Dr. Mohamed Ghalib
Internal Medicine
TUCOM
5
th
year
Osteoarthritis
Osteoarthritis (OA) is by far the most common form of arthritis
and is a major cause of pain and disability in older people.
It is characterised by focal loss of articular cartilage, subchondral
osteosclerosis, osteophyte formation at the joint margin, and
remodelling of joint contour with enlargement of affected joints.
Epidemiology
The prevalence rises progressively with age and it
has been estimated that 45% of all people develop
knee OA and 25% hip OA at some point during life.
Although some are asymptomatic, the lifetime risk
of having a total hip or knee replacement for OA in
someone aged 50 is about 11% for women and 8%
for men in the UK. There are major ethnic
differences in susceptibility: the prevalence of hip
OA is lower in Africa, China, Japan and the Indian
subcontinent than in European countries, and that of
knee OA is higher.
Pathophysiology
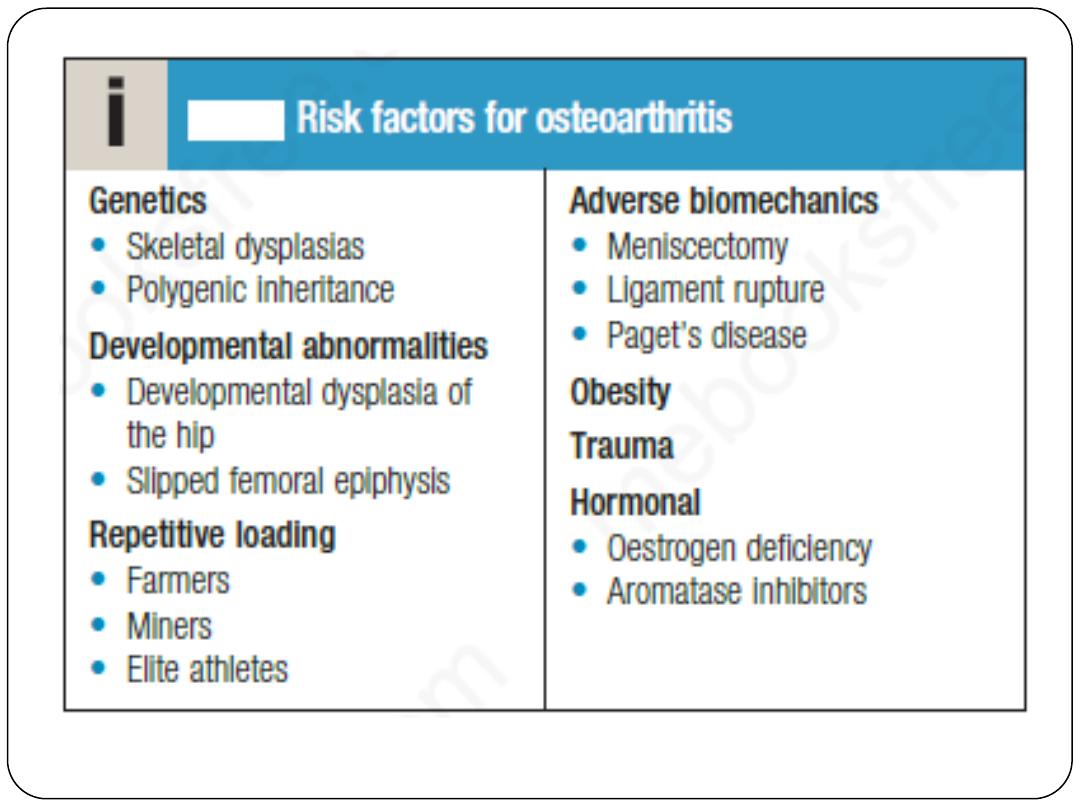
OA is a complex disorder with both genetic and environmental
components.
Genetic factors are recognised as playing a key role in the pathogenesis
of OA. Family-based studies have estimated that the heritability of OA
ranges from about 43% at the knee to between 60% and 65% at the hip
and hand, respectively. In most cases, the inheritance is polygenic and
mediated by several genetic variants of small effect.
OA can, however, be a component of multiple epiphyseal dysplasias,
which are caused by mutations in the genes that encode components of
cartilage matrix.
Structural abnormalities, such as slipped femoral epiphysis and
developmental dysplasia of the hip, are also associated with a high risk
of OA, presumably due to abnormal load distribution across the joint.
Biomechanical factors play an important role in OA related to certain
occupations, such as farmers (hip OA), miners (knee OA) and elite or
professional athletes (knee and ankle OA). It has been speculated that the
higher prevalence of knee OA in the Indian subcontinent and East Asia
might be accounted for by squatting.
There is also a high risk of OA in people who have had destabilising
injuries, such as cruciate ligament rupture, and those who have had
meniscetomy.
For most individuals, however, participation in recreational sport does not
appear to increase the risk significantly.
There is a strong association between obesity and OA, particularly of the
hip. This is thought to be due partly to biomechanical factors but it has also
been speculated that cytokines released from adipose tissue may play a
role.
Oestrogen appears to play a role; lower rates of OA have been observed
in women who use hormone replacement therapy (HRT), and women
who receive aromatase inhibitor therapy for breast cancer often
experience a flare in symptoms of OA.
