
Authors: Professor Baha Diaa Moohee Alosy,
Departments of Pediatrics- Collage of Medicine.
University of Tikrit -IRAQ.
Neonatal Infection & / or sepsis
Objectives
❖
identify the approach of
Neonatal Infection
❖
Identify clinical
manifestation of
Neonatal
Infection
❖
Know the treatment for
Neonatal Infection

Background
Neonatal sepsis may be categorized as early onset (day of life 0-3) or late onset (day
of life 4 or later). Of neorns with early-onset sepsis, 85% present within 24 hours
(median age of onset 6 hours), 5% present at 24-48 hours, and a smaller percentage
present within 48-72 hours. Onset is most rapid in premature neonates
.
Early-onset sepsis is associated with acquisition of microorganisms from the mother
is more common in early-onset sepsis, whereas
meningitis and
are more common in late-onset
sepsis. Early-onset sepsis is 10 to 20 times more likely to occur
in premature, very low birthweight infants.
Etiology
The microorganisms most commonly associated with early-
onset infection include the following
[1]
:
Group B Streptococcus (GBS)
Coagulase-negative Staphylococcus
Late-onset sepsis occurs at 4-90 days of life and is
acquired from the environment. Organisms that have
been implicated in late-onset sepsis include the
following:
•
Coagulase-negative Staphylococcus
•
E coli
•
Klebsiella
•
Enterobacter
•
Candida
•
GBS
•
Serratia
•
Acinetobacter
•
Anaerobes
Early-onset neonatal sepsis
Risk factors implicated in neonatal sepsis reflect the
level stress and illness experienced by the fetus at
delivery, as well as the hazardous uterine
environment surrounding the fetus before delivery.
The most common risk factors associated with early-
onset neonatal sepsis include, but are not limited to,
the following:
Maternal GBS colonization (particularly in the setting
of inadequate prophylactic treatment)
Premature rupture of membranes (PROM)
Preterm rupture of membranes
Prolonged rupture of membranes
Premature birth
Maternal urinary tract infection (UTI)
Maternal fever greater than 38ºC (100.4ºF)
Other factors that are associated with or predispose to
early-onset sepsis include the following :
Low Apgar score (< 6 at 1 or 5 minutes)
Poor prenatal care
Poor maternal nutrition
Low socioeconomic status
Black mother
History of recurrent abortion
Maternal substance abuse
Low birth weight
Difficult delivery
Birth asphyxia
Meconium staining
Congenital anomalies
•
Late-onset sepsis is associated with the
following risk factors
[20]
:
•
Prematurity
•
Central venous catheterization (duration >10
days)
•
Urinary catheterization
•
Chronic mechanical ventilation
•
Failure to advance enteral feeding
•
nasal cannula or continuous positive airway
pressure (CPAP)
•
Use of H
2
-receptor blocker or proton pump
inhibitor (PPI)
•
Gastointestinal tract pathology
•
Meningitis
•
The principal pathogens in neonatal meningitis
are GBS (36% of cases), E coli (31%),
and Listeria species (5%-10%). Other organisms
that may cause meningitis include the following:
•
