Traveller's diarrhea:
Diarrhea is the leading cause of illness in traveller's and it is usually
short lived (2-5 days), self limited condition occur commonly in
visitors of developing countries.
The most common identified pathogen causing traveller's diarrhea
is toxigenic E.coli, however campylobacter infection appear to
predominate in other parts of the world. Other common causative
organism include salmonella, Shigella, rota virus and the Norwalk
agent. Other less common cause include giardiasis and to less extent
vibriosis.

Clinical features:
1-The onset is usually abrupt.
2- The stool is watery.
3- Abdominal cramps.
4-Anorexia and vomiting.
5-Fever may be present.
6-Examination of the abdomen:
Shows no abnormality or occasionally diffuse tenderness.

Treatment:
1- The disorder usually resolve spontaneously.
2-Antidiarrhoeal agent are best avoided as they may occasionally cause toxic
dilatation of the colon.
3-Loperamide 4mg and fluid replacement may be sufficient.
4-Antibiotics is useful in reducing the frequency of bowel movement and
duration of illness in moderate to severe diarrhea only (3 day course of
quinolone taken twice daily). Azithromycin may be a better choice in a
quinolone resistant cases.

Prevention:
Involves good hygien, clean water and avoiding uncooked
vegetables. Doxycyclin 100mg or trimetheprim 80gm or quinolone
single daily dose is effective for susceptible individuals.

Malaria
•
Learning objectives
•
1
-
Pathogenesis and life cycle
•
2
-
Effects on RBC
•
3
-
Clinical features
•
4
-
Complications
•
5
-
Investigations
•
6
-
Management and prevention

Malaria:
Malaria is a protozoan disease transmitted by the bite of infected
anopheles mosquitoes. Human malaria is caused by plasmodium
falciparum, P. vivax, P. ovale, P.malariae. malaria is a predominantly a
disease of hot climates, however it may occur in other parts of the
world such as Europe. Less frequent modes of transmission include
blood transmission or injection and transplacental infection.

Pathogenesis and life cycle:
Almost all deaths are caused by falciparum malaria. Human
infection begins when a female anopheline mosquito inoculates
plasmodial sporozoites from its salivary gland during a blood meal
which carried rapidly via the blood to the liver, invading hepatic cells
and begin a period of asexual reproduction. This process producing
pre-erythrocytic (schizogony) in which a single sporozoite eventually
produce 10000-30000 daughter merozoites.

