BLADDER CARCINOMAS
Incidence:
• Bladder cancer is the second most common
cancer of the genitourinary tract.
• The incidence is higher in whites than in
African Americans.
• The average age at diagnosis is 65 years. At
that time, approximately 75% of bladder
cancers are localized to the bladder; 25%
have spread to regional lymph nodes or
distant sites.
Risk Factors & Pathogenesis
1-Cigarette smoking:
accounts for 50% of cases
in men and 31% in women
• smokers have approximately a 2-to-5 fold
increased risk of bladder cancer than
nonsmokers.
• The causative agents are thought to be alpha-
and beta-naphthylamine, which are secreted
into the urine of smokers.
• 2-Occupational exposure:
• Workers in the chemical, dye, rubber,
petroleum, leather, and printing industries are
at increased risk.
• Specific occupational carcinogens include
benzidine, betanaphthylamine, and 4-
aminobiphenyl, and the latency period
between exposure and tumor development
may be prolonged.

• 3-Gender:
men are 2.5 times more likely to
develop the disease than women,the cause
are unclear but may be associated with
greater urine residuals in the blaader.
• 4-Race:
black people have alower incidence
than white people but it carry apoorer
prognosis.
• 5-Chronic inflammation:
bladder
inflammation,stones,long term catheters,ova
of shistosoma haematobium(bilharziasis)are
implicated in the development of sequamous
cell carcinoma of bladder.
• 6-Druges:
phenacitin and cyclophosphamide.
• 7-Pelvic radiotherapy.

• The exact genetic events
leading to the
development of bladder cancer are unknown, but
they are likely to be multiple and may involve the
activation of oncogenes and inactivation or loss
of tumor suppressor genes.
*Loss of genetic material on chromosome 9.
*p53 tumor suppressor gene mutations.
*Deletion of Chromosome 11p, which contains the
c-Ha-ras proto-oncogene.
*Deletions of chromosome 17p.

STAGING
• Tis
--- carcinoma in situ.
• Ta
--- intraepithelial tumour.
• T1
--- tumour involve the lamina properia.
• T2a
--- tumour reach the superfecial layer of
detrusal muscle.
• T2b
--- tumour involve deep layer of detrusal
muscle.
• T3a
---microscopic invasion of perivesical tissue.

• T3b
--- macroscopic invasion of perivesical
tissue.
• T4a
---invasion of prostate,uterus,vagina.
• T4b
---invasion of pelvic wall,abdominal wall.

• The normal urothelium is composed of 3–7 layers
of transitional cell epithelium resting on a
basement membrane composed of extracellular
matrix (collagen, adhesive
glycoproteins,glycosaminoglycans).
• The muscle wall of the bladder is composed of
muscle bundles coursing in multiple directions. As
these converge near the bladder neck, 3 layers
can be recognized: inner and outer longitudinally
oriented layers and a middle circularly oriented
layer.

Histopathology
• Ninety-eight percent
of all bladder cancers are
epithelial malignancies, with most being
transitional cell carcinomas.
• The World Health Organization recognizes a
papilloma as a papillary tumor with a fine
fibrovascular stalk supporting an epithelial layer
of transitional cells with normal thickness and
cytology.
• Papillomas are a rare benign condition usually
occurring in younger patients.

TRANSITIONAL CELL CARCINOMA
• Approximately 90%
of all bladder cancers are
TCCs.
• These tumors most commonly appear as
papillary, exophytic lesions; less commonly,
they may be sessile or ulcerated.
• Carcinoma in situ (CIS)
is recognizable as flat,
anaplastic epithelium.
NONTRANSITIONAL CELL
CARCINOMAS
• 1. Adenocarcinoma:
• Adenocarcinomas account for <2% of all
bladder cancers. Primary adenocarcinomas of
the bladder may be preceded by cystitis and
metaplasia.
• adenocarcinomas arising from the urachus
occur at the dome.
• Five-year survival is usually <40%, despite
aggressive surgical management.
• 2. Squamous cell carcinoma:
• Squamous cell carcinoma accounts for
between 5% and 10% of all bladder cancers.
• It is associated with a history of chronic
infection, vesical calculi, or chronic catheter
use. It may also be associated with bilharzial
infection.
• These tumors are often nodular and invasive
at the time of diagnosis.
• 3. Undifferentiated carcinomas:
• are rare tumour type (accounting for <2%).
• 4. Mixed carcinoma:
Mixed carcinomas constitute
4– 6% of all bladder cancers and are composed of
a combination of transitional, glandular,
squamous, or undifferentiated patterns.
• The most common type comprises transitional
and squamous cell elements .
• Most mixed carcinomas are large and infiltrating
at the time of diagnosis.

