
Gestational Trophoblastic
Disease (GTD)

GTD Overview
• Heterogeneous group of related lesions
Arise from abnormal proliferation of trophoblast
of the placenta
• Unique because the maternal lesions arise from
fetal (not maternal) tissue
• Most GTD lesions produce the beta subunit of
human chorionic gonadotropin (B-hCG)

• GTD histologically is divided into
• benign
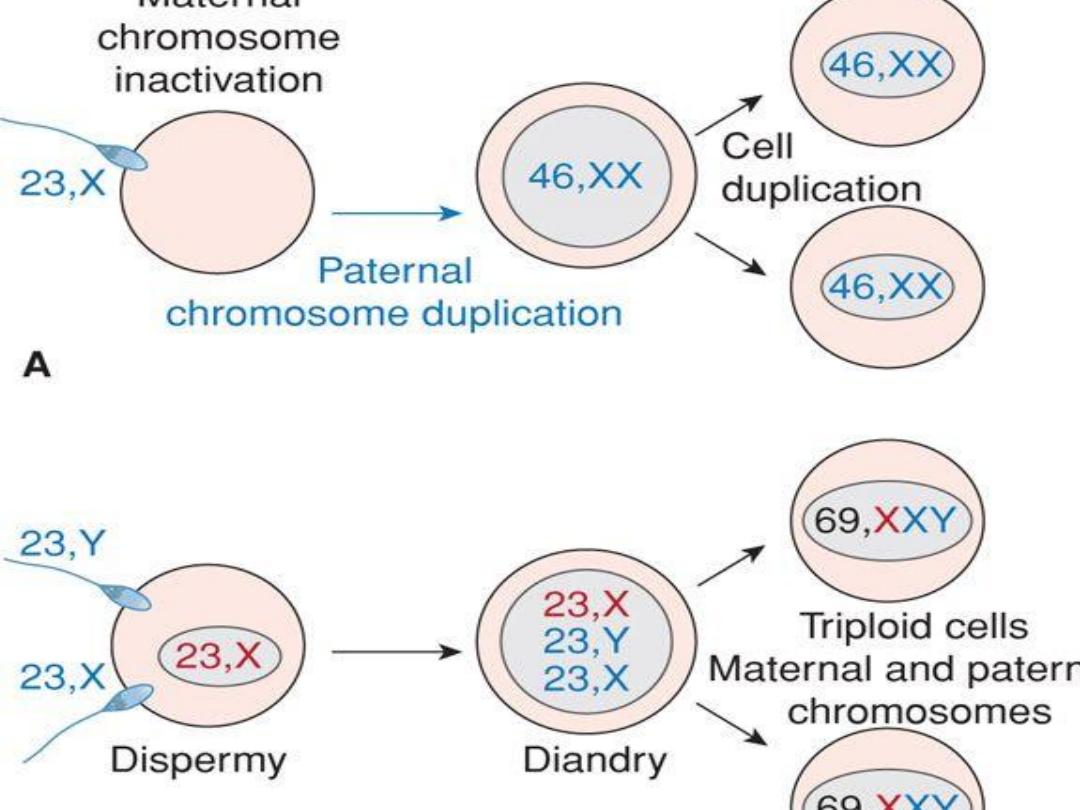
hydatidiform moles ; ( complete and partial)
• Malignant
Invasive mole
Non -molar trophoblastic neoplasms
•
Choriocarcinoma
•
Placental site trophoblastic tumor
•
Epithelioid trophoblastic tumor

Hydatidiform Mole
• North America: 0.6-1.1 per 1000 pregnancies
• Asia: 2-10 per 1000 (3x Western countries)
• Difference possibly related low dietary intake
of carotene (vitamin A deficiency) and animal
fat
• More common at reproductive extremes in
age (>35y or <20y)
Hydatidiform Mole
Risk Factors:
• History of previous GTD
– If one previous mole, 1% chance of recurrence
(vs. 0.1% in general population)
– If 2 previous moles, risk of recurrence increases
to 16-28%
• Smoking
• Vitamin A deficiency

