
Common Viral
Infections
DONE BY DR MARWAN MAJEED IBRAHIM
CABM INTERNAL MEDICINE FICM RESPIRATORY
MEDICINE

Measles
Clinical features
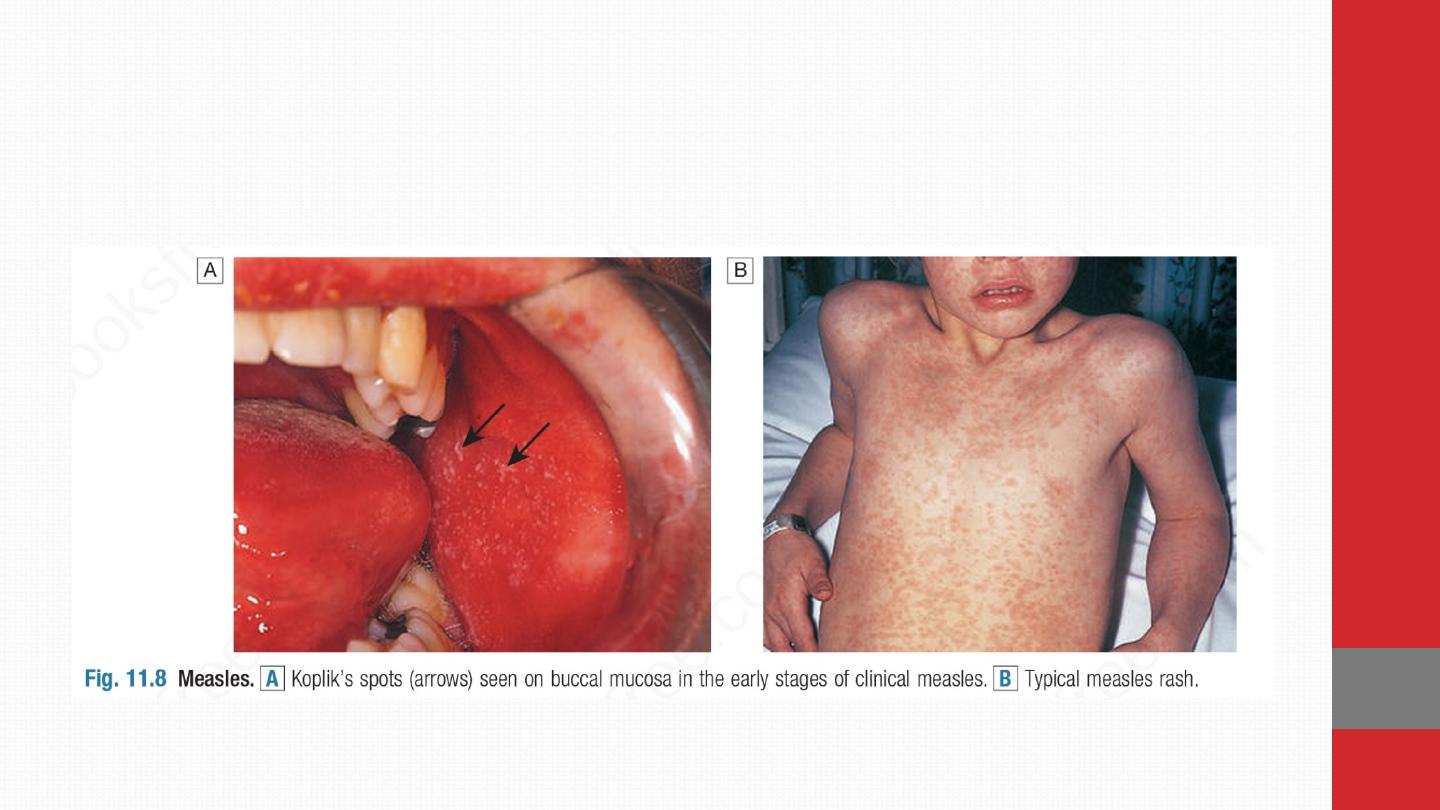
Infection is by respiratory droplets with an incubation period
of 6–19 days. A prodromal illness occurs, 1–3 days before the
rash, with upper respiratory symptoms, conjunctivitis and the
presence of the pathognomonic Koplik’s spots: small white
spots surrounded by erythema on the buccal mucosa. As
natural antibody develops, the maculopapular rash appears,
spreading from the face to the extremities . Generalised
lymphadenopathy and diarrhoea are common.