S pneumoniae
•
S aureus
•
S epidermidis
•
H influenzae
•
Pseudomonas species
•
Klebsiella species
•
Serratia species
•
Enterobacter species
•
Proteus species
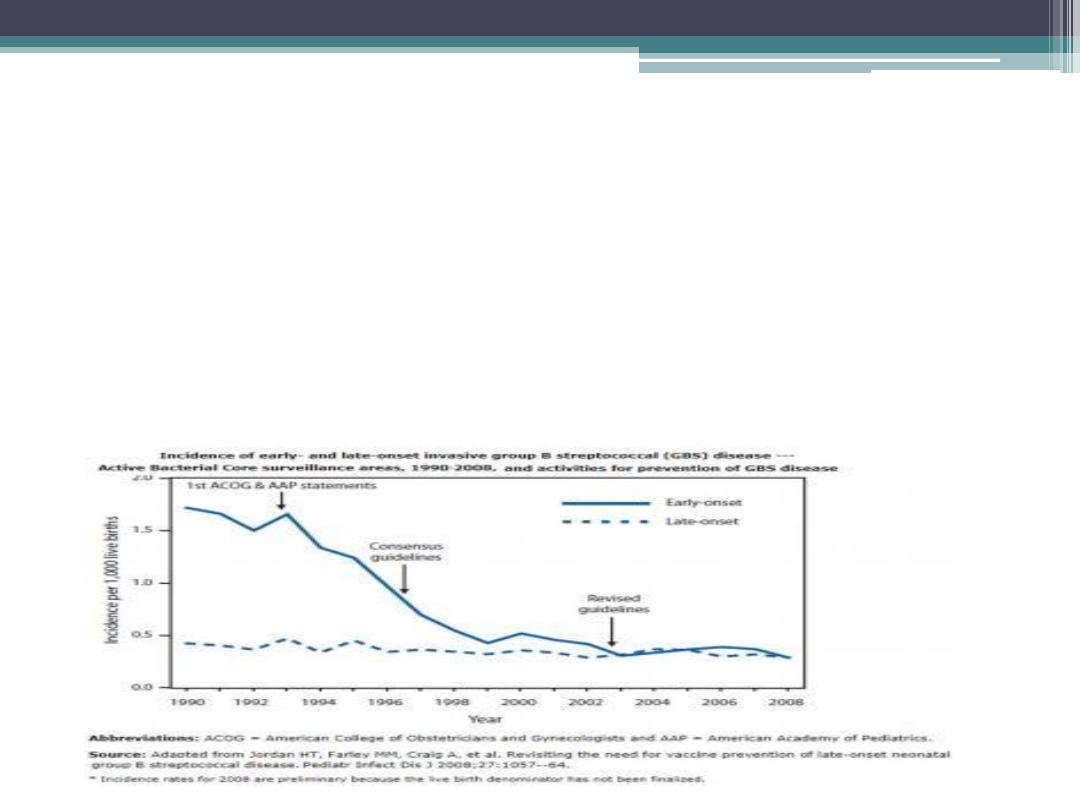
Epidemiology
•
The incidence of culture-proven early-onset
sepsis in the United States is approximately 0.3-2
per 1000 live births. Of the 7%-13% of neonates
who are evaluated for neonatal sepsis, only 3%-
8% of those screened will have culture-proven
sepsis.
Age-, race-, and sex-related demographics
•
Premature infants have an increased incidence of sepsis, with a
significantly higher occurrence in infants with a birth weight lower than
1500 g (11-22.7 per 1000 live births) than in infants born at 37 weeks or
later (0.3-0.98 per 1000 live births).
•
Black infants have an increased incidence of GBS disease and late-onset
sepsis. This is observed even after other risk factors such as low birth
weight and younger maternal age have been controlled
•
Prognosis
➢
With early diagnosis and treatment of neonatal sepsis, most term infants
will not experience associated long-term health problems. However, if
early signs or risk factors are missed, mortality increases. Residual
neurologic damage occurs in 15%-30% of neonates with septic meningitis.
➢
Mortality from neonatal sepsis may be as high as 50% for infants who are
not treated. Infection is a major cause of mortality during the first month
of life, contributing to 13%-15% of all neonatal deaths. Low birth weight
and gram-negative infection are associated with worse outcomes.
➢
Neonatal meningitis occurs in 2-4 cases per 10,000
live births and contributes significantly to mortality
from neonatal sepsis; it is responsible for 4% of all
neonatal deaths.
➢
In preterm infants who have had sepsis, impaired
neurodevelopment is a concern. Proinflammatory
molecules may negatively affect brain development
in this patient population. In a large study of 6093
premature infants who weighed less than 1000 g at
birth, preterm infants with sepsis who did not have
meningitis had higher rates of cerebral palsy (odds
ratio [OR] 1.4-1.7), developmental delay (OR 1.3-
1.6), and vision impairment (OR 1.3-2.2) as well as
other neurodevelopmental disabilities than infants
who did not have sepsis
Neonatal Sepsis Clinical Presentation
•
History
An awareness of the many risk factors associated
with neonatal sepsis prepares the clinician for
early identification and effective treatment,
thereby reducing morbidity and mortality.
Among these risk factors are the following:
•
Maternal group B Streptococcus (GBS) status
•
Prolonged and/or premature rupture of
membranes (PPROM)
•
Premature delivery
•
Chorioamnionitis
1.
Signs
1. Respiratory distress
(90%)
2. Apnea
4. Flaring or
grunting
5. Irregular
respirations
2. Temperature instability
sustained over 1 hour
(30%)
1. Newborn
Temperature < 97
F (36 C)
2. Newborn
Temperature >
99.6 F (37 C)
3. Gastrointestinal
symptoms
4. Neurologic
3. Tachycardia
1. Pallor or skin
or
3. Cold or clammy
1.
