
Ectopic pregnancy
Prof. Sumaya T. S.
Definition
Any pregnancy where the fertilised ovum gets implanted &
develops in a site other than normal uterine cavity.( either
outside the uterus (Fallopian tube, ovary or abdominal
cavity) or in an abnormal position within the uterus
(cornua, cervix)).
• Ectopic Pregnancy is a common, life–threatening condition
affecting one in 100 pregnancies
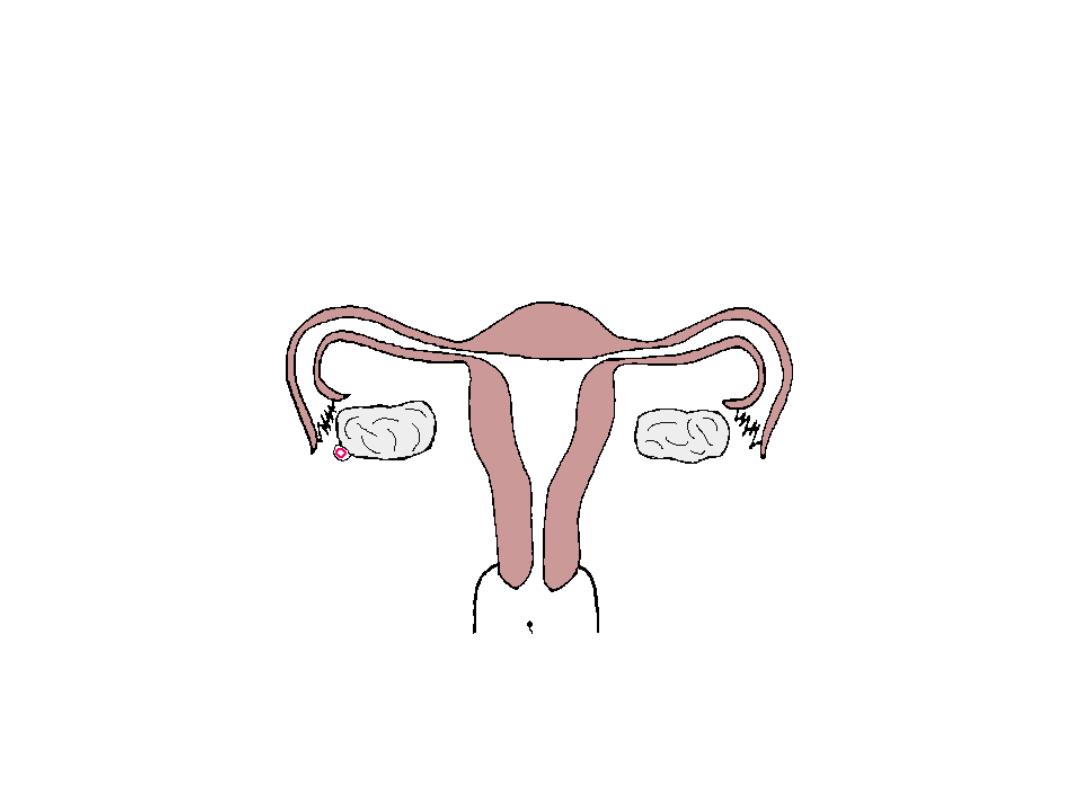
Implantation sites:
• Tubal pregnancy
(96-98%):
ampullary portion of the fallopian tube (mid) (80-90%)
isthmic portion of the fallopian tube (area closer to
uterus)
fimbrial portion of the fallopian tube (distal end away
from uterus)
cornual portion of the fallopian tube (within the uterine
muscle)
• Abdominal
primary/secondary
• Ovarian
• Cervical
• Heterotopic
(combination of ectopic + intrauterine