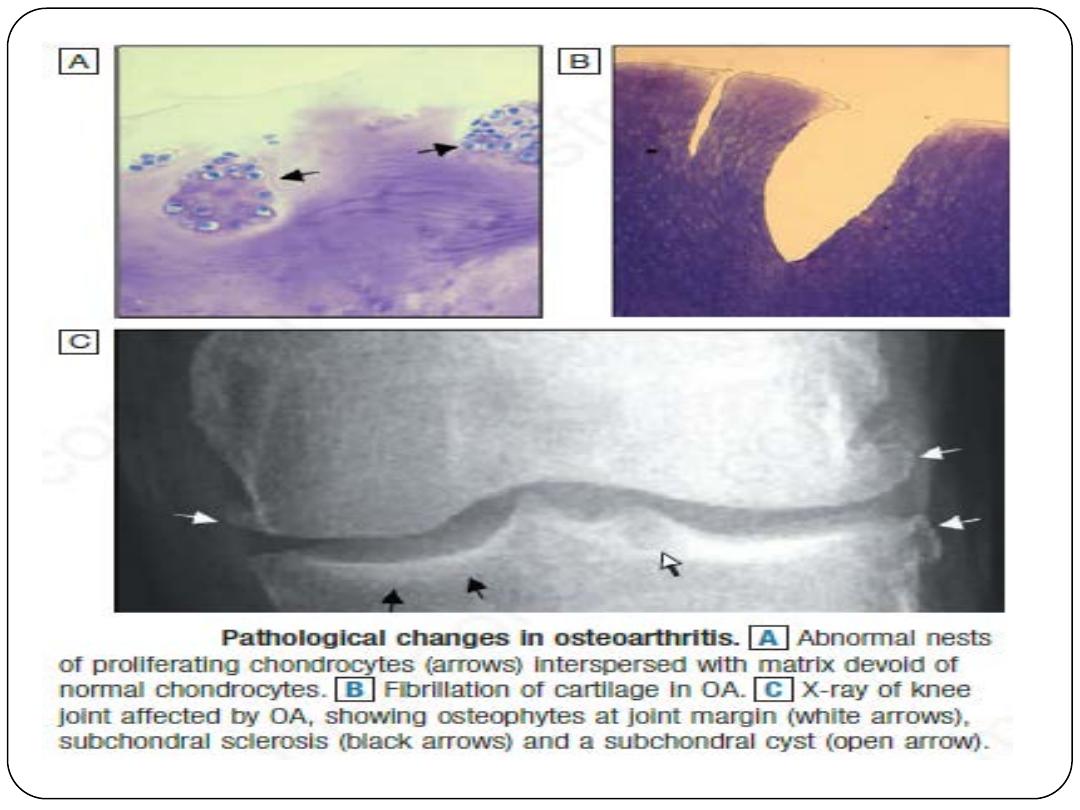
Degeneration of articular cartilage is the defining feature of OA.
Under normal circumstances, chondrocytes are terminally
differentiated cells but in OA they start dividing to produce nests
of metabolically active cells.
Initially, matrix components are produced by these cells at an
increased rate, but at the same time there is accelerated
degradation of the major structural components of cartilage
matrix, including aggrecan and type II collagen. Eventually, the
concentration of aggrecan in cartilage matrix falls and makes the
cartilage vulnerable to load-bearing injury. Fissuring of the
cartilage surface (‘fibrillation’) then occurs, leading to the
development of deep vertical clefts, localised chondrocyte death
and decreased cartilage thickness. This is initially focal, mainly
targeting the maximum load-bearing part of the joint, but
eventually large parts of the cartilage surface are damaged.
Calcium pyrophosphate and basic calcium phosphate crystals
often become deposited in the abnormal cartilage.
OA is also accompanied by abnormalities in subchondral bone,
which becomes sclerotic and the site of subchondral cysts.
Fibrocartilage is produced at the joint margin, which undergoes
endochondral ossification to form osteophytes. Bone remodelling
and cartilage thinning slowly alter the shape of the OA joint,
increasing its surface area. It is almost as though there is a
homeostatic mechanism operative in OA that causes enlargement
of the failing joint to spread the mechanical load over a greater
surface area. Patients with OA also have higher BMD values at
sites distant from the joint and this is particularly associated with
osteophyte formation. This is in keeping with observations made
in epidemiological studies that show that patients with OA are
partially protected from developing osteoporosis and vice versa.
This is likely to be due to the fact that the genetic factors that
predispose to osteoporosis might be protective for OA.
The synovium in OA is often hyperplastic and may be the site of
inflammatory change, but to a much lesser extent than in RA and
other inflammatory arthropathies. Osteochondral bodies
commonly occur within the synovium, reflecting chondroid
metaplasia or secondary uptake and growth of damaged cartilage
fragments. The outer capsule also thickens and contracts, usually
retaining the stability of the remodelling joint. The muscles
surrounding affected joints commonly show evidence of wasting
and non-specific type II fibre atrophy.
Clinical features
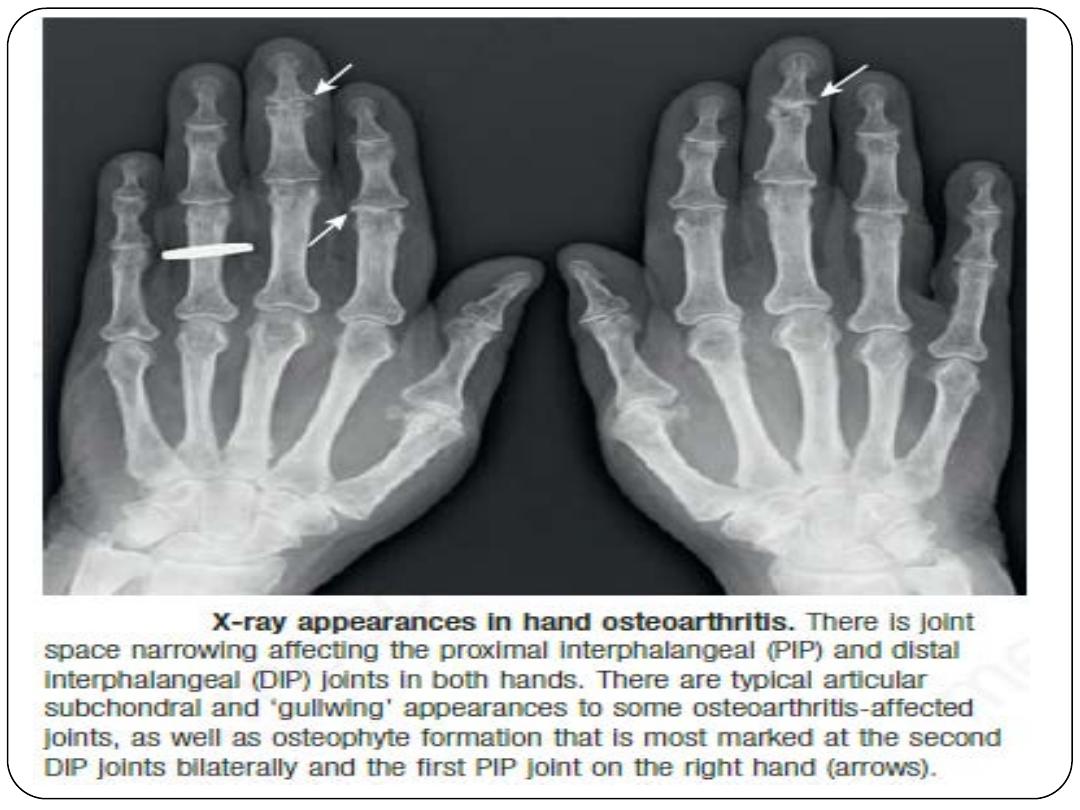
OA has a characteristic distribution, mainly targeting the hips, knees,
PIP and DIP joints of the hands, neck and lumbar spine.