At this stage symptomatic infection begins. In P-vivax and P-ovale
infections, a proportion of the intrahepatic forms do not divide
immediately but remain dormant for months to years before
reproduction begins. These dormant forms (hypnozoites) are the
cause of the replaces that characterize infection with these 2-
species. Merozoites invade erythrocytes and become trophozoites.
Attachment is mediated via a specific erythrocyte surface receptor
In the case of P-vivax this receptor is related to the duffy blood group
antigen. Most west Africans and people that carry the duffy negative
phenotype are therefore resistant to P-vivax malaria, this stage of
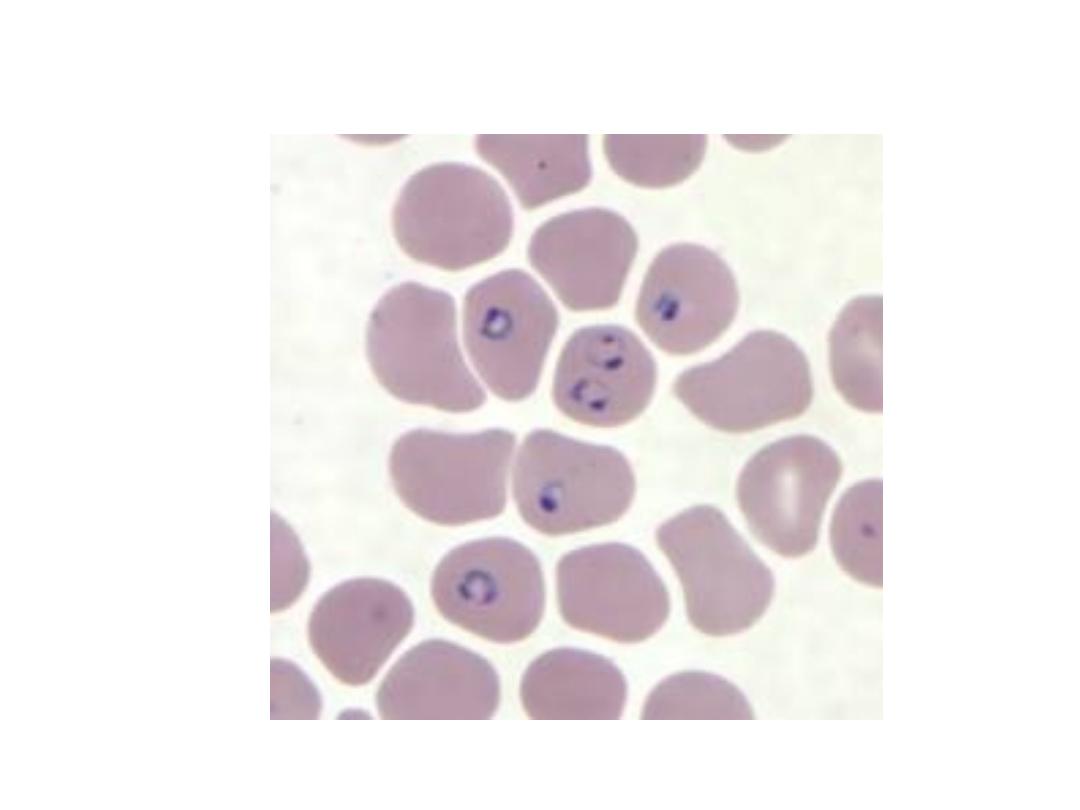
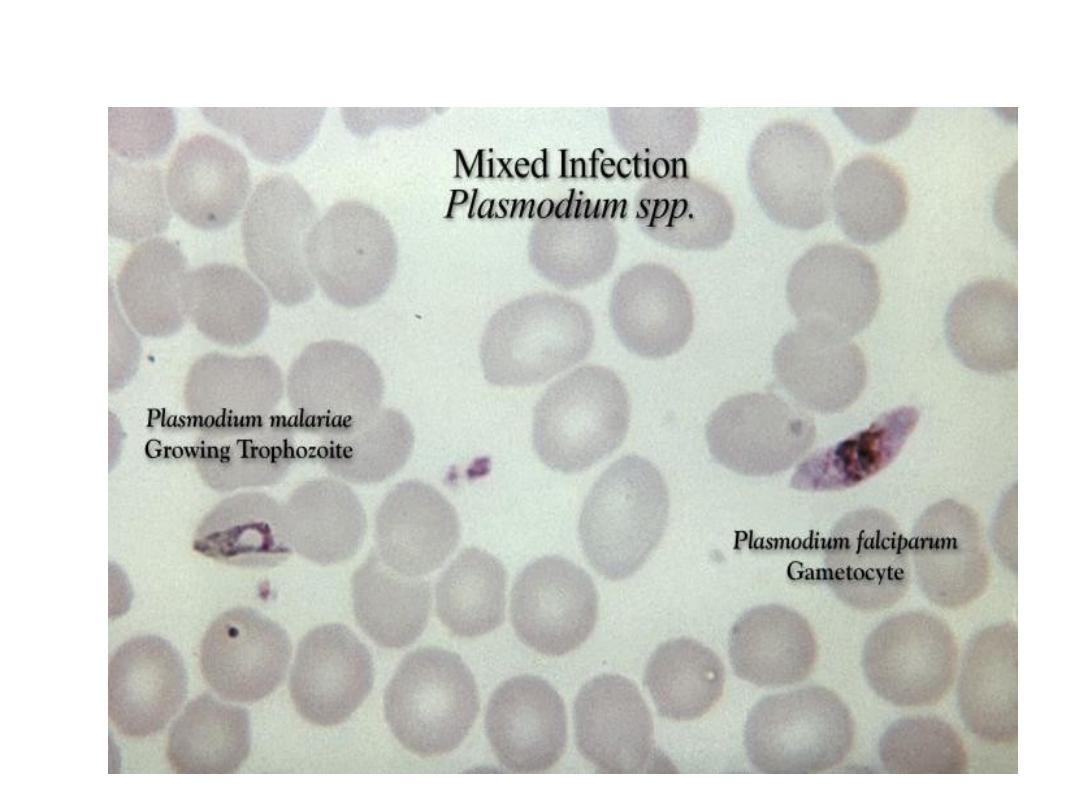
development appear as a small ring forms intraerythrocytic under
light microscopy
.

By the end of the 48 hours intraerythrocytic life cycle (72 hours for P-
malaria) the parasite grown to occupy most of the red cell. Multiple
nuclear divisions take place (merogony), and the red cells rupture to
release 6-30 daughter merozoites, each capable of invading a new
red cell and repeating the cycle. Some of the parasite develop into a
morphologically distinct long lived sexual forms (gametocytes) that
can transmit malaria
.
Effects on red blood cells
:

Malaria is always accompanied by haemolysis and in a severe or
prolonged attack anaemia may be profound. The causes of anaemia
in malaria may be due to:
1- Haemolysis of infected RBC.
2- Haemolysis of uninfected RBC.
3- Dyserythropoiesis.
4- Splenomegally causing erythrocyte sequestration.
5-Depletion of folate stores.