RARE EPITHELIAL & NONEPITHELIAL
CANCERS
• Rare epithelial carcinomas
identified in the
bladder include villous adenomas, carcinoid
tumors, carcinosarcomas, and melanomas.
• Rare nonepithelial cancers
of the urinary
bladder include pheochromocytomas,
lymphomas, choriocarcinomas, and various
mesenchymal tumors (hemangioma,
osteogenic sarcoma, and myosarcoma).

Clinical Findings
• A. SYMPTOMS:
• 1-Hematuria is the presenting symptom in 85–
90% of patients with bladder cancer. It may be
gross or microscopic, intermittent rather than
constant.
• 2-Irritative voiding symptoms seem to be
more common in patients with diffuse CIS.
• 3-Pain:is unusual(e.g obstructive uropathy).

• 4-Recurrent UTI &pneumaturia due to
malignant colovesical fistula.
• 5-More advanced cases may presented with
lower limb sweeling(due to lymphatic or
venous obstruction),bone pain,weight
loss,anorexia,confusion&anuria.
• 6-Urachal adenocarcinoma may presented
with umbilical discharge mucous or bloody,or
presented with deep umbilical mass.
• B. SIGNS:
• 1-General examination may reveal
pallor,indicating anemia due to blood loss or
chronic renal impairment.
• 2-palpable mass due to large-volume or invasive
bladder tumors.
• 3-Hepatomegaly and supraclavicular
lymphadenopathy are signs of metastatic disease.
• 4-Lymphedema from occlusive pelvic
lymphadenopathy may be seen occasionally.

C. LABORATORY FINDINGS
1. Routine testing:
• The most common laboratory abnormality is
hematuria.
• pyuria, which may result from concomitant
urinary tract infection.
• Azotemia may be noted in patients with ureteral
occlusion.
• Anemia may be a presenting symptom owing to
chronic blood loss, or replacement of the bone
marrow with metastatic disease.

• 2. Urinary cytology:
• Exfoliated cells from both normal and neoplastic
urothelium can be readily identified in voided
urine.
• Cytologic examination of exfoliated cells may be
especially useful in detecting cancer in
symptomatic patients and assessing response to
treatment. Detection rates are high for tumors of
high grade and stage as well as CIS but not as
impressive for low grade superficial tumors.

3-Tumour markers:
• BTA
• NMP22
• Lewis X antigen
• Telomeras
• Hyaluronidase.
• These tests have been demonstrated to enhance
detection of bladder cancer when used either
individually or in combination with cytology.