Complications are more common in older children and adults,
and include otitis media, bacterial pneumonia, transient
hepatitis, pancreatitis and clinical encephalitis
(approximately 0.1% of cases). A rare late complication is
subacute sclerosing panencephalitis (SSPE), which occurs
up to 7 years after infection.
Diagnosis is clinical (although this has become unreliable in
areas where measles is no longer common) and by detection of
antibody (serum immunoglobulin M (IgM), seroconversion or
salivary IgM).

Meaes is a serious disease in the malnourished, vitamin
deficient or immunocompromised, in whom the typical
rash may be missing and persistent infection with a
giant cell pneumonitis or encephalitis may occur.
In
tuberculosis infection, measles suppresses cell-mediated
immunity and may exacerbate disease; for this reason,
measles vaccination should be deferred until after
commencing antituberculous treatment
. Measles does not
cause congenital malformation but may be more severe
in pregnant women.
Mortality clusters at the extremes of age, averaging 1 :
1000 in developed countries and up to 1 : 4 in developing
countries.
Death usually results from a bacterial
superinfection, occurring as a complication of measles:
most often pneumonia, diarrhoeal disease or
noma/cancrum oris, a gangrenous stomatitis. Death may
also result from complications of measles encephalitis
.
Management and prevention Normal immunoglobulin
attenuates the disease in the immunocompromised (regardless of
vaccination status) and in non-immune pregnant women, but
must be given within 6 days of exposure. Vaccination can be
used in outbreaks and vitamin A may improve the