Haemolysis is most severe with P-falciparum, which invades red cells
of all ages but especially young cells. P-vivax and ovale invade
reticulocyts and P-malaria invade normoblast, so that infections
remain lighter. Sequestration of red cells containing mature parasite
in P-falciparum occur which interfere with microcirculation
especially in the vital organs which defence the parasite and as a
consequence only the younger ring forms of the parasites are seen in
the peripheral blood in falciparum malaria
.

In the other three (benign) malarias, sequestration doesn't occur and
all stages of the parasites development are evident on peripheral
blood smears.
P-falciparum doesn't grow well in red cells that contains HbF, C or
especially S. Hbs hetrozygotes are protected against the lethal
complications of malaria which might be related to the low oxygen
tensions.
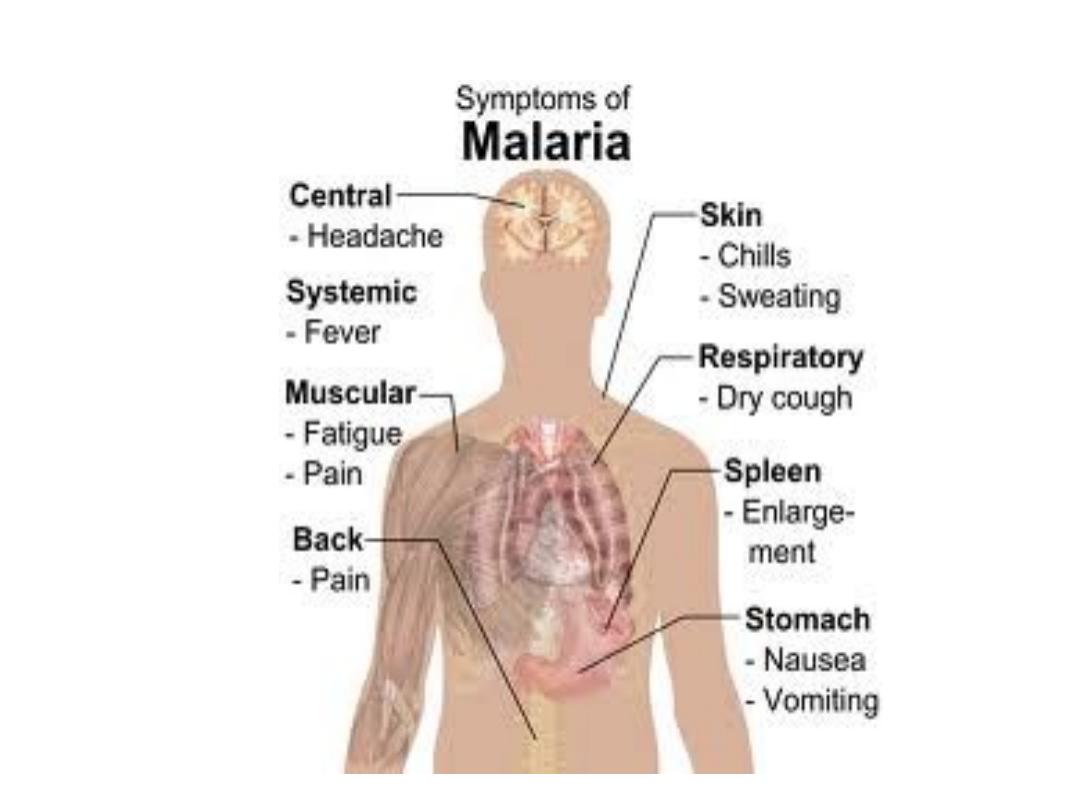
Clinical features
:

1- The first symptoms of malaria are nonspecific:
The lack of a sense of well being, headache, fatigue, abdominal
discomfort and muscle ache followed by fever.
2- Headache may be severe in malaria however there is no neck
stiffness or photophobia as that seen in meningitis.
3-Nausea, vomiting and orthostatic hypotension are common.

4
-
The classical malaria paroxysms in which fever occur at regular
intervals suggest infection with P-vivax or P-ovale. Fever starts with a
rigor ,the patients feels cold and the temperature rises to about 40C°
after half an hour to an hour the hot or flush phase begin. It last
several hours and gives way to profuse perspiration and gradual fall
in temperature. The cycle is repeated 48 hours later. Gradually the
spleen and liver enlarge and may become tender. Anaemia develops
slowly. Replaces are common two years after leaving the endemic
area
.