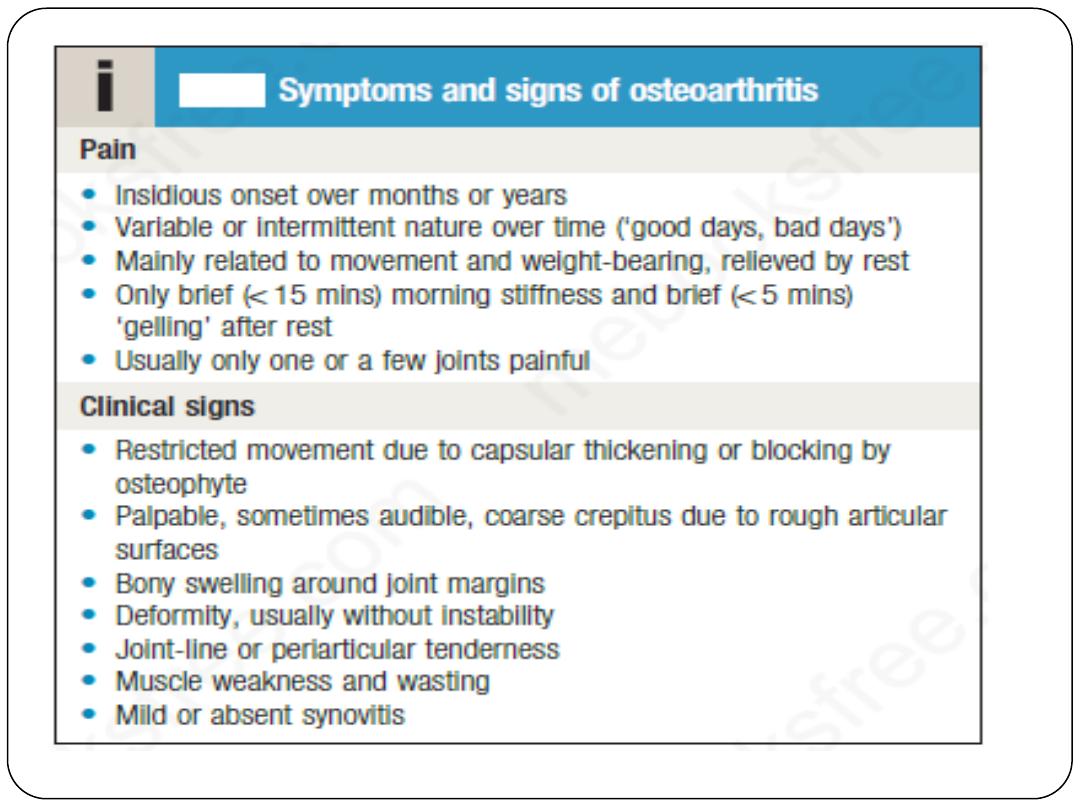
The main presenting symptoms are pain and functional restriction.
The causes of pain in OA are not completely understood but may
relate to increased pressure in subchondral bone (mainly causing night
pain), trabecular microfractures, capsular distension and low-grade
synovitis. Pain may also result from bursitis and enthesopathy
secondary to altered joint mechanics. Typical OA pain has the
characteristics listed in Box. For many people, functional restriction of
the hands, knees or hips is an equal, if not greater, problem than pain.
The clinical findings vary according to severity but are principally those
of joint damage.
The correlation between the presence of structural change, as
assessed by imaging, and symptoms such as pain and disability
varies markedly according to site. It is stronger at the hip than at
the knee, and poor at most small joints. This suggests that the risk
factors for pain and disability may differ from those for structural
change. At the knee, for example, reduced quadriceps muscle
strength and adverse psychosocial factors (anxiety, depression)
correlate more strongly with pain and disability than the degree
of radiographic change.
Radiological evidence of OA is very common in middle-aged and
older people, and the disease may coexist with other conditions,
so it is important to remember that pain in a patient with OA
may be due to another cause.