pregnancy)
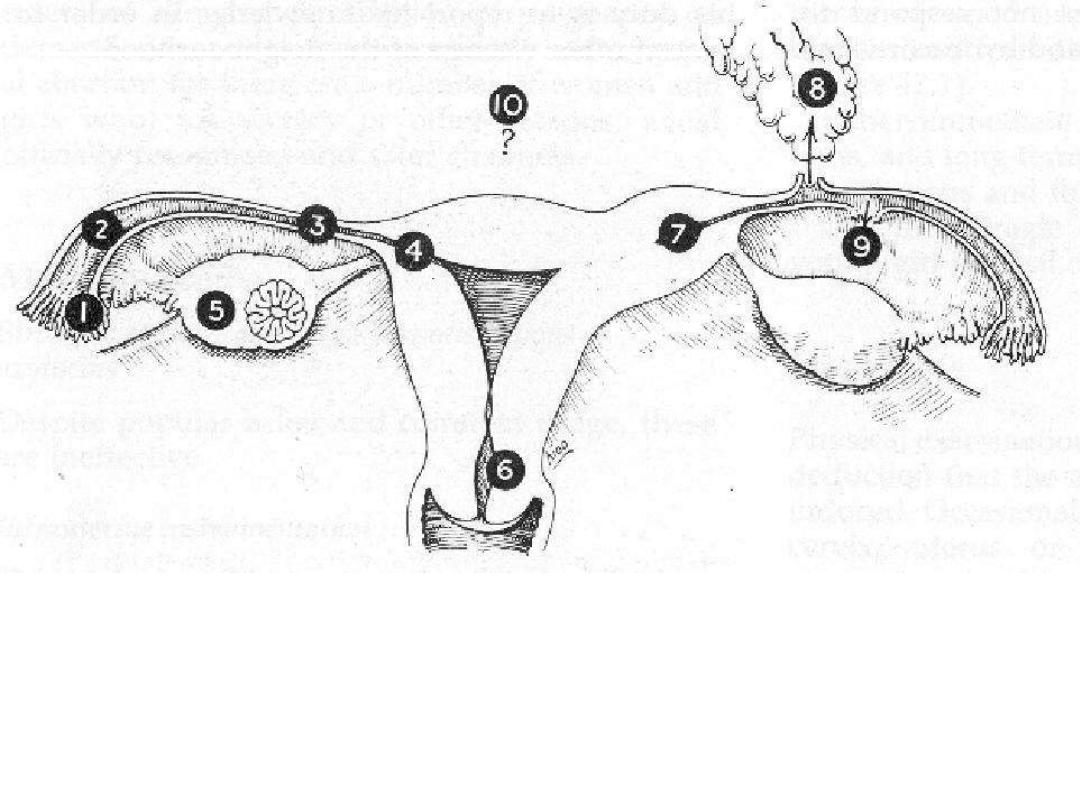
SITES OF ECTOPIC PREGNANCY
1)Fimbrial 2)Ampullary 3)Isthemic 4)Interstitial
5)Ovarian 6)Cervical 7)Cornual-Rudimentary horn
8)Secondary abdominal 9)Broad ligament 10)Primary
abdominal
Ampulla (>85%)
Isthmus (8%)
Cornual (< 2%)
Ovary
Abdomen (< 2%)
Cervix
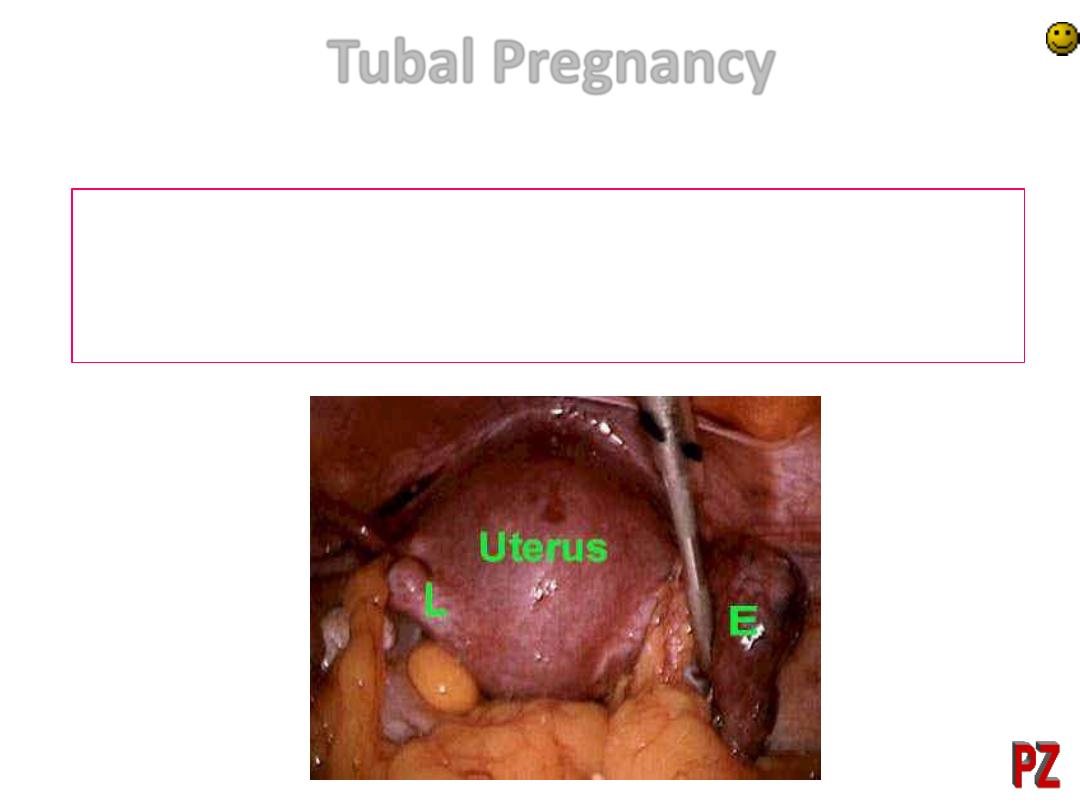
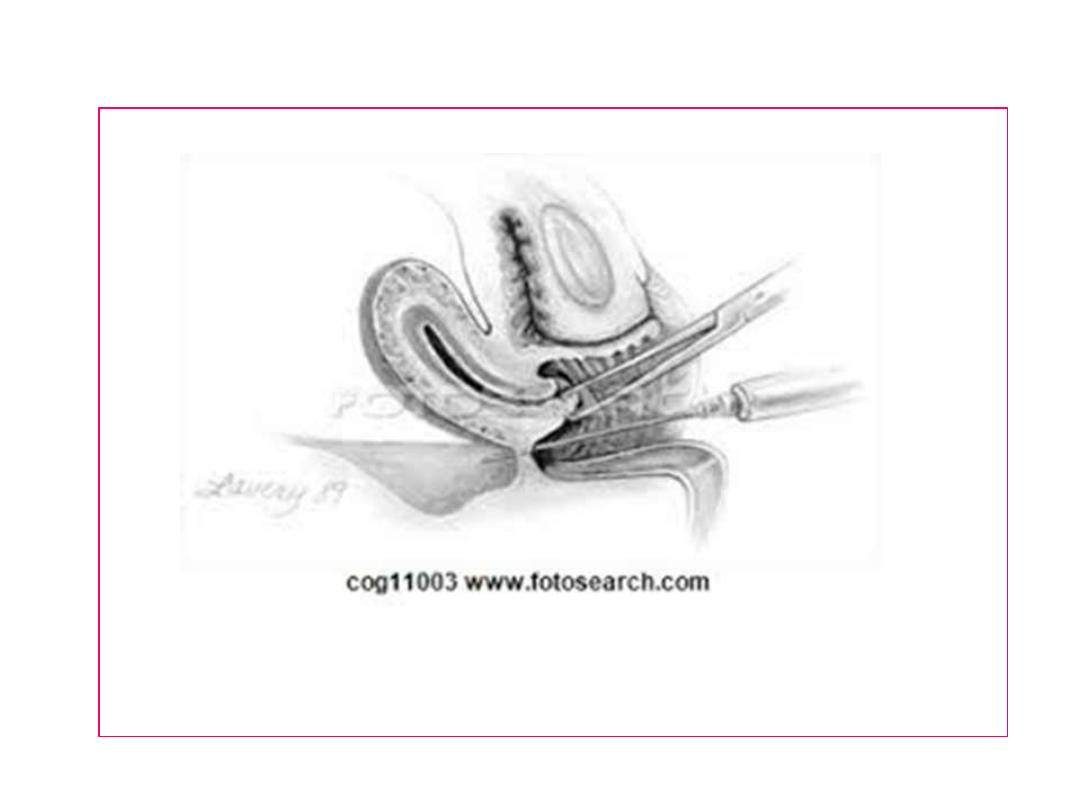
Tubal Pregnancy
•
A right tubal ectopic pregnancy seen at laparoscopy
•
The swollen right tube containing the ectopic pregnancy is on the right at E
•
The stump of the left tube is seen at L - this woman had a previous tubal
ligation
Uncommon Ectopics
• Intraligamentous pregnancy (in broad ligament)
• Pregnancy in a uterine diverticulum or sacculation
• Pregnancy in a rudimentary horn of uterus
• Multiple tubal pregnancy
• Cesarean scar pregnancy
intrauterine implantation
Ectopic implantation

Uterine Changes in Ectopic Pregnancy
The uterus undergoes some of the changes associated
with early normal pregnancy, including increase in size
and softening of the cervix and isthmus. (Lack of uterine
changes does not exclude an ectopic pregnancy).
– The finding of uterine decidua without trophoblast
suggests ectopic pregnancy but is not absolute.
Arias-Stella reaction:
Histologic findings, which is characterized by localized
hyperplasia of endometrial glands that are hypersecretory.
The cells have enlarged nuclei that are hyperchromatic and
irregular. The Arias- Stella reaction is a nonspecific finding
that can be seen in patients with intrauterine pregnancies.
External bleeding – from degeneration and sloughing of
uterine deciduas.
