Dr. Mohamed Ghalib Zakari
Internal Medicine
TUCOM
5
th
year
Multiple Myeloma
This is a malignant proliferation of plasma cells. Normal plasma
cells are derived from B cells and produce immunoglobulin that
contain heavy and light chains. Normal immunoglobulins are
polyclonal, which means that a variety of heavy chains are
produced and each may be of kappa or lambda light chain type.
In myeloma, plasma cells produce immunoglobulin of a single
heavy and light chain, a monoclonal protein commonly referred to
as a paraprotein. In most cases an excess of light chain is produced,
and in some cases only light chain is produced; this appears in the
urine as Bence Jones proteinuria and can be measured in the urine
or serum as free light chain.
Although a small number of malignant plasma cells are present in
the circulation, the majority are present in the bone marrow.
The malignant plasma cells produce cytokines, which stimulate
osteoclasts and result in net bone reabsorption. The resulting lytic
lesions cause bone pain, fractures and hypercalcaemia.
Marrow involvement can result in anaemia or pancytopenia.
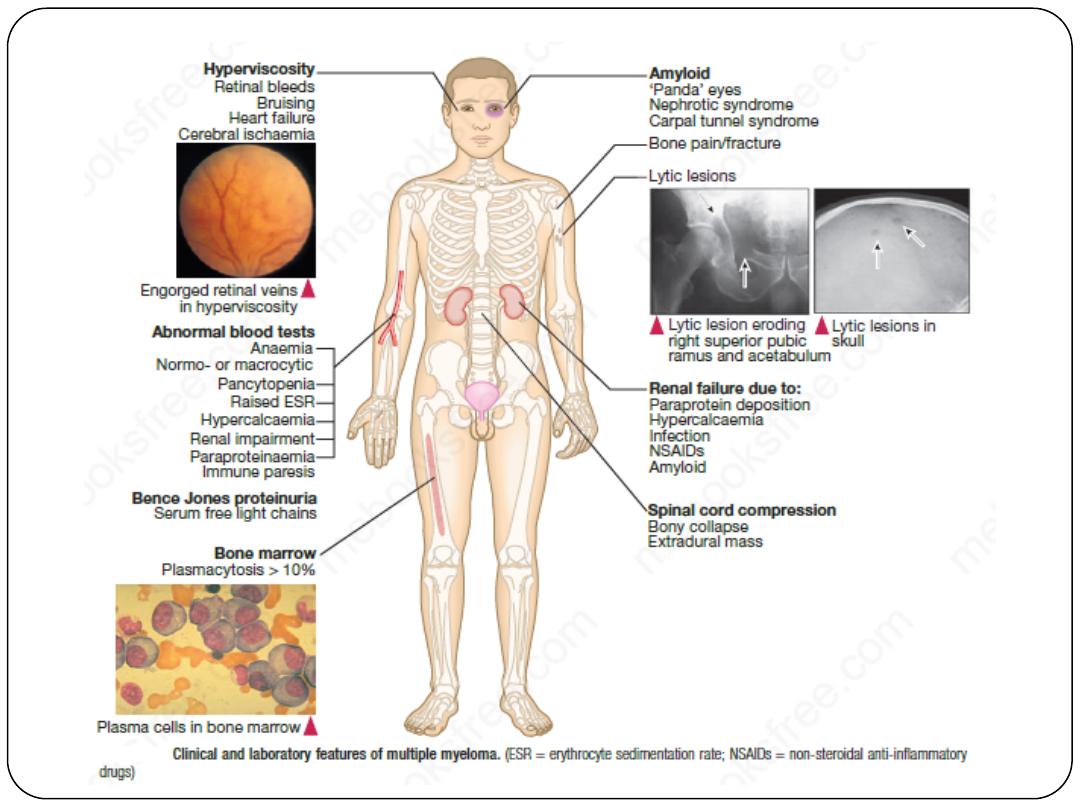
Clinical features and investigations
The incidence of myeloma is 4/100 000 new cases per annum,
with a male-to-female ratio of 2 : 1. The median age at diagnosis
is 60–70 years and the disease is more common in Afro-
Caribbeans.
