Prof. Sumaya T. S.
Chronic Pelvic Pain (CPP)
is pain of
apparent pelvic origin that has been
present most of the time for the
past six months
Definition
Difficult to diagnose
Difficult to treat
Difficult to cure
Frustration for
patient and
physician
Definition
Affects 15-20% of women of reproductive age
Accounts for 20% of all laparoscopies
Accounts for 12-16% of all
hysterectomies
Associated medical costs of $3 billion
annually
Incidence
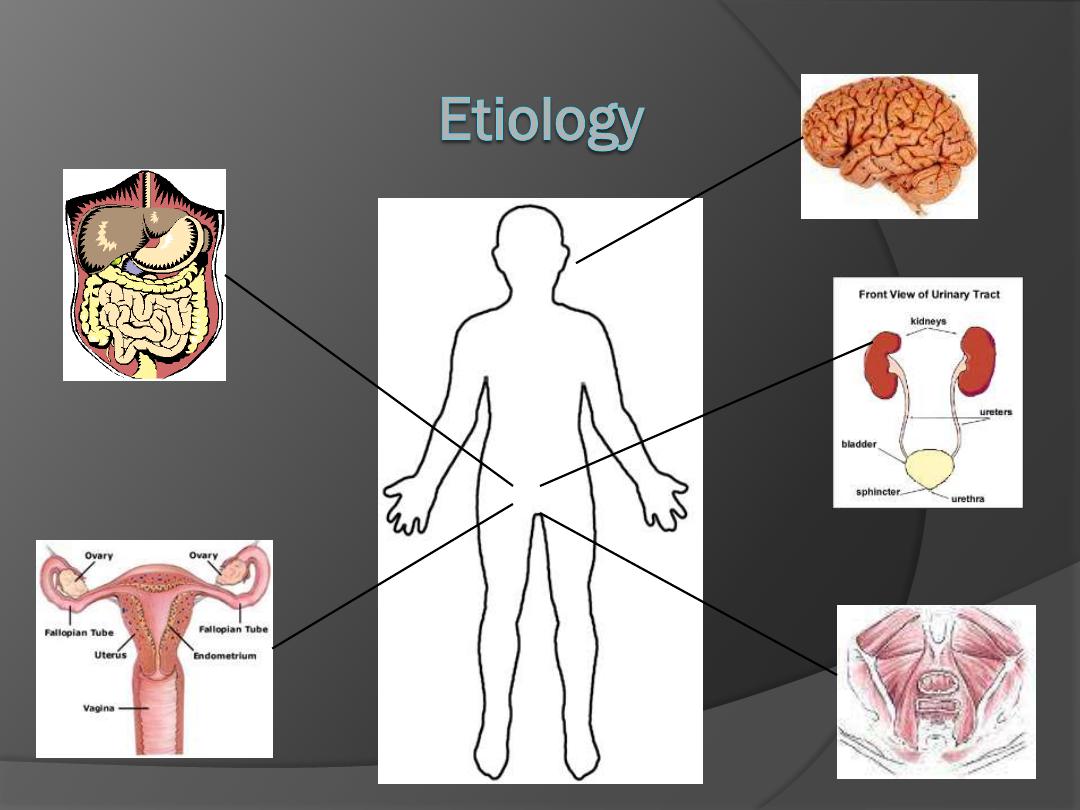
Gynecological 20%
Gastrointestinal 37%
Musculoskeletal
Urological 30%
Psychological
25-50% of women had more than one diagnosis
Severity and consistency of pain increased with
multisystem symptoms
Most common diagnoses:
• endometriosis
• adhesive disease
• irritable bowel syndrome
• interstitial cystitis
Obtaining a
COMPLETE and DETAILED HISTORY
is the most important key to
formulating a diagnosis
Diagnosis
Diagnosis: Obtaining the History
Associated with menses?
Association with sexual activity? (Be specific)
New sexual partner and/or practices?
Symptoms of vaginal dryness or atrophy?
Other changes with menses?
Use of contraception?
Detailed childbirth history?
History of pelvic infections?
History of gynecological surgeries or other problems?
Gynecological Review of Systems
Diagnosis: Obtaining the History
Regularity of bowel movements?
Diarrhea/ constipation/ flatus?
Relief with defecation?
