
CHOLERA
means "flow of bile."
most feared epidemic diarrheal disease
because of its severity.
is caused by Vibrio cholerae,
Dehydration and death can occur within a
matter of hours of
infection.

ETIOLOGY:
The organism is a comma-shaped, gram-negative aerobic bacillus
Its antigenic structure consists of a flagellar H
antigen and a somatic O antigen.
O antigen allows for separation into pathogenic
and nonpathogenic strains.
V cholerae O1 was the cause of most pandemics until a new
strain, termed V cholerae O139 (non-O1 type)
V cholerae O1 is classified into 2 major biotypes: Classic
and El Tor. Currently, El Tor is the predominant cholera
pathogen. Organisms in both biotypes are subdivided into
serotypes according to the structure of the O antigen, as follows:
•
Serotype Inaba - O antigens A and C
•
Serotype Ogawa - O antigens A and B
•
Serotype Hikojima - O antigens A, B, and C

EPIDEMIOLOGY:
Cholera is an ancient disease caused by Vibrio cholerae O1
or, more recently, by V cholerae O139.It can be
spread as an endemic, epidemic, or pandemic disease.
Cholera has been rare in industrialized nations for last 100
years; however, the disease is still common in other parts of
the world, including the Indian subcontinent and sub-
Saharan Africa
In nonendemic areas, incidence of infection is similar in
all age groups, although adults are less likely to become
asymptomatic than children.Infants are protected

V cholerae is a saltwater organism, and its primary habitat
is the marine ecosystem where it lives in association with
plankton.Cholera has 2 main reservoirs, man and water. V cholerae
rarely is isolated from animals, and animals do not play a role in
transmission of disease.Primary infection in humans is acquired
incidentally. Risk of primary infection is facilitated by seasonal
increases in the number of organisms, possibly associated with changes
in water temperature and algal blooms.Secondary transmission occurs
through fecal-oral spread of the organism through person-to-person
contact or through contaminated water and food. Such secondary
spread commonly occurs in households but also can occur in clinics or
hospitals where patients with cholera are treated.Transmission by direct
person-to-person contact is rare.Infection rates predictably are highest
in communities in which water is not potable and personal and
community hygiene standards are low
.
PATHOPHYSIOLOGY:
The infectious dose of bacteria required to cause clinical disease varies with the mode of
administration. If ingested with water, the infectious dose is 103-106 organisms. When
ingested with food, fewer organisms are required to produce disease: 102-104
organisms. The use of antacids, histamine receptor blockers, and proton pump inhibitors
increases the risk of cholera infection and predisposes patients to more severe disease
as a result of reduced gastric acidity. The same applies to patients with chronic gastritis
or those who have undergone a gastrectomy. V cholerae O1 and O139 cause clinical
disease by producing an enterotoxin called cholera toxin (CTX)which is a potent protein
elaborated by the organism in the small intestine.The enterotoxin is a protein molecule
composed of subunits A and B. The B subunit is the binding subunit, and the A subunit is
the enzymatic subunit The B subunits are responsible for binding to a ganglioside
(monosialosyl ganglioside, GM1) receptor located on the surface of the cells that line the
intestinal mucosa. The activation of the A subunit by adenylate cyclase is responsible for
the net increase in cyclic adenosine monophosphate (cAMP). cAMP blocks the
absorption of sodium and chloride by the microvilli and promotes the secretion of chloride
and water by the crypt cells. The result is watery diarrhea with electrolyte concentrations
isotonic to those of plasma.Fluid loss originates in the duodenum and upper jejunum; the
ileum is less affected. The colon is usually in a state of absorption because it is relatively
insensitive to the toxin. However, the large volume of fluid produced in the upper intestine
overwhelms the absorptive capacity of the lower bowel, which results in severe diarrhea.
The enterotoxin acts locally and does not invade the intestinal wall. As a result, few
neutrophils are found in the stool.
:
CLINICALMANIFESTAIONS
After a 24-to 48-hour incubation period, symptoms begin with
the sudden onset of painless, watery diarrhea that may quickly
become voluminous and is often followed by vomiting. The patient
may experience accompanying abdominal cramps. Fever is typically
absent.
Diarrhea
Profuse watery diarrhea is a hallmark of cholera.Stool volume is more
than that of any other infectious diarrhea,with a severe disease the stool
volume is more than 250 mL/kg body weight in a 24-hour

The characteristic cholera stool is an opaque white
liquid that is not malodorous or fishy odor and
often is described as having a rice water
appearance (ie, in color and consistency, it
resembles water that has been used to wash or
cook rice).It contains few leukocytes and no
erythrocytes.Patients have frequent and often
uncontrolled bowel movements and experience
abdominal cramps caused by distention of loops of
small bowel as a result of the large volume of
intestinal secretions.

