 to 150 mg of protein in the urine daily
• Proteinuria may be the first indication of renovascular, glomerular, or
tubulointerstitial renal disease, or it may represent the overflow of
abnormal proteins into the urine in conditions such as multiple
myeloma.
• Normally, urine protein is about 30% albumin, 30% serum globulins,
and 40% tissue proteins, of which the major component is Tamm-
Horsfall protein.
Glucose and Ketones
• Urine testing for glucose and ketones is useful in screening patients
for diabetes mellitus
• A serum glucose of about 180 mg/dL; above this level, glucose will be
detected in the urine.
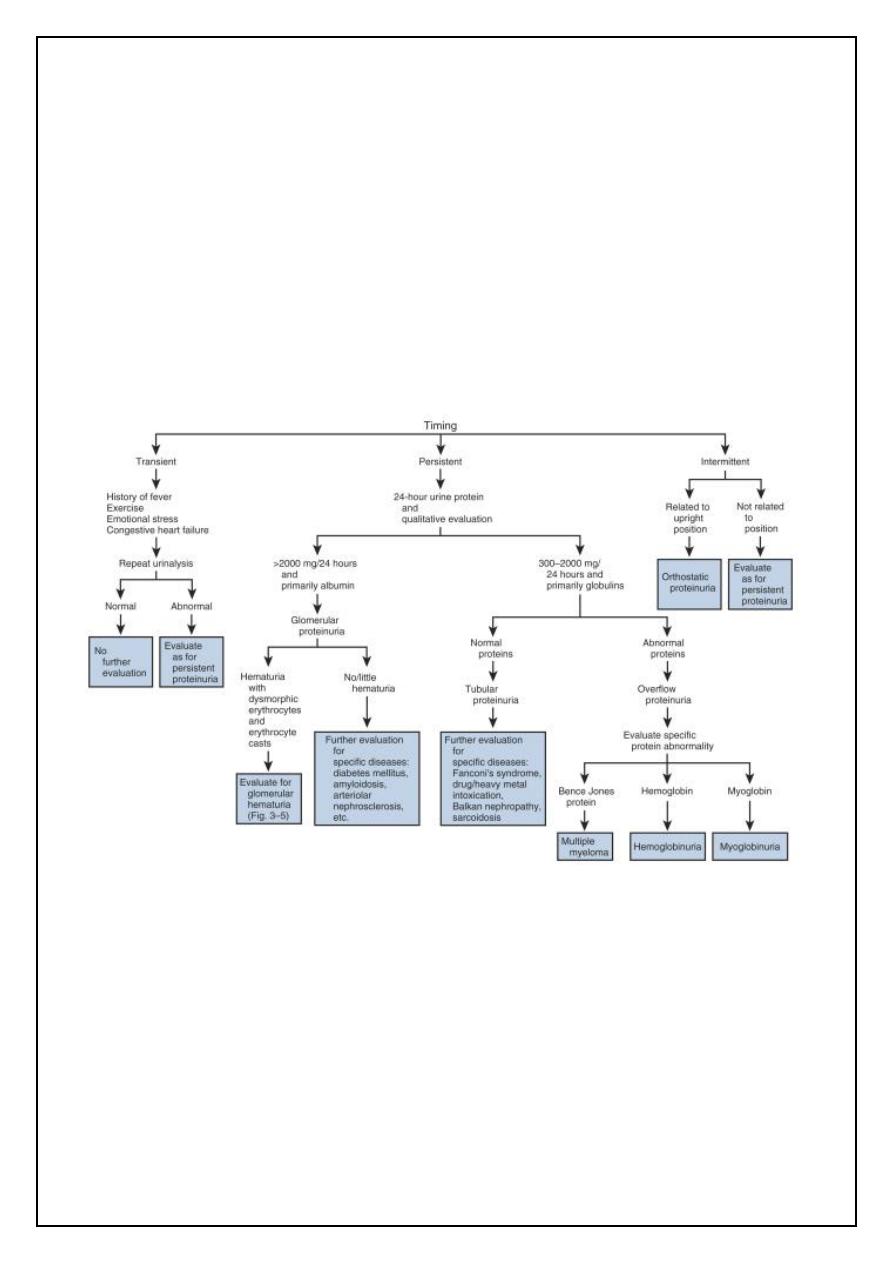
Evaluation of proteinuria.