History of hemorrhoids/ fissures/ polyps?
Blood in stools, melena, mucous?
Nausea, emesis or change in appetite?
Abdominal bloating?
Weight loss?
Gastrointestinal Review of Systems
Diagnosis: Obtaining the History
Pain with urination?
History of frequent or recurrent urinary tract infxn?
Hematuria?
Symptoms of urgency or urinary incontinence?
Difficulty voiding?
History of nephrolithiasis?
Urological Review of Systems
Diagnosis: Obtaining the History
History of trauma?
Association with back pain?
Other chronic pain problems?
Association with position or activity?
Musculoskeletal Review of Systems
Diagnosis: Obtaining the History
History of verbal, physical or sexual abuse?
Diagnosis of psychiatric disease?
Onset associated with life stressors?
Exacerbation associated with life stressors?
Familial or spousal support?
Psychological Review of Systems
Diagnosis: The Physical Exam
Evaluate each area individually
Abdomen
Anterior abdominal wall
Pelvic Floor Muscles
Vulva
Vagina
Urethra
Cervix
Viscera
– uterus, adnexa, bladder
Rectum
Rectovaginal septum
Coccyx
Lower Back/Spine
Posture and gait
A bimanual exam alone is
NOT sufficient for
evaluation
Diagnosis: Objective Evaluative Tools
Basic Testing
Pap Smear
Gonorrhea and Chlamydia
Wet Mount
Urinalysis
Urine Culture
Pregnancy Test
CBC with Differential
ESR
PELVIC ULTRASOUND
Specialized Testing
MRI or CT Scan
Endometrial Biopsy
Laparoscopy
Cystoscopy
Urodynamic Testing
Urine Cytology
Colonoscopy
Electrophysiologic studies
Referral to Specialist
Differential Diagnosis: Gynecological Conditions
Cyclical
Endometriosis
Adenomyosis
Primary Dysmenorrhea
Ovulation Pain/ Mittleschmertz
Ovarian Remnant Syndrome
Non-cyclical
Pelvic Masses
Adhesive Disease
Pelvic Inflammatory Disease
Pelvic Congestion Syndrome
Symptomatic Pelvic Organ Prolaps
Pelvic Floor Pain Syndrome
Pelvic Inflammatory Disease
Description:
Spectrum of inflammation and infection
in the upper female genital tract
Endometritis/ endomyometritis
Salpingitis/ salpingoophritis
Tubo-ovarian Abscess
Pelvic Peritonitis
Pathophysiology:
Ascending infection of vaginal and
cervical microorganisms
Chlamydia and Gonorrhea (developed countries)
Tuberculosis (developing countries)
Acute PID usually polymicrobial infection
Pelvic Inflammatory Disease
Risk Factors
Adolescent
Multiple sexual partners
Greater than 2 sexual partners in past 4 weeks
New partner in the past 4 weeks
Prior history of PID
Prior history of gonorrhea or chlaymdia
Smoking
None or inconsistent condom use
Instrumentation of the cervix
Pelvic Inflammatory Disease
Minimum Criteria (one required):
Uterine Tenderness
Adnexal Tenderness
Cervical Motion Tenderness
No other identifiable causes
Additional criteria for dx:
Oral temperature greater than
101
Abnormal cervical or vaginal
discharge
Presence of increased WBC in
vaginal secretions
Elevated ESR or C-reactive
protein
Documented of CT
Specific criteria for dx:
Pathologic evidence of
endometritis
US or MRI showing
hydrosalpinx,
Laparosopic findings
consistent with PID
Pelvic Inflammatory Disease
Treatment:
Multiple outpatient antibiotic regimens;
total therapy for 14 days.
A)CEFTERIAXON 500 mg im single dose and
doxycycline 100 mg twice daily plus metronidazole 400
mg twice daily.
B )ofloxacin 400 mg twice daily plus metronidazole twice
daily.
Inpatient regimens in form of i.v. cefteriaxon 2g daily plus
i.v. or oral doxycycline 100 mg BD followed by oral
doxycycline 100 mg BD plus metronidazole 400 mg BD.
*laparoscopy to confirm the diagnosis
*drainage of abscess
*treatement of concomitent diseases.