Labs
suggestive of
Count
1. Decreased
below 5000
/mm3
2. Increased
above
25000
/mm3
(ANC) < 1000
/mm3
3. Bands to total
ratio > 0.2
4. Immature to
mature
ratio > 0.2
(positive in 5-10% of
1. Indicated for
1. Indications
2. Specific Tests
1. Indicated for late-
perinatal period
(age <3 days old)
Differential Diagnoses
Hemolytic Disease of the Newborn
▪
Metabolic Disorders
Pediatric Congenital Diaphragmatic Hernia
Pediatric Congestive Heart Failure
•
Management: General
▫ Monitor infant for signs of
▫ Antibiotic indications (contrast
with observation only)
Symptomatic infants
Asymptomatic infants with
>2 risk factors (see above)
▫ Continue monitoring and
antibiotics for 48 to 72 hours
Indications to continue
antibiotics 14 to 21 days
Symptomatic newborn
positive
Discontinue antibiotics and
monitoring if
s negative at 48
to 72 hours and
No signs of
on
examination
▫ Signs of
with negative
culture
Consider
infection
•
Management: Antibiotics for
Early Onset (age <1 week)
▫ Bacterial spectrum
(not
common)
Listeria (rare in United
States)
▫ Primary Antibiotic Protocol
(
dose often used
empirically)
: 50 mg/kg/dose IV
or IM q12 hours
: 100
mg/kg/dose IV or IM q12
hours
Gestation <28 weeks: 2.5
mg/kg/dose IV/IM q24
hours
Gestation <34 weeks: 2.5
mg/kg/dose IV/IM q18
hours
Gestation >34 weeks: 2.5
mg/kg/dose IV/IM q12
hours
▫ Alternative Options
Alternative Protocol 1
(dosed as
above)
50
mg/kg/dose IV or IM q12
hours
Alternative Protocol 2
(dosed as
above)
50 mg/kg IV
or IM q24 hours
•
Management: Antibiotics
for Late Onset (age 1-4
weeks)
▫ Coverage broadened over
early onset
epidermidis
▫ )
▫ Antibiotic Dosing for infant over 7 days old
(the higher dose in possible
Weight <2 kg: 25-50 mg/kg/dose IV or IM q8 hours
Weight >2 kg: 25-50 mg/kg/dose IV or IM q6 hours
Gestation <37 weeks: 2.5 mg/kg/dose IV/IM q12 hours
Gestation >37 weeks: 2.5 mg/kg/dose IV/IM q8 hours
▫ Primary Protocol 1
(dosed as above)
50 mg/kg/dose IV or IM q8 hours
▫ Primary Protocol 2
(dosed as above)
75 mg/kg/dose IV or IM q24 hours
▫ Alternative Protocol
(dosed as above)
(dosed as above)
•
Prevention
Rupture of Membranes GBS Prophylaxis
▫ Routine Group B Strep Screening in pregnancy (36 weeks
1 )
Klinger G, Levy I, Sirota L, et al, for the Israel Neonatal Network. Epidemiology and risk factors for early onset sepsis among very -low-birthweight infants. Am J Obstet
Gynecol. 2009 Jul. 201 (1 ):38.e1-6.
2)
v an den Hoogen A, Gerards LJ, Verboon-Maciolek MA, Fleer A, Krediet TG. Long-term trends in the epidemiology of neonatal sepsis and antibiotic susceptibility of
causative agents. Neonatology. 2010. 97 (1):22-8.
3)
[Guideline] Verani JR, McGee L, Schrag SJ, for the Division of Bacterial Diseases, National Center for Im munization and Respiratory Diseases, Centers for Disease
Con trol and Prevention (CDC). Prevention of perinatal group B streptococcal disease--revised guidelines from CDC, 2010. MMWR Recomm Rep. 2010 Nov 19. 59 (RR-
1 0):1-36.
4)
Ber ardi A, Rossi C, Spada C, et al, for the GBS Prevention Working Group of Em ilia-Rom agna. Strategies for preventing early-onset sepsis and for managing neonates at-
r isk: wide variability across six Western countries. J Matern Fetal Neonatal Med. 2019 Sep. 32 (18):3102-8.
5)
Lin FY, Weisman LE, Azimi P, et al. Assessment of intrapartum antibiotic prophylaxis for the prevention of early-onset group B Streptococcal disease. Pediatr Infect Dis
J. 2 011 Sep. 30 (9):759-63.
6)
W eston EJ, Pondo T, Lewis MM, et al. The burden of invasive early-onset neonatal sepsis in the United States, 2005-2008. Pediatr Infect Dis J. 2011 Nov. 30 (11):937-
4 1 .
7)
Mor ales WJ, Dickey SS, Bornick P, Lim DV. Change in antibiotic resistance of group B streptococcus: impact on intrapartum management. Am J ObstetGynecol. 1999
A ug. 181 (2):310-4.