5- P-malaria infection: fever occur in bouts every third day. (parasitaemia
may persist for many years with or without symptoms). P-malaria causes
GN and nephritic syndrome in children.
6- P-falciparum
infection: more dangerous than other forms of malaria.
The onset is often insidious with malaise, headache and cough. Cough and
mild diarrhea are common.
Fever has no particular pattern, jaundice is common due to haemolysis
and hepatic dysfunction. The liver and spleen enlarged and become
tender. Anaemia develops rapidly. Splenoctomy increases the risk of
severe malaria.
Complications of malaria due to P-falciparum

1- Sever anaemia.
2- Organ damage due to anoxia.
- Brain (confusion, coma).
- Kidney's (oligurea, uraemia due to acute tabular necrosis).
- Lungs (cough, pulmonary oedema).
- Intestine (diarrhoea, congestion).
- Liver (jaundice, encephalopathy which is rare).

3
-
Intravascular haemolysis (black water fever): this is associated
with chronic falciparum malaria, most commonly in those who take
antimalarial treatment irregularly or are deficient in G6PD.
Haemolysis is unpredictable and severe, destroying uninfected as
well as infected red cells. The urine is dark or black
.

4- Hypoglycemia especially with quinine treatment.
5- Shock secondary to septicaemia.
6- Hypotensive shock.
7- Metabolic acidosis.
8- Splenic rupture.
9- Complication during pregnancy (maternal death, abortion, still
birth, low birth weight).
Tropical splenomegally syndrome (hyperreactive malarial
splenomegally):

In some hyperendemic areas gross splenomegaly is associated with
an exaggerated immune response to malaria and is seen more
common in adult. The condition is more common in female and in
certain ratial and family groups and is characterized by over
production of IgM. IgM aggregates are phagocytosed by
reticuloendothelial cells in the spleen and liver. Light microscopy of
the liver usually shows sinusoidal lymphocytosis. Anaemia and
lymphocytosis can be confused with leukaemia. Portal hypertension
may develop
.

Investigations:
Malaria should be considered if febrile patients is in or has
recently left a malarias locality.
1- Thick and thin blood films should be repeated if necessary. In P-
falciparum only ring forms are normally seen in the early stages.
(Gametocytes may persist despite treatment and are harmless).

2- Immunochromatographic (Dip sticks test for P-falciparum antigen
are non microscopic means of diagnosis) they should be used in
parallel with blood film examination.

D.DX:
Other causes of fever with splenomegally in the tropics should be
considered such as T.B, visceral leishmaniasis, schistosomiasis,
chronic brucellosis in addition to leukaemia and lymphoma.

Management:
1- For all infections with P-vivax, P-ovale and P-malaria the drug of
choice is chloroquin (600 mg base followed by 300mg base in six
hours then 150 mg base twice daily for 2 more days). P-falciparum is
now resistant to chloroquin and so not used to treat this type of
malaria except in an area of chloroquin sensitivity.

2- Quinine dihydrochloride or sulphate 600 mg eight hourly until the
blood is free of parasite (3-5 days) then followed by a single dose of
sulfadoxine with pyrimethamine (3 tablets of fansidar). In pregnancy
a seven day course of quinine should be given.
3- Alternative to quinine + fansidar are mefloquin.

4- In complicated P-falciparum quinine is given as an I.V infusion over
4 hours (10mg/kg up to 700 mg repeated 8-12 hourly until the
patient can take drug orally). Intramuscular quinine may cause
necrosis of muscle.
5- In comatose patient L.P may be indicated to exclude co-existing
bacterial meningitis.

6-Severe anaemia requires transfusion, careful attention to fluid
balance is essential. Oligurea can be treated by frusemide or infusion
of manitol. Exchange transfusion is life saving in complicated very
heavy infection (> 10% of red cell infected). Hypoglycaemia and
septicaemia should be treated. Dialysis may be needed if renal failure
is developed.

Prevention:
Clinical attacks of malaria may be preventable by drugs such as
proguanil which attack the preerythrocytic form or by drugs such as
chloroquin or mefloquine after it has inter the erythrocyte.
Chemotherapy is begun one week before entering the malarias area
and is continued until 4-weeks after leaving it. Chloroquine over 5
years may cause irreversible retinopathy. (proguanil and chloroquine
is safe during pregnancy). Mefloquine is contraindicated in the first
trimester of pregnancy. Fansidar should not use for chemoprophylaxis
as it may cause death from agranulocytosis or Stevens Johnson's
syndrome. Mefloquine is useful in areas of multiple drugs resistant.