Infertility
Ectopic Pregnancy
Chronic Pelvic Pain
Occurs in 18-35% of women who develop PID
May be due to inflammatory process with development of pelvic
adhesions
Pelvic Congestion Syndrome
Description:
Retrograde flow through incompetent
valves venous valves can cause tortuous and
congested pelvic and ovarian varicosities; Etiology
unknown.
Symptoms:
Pelvic ache or heaviness that may
worsen premenstrually, after prolonged sitting or
standing, or following intercourse
Diagnosis:
Pelvic venogrpahy, CT, MRI, ultrasound,
laparoscopy
Treatment:
Progestins, GnRH agonists, ovarian vein
embolization or ligation, and hysterectomy with
bilateral salpingo-oophorectomy (BSO)
Pelvic Floor Pain Syndrome
Description:
Spasm and strain of pelvic floor muscles
Levator Ani Muscles
Coccygeus Muscle
Piriformis Miscle
Symptoms:
Chronic pelvic pain symptoms; pain in
buttocks and down back of leg, dyspareunia
Treatment:
Biofeedback, Pelvic Floor Physical
Therapy, TENS (Transcutaneous Electrical Nerve
Stimulation) units, antianxiolytic therapy, cooperation
from sexual partner
Differential Diagnosis:
Urological Conditions that may Cause or
Exacerbate Chronic Pelvic Pain
Bladder Carcinoma
Interstitial Cystitis
Radiation Cystitis
Urethral Syndrome
Detrussor Dyssynergia
Urethral Diverticulum
Chronic Urinary Tract Infection
Recurrent Acute Cystitis
Recurrent Acute Urethritis
Stone/urolithiasis
Urethral Caruncle
Source: ACOG Practice Bulletin #51, March
2004
Interstitial Cystitis
Description:
Chronic inflammatory condition of the bladder
Etiology:
Loss of mucosal surface protection of the
bladder and thereby increased bladder permeability
Symptoms:
Urinary urgency and frequency
Pain is worse with bladder filling; improved with urination
Pain is worse with certain foods
Pressure in the bladder and/or pelvis
Pelvic Pain in up to 70% of women
Present in 38-85% presenting with chronic pelvic pain
Interstitial Cystitis
Diagnosis:
Cystoscopy with bladder distension
Presence of glomerulations (Hunner Ulcers)
Treatment:
Avoidance of acidic foods and beverages
Antihistamines
Tricyclic antidepressants
Elmiron (pentosan polysulphate)
Intravesical therapy: DMSO (dimethyl sulfoxide)
Differential Diagnosis:
Gastrointestinal Conditions that may Cause or
Exacerbate Chronic Pelvic Pain
Colon Cancer
Constipation
Inflammatory Bowel Disease
Colitis
Chronic Intermittent Bowel
Obstruction
Diverticular Disease
Source: ACOG Practice Bulletin #51, March
2004
Irritable Bowel Syndrome
Irritable Bowel Syndrome (IBS)
Description:
Chronic relapsing pattern of abdominopelvic
pain and bowel dysfunction with diarrhea and constipation
Prevalence
Affects 12% of the U.S. population
2:1 prevalence in women: men
Peak age of 30-40
’s
Rare on women over 50
Associated with elevated stress level
Symptoms
Diarrhea, constipation, bloating, mucousy stools
Symptoms of IBS found in 50-80% women with CPP
Irritable Bowel Syndrome (IBS)
Diagnosis based on Rome II
criteria
Treatment
Dietary changes
Decrease stress
Cognitive Psychotherapy
Medications
Antidiarrheals
Antispasmodics
Tricyclic Antidepressants
Serotonin receptor (3, 4)
antagonists
40
– 50% of women with CPP have a history of
abuse (physical, verbal , sexual)
Psychological Associations
Psychosomatic factors play a prominent role in CPP
Approach patient in a gentle, non-judgmental manner
• Do not want to imply that “pain is all in her head”
Psychotropic medications and various modes of
psychotherapy appear to be helpful as both primary and
adjunct therapy for treatment of CPP
Chronic Pelvic Pain requires patience, understanding
and collaboration from both patient and physician
Obtaining a thorough history is key to accurate
diagnosis and effective treatment
Diagnosis is often multifactorial
– may affect more
than one pelvic organ
Treatment options often multifactorial
– medical, surgical,
physical therapy, cognitive
Conclusions