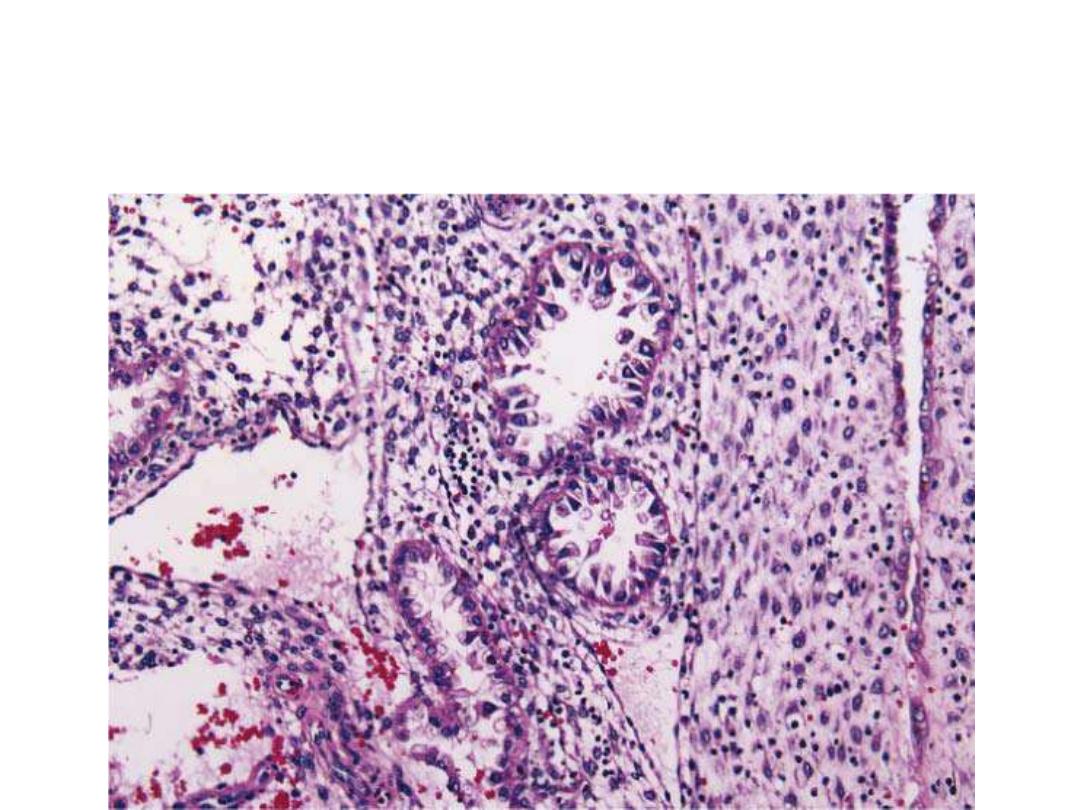
The Arias-Stella reaction of the endometrium.
The glands are closely packed and hypersecretory with
large, hyperchromatic nuclei
.
Risk Factors for Ectopic
Pregnancy
•
In theory, any mechanical or functional
factors that prevent or interfere with the
passage of the fertilized egg to the uterine
cavity may be aetiological factors for an
ectopic pregnancy.
Known aetiological factors contributing to the risk
of ectopic pregnancy are:
• tubal disease; pelvic infection, such as Chlamydia
infection, has been estimated to account for 40 per
cent of all ectopic pregnancies;
• previous ectopic pregnancy;
• previous tubal surgery;
• subfertility;
• use of intrauterine device
.
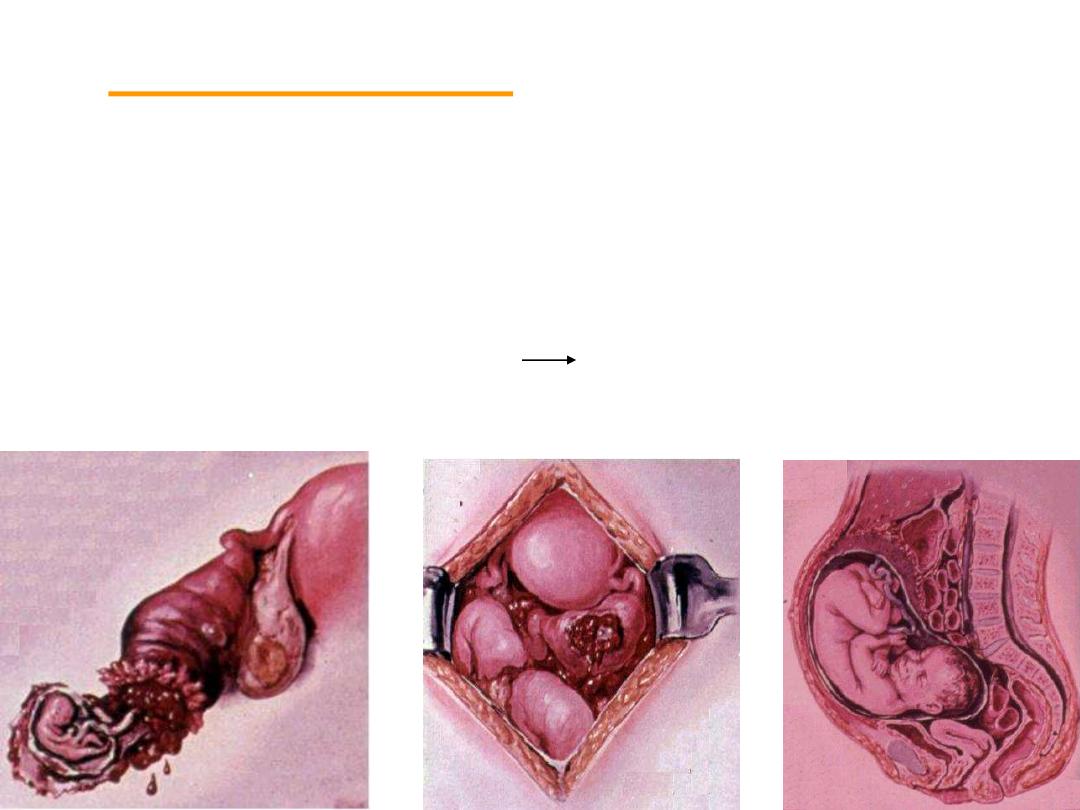
course and outcome
1.Tubal Abortion
2.Tubal Rupture
3.Continuation of Pregnancy
Secondary Abdominal pregnancy
CLINICAL APPROACH
• Dignosis can be done by history, detailed examination and
investigation.