8
• Ketones are not normally found in the urine but will appear when the
carbohydrate supplies in the body are depleted and body fat
breakdown occurs
• Ketones excreted include acetoacetic acid, acetone, and β-
hydroxybutyric acid. With abnormal fat breakdown, ketones will
appear in the urine before the serum.
Bilirubin and Urobilinogen
• Normal urine contains no bilirubin and only very small amounts of
urobilinogen
• Conjugated bilirubin has a low molecular weight, is water soluble, and
normally passes from the liver into the small intestine through the
bile ducts, where it is converted to urobilinogen.
• Therefore, conjugated bilirubin does not appear in the urine except
in pathologic conditions in which there is intrinsic hepatic disease or
obstruction of the bile ducts.
• Indirect bilirubin is of high molecular weight and bound in the serum
to albumin. It is water insoluble and, therefore, does not appear in
the urine even in pathologic conditions.
• Urobilinogen is the end product of conjugated bilirubin metabolism.
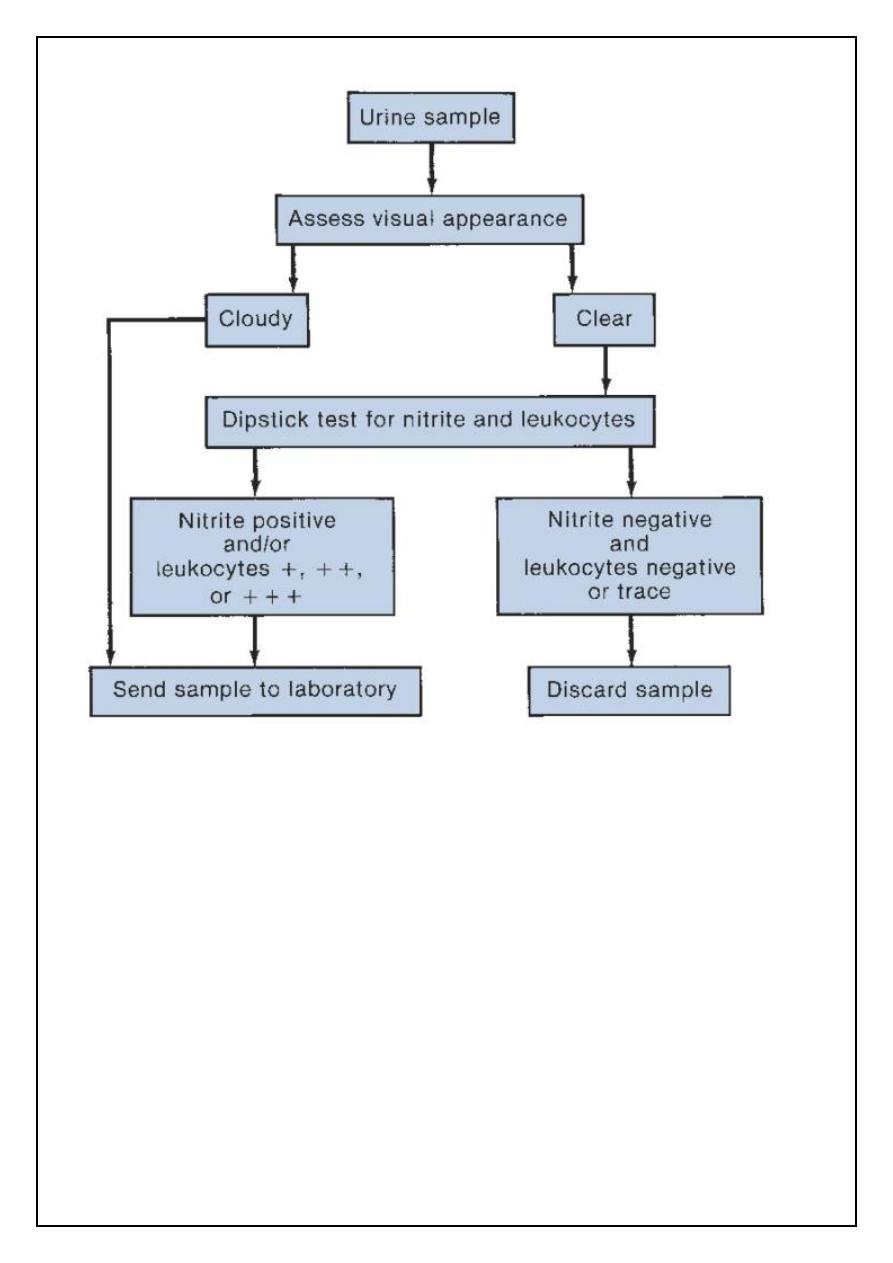
Leukocyte Esterase and Nitrite Tests
• Leukocyte esterase activity indicates the presence of white blood
cells in the urine.