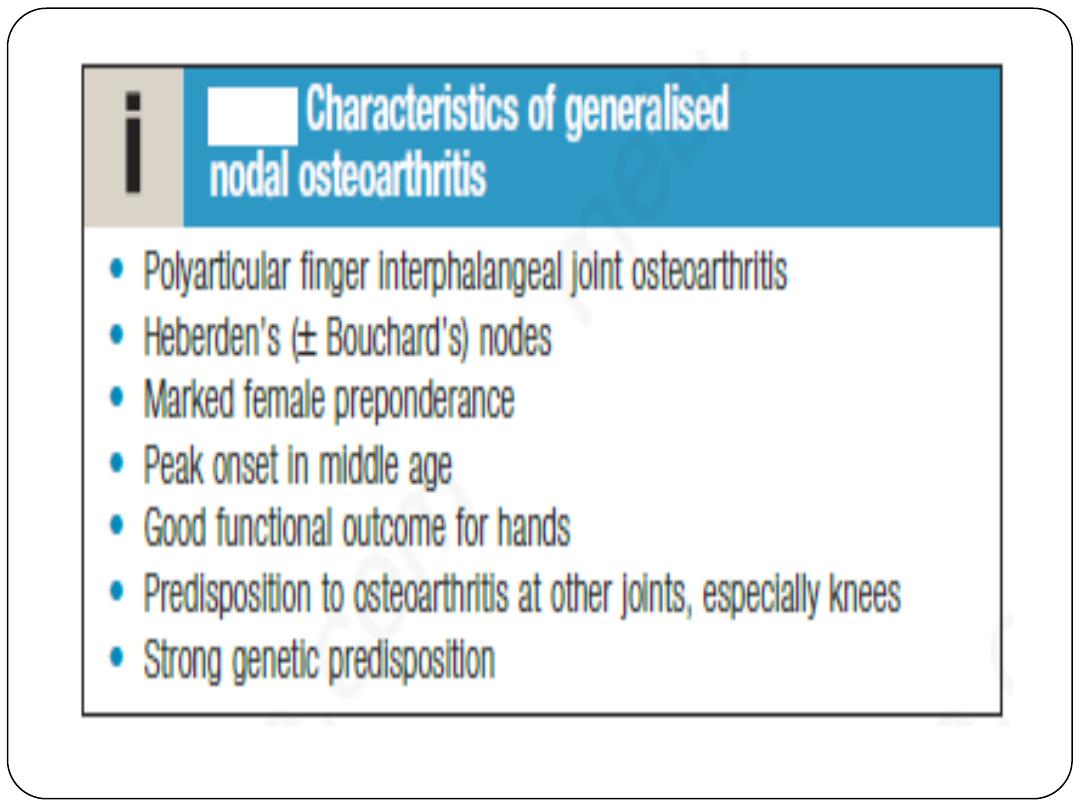
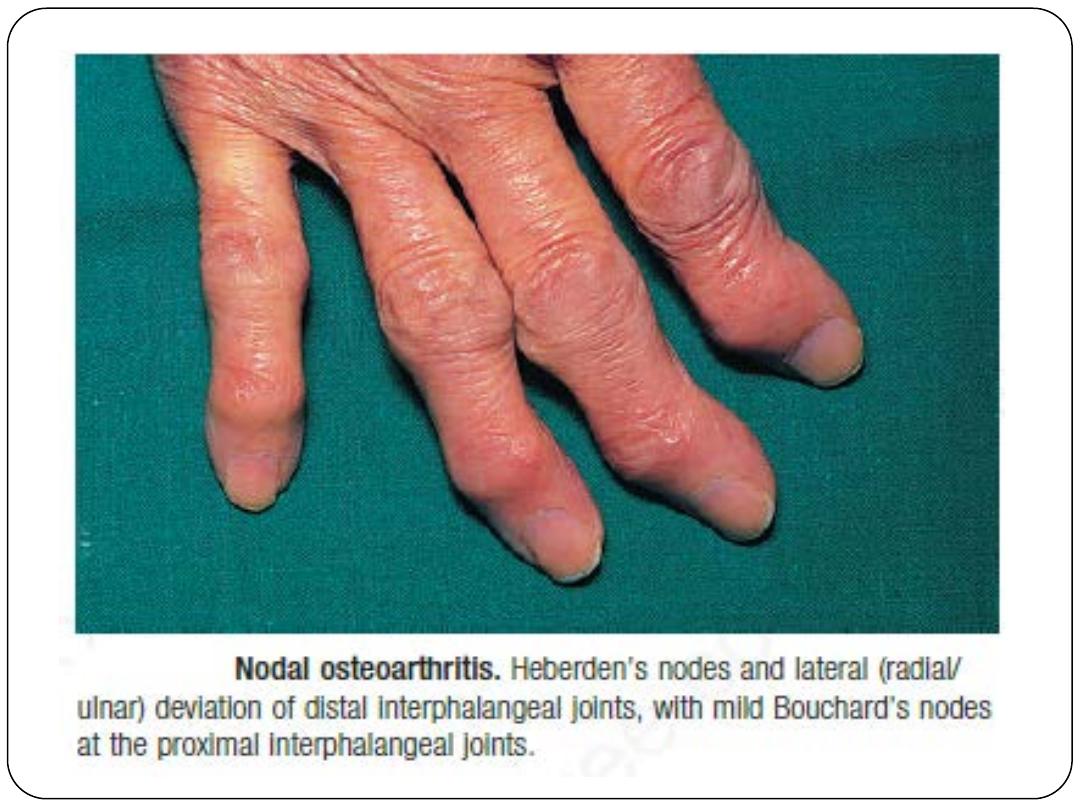
Generalised nodal OA
Some patients are asymptomatic whereas others develop pain, stiffness and
swelling of one or more PIP and DIP joints of the hands from the age of
about 40 years onwards. Gradually, these develop posterolateral swellings on
each side of the extensor tendon, which slowly enlarge and harden to
become Heberden’s (DIP) and Bouchard’s (PIP) nodes.