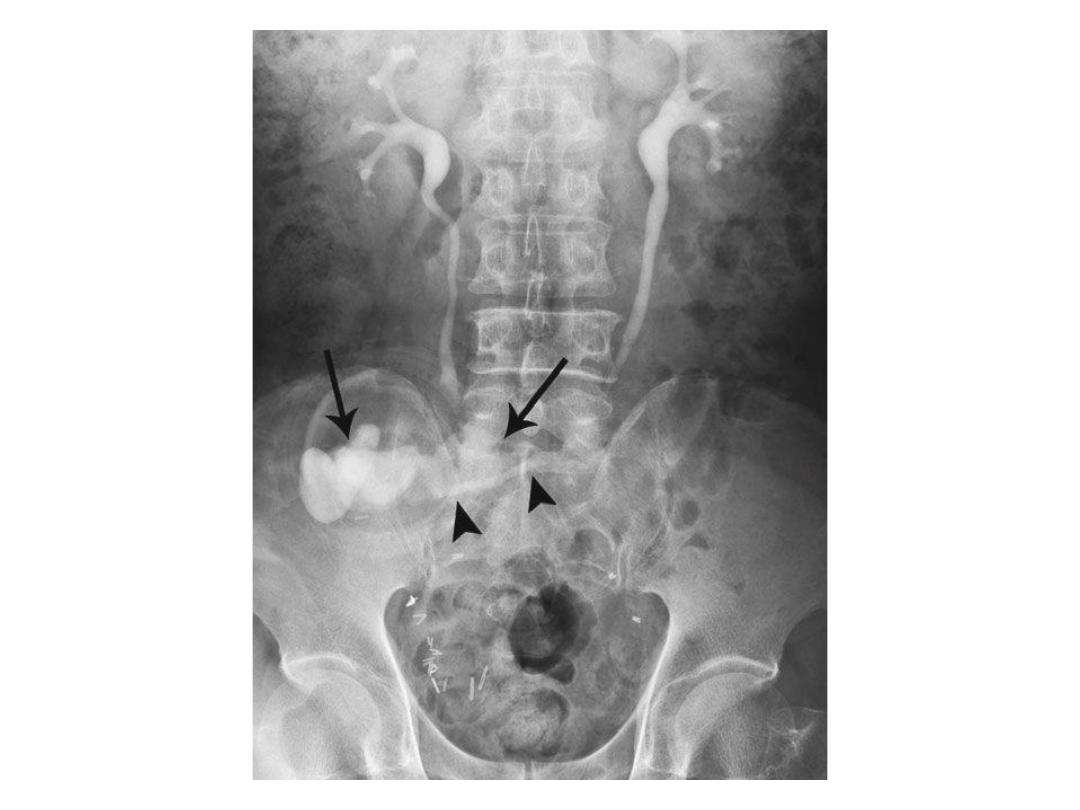
D. IMAGING
• Although bladder cancers may be detected by
various imaging techniques, their presence is
confirmed by cystoscopy and biopsy.
• Intravenous urography remains one of the most
common imaging tests for the evaluation of
hematuria.
• computed tomography (CT) urography, which is
more accurate, for evaluation of the entire
abdominal cavity, renal parenchyma, and ureters
in patients with hematuria

• Hydronephrosis from ureteral obstruction is
usually associated with deeply infiltrating
lesions and poor outcome after treatment.
• CT and magnetic resonance imaging (MRI)
have been used to characterize the extent of
bladder wall invasion and detect enlarged
pelvic lymph node. With overall staging
accuracy ranging from 40% to 85% for CT and
from 50% to 90% for MRI.

E. CYSTOURETHROSCOPY & TUMOR
RESECTION
• The diagnosis and initial staging of bladder
cancer is made by cystoscopy and
transurethral resection (TUR).
• Cystoscopy can be done with either flexible or
rigid instruments.
• Once a tumor is visualized or suspected, the
patient is scheduled for examination under
anesthesia and TUR or biopsy of the
suspicious lesion.

Treatment
• At initial presentation, approximately 50–70%
of bladder tumors are superficial—stage Tis or
Ta.
• regional or distant metastases are found in
approximately 25%.
• Unfortunately, 80% of patients with invasive
or metastatic disease have no previous history
of bladder cancer.

Initial Treatment Options for
Bladder Cancers
• Tis---
Complete TUR followed by intravesical BCG.
• Ta (single, low-to-moderate grade, not recurrent) ---
Complete TUR.
• Ta (large, multiple, highgrade, or recurrent)--
Complete TUR
followed by intravesical chemo- or immunotherapy
• T1 ---
Complete TUR followed by intravesical chemo- or
immunotherapy.
• T2–T4---
Radical cystectomy Neoadjuvant chemotherapy
followed by radical cystectomy Radical cystectomy followed
by adjuvant chemotherapy Neoadjuvant chemotherapy
followed by concomitant chemotherapy and irradiation
• Any T, N+, M+ ---
Systemic chemotherapy followed by
selective surgery or irradiation.

