
Congenital Malformations of female gential organs
Embryology Related to Development in Males and Females ;
The sexual differentiation depends on sex determining region
(SRY region) present on short arm of Y-chromosome.
If Y-chromosome is present → gonads which are initially
bipotential develop into testes (7 weeks)
If SRY region is absent, i.e. Y chromosome is absent → gonads
develop into ovaries
Development of External Genital Organs in Females ;
The external genital organs start developing almost
simultaneously with the development of the internal genital
organs. The site of origin is from the urogenital sinus.
Clitoris is developed from the genital tubercle.
Labia minora are developed from the genital folds.
Labia majora are developed from the genital swellings.
The Bartholin’s glands are developed as outgrowths from the
caudal part of the urogenital sinus and correspond to the
bulbourethral glands of male

The vestibule develops from inferior portion of the pelvic part
and whole of the phallic part of the urogenital sinus.
Female genital development is complete by 11 weeks.
Development of Internal Genital Organs;
The major part of the female genital tract develops from the
Mullerian ducts.
Development of Mullerian ducts/paramesonephric ducts in
females
In the 5th-6th week of intrauterine life of the embryo mullerian
ducts develop as an invagination of intermediate cell mass. Two
Mullerian ducts develop, one on either side and grow caudally.
They approach each other in the midline after crossing the
Wolffian duct and fuse. Fusion begins by 7–8 weeks and is
completed by 12 weeks.
The cervix can be differentiated from corpus by 10th week.
Fusion proceeds in below upwards direction. Initially when the
two Mullerian ducts fuse, an intervening septum is present but
later by 5th month of intrauterine life, it also disappears.
Development of Vagina;
Vagina develops from two sources: Mainly from the Mullerian
duct (forms upper 3/5th part) Partly from the urogenital sinus

(forms lower 1/5th part) which together form a solid vaginal
plate. Canalization of the solid vaginal plate occurs at 20 weeks
.
If this canalization fails to occur it leads to – transverse vaginal
septum. The mucous membrane of vagina is derived from
endoderm of urogenital sinus and muscles from mesoderm of
mullerian duct.
Development of Ovary ;
Ovaries are formed because of absence of y chromosome. For
proper development of ovaries-presence of two X
chromosomes is required. This is the reason why- in Turner’s
syndrome (45X0) ovaries are not developed properly-called as
streak gonads. WNT-4 is the ovary determining gene.The ovary
is developed from the genital ridge. Genital ridge appears at 5
weeks of POG. The cortex and the covering epithelium are
developed from the coelomic epithelium and the medulla from
the mesenchyme. The germ cells are ectodermal in origin and
migrate to the yolk sac (at 2 weeks) and to the genital ridge (3
weeks). The estimated number at birth is about 2 million. The
ovaries descend during seventh to ninth months, and at birth,
they are situated at the pelvic brim.

Notes;
Mullerian Ducts Form
• Both the fallopian tubes
• Uterus
• Cervix
• Upper part of vagina
Ovaries are not formed by Mullerian duct hence in Mullerian
agenesis – ovaries/ovulation is normal .
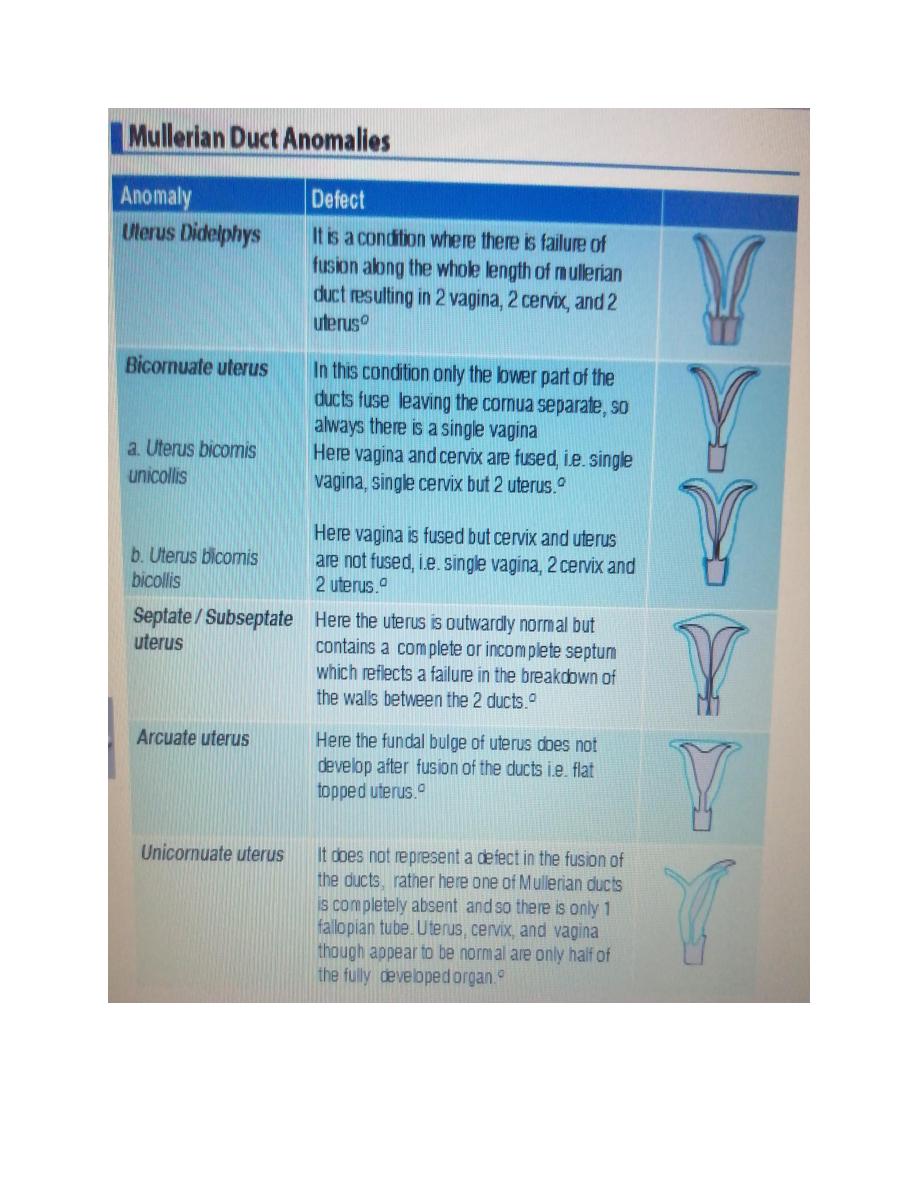