Vomiting
Vomiting is a prominent manifestation of illness.Early
vomiting is caused by decreased gastric and intestinal
motility and later the acedemia is more likely.If
untreated, the diarrhea and vomiting isotonic
dehydration and, in severe disease vascular collapse,
shock, and death.Dehydration can develop within hours
after the onset of symptoms. This contrasts with disease
produced by infection from any other enteropathogen.
Water loss is proportional between three body
compartments(intracellular, intravascular, and interstitial).

Physical:
Dehydration:
Dehydration has been classified into the following 3 categories to facilitate
patient treatment: severe, some (previously termed moderate in the WHO
criteria for the classification of dehydration), and none (previously termed
mild by the WHO).
Decreased intravascular volume is manifested by tachycardia, absent or
barely palpable peripheral pulses, and hypotension .Tachypnea and
hypercapnia also are part of the clinical picture.Patients with severe
dehydration loose approximately 15% of total body water (approximately 10%
of total body weight).In some (moderate) dehydration the loss is
approximately 7-10% of body water (approximately 5% of body
weight).Children have decreased skin turgor, as manifested by prolonged skin
tenting in response to a skin pinch (the most reliable sign of isotonic
dehydration), and a normal pulse.Children without clinically significant
dehydration (<5% loss of body weight) may have increased thirst without
other signs of dehydration.

Metabolic and systemic manifestations
Hypoglycemia is the second most common lethal complication of
cholera. The causes :diminished food intake, exhaustion of glycogen
stores, and defective gluconeogenesis.
Acidosis:
bicarbonate loss in stools, accumulation of lactate because of
diminished perfusion of peripheral tissues, and hyperphosphatemia.
Hypokalemia:
potassium loss in the stool, severe total body potassium depletion and
after the correction of acidosis . Hypokalemia may be manifested as
paralytic ileus.
Hypocalcemia:
rehydration therapy with bicarbonate-containing fluids also can
produce by decreasing the serum calcium that is ionized. Chvostek and
Trousseau signs often are present, and spontaneous titanic
contractions can occur.

Lab.studies
Direct microscopic examination: a gram-negative curved bacillus that is motile by means of a single
flagellum which observed by Gram stain or by direct dark field examination of the stool.
Culture: routine differential media( triple sugar iron agar) in which the organism is sucrose-
positive,.lactose-negativ,and
oxidase-positive.These media used routinely to differentiate the organism from other intestinal
bacteria. selective media: Vibrio species has the ability to grow at a high pH or in bile salts (eg,
thiosulfate-citrate-bile-sucrose-agar [pH 8.6]).These media are recommended to facilitate isolation and
lab diagnosis
Serotyping and biotyping: by immobilization tests in which specific antisera can be used. Classic and El
Tor biotypes also can be identified using the same method.
Hematological tests:Hematocrit, serum-specific gravity, and serum protein are elevated in dehydrated
patients.They generally have a leucocytosis.
Serum electrolytes:Serum sodium usually is low. Serum potassium levels are either normal or low.
Bicarbonate concentration usually is less than 15 mmol/L in severely dehydrated patients and often is
nondetectabl.Calcium and magnesium levels are usually high .Renal profile: Blood urea nitrogen and
serum creatinine are elevated. Blood glucose is elevated and the arterial pH is usually low(metabolic
acidosis).
Other Tests:More recently, polymerase chain reaction (PCR) has been used with a high degree of
sensitivity and specificity.

TREATMENT
Steps in the treatment of a patient with suspected cholera
Step 1: Assess the degree of dehydration and categorize it into
severe dehydration, some dehydration, or no signs of
dehydration
Step 2: Rehydrate the patient and monitor frequently. Then
reassess hydration status. The primary objectives of the
treatment are to correct dehydration, and then maintain
hydration.
Step 3: Maintain hydration. Replace ongoing fluid losses until
diarrhea stops.
Step 4: Administer an oral antibiotic to the patient with severe
dehydration.
Step 5: Feed the patient.