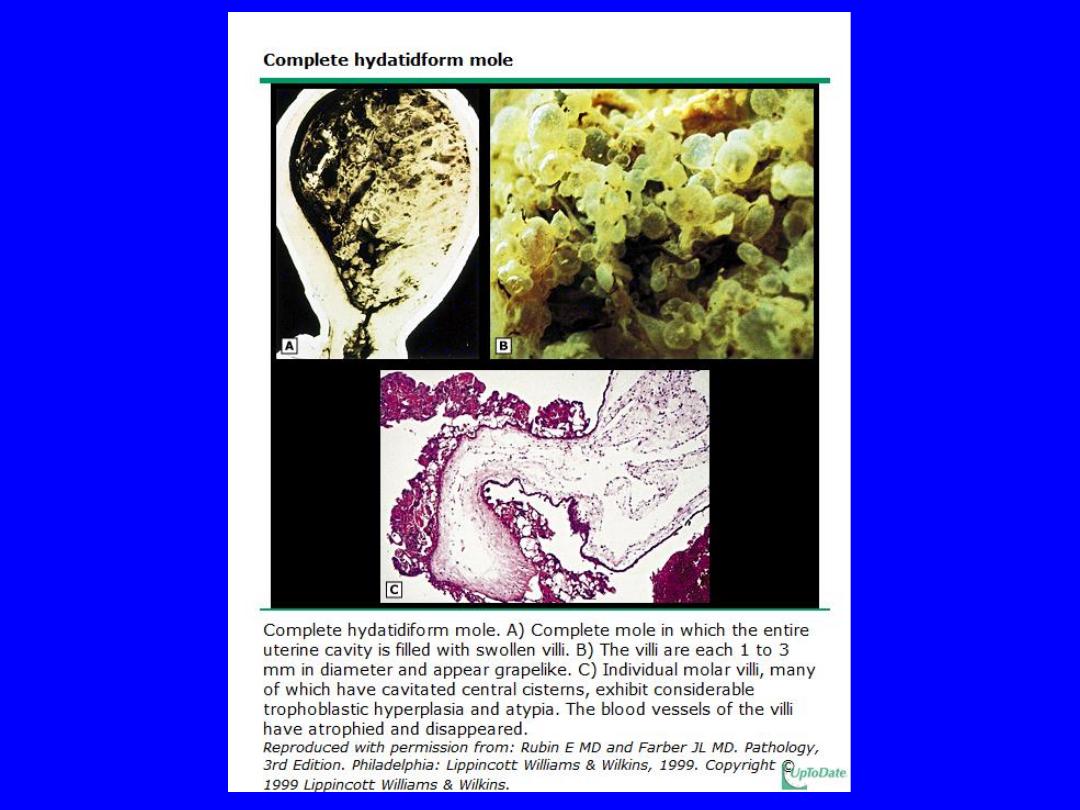
Hydatidiform mole
• Microscopic (classic findings)
Absence embryonic elements
Trophoblastic proliferation (cytotrophoblast
and syncytiotrophoblast)
Stromal edema and hydropic
degeneration
Absence of blood vessels
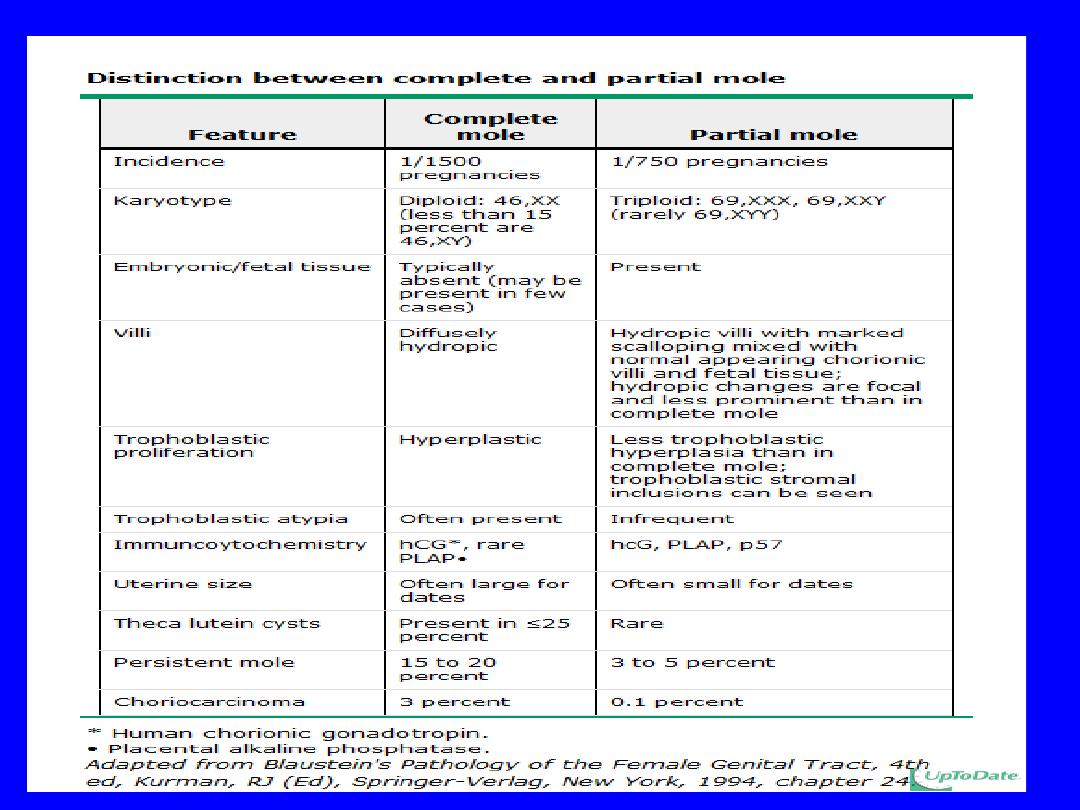
Hydatidiform Mole
Clinical Manifestations:
• Vaginal bleeding/anemia
• Enlarged uterus (size > dates)
• Pelvic pain
• Theca lutein cysts
• Hyperemesis gravidarum
• Hyperthyroidism
• Preeclampsia <20 weeks gestation
• Vaginal passage of hydropic vesicles