The clinical manifestations of multiple myeloma are the direct
effects of bone marrow and bone infiltration by malignant plasma
cells, the systemic effects of the M protein, and the effects of the
concomitant deficiency in humoral immunity that occurs in this
disease.
The most common symptom in multiple myeloma is bone pain.
Diagnosis of myeloma requires two of the following criteria
to be fulfilled:
• increased malignant plasma cells in the bone marrow
• serum and/or urinary M-protein
• skeletal lytic lesions.
Bone marrow aspiration, plasma and urine electrophoresis, and a
skeletal survey are thus required.
Normal immunoglobulin levels, i.e. the absence of immunoparesis,
should cast doubt on the diagnosis. Paraproteinaemia can cause
an elevated ESR but this is a non-specific test; only approximately
5% of patients with a persistently elevated ESR above 100
mm/hr have underlying myeloma.
Bone radiographs typically show pure osteolytic punched-out lesions,
often in association with generalized osteopenia and pathologic
fractures. Bony lesions can show as expansile masses associated with
spinal cord compression.
Hypercalcemia caused by extensive bony involvement is common in
myeloma and may dominate the clinical picture.
Anemia occurs in most patients as a result of marrow infiltration and
suppression of hematopoiesis and causes fatigue; granulocytopenia and
thrombocytopenia are less common.
Patients with myeloma are susceptible to bacterial infections because of
impaired production and increased catabolism of normal
immunoglobulins.
Gram-negative urinary tract infections are common, as are respiratory
tract infections caused by Streptococcus pneumoniae, Staphylococcus aureus,
Haemophilus influenzae, and Klebsiella pneumoniae.
Renal insufficiency occurs in about 25% of patients with
myeloma. The cause of renal failure is often multifactorial;
hypercalcemia, hyperuricemia, infection, and amyloid deposition
can contribute. However, direct tubular damage from light-chain
excretion invariably occurs.
Because of their physicochemical properties, M proteins can
cause a host of diverse effects, including cryoglobulinemia,
hyperviscosity, amyloidosis, and clotting abnormalities resulting
from interaction of the M protein with platelets or clotting
factors.
Management
If patients are asymptomatic with no evidence of end-organ
damage (e.g. to kidneys, bone marrow or bone), treatment
may not be required.
So-called asymptomatic myeloma should be monitored
closely for the development of end-organ damage.
Immediate support
High fluid intake to treat renal impairment and hypercalcaemia.
Analgesia for bone pain.
Bisphosphonates for hypercalcaemia and to delay other skeletal
related events.
Allopurinol to prevent urate nephropathy.
Plasmapheresis, if necessary, for hyperviscosity.
Chemotherapy with or without HSCT
Myeloma therapy has improved with the addition of novel agents, initially
thalidomide
and more recently the proteasome inhibitor
bortezomib
and
the second-generation immunomodulatory drug
lenalidomide
. For first-
line therapy in older patients, thalidomide combined with the alkylating
agent melphalan and prednisolone (MPT) has increased the median
overall survival to more than 4 years. Lenalidomide is approved first-
line treatment for patients not eligible for transplantation and who are
intolerant of, or unsuitable for, thalidomide. Thalidomide and
lenalidomide both have anti-angiogenic effects against tumour blood
vessels and immunomodulatory effects. Both can cause somnolence,
constipation, peripheral neuropathy and thrombosis, though lenalidomide
has a better side-effect profile. It is vital that females of child-bearing age
use adequate contraception, as thalidomide and lenalidomide are
teratogenic. Treatment is administered until paraprotein levels have
stopped falling. This is termed ‘plateau phase’ and can last for weeks or
years.
In younger, fitter patients, standard treatment includes firstline
therapies, such as cyclophosphamide, thalidomide and
dexamethasone (CTD) or bortezomib (Velcade), thalidomide
and dexamethasone (VTD) to maximum response, and then
autologous HSCT, which improves quality of life and prolongs
survival but does not cure myeloma.
In all patients who have achieved maximal response,
lenalidomide maintenance has been shown to prolong the
response.
