Dr. Mohamed Ghalib
Internal Medicine
TUCOM
5
TH
CLASS

Amoebiasis is caused by
Entamoeba
histolytica, which is spread between humans
by its cysts.
It is one of the leading parasitic causes of
morbidity and mortality in the tropics and is
occasionally acquired in non-tropical
countries.
Two nonpathogenic Entamoeba species (E.
dispar and E. moshkovskii) are
morphologically identical to E. histolytica, and
are distinguishable only by molecular
techniques, isoenzyme studies or monoclonal
antibody typing. However, only E. histolytica
causes amoebic dysentery or liver abscess.
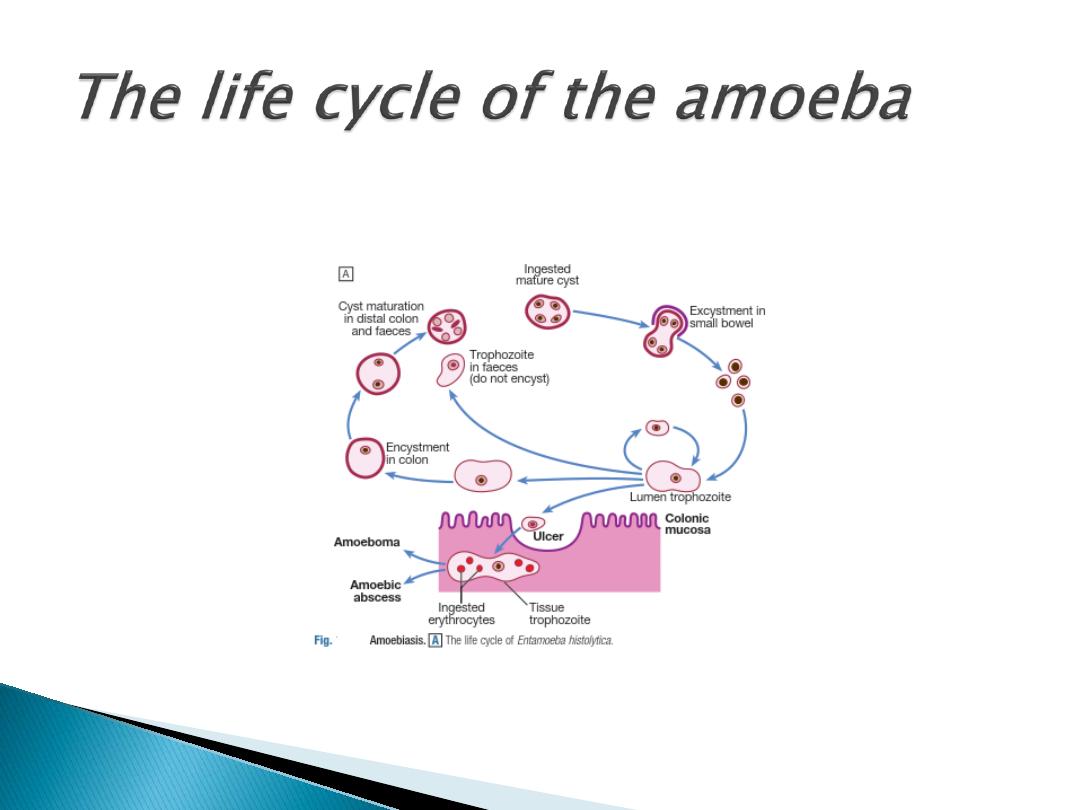

Cysts of
E. histolytica are ingested in water or
uncooked foods contaminated by human faeces. In
the colon, trophozoite forms emerge from the cysts.
The parasite invades the mucous membrane of the
large bowel, producing lesions that are maximal
in
the caecum but extend to the anal canal. These are
flask-shaped ulcers, varying greatly in size and
surrounded by healthy mucosa.
A localised granuloma (amoeboma), presenting as a
palpable mass in the rectum or a filling defect in the
colon on radiography, is a rare complication that
should be differentiated from carcinoma.
Amoebic ulcers may cause severe haemorrhage but
rarely perforate the bowel wall.

Amoebic trophozoites can emerge from the
vegetative cyst from the bowel and be carried
to the liver in a portal venule. They can
multiply rapidly and destroy the liver
parenchyma, causing an abscess. The liquid
contents at first have a characteristic pinkish
colour, which may later change to chocolate-
brown.
Cutaneous amoebiasis, though rare, causes
progressive genital, perianal or peri-
abdominal surgical wound ulceration.

Intestinal amoebiasis – amoebic dysentery
Most amoebic infections are asymptomatic. The
incubation period of amoebiasis ranges from 2 weeks
to many years, followed by a chronic course with
abdominal pains and two or more unformed stools a
day.
Offensive diarrhoea, alternating with constipation, and
blood or mucus in the stool are common. There may be
abdominal pain, especially in the right lower quadrant
(which may mimic acute appendicitis).
A dysenteric presentation with passage of blood,
simulating bacillary dysentery or ulcerative colitis,
occurs particularly in older people, in the puerperium
and with super-added pyogenic infection of the ulcers.