outcome in uncomplicated disease. Antibiotic therapy is
reserved for bacterial complications. All children aged 12–15
months should receive measles vaccination (as combined
measles, mumps and rubella (MMR), a live attenuated vaccine), and
a further MMR dose at age 4 years
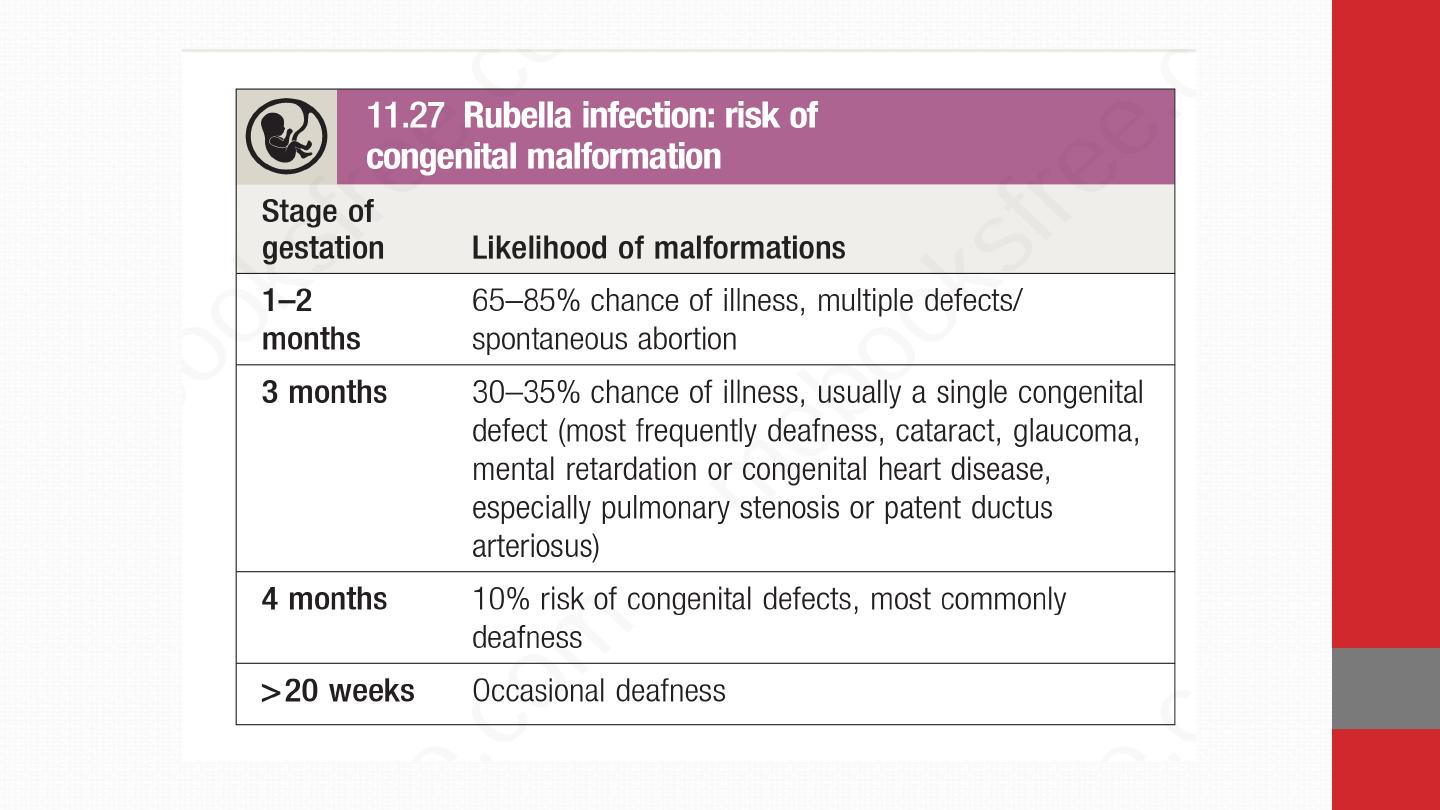
Rubella (German measles)
Clinical features Rubella is spread by respiratory droplet,
with infectivity from up to 10 days before to 2 weeks after the
onset of the rash. The incubation period is 15–20 days. In
childhood, most cases are subclinical, although clinical features
may include fever, maculopapular rash spreading from the
face, and lymphadenopathy. Complications are rare but
include thrombocytopenia and hepatitis. Encephalitis and
haemorrhage are occasionally reported. In adults, arthritis
involving hands or knees is relatively common mainly in women.
If transplacental infection takes place in the first
trimester or later, persistence of the virus is likely and
severe congenital disease may result . Even if normal at
birth, the infant has an increased incidence of other
diseases developing later, e.g. diabetes mellitus

Diagnosis Laboratory confirmation of rubella is required if
there has been contact with a pregnant woman. This is
achieved either by detection of
rubella IgM in serum or by
IgG seroconversion. In the exposed pregnant woman,
absence of rubella-specific IgG confirms the potential for
congenital infection
.
Prevention All children should be immunised with MMR vaccine.
Congenital rubella syndrome may be controlled by testing
women of childbearing age for rubella antibodies and
offering vaccination if seronegative

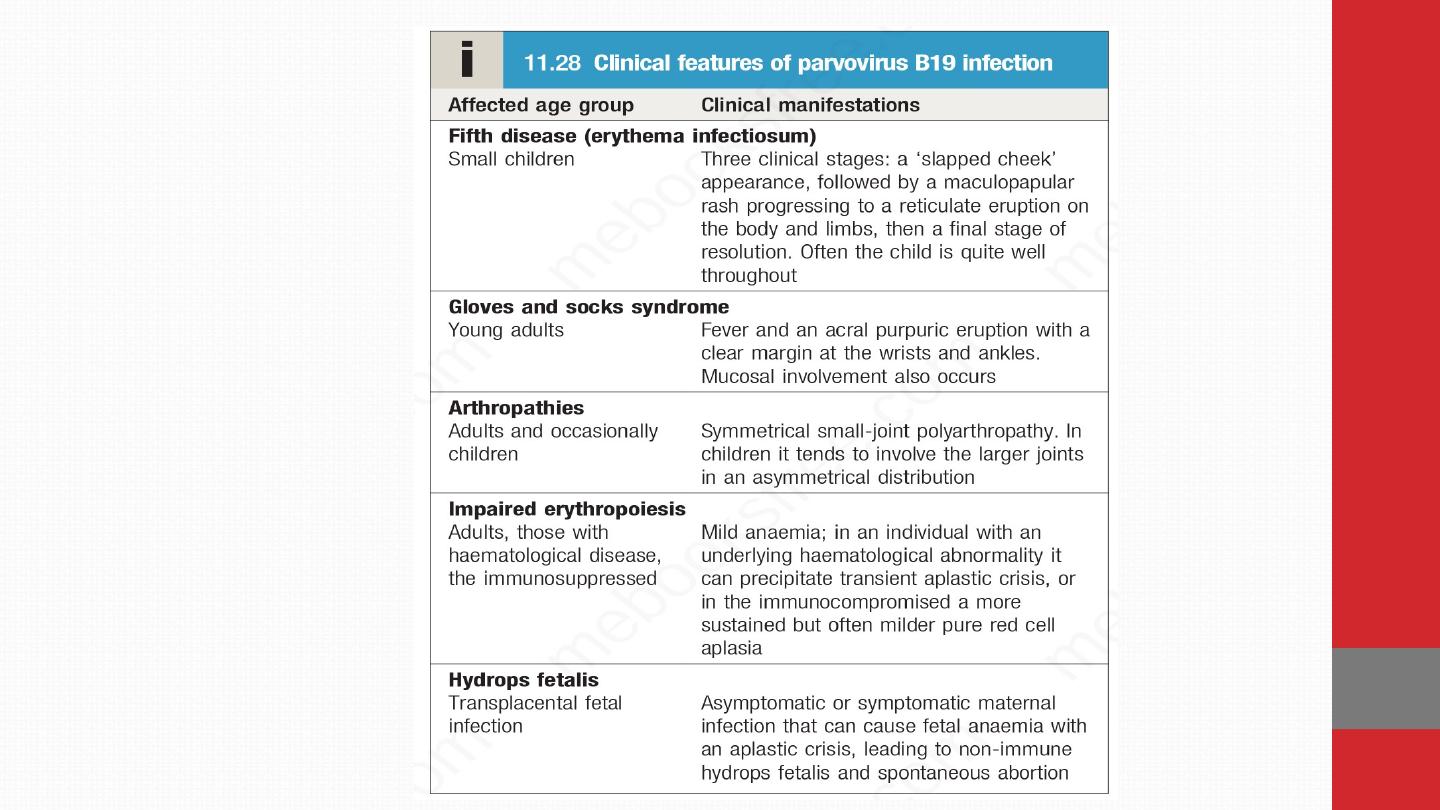