• History of past PID, tubal surgery, current contraceptive
measures should be asked.
• Wide spectrum of clinical presentation from
asymptomatic
pt
to others with
acute abdomen
and in
shock
.
The classic symptom triad of ectopic pregnancy
is
pain
,
amenorrhea
, and
vaginal bleeding
.
This symptom group is present in only about
50%
of patients, however, and is most typical in
patients in whom an ectopic pregnancy has
ruptured.
Abdominal pain is the most common presenting
symptom, but the severity and nature of the
pain vary widely.
Shoulder pain, thought to result from
hemoperitoneal irritation of the diaphragm,
may indicate intraabdominal hemorrhage
The physical examination should include measurements of vital signs
and examination of the abdomen and pelvis. Frequently, the findings
before rupture and hemorrhage are nonspecific, and vital signs are
normal.
• Ruptured ectopic:
patient is restless, looks pale, sweating with
cold clammy skin. Features of shock, tachycardia, hypotension.
Abdomenal:-
abdomen may look distended (if significant
intraperitoneal haemorrhage is present), tenderness mostly in
lower abdomen, rebound tenderness, guarding & rigidity may be
present.
Pelvic:-
bimanual examination must be performed in an environment
where facilities for resuscitation are available, as this examination
may provoke the rupture of the tube.
• Enlarged uterus
•
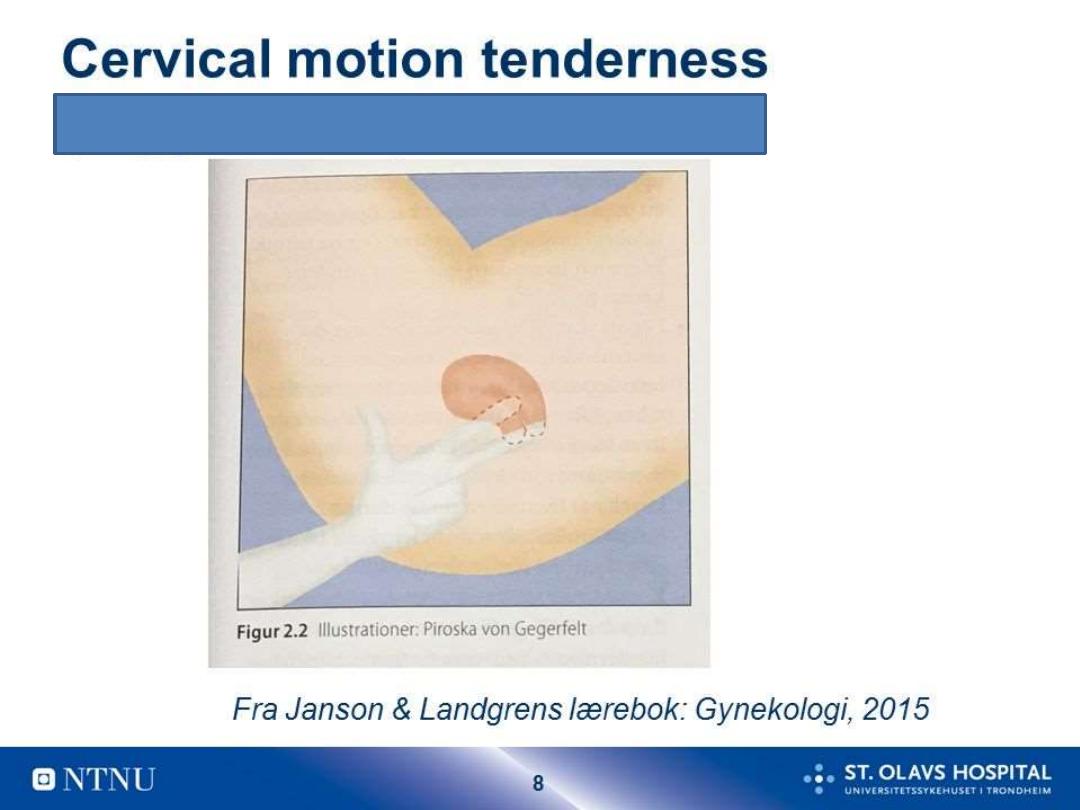
Cervical Motion Tenderness (cervical excitation test)
•
adnexal fullness or tenderness, sometime adnexal mass
• Cul-de-sac fullness
• Decidual cast (Passage of decidua in one piece)
•
vaginal bleeding may be present .