8)
Strunk T, Richmond P, Simmer K, Currie A, Levy O, Burgner D. Neonatal immune responses to coagulase-negative staphylococci. Curr Opin Infect Dis. 2007 Aug. 20
(4 ):370-5.
9)
Pow er Coombs MR, Kronforst K, Levy O. Neonatal host defense against Staphylococcal infections. Clin Dev Immunol. 2013. 2013:826303.
10)
Sr inivasan L, Kirpalani H, Cotten CM. Elucidating the role of genomics in neonatal sepsis. Semin Perinatol. 2015 Dec. 39 (8):611-6.
11)
Gr oer MW, Gregory KE, Louis-Jacques A, Thibeau S, Walker WA. The very low birth weight infant microbiome and childhood health. Birth Defects Res C Embryo Today.
2 015 Dec. 105 (4):252-64.
12)
Koen ig JM, Yoder MC. Neonatal neutrophils: the good, the bad, and the ugly. Clin Perinatol. 2004 Mar. 31 (1):39-51.
13)
W einberg AG, Rosenfeld CR, Manroe BL, Browne R. Neonatal blood cell count in health and disease. II. Values for lymphocytes, monocytes, and eosinophils. J Pediatr.
1 985 Mar. 1 06 (3):462-6.
14)
La ndor M. Maternal-fetal transfer of immunoglobulins. Ann Allergy Asthma Immunol. 1995 Apr. 74 (4):279-83; quiz 284.
15)
Gr iffiths PD, Stagno S, Pass RF, Smith RJ, Alford CA Jr. Congenital cytomegalov irus infection: diagnostic and prognostic significance of the detection of specific
im munoglobulin M antibodies in cord serum. Pediatrics. 1982 May. 69 (5):544-9.
16)
Koh ler PF. Maturation of the human complement system. I. Onset time and sites of fetal C1q, C4, C3, and C5 synthesis. J Clin Invest. 1973 Mar. 52 (3):671-7.
17)
Stocker J, Dehner L, eds. Pediatric Pathology. Vol 2. Philadelphia, PA: JB Lippincott; 1992.
18)
A rnon S, Litmanovitz I. Diagnostic tests in neonatal sepsis. Curr Opin Infect Dis . 2008 Jun. 21 (3):223-7 .
19)
Sim onsen KA, Anderson-Berry AL, Delair SF, Davies HD. Early-onset neonatal sepsis. Clin Microbiol Rev. 2014 Jan. 27 (1):21-47.
20)
Graham PL 3rd, Begg MD, Larson E, Della-Latta P, Allen A, Saiman L. Risk factors for late onset gram-negative sepsis in low birth weight infants hospitalized in the
n eonatal intensive care unit. Pediatr Infect Dis J. 2006 Feb. 25 (2):113-7.
21)
Stoll BJ, Hansen NI, Sánchez PJ, et al, for the Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Early
on set neonatal sepsis: the burden of group B Streptococcal and E. coli disease continues. Pediatrics. 2011 May. 127 (5):817-26.
22)
Am erican Academy of Pediatrics. Red Book 2003: Report of the Committee on Infectious Diseases. 26th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2003.
1 1 7-123, 237-43, 561-73, 584-91.
23)
Am erican Academy of Pediatrics. Red Book 2018-2021: Report of the Committee on Infectious Dis eases. 31st ed. Elk Grove Village, IL: American Academy of Pediatrics;
2 018.
24)
Am erican College of Obstetricians and Gynecologists Committee on Obstetric Practice. ACOG Committee opinion no. 485: Prevention of early-onset group B
str eptococcal disease in newborns (reaffirmed in 2016). Obstet Gynecol. 2011 Apr. 117 (4):1019-27.
25)
[Guideline] Schrag S, Gorwitz R, Fultz-Butts K, SchuchatA. Prevention of perinatal group B streptococcal disease. Revised guidelines from CDC. MMWR Recomm Rep.
2 002 Aug 16. 51 (RR-11):1-22.
26)
Mu khopadhyay S, Lieberman ES, Puopolo KM, Riley LE, Johnson LC. Effect of early-onset sepsis evaluations on in-hospital breastfeeding practices among asymptomatic
term neonates. Hosp Pediatr. 2015 Apr. 5 (4):203-10.
27)
Kermorvant-Duchemin E, Laborie S, Rabilloud M, Lapillonne A, Claris O. Outcome and prognostic factors in neonates with septic shock.Pediatr Crit Care Med. 2008
Ma r. 9 (2):186-91.
[Medline]
.