Typically, each joint goes through a phase of episodic symptoms (1–5 years)
while the node evolves and OA develops. Once OA is fully established,
symptoms may subside and hand function often remains good. Affected joints
are enlarged as a result of osteophyte formation and often show
characteristic lateral deviation, reflecting the asymmetric focal cartilage loss
of OA. Involvement of the first CMC joint is also common, leading to pain
on trying to open bottles and jars, and functional impairment. Clinically, it
may be detected by the presence of crepitus on joint movement, and
squaring of the thumb base.
Generalised nodal OA has a very strong genetic component: the daughter of an
affected mother has a 1 in 3 chance of developing nodal OA herself. People
with nodal OA are also at increased risk of OA at other sites, especially the
knee.
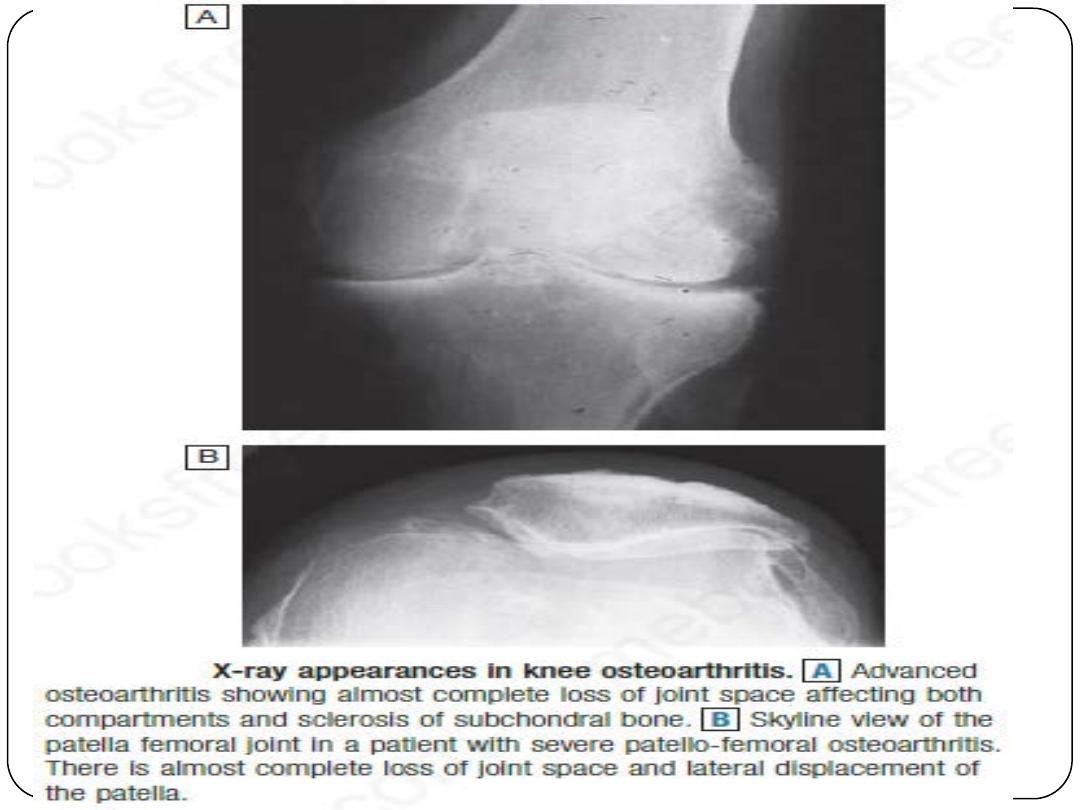
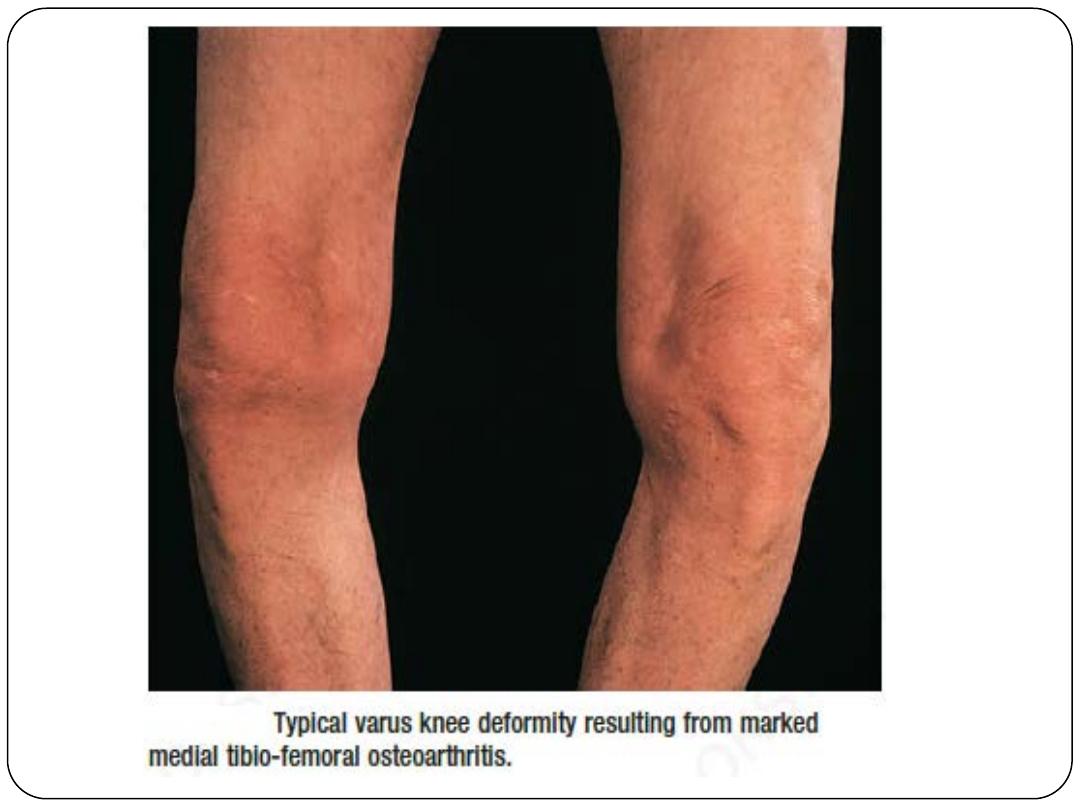
Knee OA
At the knee, OA principally targets the patello-femoral and
medial tibio-femoral compartments but eventually spreads to
affect the whole of the joint. It may be isolated or occur as part
of generalised nodal OA.