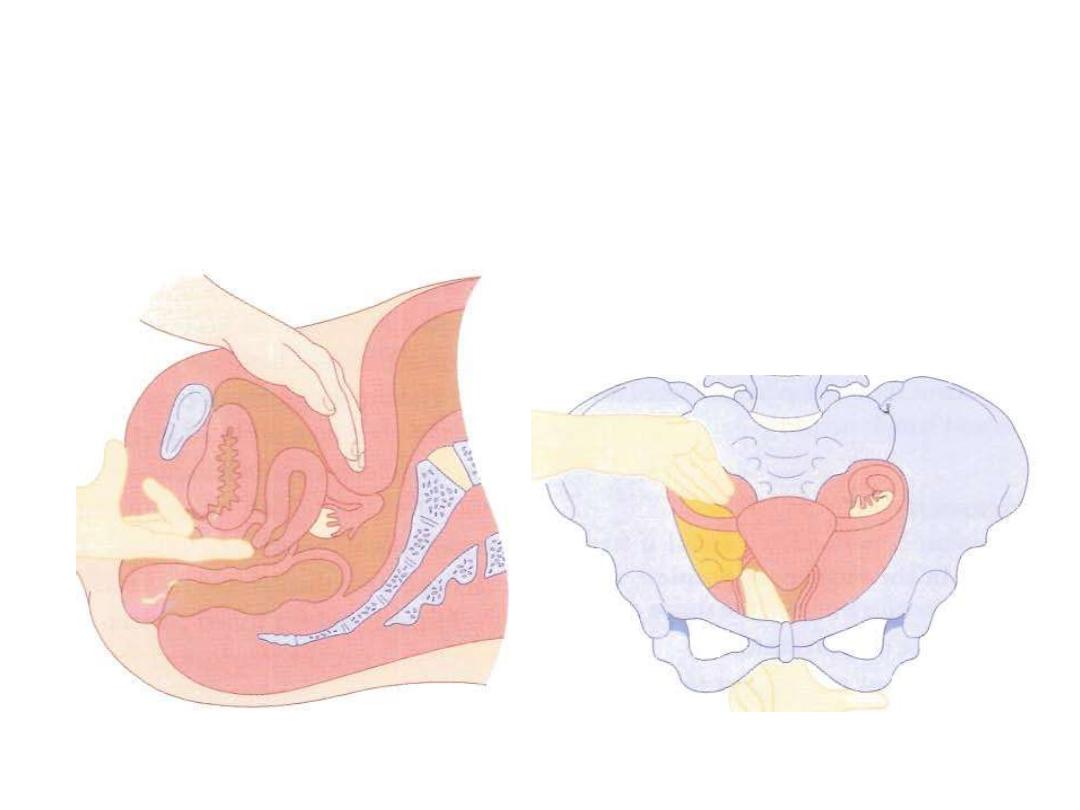
Bimanual examination of the pelvis
a. Assessing the uterus
b. Assessing the adnexia

CHRONIC ECTOPIC PREGNANCY
• It can be diagnosed by high clinical suspicion.
• Patient had previous attack of acute pain from which she has
recovered.
• She may have amenorrhoea, vaginal bleeding with dull pain
in abdomen, and with bladder and bowel complaints like
dysuria, frequency.
• Pelvic examination reveals that the uterus may be normal in
size or bulky, ill defined boggy tender mass may be felt in one
of the fornix.

In a woman of child bearing age with pelvi-
abdominal pain and/ or vaginal bleeding ……
ALWAYS….think
Diagnosis:
• In recent years, in spite of an increase in the
incidence of ectopic pregnancy there has been a
fall in the case fatality rate. This is due to the
widespread introduction of diagnostic tests and an
increased awareness of the serious nature of this
disease.This has resulted in early diagnosis and
effective treatment.
• Now the rate of tubal rupture is as low as 20%.

METHODS OF EARLY DIAGNOSIS
• Ultrasound scanning – Abdominal & Vaginal
including Colour Doppler
• Serum B-hCG: Immunoassay utilising
monoclonal antibodies to beta HCG
• Laparoscopy
• Serum progesterone estimation
not
helpful
A combination of these methods may have
to be employed.
Diagnosis
• Occasionally culdocentesis
Sometimes dilatation and curettage:
the diagnostic value of curettage is very limited

Ultra Sonography:
Transvaginal ultrasound is the diagnostic tool of choice for tubal
ectopic pregnancy.