Diagnosis
• Amenorrhea followed by irregular
bleeding
• Spontaneous passage of molar tissue
• High values Serum β-HCG
measurement
•
confirming the diagnosis

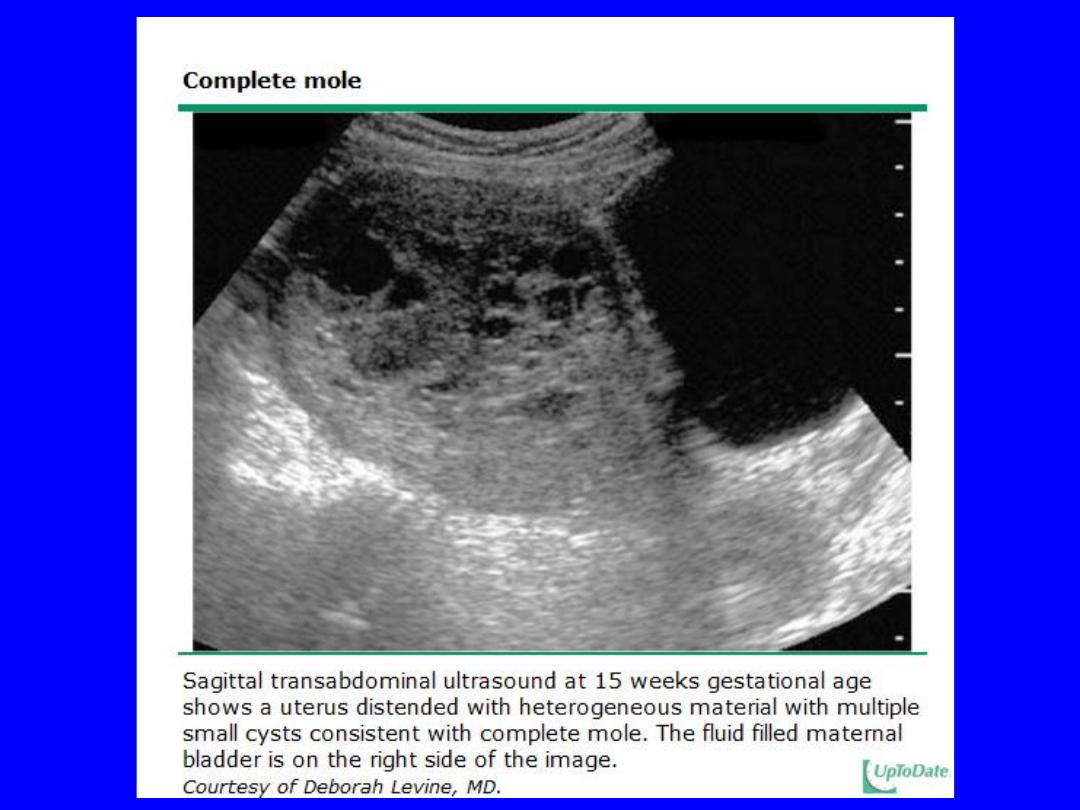
Sonography
Echogenic uterine mass with
anechoic cystic spaces
without a fetus or amnionic sac
The appearance as “snowstorm