Most patients have bilateral and symmetrical involvement.
In men, trauma is often a more important risk factor and may
result in unilateral OA.
The pain is usually localised to the anterior or medial aspect of
the knee and upper tibia. Patello-femoral pain is usually worse
going up and down stairs or inclines. Posterior knee pain
suggests the presence of a complicating popliteal cyst (Baker’s
cyst). Prolonged walking, rising from a chair, getting in or out of
a car, or bending to put on shoes and socks may be difficult.
Local examination findings may include:
• a jerky, asymmetric (antalgic) gait with less time weightbearing on the
painful side
• a varus or, less commonly, valgus and/or a fixed flexion deformity
• joint-line and/or periarticular tenderness (secondary anserine bursitis
and medial ligament enthesopathy, causing tenderness of the upper
medial tibia)
.
restricted flexion and extension with coarse crepitus
• weakness and wasting of the quadriceps muscle
• bony swelling around the joint line.
CPPD crystal deposition in association with OA is common at the knee.
This may result in a more overt inflammatory component (stiffness,
effusions) and super-added acute attacks of synovitis (‘pseudogout’),
which may be associated with more rapid radiographic and clinical
progression.
Hip OA
Hip OA most commonly targets the superior aspect of the joint. It is
often unilateral at presentation, frequently progresses with superolateral
migration of the femoral head, and has a poor prognosis.
The less common central (medial) OA shows more central cartilage loss
and is largely confined to women. It is often bilateral at presentation and
can be associated with generalised nodal OA. It has a better prognosis
than superior hip OA and progression to axial migration of the femoral
head is uncommon.
The hip shows the best correlation between symptoms and radiographic
change. Hip pain is usually maximal deep in the anterior groin, with
variable radiation to the buttock, anterolateral thigh, knee or shin. Lateral
hip pain, worse on lying on that side with tenderness over the greater
trochanter, suggests secondary trochanteric bursitis. Common functional
difficulties are the same as for knee OA; in addition, restricted hip
abduction in women may cause pain during sexual intercourse.
Examination may reveal:
an antalgic gait
weakness and wasting of quadriceps and gluteal muscles
pain and restriction of internal rotation with the hip
flexed – the earliest and most sensitive sign of hip OA; other
movements may subsequently be restricted and painful
anterior groin tenderness just lateral to the femoral pulse
fixed flexion, external rotation deformity of the hip
ipsilateral leg shortening with severe joint attrition and superior
femoral migration.
Obesity is associated with more rapid progression of hip OA.
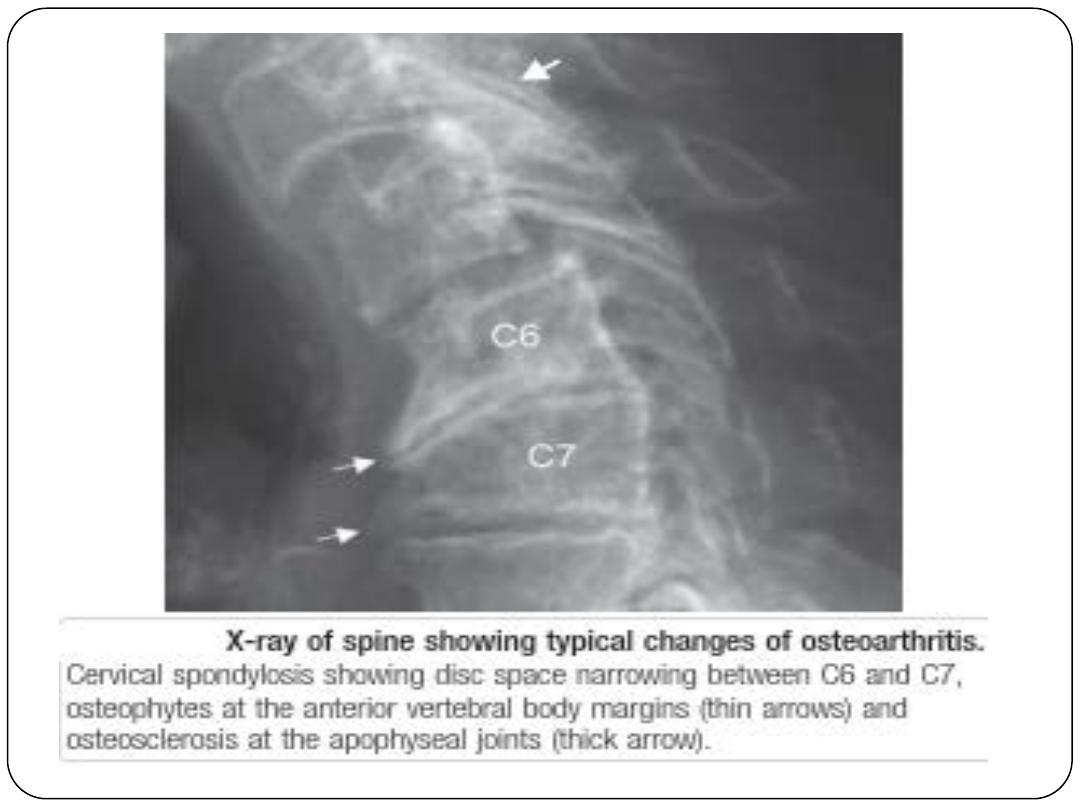
Spine OA
The cervical and lumbar spine are the sites most often targeted by OA,
where it is referred to as cervical spondylosis and lumbar spondylosis,
respectively. Spine OA may occur in isolation or as part of generalised
OA.