Parvovirus B19
Parvovirus B19 causes exanthem and other clinical syndromes. Some
50% of children and 60–90% of adults are seropositive.
Clinical features Many infections are subclinical. Clinical
manifestations result after an incubation period of 14–21 days. The
classic exanthem (erythema infectiosum) is preceded by a
prodromal fever and coryzal symptoms. A ‘slapped cheek’
rash is characteristic but the rash is very variable . In adults,
polyarthropathy is common. Infected individuals have a transient
block in erythropoiesis for a few days, which is of no clinical
consequence, except in individuals with increased red cell turnover
due to haemoglobinopathy or haemolytic anaemia.

These individuals develop an acute anaemia that may be severe
(transient aplastic crisis). Erythropoiesis usually recovers
spontaneously after 10–14 days. Immunocompromised individuals,
including those with congenital immunodeficiency or AIDS, can
develop a more sustained block in erythropoiesis in response to the
chronic viraemia that results from their inability to clear the infection.
Infection during the first two trimesters of pregnancy can
result in intrauterine infection and impact on fetal bone
marrow; it causes 10–15% of non-immune (non-Rhesus-
related) hydrops fetalis, a rare complication of pregnancy.

Diagnosis IgM to parvovirus B19 suggests recent infection but may
persist for months Detection of parvovirus B19 DNA in blood is
particularly
useful
in
immunocompromised patients.
Giant
pronormoblasts or haemophagocytosis may be demonstrable
in the bone marrow.
Management Infection is usually self-limiting. Symptomatic relief for
arthritic symptoms may be required.