WHO classification of Mullerian anomalies;
Class I Mullerian agenesis (MRKH syndrome)
Class II Unicornuate uterus
Class III Didelphys uterus
Class IV Bicornuate uterus
Class V Septate uterus Class VI Arcuate uterus
Class VII DES related abnormalities/T shaped uterus
Diagnosis ;
HSG: Hysterosalpingogram (HSG) is mainly preferred in uterine
anomalies but it cannot distinguish between a septate and
bicornuate uterus. This is because in order to distinguish
between the two, uterine fundus should be visible.
IOC: MRI followed by 3 dimension USG
Gold Standard — Laparoscopy
Management of Bicornuate or Septate Uterus Presence of
uterine malformation per se is not an indication of surgical
correction. Unification operation is indicated in otherwise
unexplained cases of infertility or if it has lead to ≥ 3 abortions.
Options Include For bicornuate uterus: (and if needed for
Didelphys uterus) Unification surgery (done either

hysteroscopically or by abdominal route- Strassman
metroplasty). For septate uterus: Earlier: Jones/Tompkins
metroplasty was done. Nowadays: Hysteroscopic resection of
septa is being done after inducing endometrial atrophy by
administering GnRH analogue for 2 months. Main
complications: Uterus perforation and fluid overload.
Transverse Vaginal Septum ;
If there is a disorder in fusion of downgrowing Mullerian duct
and upgrowing derivative of urogenital sinus, results in
transverse vaginal septum which causes imperforate vagina (or
vaginal agenesis). 46% septa are located in upper part. 40%
septa are located in middle part.Q 14% septa are located in
lower part. Transverse vaginal septum can present either in :
Neonatal Age-group ; The placental transfer of estrogen results
in stimulating the glands of the endocervix which results in
formation of mucocolpos, and can present as: Abdominal
tumour. Can compress the ureter resulting in hydroureter
followed by hydronephrosis. Can compress the rectum resulting
in obstipation/intestinal obstruction.
At Puberty ; Patient can present with primary amenorrhea
(actually called as cryptomenorrhea as uterus menstruates
normally but blood does not come out due to outflow tract

obstruction). Secondary sexual characteristics are normal. Due
to cryptomenorrhoea, blood gradually collects and distends
first the vagina (hematocolpos) then cervix, uterus
(hematocervix and hematometra) and finally the tube
(hematosalpinx). All these present as pelvic/abdominal tumor.
The abdominal tumor can irritate the bladder followed by
compression of internal urinary meatus leading to complete
retention of urine (This occurs 3–4 years after the onset of
hidden menstruation and therefore, patient is generally aged
15–18 years). Patient may complain of monthly cyclic pain
(backache/lower abdomen pain).
Management ; In case of septa in lower and middle part of
vagina- surgical removal of septa vaginally followed by
reanastomosis. In case of upper septa, abdominal surgery is
required.
Mullerian Agenesis ;
is the complete failure in the development of the mullerian
ducts, resulting in absence of the fallopian tubes, uterus, and
most of vagina (as 2/3rd of vagina is formed by Mullerian duct).
Karyotype = 46 XX. Phenotype = Female .Associated
AbnormalitiesRenal anomalies (M/C Renal agenesis followed by
horse-shoe shaped kidney). Skeletal abnormalities (most
common - scoliosis). Cardiac anomalies. When mullerian

agenesis is associated with Renal anomalies and skeletal
anomalies-it is called Mayer Rokitansky Kuster Hauser
syndrome.
Clinical Features ; Patient present between 15–18 years of age
with primary amenorrhoea. Secondary sexual characteristics
are normalas ovaries are normal (because ovaries do not
develop from mullerian duct but from genital ridge, so
ovulation is also normal) i.e. breast, pubic hair and axillary hair
all are normal.
P/V = Vagina is felt like a blind pouch and uterus is absent.
“Although in MRKH fallopian tube should be absent, typically a
part of the distal tube is present (distal 1/3rd present). Findings
are confirmed by USGQ.
Management ;Repair of vaginal agenesis is done either by frank
dilatation or vaginoplasty. Vaginoplasty should only be
performed when the girl is just married or about to be married.
Surgical management: Vaginoplasty either by McIndoe reed
procedure or Williams vaginoplasty or amnion vaginoplasty.
These females are capable of having their biological child
because their ovares are normal hence - oocyte can be,
pickedup and with husband semen, IVF can be done Zygotes
are then transferred to surrogate mothers uterus.
Frank Dilatation This non-surgical procedure consists of a
woman applying gradual pressure with progressively increasing

dilators over the mullerian pit for 15 minutes twice a day. An
indentation is created by the end of 3 to 6 month. Some have
satisfactory intercourse, but in many, vaginal size is inadequate
and they need a surgical procedure eventually.