The typical presentation is with pain localised to the low back region
or the neck, although radiation of pain to the arms, buttocks and legs
may also occur due to nerve root compression. The pain is typically
relieved by rest and worse on movement.
On physical examination, the range of movement may be limited and
loss of lumbar lordosis is typical. The straight leg-raising test or
femoral stretch test may be positive and neurological signs may be
seen in the legs where there is complicating spinal stenosis or nerve
root compression.
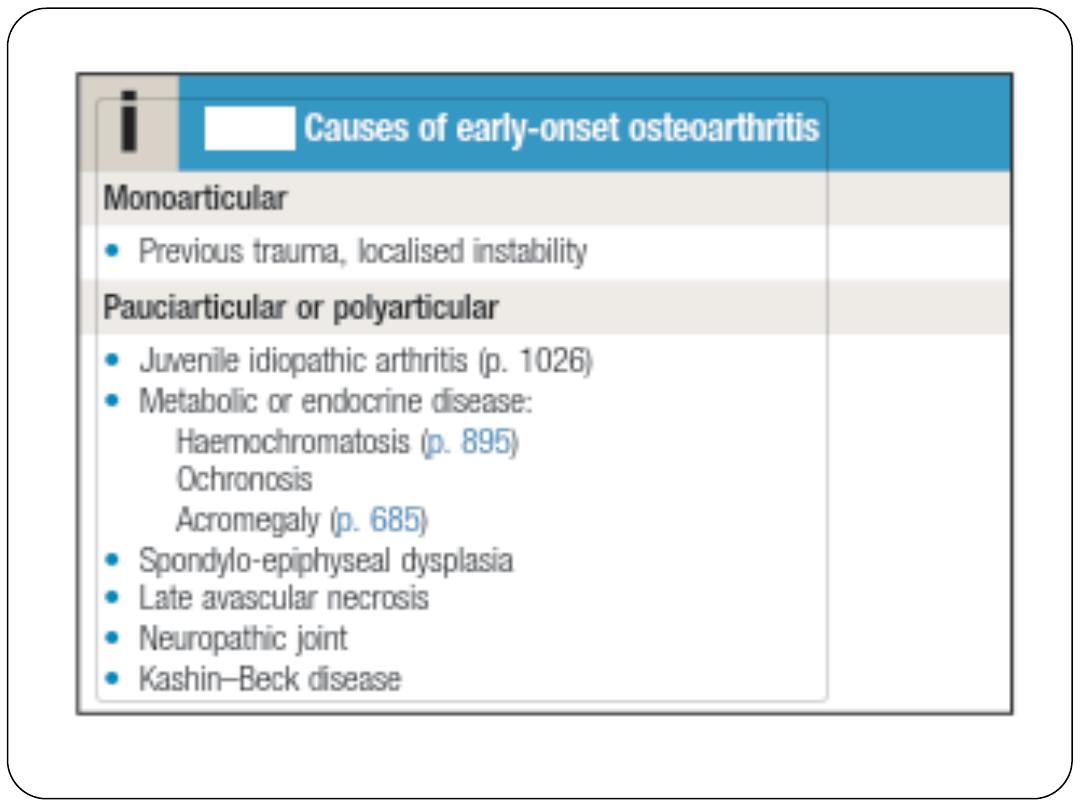
Early-onset OA
Unusually, typical symptoms and signs of OA may present before the
age of 45. In most cases, a single joint is affected and there is a clear
history of previous trauma. However, specific causes of OA need to be
considered in people with early-onset disease affecting several joints,
especially those not normally targeted by OA, in which case rare
causes need to be considered (Box).
Kashin–Beck disease is a rare form of OA that occurs in children,
typically between the ages of 7 and 13, in some regions of China. The
cause is unknown but suggested predisposing factors are selenium
deficiency and contamination of cereals with mycotoxin-producing
fungi.
Investigations
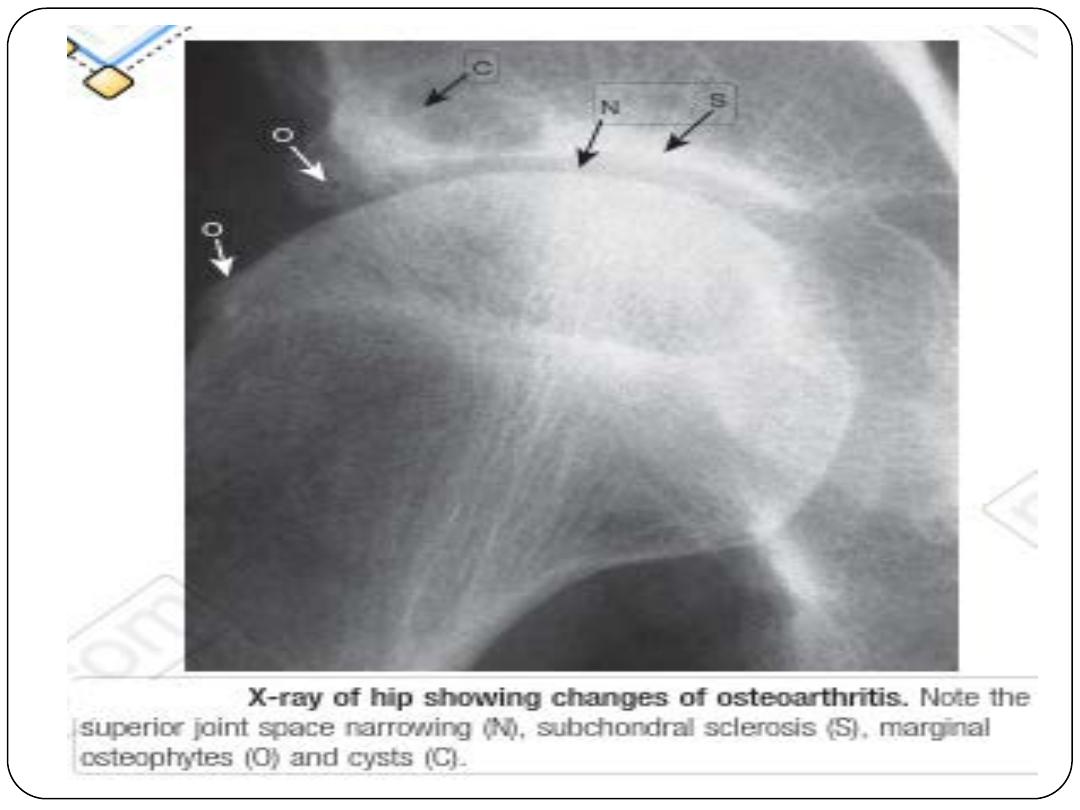
A plain X-ray of the affected joint should be performed and often this will show one or
more of the typical features of OA. In addition to providing diagnostic information, X-rays
are of value in assessing the severity of structural change, which is helpful if joint
replacement surgery is being considered. Non-weight-bearing postero-anterior views of
the pelvis are adequate for assessing hip OA. Patients with suspected knee OA should have
standing anteroposterior X-rays taken to assess tibio-femoral cartilage loss, and a flexed
skyline view to assess patello-femoral involvement. Spine OA can often be diagnosed on a
plain X-ray, which typically shows evidence of disc space narrowing and osteophytes.