• The presence of nitrites in the urine is strongly suggestive of
bacteriuria
• The major cause of false-positive leukocyte esterase tests is specimen
contamination
• Nitrites are not normally found in the urine, but many species of
gram-negative bacteria can convert nitrates to nitrites
9
Microscopy Technique
• Low-power magnification is sufficient to identify erythrocytes,
leukocytes, casts, cystine crystals, oval fat macrophages, and
parasites such as Trichomonas vaginalis and Schistosoma
hematobium.
• High-power magnification is necessary to distinguish circular from
dysmorphic erythrocytes, to identify other types of crystals, and,
particularly, to identify bacteria and yeast
• The urinary sediment should be examined microscopically for (1)
cells, (2) casts, (3) crystals, (4) bacteria, (5) yeast, and (6) parasites
Protocol for determining the need for urine sediment microscopy
in an asymptomatic population
11
Cells
1- Erythrocyte
Morphology may be determined under high power magnification
2- Leukocyte
Can generally be identify under low power and definitive diagnosed under
high power magnification. It is normal 1 or 2 leukocytes/HPF in men and
up to 5/HPF in women in whow urine sample may be contaminated with
vaginal secrestions. A great number of leukocyte generally indicates
infection or inflammation in the urinary tract.
3- Epithelial cells :
Epithelial cells are commonly observed in the urinary sediment. Squamous
cells are frequently detected in female urine specimens and are derived
from the lower portion of the urethra, the trigone of postpubertal females,
and the vagina. Squamous epithelial cells are large, have a central
small nucleus about the size of an erythrocyte, and have an irregular
cytoplasm with fine granularity.
Transitional epithelial cells may arise from the remainder of the urinary
tract .Transitional cells are smaller than squamous cells, have a larger
nucleus, and demonstrate prominent cytoplasmic granules near the
nucleus. Malignant transitional cells have altered nuclear size and
morphology and can be identified with either routine Papanicolaou
staining or automated flow cytometry.
4- Renal tubular cells
are the least commonly observed epithelial cells in the urine but are most
significant, because their presence in the urine is always indicative of renal
pathology. Renal tubular cells may be difficult to distinguish from
leukocytes, but they are slightly larger
11
Casts
• Tamm-Horsfall mucoprotein is the basic matrix of all renal casts; it
originates from tubular epithelial cells and is always present in the
urine
• When the casts contain only mucoproteins, they are called hyaline
casts and may not have any pathologic significance.
• Red blood cell casts contain entrapped erythrocytes and are
diagnostic of glomerular bleeding, most likely secondary to
glomerulonephritis
• White blood cell casts are observed in acute glomerulonephritis,
acute pyelonephritis, and acute tubulointerstitial nephritis
• Granular and waxy casts result from further degeneration of cellular
elements.
• Fatty casts are seen in nephrotic syndrome, lipiduria, and
hypothyroidism.