The pregnancy should be closely monitored by ultrasound scanning,
so that hydrops fetalis can be treated by fetal transfusion

Chickenpox (VARICELLA)
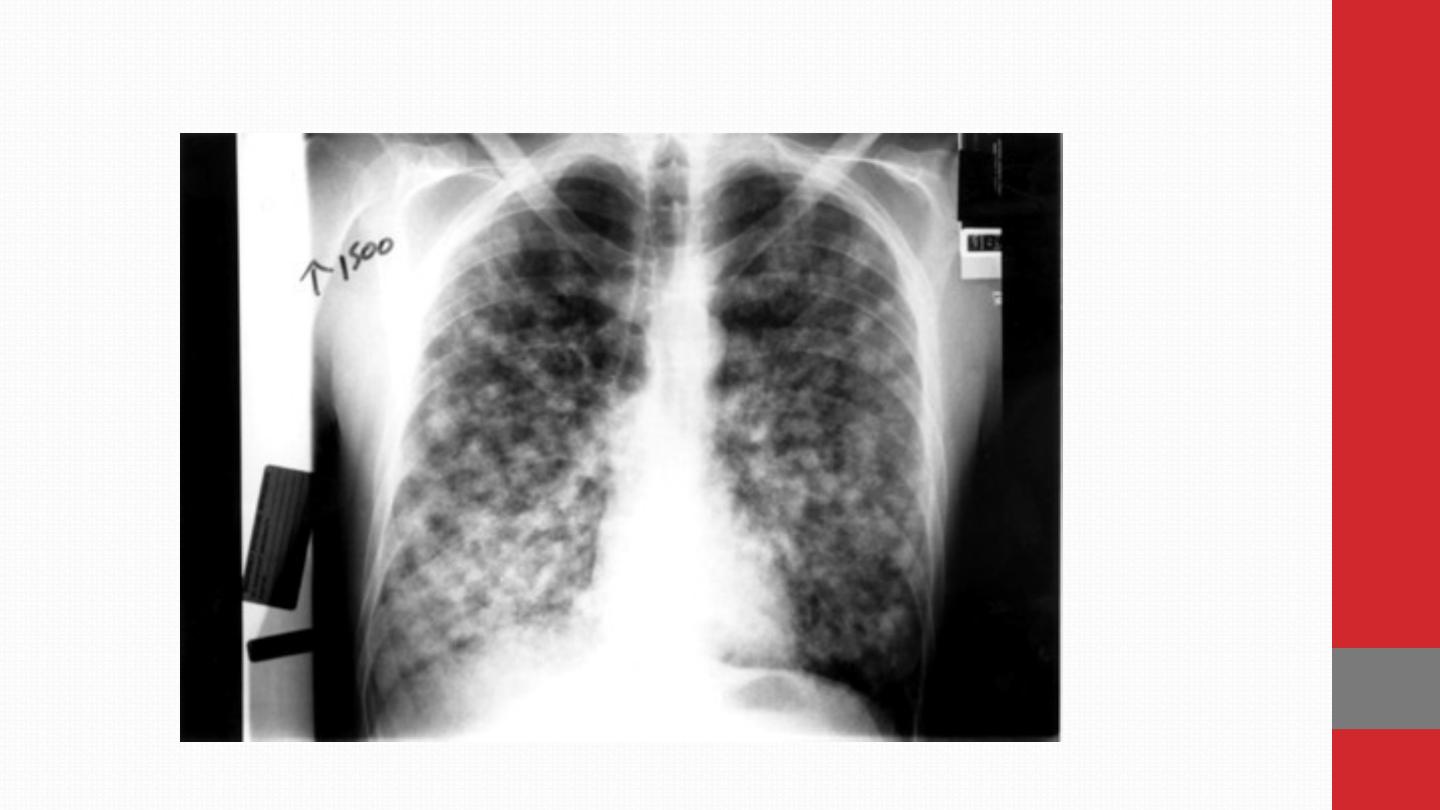
Varicella zoster virus (VZV) happens usually in childhood, which may
reactivate in later life. VZV is spread by aerosol and direct contact. It
is highly infectious to non-immune individuals. Disease in children
is usually well tolerated. Manifestations are more severe in
adults, pregnant women and the immunocompromised.
Clinical features The incubation period is 11–20 days, after which a
vesicular eruption begins , often on mucosal surfaces first, followed
by rapid dissemination in a centripetal distribution (most dense
on trunk and sparse on limbs). New lesions occur every 2–4 days and
each crop is associated with fever. The rash progresses from small
pink macules to vesicles and pustules within 24 hours. Infectivity
lasts from up to 4 days (but usually 48 hours) before the
lesions appear until the last vesicles crust over. Due to intense
itching, secondary bacterial infection from scratching is the most
common complication of primary chickenpox. Self-limiting
cerebellar ataxia and encephalitis are rare complications.
Adults, pregnant women and the immunocompromised are at
increased risk of visceral involvement, which presents as
pneumonitis, hepatitis or encephalitis. Pneumonitis can be
fatal and is more likely to occur in smokers. Maternal infection in
early pregnancy carries a 3% risk of neonatal damage with
developmental abnormalities of eyes, CNS and limbs. Chickenpox
within 5 days of delivery leads to severe neonatal varicella with
visceral involvement and haemorrhage. Diagnosis is clinical.