Amoebic liver abscess
The abscess is usually found in the right hepatic
lobe.
There may not be associated diarrhoea.
Early symptoms may be only local discomfort
and malaise; later, a swinging temperature and
sweating may develop, usually without marked
systemic symptoms or signs. An enlarged, tender
liver, cough and pain in the right shoulder are
characteristic but symptoms may remain vague
and signs minimal. A large abscess may
penetrate the diaphragm, rupturing into the lung,
and may be coughed up through a
hepatobronchial fistula. Rupture into the pleural
or peritoneal cavity, or rupture of a left lobe
abscess in the pericardial sac, is less common
but more serious.

The stool and any exudate should undergo prompt
microscopic examination for motile trophozoites
containing red blood cells. Movements cease rapidly as the
stool preparation cools. Several stools may need to be
examined in chronic amoebiasis before cysts are found.
Sigmoidoscopy may reveal typical flask-shaped ulcers,
which should be scraped and examined immediately for
E.
histolytica. In endemic areas, one-third of the population
are symptomless passers of amoebic cysts.
An amoebic abscess of the liver is suspected on clinical
grounds; there is often a neutrophil leucocytosis and a
raised right hemidiaphragm on chest X-ray. Confirmation
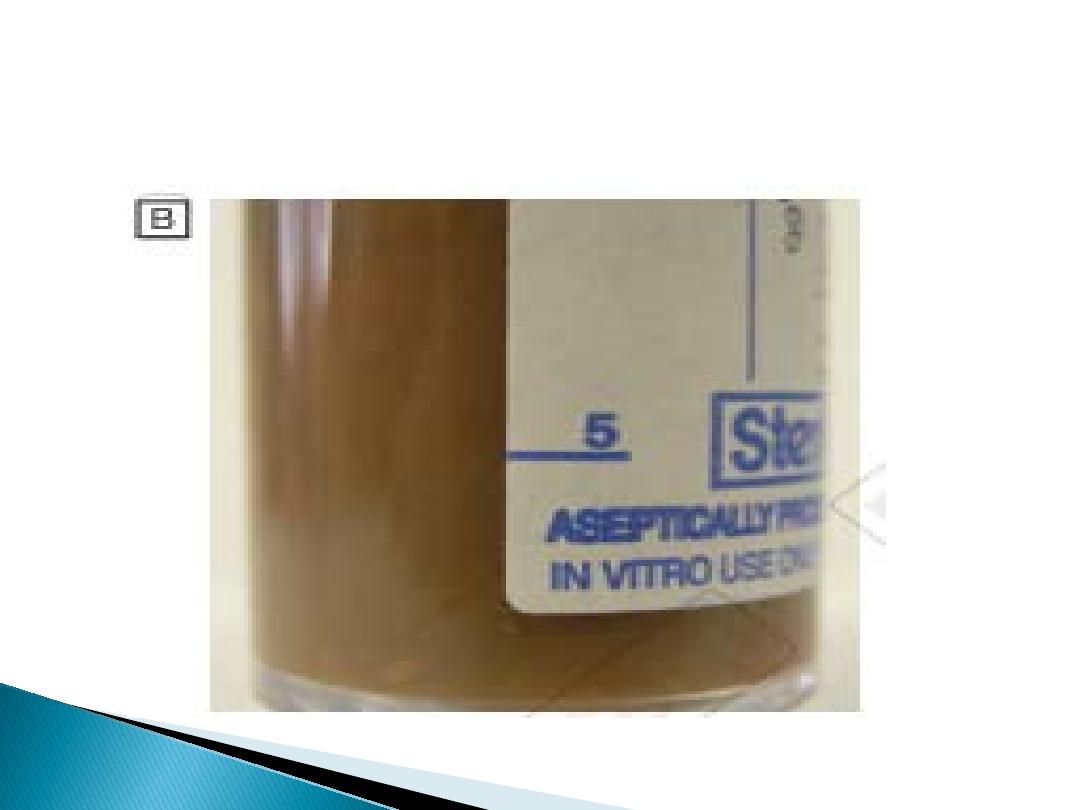
is by ultrasonic scanning. Aspirated pus from an amoebic
abscess has the characteristic chocolate-brown
appearance but only rarely contains free amoebae.

Serum antibodies are detectable by
immunofluorescence in over 95% of patients
with hepatic amoebiasis and intestinal
amoeboma, but in only about 60% of
dysenteric amoebiasis.
DNA detection by PCR has been shown to be
useful in diagnosis of
E. histolytica infections
but is not generally available.

Intestinal and early hepatic amoebiasis responds quickly
to oral metronidazole (800 mg 3 times daily for 5–10
days) or other long-acting nitroimidazoles like tinidazole
or ornidazole (both in doses of 2 g daily for 3 days).
Nitazoxanide (500 mg twice daily for 3 days) is an
alternative drug.
Either diloxanide furoate or paromomycin, in doses of
500 mg orally 3 times daily for 10 days after treatment,
should be given to eliminate luminal cysts.
If a liver abscess is large or threatens to burst, or if the
response to chemotherapy is not prompt, aspiration is
required and is repeated if necessary. Rupture of an
abscess into the pleural cavity, pericardial sac or
peritoneal cavity necessitates immediate aspiration or
surgical drainage. Small serous effusions resolve without
drainage.

Prevention
Personal precautions against contracting
amoebiasis include not eating fresh,
uncooked vegetables or drinking unclean
water.

THANKS