Tubal ectopic pregnancies should be positively identified, if
possible,
by visualising an adnexal mass that moves separate to the ovary.
sonographic finding in ectopic pregnancy include the following;-
An inhomogeneous or noncystic adnexal mass is the most
common finding.
An empty extrauterine gestational sac
An extrauterine gestational sac containing a yolk sac c and/or
embryonic pole that may or may not have cardiac activity.
(Live embryo (fetal heart positive) in adnexa is the most specific but
least sensitive sign of ectopic pregnancy, occurring in only 10% to
17% of cases).

In up to 20% of cases, a collection of fluid may
be seen within the uterine cavity, classically
referred to as a
‘pseudosac’.
The key is to
distinguish this from an early intrauterine
gestational sac.
Free fluid is often seen on ultrasound , but is
not diagnostic of ectopic pregnancy. A small
amount of anechoic fluid in the pouch of
Douglas may be found in both intrauterine
and ectopic pregnancies.
-
Negative pelvic U/S does not exclude ectopic
pregnancy.
2. β-HCG Assay: may be helpful in the diagnosis in the following
ways:
*Serum β-HCG test are positive in 99% of ectopic pregnancy
*Serial estimation of β-HCG concentration;
In 85 per cent of pregnancies, the bHCG levels almost double every
48 hours in a normally developing pregnancy. In patients with
ectopic pregnancies, the rise of bHCG is often suboptimal.
However, bHCG levels can vary widely in individuals and thus often
multiple readings are required for comparison purposes.
*
β-HCG with U/S (dicriminatory zone);
B-hCG level above which a viable intrauterine pregnancy should be visualized by TV
US. This is usually taken as 1000-1500mIU/ml.
With use of transabdominal Sonography a normal intrauterine pregnancy could be
seen in most cases when serum β-HCG exceeded 6500 IU/L & with transvaginal
Sonography this threshold can be as low as 1500 IU/L
If there were discrepancy between the bHCG concentrations and that seen on
ultrasound scan (e.g. a high bHCG with no intrauterine pregnancy on ultrasound scan),
the differential diagnosis of an ectopic pregnancy must be made.
A meta-analysis has confirmed that a single b-hCG level cannot be used in isolation to
predict an ectopic pregnancy.
*ß-hCG assay is negative (when less than 5 mIU/mL);
this mostly exclude ectopic
pregnancy.
•
A serum beta-human chorionic gonadotrophin (b-hCG) level is useful for planning the
management of an ultrasound visualised ectopic pregnancy.

Diagnostic modalities
If early pregnancy problems
…. Urine B-hCG +
AScan
Intra-uterine pregnancy
…….GOOD
No Intra-uterine gestation Seen
…… serum B-hCG + TVS.
with serum B-hCG of 1500-2000 ml I.U/ml Intra uterine gestation should
be seen using TVS
…… otherwise suspect Ectopic pregnancy
When B-hCG below the discriminatory zone
…..serial B-hCG estimation
or laparoscope.
The choice of diagnostic algorithm applies only to
hemodynamically stable women; those with presumed
rupture should undergo prompt surgical therapy

MANAGEMENT
Depending on the presentation:
Acute
… with ruptured ectopic and intra-abdominal bleeding….
ABC,,, + surgical approach.
Early stages
, with intact ectopic:
1. Expectant
… decreasing B-hCG …. Tubal abortion
2. Medical
… Depending on size of ectopic and level of B-hCG…..
Use methotrexate.
3. Surgical
Methotrexate Treatment
• methotrexate has been found to be equally successful to
surgery in certain cases of tubal ectopic pregnancy (overall
success rate 65– 95%).
• methotrexate is most commonly given as a single
intramuscular dose of 50 mg/ m
2
• Serum b-hCG levels are measured on days 4 and 7 post
methotrexate:
o
If the b -hCG level decreases by more than 15% between
days 4 an d 7, b-hCG levels are then measured weekly until
less than 15 iu/ l.
o
If the level does not decrease by 15%, a repeat transvaginal
ultrasound should be considered to exclude ectopic fetal
cardiac activity and the presence of significant
haemoperitoneum . Consideration may then be given to
administration of a second dose of methotrexate.
•
Systemic methotrexate may be offered to
suitable women with a tubal ectopic
pregnancy. It should never be given at the first
visit, unless the diagnosis of ectopic
pregnancy is absolutely clear and a viable
intrauterine pregnancy has been excluded.
Candidate for methotrexate treatment:
The best candidates for methotrexate treatment
are women with:
• asymptomatic ectopic pregnancy,
• who have high compliance,
• serum hCG of < 5000 mIU/ml,
• adnexial mass < 3.5 cm on US scan,
• no cardiac activity on ultrasound
• and no contraindication to methotrexate.
INSTRUCTION TO THE PATIENTS
If treatment on outpatient basis rapid transportation should be
available
Refrain from alcohol, sunlight, multivitamins, NSAIDs and sexual
intercourse.