Management and prevention The benefits of antivirals for
uncomplicated primary VZV infection in children are marginal,
shortening the duration of rash by only 1 day, and treatment is not
normally
required.
Antivirals
are,
however,
used
for
uncomplicated chickenpox in adults when the patient
presents within 24–48 hours of onset of vesicles, in all
patients with complications, and in those who are
immunocompromised, including pregnant women, regardless
of duration of vesicles . More severe disease, particularly in
immunocompromised hosts, requires initial parenteral therapy.
Immunocompromised patients may have prolonged viral shedding
and may require prolonged treatment until all lesions crust over.
Human VZ immunoglobulin (VZIG) is used to attenuate
infection in people who have had significant contact with VZV,
are susceptible to infection (i.e. have no history of chickenpox
or shingles and are seronegative for VZV IgG) and are at risk
of severe disease (e.g. immunocompromised or pregnant)
.
Ideally, VZIG should be given within 7 days of exposure, but it may
attenuate disease even if given up to 10 days afterwards
.
Susceptible contacts who develop severe chickenpox after
receiving VZIG should be treated with aciclovir.

Shingles (herpes zoster)
After initial infection, VZV persists in latent form in the dorsal
root ganglion of sensory nerves and can reactivate in later
life .
Clinical features
Burning discomfort occurs in the affected
dermatome following reactivation and discrete vesicles
appear 3–4 days later
. This is associated with a brief viraemia,
which
can
produce
distant
satellite
‘chickenpox’
lesions.
Occasionally, paraesthesia occurs without rash (‘zoster sine
herpete’).
Severe disease, a prolonged duration of rash,
multiple dermatomal involvement or recurrence suggests
underlying immune deficiency, including HIV. Chickenpox may
be contracted from a case of shingles but not vice versa.
Although thoracic dermatomes are most commonly involved ,
the
ophthalmic division of the trigeminal nerve is also frequently
affected; vesicles may appear on the cornea and lead to
ulceration. This condition can lead to blindness and urgent
ophthalmology review is required.
Geniculate ganglion
involvement causes the Ramsay Hunt syndrome of facial palsy
, ipsilateral loss of taste and buccal ulceration, plus a rash in
the external auditory canal
This may be mistaken for Bell’s palsy . Bowel and bladder dysfunction
occur with sacral nerve root involvement. The virus occasionally
causes cranial nerve palsy, myelitis or encephalitis. Granulomatous
cerebral angiitis is a cerebrovascular complication that leads to a
stroke-like syndrome in association with shingles, especially in an
ophthalmic distribution.
Post-herpetic neuralgia causes troublesome persistence of
pain for 1–6 months or longer, following healing of the rash. It
is more common in elderly.
Management Early therapy with aciclovir or related agents has
been shown to reduce both early- and late-onset pain, especially in
patients over 65 years. Post-herpetic neuralgia requires aggressive
analgesia, along with agents such as amitriptyline 25–100 mg
daily, gabapentin (commencing at 300 mg daily and building
slowly to 300 mg twice daily or more) or pregabalin
(commencing at 75 mg twice daily and building up to 100 mg
or 200 mg 3 times daily if tolerated). Capsaicin cream
(0.075%) may be helpful. Although controversial, glucocorticoids
have not been demonstrated to reduce post-herpetic neuralgia to
date.
Mumps
Mumps is a systemic viral infection characterised by swelling of the
parotid glands. Infection is endemic worldwide and peaks at 5–9 years
of age. Vaccination has reduced the incidence in children but
incomplete coverage and waning immunity with time have led to
outbreaks in young adults. Infection is spread by respiratory
Clinical features The median incubation period is 19 days, with a
range of 15–24 days. Classical tender parotid enlargement,
which is bilateral in 75%, follows a prodrome of pyrexia and
headache. Meningitis complicates up to 10% of cases.
Rare complications include encephalitis, transient hearing loss,
labyrinthitis, electrocardiographic abnormalities, pancreatitis and
arthritis. Approximately 25% of post-pubertal males with mumps
develop epididymo-orchitis but, although testicular atrophy occurs,
sterility is unlikely. The diagnosis is usually clinical. Treatment is
with analgesia.