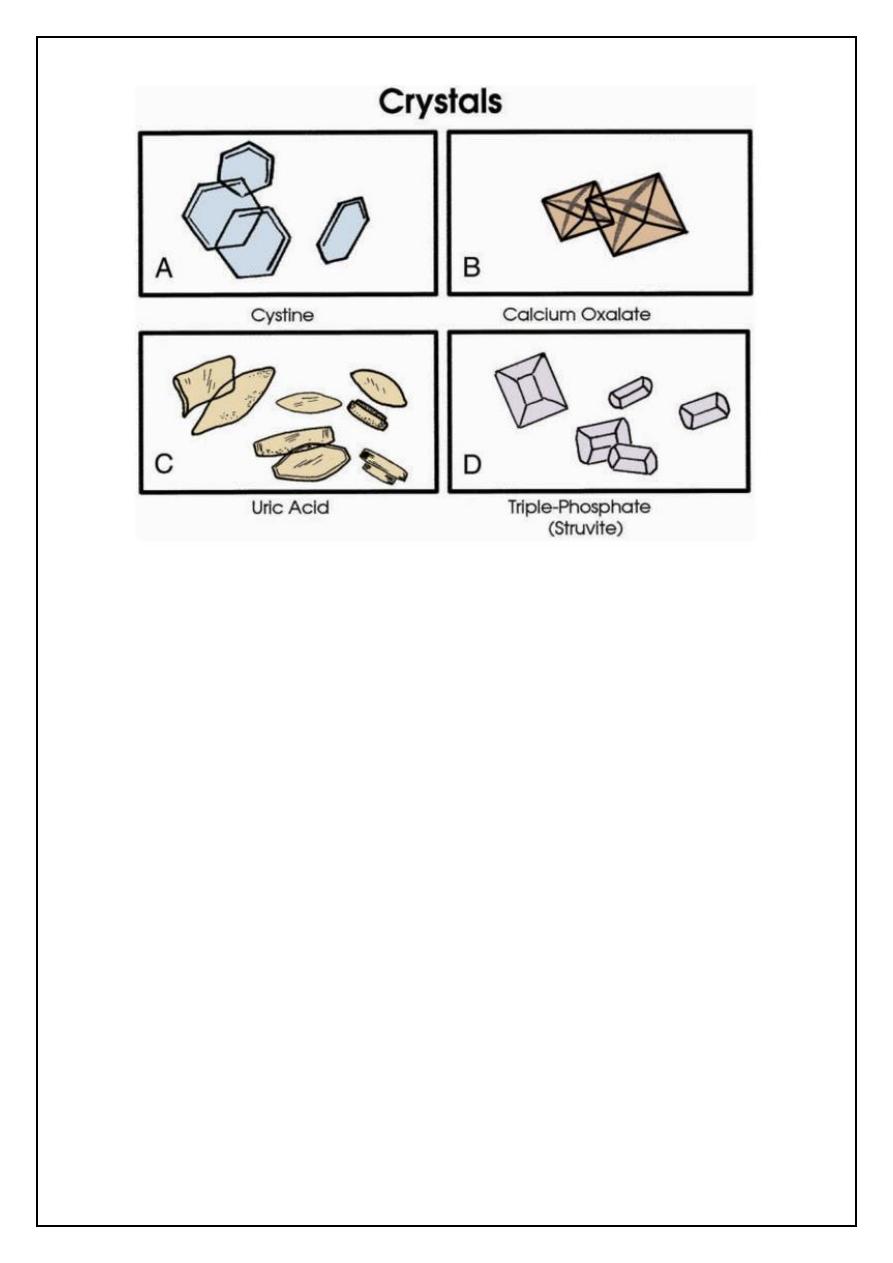
Crystals
• Identification of crystals in the urine is particularly important in
patients with stone disease
• The identification of cystine crystals establishes the diagnosis of
cystinuria
• Crystals precipitated in acidic urine include calcium oxalate, uric acid,
and cystine.
• Crystals precipitated in an alkaline urine include calcium phosphate
and triple-phosphate (struvite) crystals.
12
Bacteria
• Normal urine should not contain bacteria.
• In a fresh uncontaminated specimen, the finding of bacteria is
indicative of a UTI.
• Because each HPF views between 1/20,000 and 1/50,000 mL, each
bacterium seen per HPF signifies a bacterial count of more than
20,000/mL.
• Therefore, 5 bacteria/HPF reflects colony counts of about
100,000/mL.
Yeast
• The most common yeast cells found in urine are Candida albicans
• Yeasts are most commonly seen in the urine of patients with diabetes
mellitus or as contaminants in women with vaginal candidiasis.
Parasites
• Trichomonas vaginalis is a frequent cause of vaginitis in women and
occasionally of urethritis in men
Alzaidi