Hydatidiform Mole Treatment
• Evaluate for coexisting conditions:
- History and physical
- CBC, coagulation profile, serum chemistry
- thyroid function
- blood type and crossmatch
- chest radiography
- pelvic ultrasonography
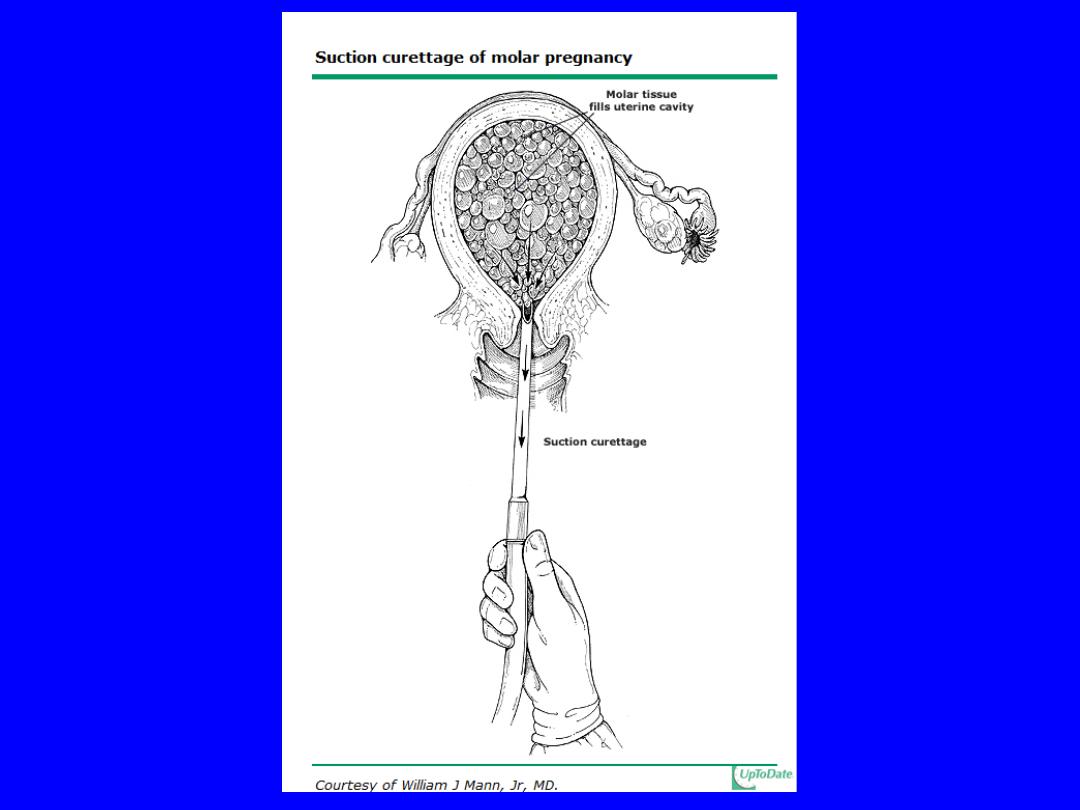
• Evacuation of mole
- Suction curettage
- Hysterectomy if completed childbearing
Follow-Up Care – Molar Pregnancy
• 80% of patients cured by evacuation
• Follow B-hCG levels every two weeks until 3
consecutive tests negative
• Then monthly B-hCG every month for 6-12 months
• Avoid pregnancy for at least 6 months after first
normal B-hCG
• Birth control during follow-up period
• Subsequent Pregnancies:
– Send placenta for pathology
– Check B- hCG 6 weeks postpartum