Radiotherapy
This is effective for localised bone pain not responding to simple
analgesia and for pathological fractures. It is also useful for the
emergency treatment of spinal cord compression complicating
extradural plasmacytomas.
Bisphosphonates
Long-term bisphosphonate therapy reduces bone pain and
skeletal events. These drugs protect bone and may cause
apoptosis of malignant plasma cells. There is evidence that
intravenous zoledronate in combination with anti-myeloma
therapy confers a survival advantage over oral bisphosphonates.
Osteonecrosis of the jaw may be associated with long-term use
or poor oral hygiene and gum sepsis; regular dental review,
including a check before starting therapy, is therefore important.
Prognosis
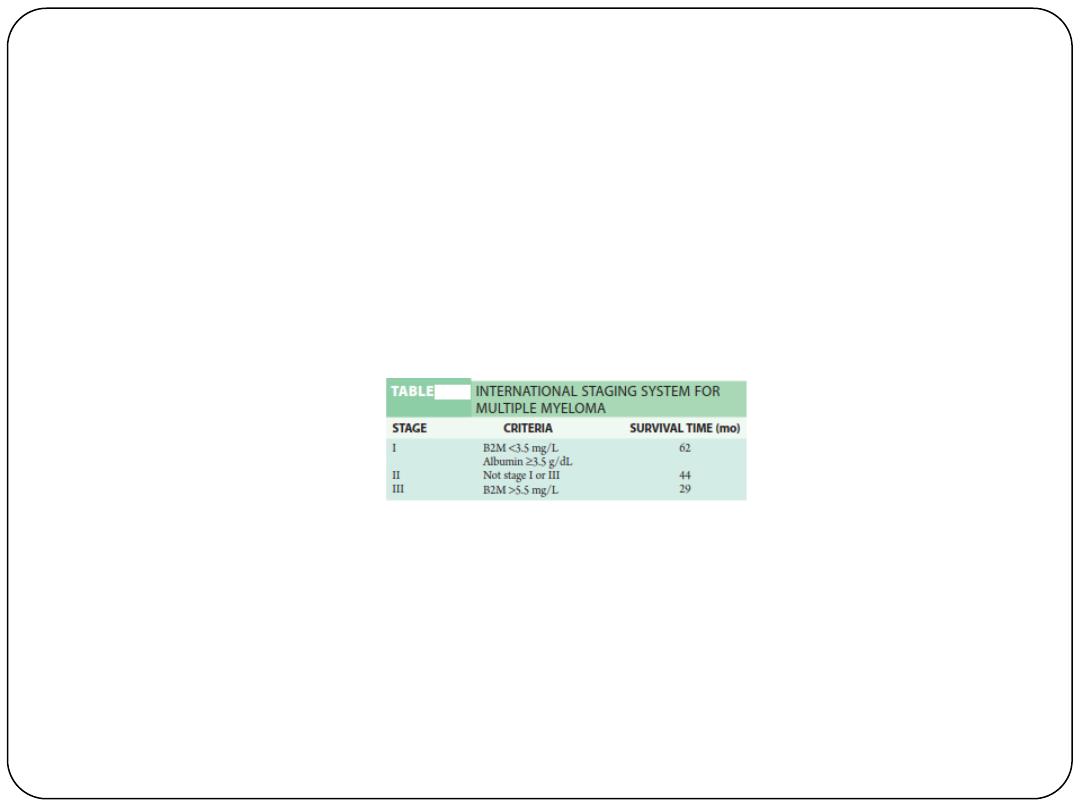
The international staging system (ISS) identifies poor prognostic
features, including a high
β
2
-microglobulin and low albumin at
diagnosis (ISS stage 3, median survival 29 months). Those with a
normal albumin and a low
β
2
-microglobulin (ISS stage 1) have a
median survival of 62 months. Increasingly, cytogenetic analysis
is used to identify poor-risk patients, e.g. t(4;14), del(17/17p),
t(14;16), t(14;20), non-hyperdiploidy and gain(1q).
Use of autologous HSCT and advances in drug therapy with the
newer agents have increased survival. Over one-third of patients
are now surviving for 5 years, compared with only one-quarter
10 years ago. The outlook may improve further with new drugs
and combinations of treatments.