If nerve root compression or spinal stenosis is suspected, MRI should be performed.
Routine biochemistry, haematology and autoantibody tests are usually normal, though OA
is associated with a moderate acute phase response.
Synovial fluid aspirated from an affected joint is viscous with a low cell count.
Unexplained early-onset OA requires additional investigation, guided by the suspected
underlying condition. X-rays may show typical features of dysplasia or avascular necrosis,
widening of joint spaces in acromegaly, multiple cysts, chondrocalcinosis and MCP joint
involvement in haemochromatosis, or disorganised architecture in neuropathic joints.
Management
Education
It is important to explain the nature of the condition fully, outlining the
role of relevant risk factors such as obesity, heredity and trauma. The
patient should be informed that established structural changes are
permanent and that, although a cure is not possible at present, pain
and function can often be improved.
The prognosis should also be discussed, mentioning that it is generally
good for nodal hand OA and better for knee than hip OA.
Lifestyle advice
Weight loss has a substantial beneficial effect on symptoms if
the patient is obese and is probably one of the most effective
treatments available for OA of the lower limbs.
Strengthening and aerobic exercises also have beneficial
effects in OA and should be advised, preferably with
reinforcement by a physiotherapist.
Quadriceps strengthening exercises are particularly beneficial
in knee OA.
Shock-absorbing footwear, pacing of activities, use of a walking
stick for painful knee or hip OA, and provision of built-up
shoes to equalise leg lengths can all improve symptoms.
Non-pharmacological therapy
Acupuncture and transcutaneous electrical nerve stimulation
(TENS) have been shown to be effective in knee OA.
Local physical therapies, such as heat or cold, can sometimes give
temporary relief.
Pharmacological therapy
If symptoms do not respond to non-pharmacological measures,
paracetamol should be tried.
Addition of a topical NSAID, and then capsaicin, for knee and hand
OA can also be helpful. Oral NSAIDs should be considered in
patients who remain symptomatic. These drugs are significantly more
effective than paracetamol and can be successfully combined with
paracetamol or compound analgesics if the pain is severe. Strong
opiates may occasionally be required. Antineuropathic drugs,
such as amitriptyline, gabapentin and pregabalin, are sometimes used
in patients with symptoms that are difficult to control but the evidence
base for their use is poor. Neutralising antibodies to nerve growth
factor have been developed and are a highly effective treatment for
pain in OA but they are not yet licensed for routine clinical use.
Intra-articular injections
Intra-articular glucocorticoid injections are effective in the
treatment of knee OA and are also used for symptomatic
relief in the treatment of OA at the first CMC joint. The
duration of effect is usually short but trials of serial
glucocorticoid injections every 3 months in knee OA have
shown efficacy for up to 1 year.
Intra-articular injections of hyaluronic acid are effective in
knee OA but the treatment is expensive and the effect short-
lived.
Neutraceuticals
Chondroitin sulphate and glucosamine sulphate have been used
alone and in combination for the treatment of knee OA. There is
evidence from randomised controlled trials that these agents can
improve knee pain to a small extent (3–5%) compared with
placebo.
Surgery
Surgery should be considered for patients with OA whose symptoms and
functional impairment impact significantly on their quality of life
despite optimal medical therapy and lifestyle advice. Total joint
replacement surgery is by far the most common surgical procedure for
patients with OA. It can transform the quality of life for people with
severe knee or hip OA and is indicated when there is significant
structural damage on X-ray. Although surgery should not be
undertaken at an early stage during the development of OA, it is
important to consider it before functional limitation has become
advanced since this may compromise outcome.
Patient-specific factors, such as age, gender, smoking and presence of
obesity, should not be barriers to referral for joint replacement.
Only a small proportion of patients with OA progress to the
extent that total joint replacement is required but OA is by far
the most frequent indication for this. Over 95% of joint
replacements continue to function well into the second decade
after surgery and most provide life-long, pain-free function. Up
to 20% of patients are not satisfied with the outcome, however,
and a few experience little or no improvement in pain. Other
surgical procedures are performed much less frequently.
Osteotomy is occasionally carried out to prolong the life of
malaligned joints and to relieve pain by reducing intraosseous
pressure. Cartilage repair is sometimes performed to treat focal
cartilage defects resulting from joint injury.
THANKs