• After molar evacuation
• risk factors for malignant squeal
• 15 - 20 % complete moles
•
1 - 5 % partial moles
•
• 1 5% of HM become invasion moles
•
2.5% progress into
choriocarcinoma

Gestational Trophoblastic Neoplasia
(GTN)
• Persistent/Invasive Mole
• Choriocarcinoma
• Placental-Site Trophoblastic Tumor (PSTT)

Risk Factors for GTN After Mole
• Preevacuation uterine size greater than
gestationl age or larger than 20 weeks
gestation
• Theca-lutein cysts larger than 6 cm
• Age > 40 years
• Serum hCG levels > 100,000 mIU/mL
• Medical complications of molar pregnancy
• Previous hydatidiform mole

Criteria for Diagnosis of
Gestational Trophoblastic
Neoplasia
1
. Plateau or rise of serum β-hCG level
2
. Detectable serum β-hCG level for
6 months or more
3. Histological criteria for choriocarcinoma
4-Irregular bleeding ,uterine sub involution

• Plateau of serum β-hCG level (± 10 percent)
• for
four
easurements during a period of
• 3 weeks or longer
• days 1, 7, 14, 21
. Rise of serum β-hCG level > 10 percent
• during three weekly consecutive , during a
• period of
2
weeks or more—days 1, 7, 14

Invasive Mole
• Myometrial invasion by hydatidiform mole
• 1 in 15,000 pregnancies
• 10-17% of hydatidiform moles will progress
to invasive moles

Choriocarcinoma
• Most aggressive type of GTN
• Abnormal trophoblastic hyperplasia
• Absence of chorionic villi
• Direct invasion of myometrium
• Vascular spread to distant sites:
– Lungs
– Brain
– Liver
– Pelvis and vagina
– Spleen, intestines, and kidney

Choriocarcinoma
• May come from any type of pregnancy
- 25% follow abortion or tubal pregnancy
- 25% with term gestation
- 50% from hydatidiform moles
• 2-3% of moles progress to choriocarcinoma
• Incidence 1 in 40,000 pregnancies

Symptoms
• Metastatic symptoms
• Profuse vaginal bleeding
• Vaginal or cervical metastasis
•
(bluish nodule in vaginal)
• Abdominal pain (intra-abdominal
hemorrhage)
• Cough, hemoptysis
• Headache, nausea, vomit, paralysis or
coma
• Urologic hemorrhage

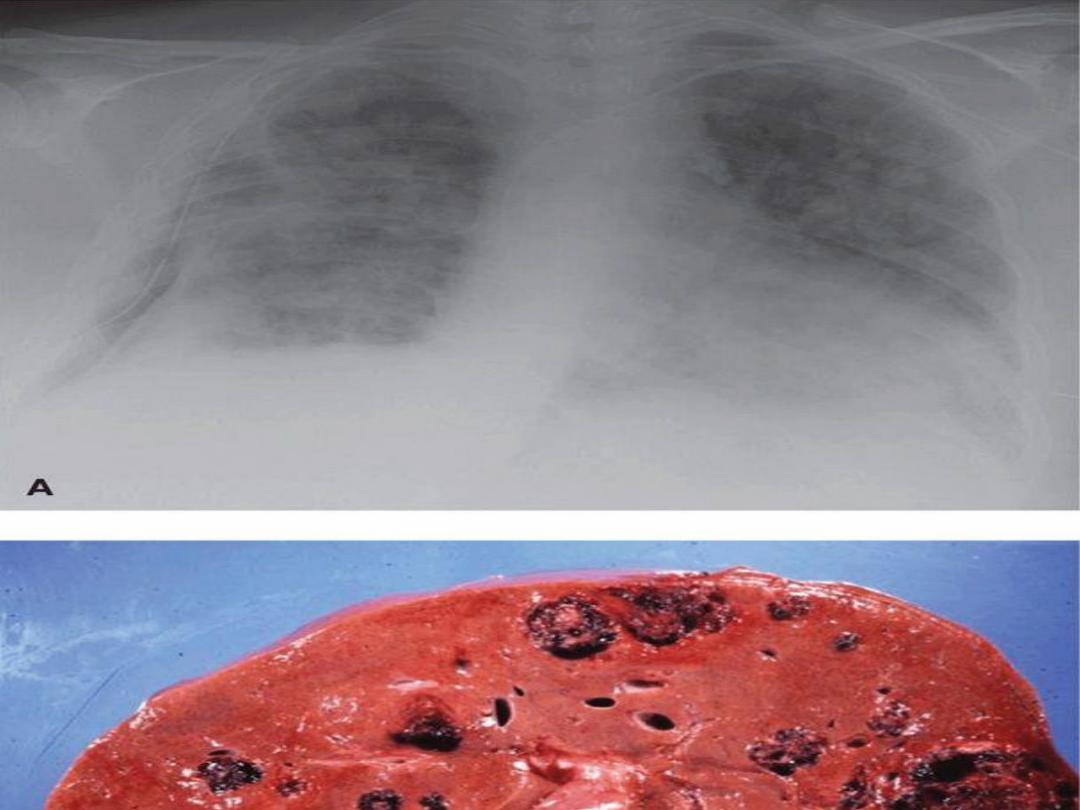
Lung metastasis
Four principal pulmunary radiologic patterns:
• Snowstorm pattern (Alveolar pattern )
• Discrete rounded densities
• Plural effusion
• Embolic pattern