A. INTRAVESICAL CHEMOTHERAPY
• Immunotherapeutic or chemotherapeutic agents
can be instilled into the bladder directly via
catheter, thereby avoiding the morbidity of
systemic administration in most cases.
• Intravesical therapy can have a prophylactic or
therapeutic objective.
Adjunctive --
At TUR Prevent implantation.
Prophylactic--
After complete TUR Prevent or delay
recurrence or progression.
Therapeutic --
After incomplete TUR Cure residual
disease.

• The intravesical chemotherapy include:
1- Mitomycin C:
Mitomycin C is an antitumor,
antibiotic, alkylating agent that inhibits DNA
synthesis.
The usual dose is 40 mg in 40 cc of sterile water
or saline given once a week for 6 weeks.
• 2-Thiotepa:
Thiotepa is an alkylating agent.
Although various doses have been used, 30
mg weekly seems to be sufficient.

• 3-BCG:
BCG is an attenuated strain of
Mycobacterium bovis.
• The exact mechanism by which BCG exerts its
antitumor effect is unknown, but it seems to be
immunologically mediated.
• Mucosal ulceration and granuloma formation are
commonly seen after intravesical instillation.
Activated helper T lymphocytes can be identified
in the granulomas, and interleukin-2 reportedly
can be detected in the urine of treated patients.

• It appears to be the most efficacious
intravesical agent for the management of CIS.
• BCG has been shown to be superior to
intravesical chemotherapy in preventing
recurrence in patients with high-risk
superficial bladder cancer . Although BCG
appears to be effective in delaying progression
of high-risk superficial bladder cancer.
• The most commonly recommended induction
regimen for BCG is weekly for 6 weeks
followed by a period of 6 weeks where no BCG
is given.
• The optimal regimen for maintenance therapy
is also unclear. Published regimens involve 3
instillations once a week at 3- to 6-month
intervals for 3 years following TUR.
• Side effects:Most patients experience some
degree of urinary frequency ,urgency&
hemorrhagic Cystitis.
• Patients with mild systemic or moderate local
symptoms should be treated with isoniazid (300
mg daily) and pyridoxine (vitamin B6 50 mg/day),
and the dosage of BCG should be reduced.
Isoniazid is continued while symptoms persist
and restarted 1 day before the next instillation.

• Patients with severe systemic symptoms should have
Instillation stopped. Patients with prolonged high fever
(>103°F), symptomatic granulomatous prostatitis, or
evidence of systemic infection require treatment with
isoniazid and rifampin (600 mg daily).
• Patients with signs and symptoms of BCG sepsis (eg,
high fever, chills, confusion, hypotension, respiratory
failure, jaundice) should be treated with isoniazid,
rifampin, and ethambutol (1200 mg). The addition of
cycloserine (500 mg twice daily) or prednisolone (40
mg daily) increases survival rates

URETERAL & RENAL PELVIC CANCERS
• Carcinomas of the renal pelvis and ureter are
rare, accounting for only 4% of all urothelial
cancers
• Male female ratio is 2–4:1
• Patients with a single upper-tract carcinoma are
at risk of developing bladder carcinomas (30–
50%) and contralateral upper-tract carcinoma (2–
4%).
• Conversely, patients with primary bladder cancer
are at low risk (<2%) of developing upper urinary
tract

• As with bladder carcinoma, smoking and
exposure to certain industrial dyes or solvents
are associated with an increased risk of upper
urinary tract TCCs.
• Patients with carcinomas associated with
analgesic abuse are more likely to be women,
have higher stage disease, and be younger
than others.

• Balkan nephropathy is an interstitial
inflammatory disease of the kidneys that
affects Yugoslavians, Rumanians, Bulgarians,
and Greeks; associated upper-tract
carcinomas are generally superficial and more
likely to be bilateral.
• Thus, most renal pelvic and ureteral cancers
(90% and 97%, respectively) are TCCs.

• Squamous carcinomas account for
approximately 10%.
• Benign tumors include fibroepithelial polyps
(the most common), leiomyomas, and
angiomas.