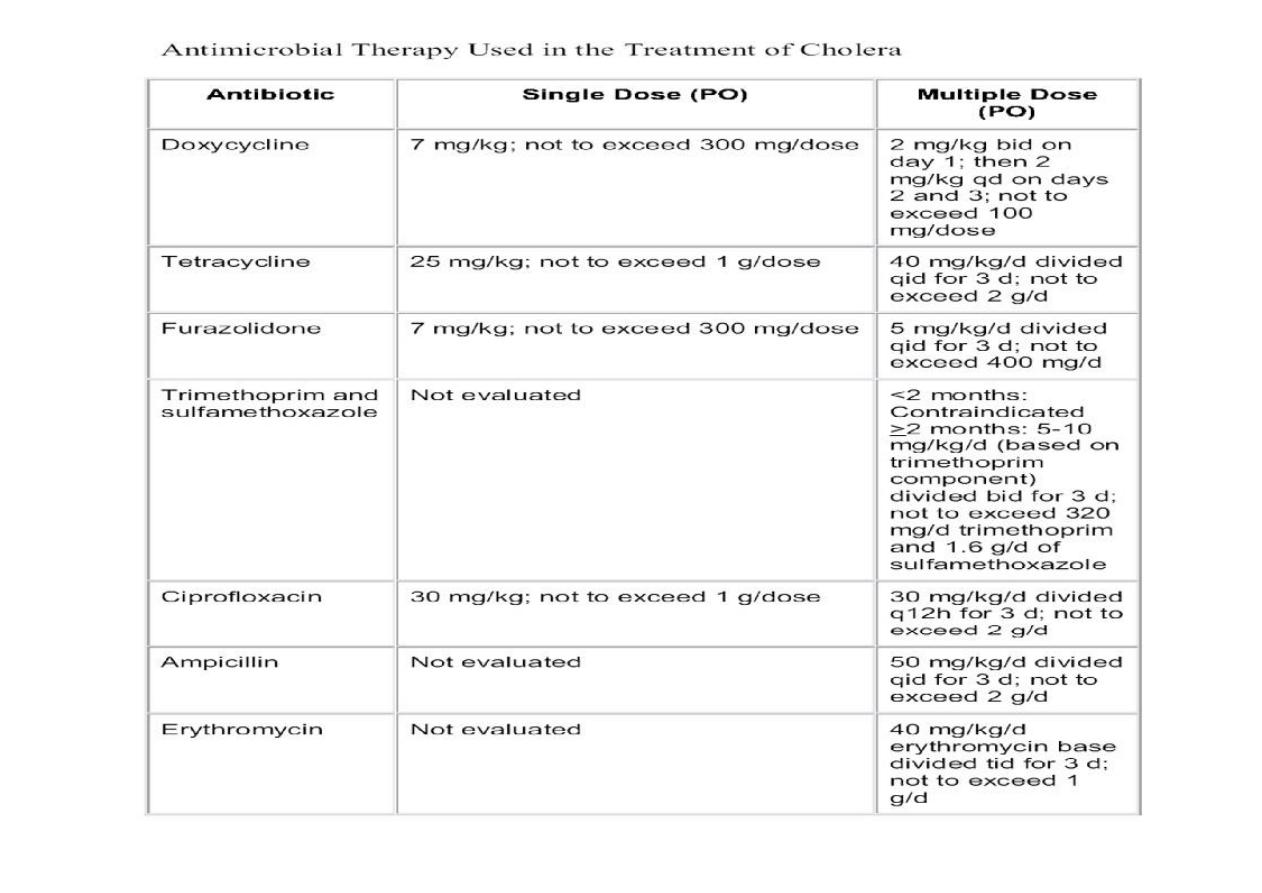
Antimicrobial therapy
Antimicrobial therapy is an adjunct to fluid
therapy of cholera and is not an essential
component. However, it reduces diarrhea
volume and duration by approximately 50%. The
choice of antibiotics is determined by the
susceptibility patterns of the local strains of V
cholerae O1 or O139.

Complications:
Complications of the disease
Dehydration renal failure (acute tubular necrosis) and death, is the most important
complication.Another complication is electrolyte imbalance if appropriate solutions are
not used for rehydration.Hypoglycemia is an important complication that should be
evaluated for and treated with glucose therapy.
Complications of therapy:
Overhydration with parenteral fluid therapy. If not recognized leading to pulmonary
edema.
PREVENTION:
Efforts in prevention of cholera should involve the following strategies:
o
Rapid identification of cases and prompt treatment will limit further
spread of the disease.
o
Sensitive surveillance and prompt reporting contribute to the rapid
containment of cholera
o
Improvements in Water supply and sanitation
o
Education on specific hygiene practices, food preparation, and
health education.
o
Vaccines: Parenteral vaccines have poor efficacy
�discontinued.
Oral vaccines, which are available in some countries but are used mainly by travelers.