Report immediately when vaginal bleeding, abdominal pain,
dizziness, syncope (mild pain is common called separation pain or
resolution pain)
Failure of medical therapy require retreatment
Chance of tubal rupture in 5-10 % require emergency laparotomy.
Contraindications & Side effects of
Methotrexate
The few contraindications to medical treatment include :
• (1) chronic liver, renal or haematological disorder;
• (2) active infection;
• (3) immunodeficiency; and
• (4) breastfeeding.
There are also known side effects such as nausea,
vomiting, stomatitis, conjunctivitis, gastrointestinal upset,
photosensitive skin reaction and about two-thirds of
patients suffer nonspecific abdominal pain.
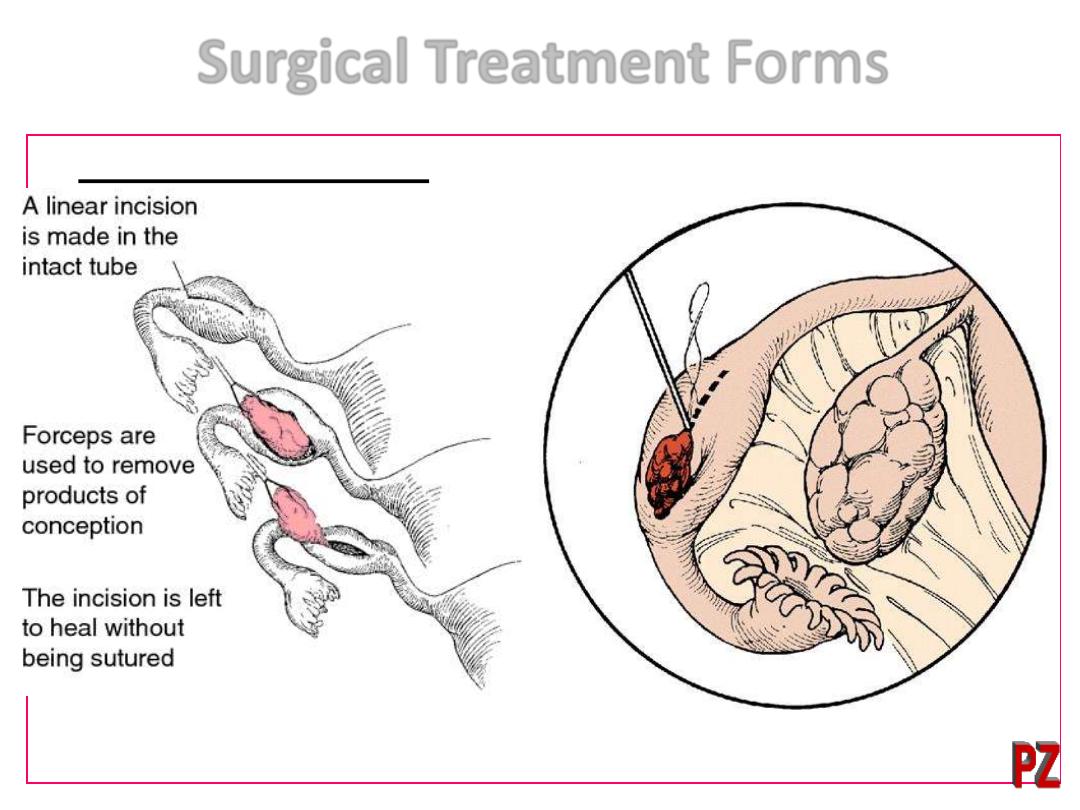
Surgical Treatment Forms
• Conservative surgery:
• Salpingostomy: Making an incision on the tube and
removing the pregnancy and leaving the incision without
suturing.
–
Salpingotomy: procedure is the same as salpingostomy
except that the incision is closed with a suture
• Fimbrial expression: "Milking" the pregnancy out the end of
the tube
• Radical surgery:
• Salpingectomy: Cutting the tube out

• Approach:
• Usually, if the tube is not ruptured → laparoscopy
• Cases of rupture with significant hemorrhage into
the abdomen → laparotomy
• A laparoscopic surgical approach is preferable to an open
approach.
• In the presence of a healthy contralateral tube,
salpingectomy should be performed in preference to
salpingotomy.
• In women with a history of fertility-reducing factors
(previous ectopic pregnancy, contralateral tubal damage,
previous abdominal surgery, previous pelvic
inflammatory disease), salpingotomy should be
considered.

Ectopic pregnancy is a life threatening condition & on the increase
Not all cases present with a classical picture
ALWAYS suspect ectopic pregnancy in a woman of a child-
bearing age c/o pain and/or p.v. bleeding
Even if woman has ectopic, first urine pregnancy test may be
negative
!
Early diagnosis and management is feasible, which should be
available in referral centers
Tailor your management on the patient presentation.+/_ F.up