Placental-Site Trophoblastic Tumor
(PSTT)
• Originate from intermediate cytotrophoblast
cells
• Secrete human placental lactogen (hPL)
• B-hCG often normal
• Less vascular invasion, necrosis and
hemorrhage than choriocarcinoma
• Lymphatic spread
• Arise months to years after term pregnancy
but can occur after spontaneous abortion or
molar pregnancy

Placental-Site Trophoblastic Tumor
(PSTT)
• Most common symptom is vaginal bleeding
• Tend to:
- Remain in uterus
- Disseminate late
- Produce low levels of B-hCG compared to
other GTN
- Be resistant to chemotherapy (treat with
surgery)

Signs & Symptoms GTN
• Continued uterine bleeding, uterine
perforation, enlarged irregular uterus,
persistent bilateral ovarian enlargement
• From metastatic lesions: abdominal pain,
hemoptysis, melena, increased intracranial
pressure (headaches, seizures, hemiplegia),
dyspnea, cough, chest pain
Diagnosis of GTN
• Increase or plateau in B-hCG after molar
pregnancy
• Pathologic diagnosis by D&C or biopsy of
metastatic lesions
• WARNING: biopsy of metastatic lesions can
result in massive hemorrhage
• Metastatic workup: CXR (or CT chest), CT
abdomen/pelvis +/- CT/MR of brain

Classification & Staging of GTD
• World Health Organization (WHO) Scoring
Index
– Describes anatomic distribution of disease
– FIGO staging ;Describes prognosis
WHO Staging
Stage
Description
I
Disease confined to the uterus
II
Disease extends outside the uterus but
limited to genital structures (adnexa,
vagina, and broad ligament)
III
Disease extends to the lungs with or
without genital tract involvement
IV
Disease involves any other metastatic sites
Therapy for GTN
• Low-risk = score ≤6
• High-risk = score ≥7
• Single agent therapy for nonmetastatic
(stage I) or low-risk metastatic (stage II and
III) with score <7 → survival rates ~ 100%
• Combination chemotherapy +/- adjuvant
radiation and/or surgery for high-risk
metastatic disease or score ≥7

Therapy: Nonmetastatic GTN
• Single-agent with either methotrexate or
dactinomycin
• Chemotherapy continued until hCG values normal
and then 2-3 cycles beyond
• Change to alternative single-agent for hCG plateaus
above normal or toxicities
• If significant elevation of hCG or new metastases,
switch to multiagent
• 85-90% cured with initial regimen, <5% will require
hysterectomy for cure

Follow-up Care
• After completion of chemotherapy, follow
serial hCG every 2 weeks for three months,
then monthly for one year
• Physical examinations every 6-12 months and
imaging as indicated

Reproductive Performance
• Most women resume normal ovarian
function
• No increase risk of stillbirths, abortions,
congenital anomalies, prematurity, or major
obstetric complications
• No evidence of reactivation
• At increased risk for development of second
episode
Summary
• Hydatidiform mole is a benign condition, 80%
cured with suction D&C
• Malignant GTN:
– Persistent or invasive mole
– Choriocarcinoma
– PSTT
• WHO score > 7 represents high-risk disease
• GTN very sensitive to chemotherapy