SYMPTOMS AND SIGNS
• Gross hematuria is noted in 70–90% of patients.
• Flank pain, is the result of ureteral obstruction from blood clots or
tumor fragments, renal pelvic or ureteral obstruction by the tumor
itself, or regional invasion by the tumor.
• Irritative voiding symptoms are present in approximately 5–10% of
patients.
• Constitutional symptoms of anorexia, weight loss, and lethargy are
uncommon and are usually associated with metastatic disease.
• A flank mass owing to hydronephrosis or a large tumor , and flank
tenderness may be elicited as well.
• Supraclavicular or inguinal adenopathyor hepatomegaly may be
identified in a small percentage of patients with metastatic disease.

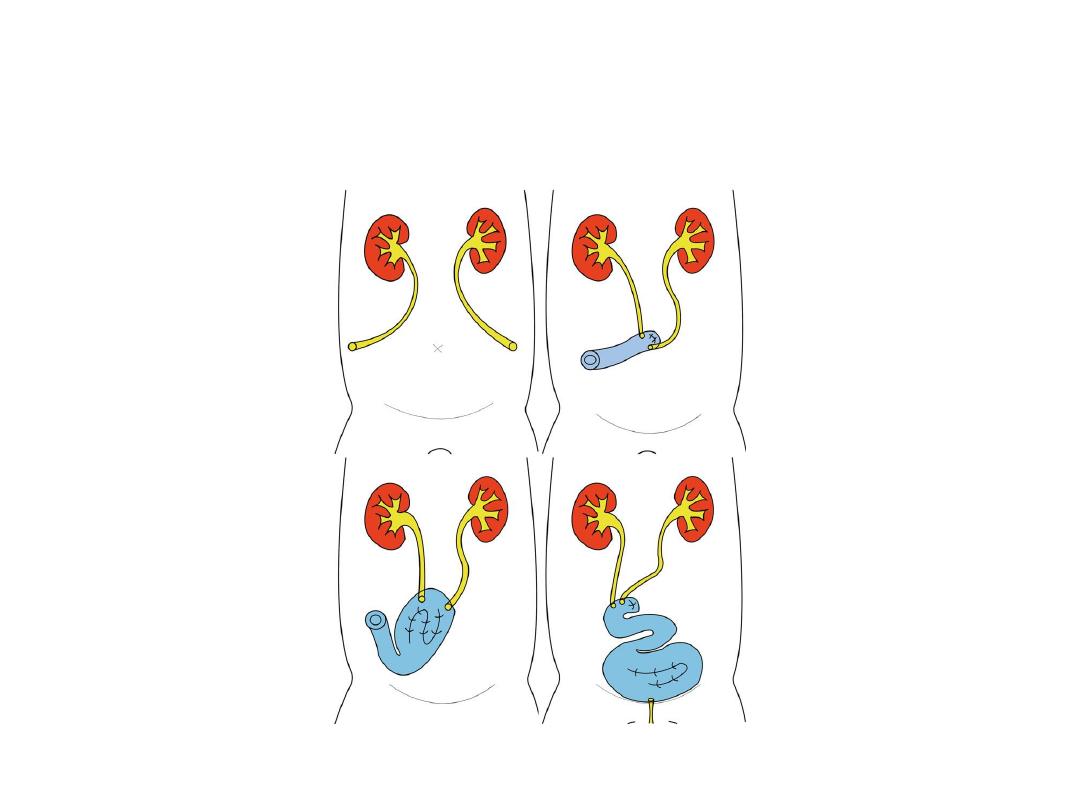
Treatment
• Treatment of renal pelvic and ureteral tumors
should be based primarily on grade, stage,
position, and multiplicity. Renal function and
anatomy should be assessed.
• The standard therapy for both tumor types
has been
nephroureterectomy with excision
of a bladder cuff.

• Indications for more conservative surgery,
including open or endoscopic excision, are not
well defined.
• Absolute indications for renal-sparing
procedures include tumor within the
collecting system of a single kidney and
bilateral urothelial tumors of the upper
urinary tract or in patients with 2 kidneys but
marginal renal function.