Infectious mononucleosis and
Epstein–Barr virus
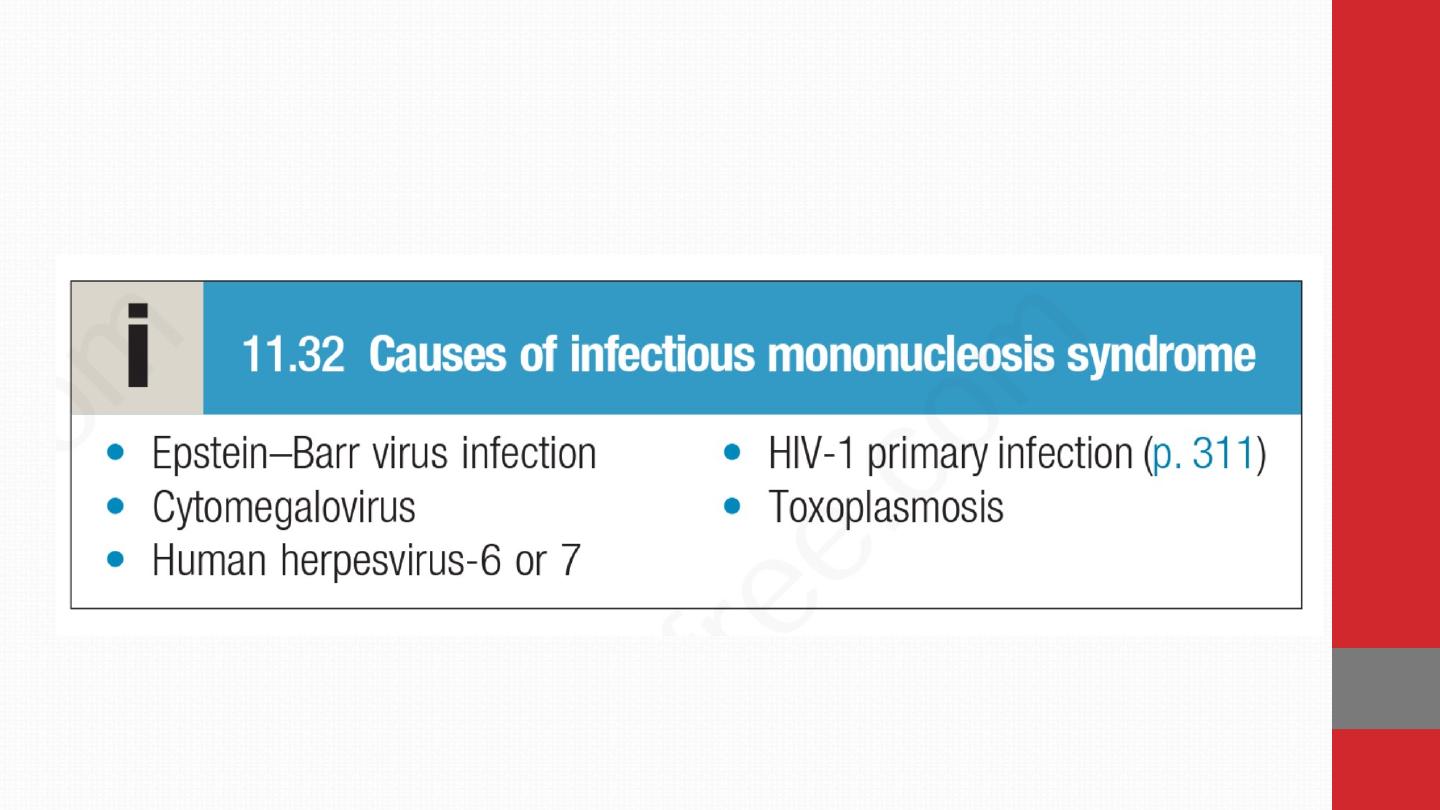
Infectious mononucleosis (IM) is a clinical syndrome
characterised by pharyngitis, cervical lymphadenopathy,
fever and lymphocytosis (known colloquially as glandular
fever). It is most often caused by Epstein–Barr virus (EBV) but
other infections can produce a similar clinical syndrome

EBV is a gamma herpesvirus. In developing countries, subclinical
infection in childhood is virtually universal. In developed
countries, primary infection may be delayed until adolescence or
early adult life. Under these circumstances, about 50% of
infections result in typical IM. The virus is usually acquired from
asymptomatic excreters via saliva, either by droplet infection or
environmental contamination in childhood, or by kissing among
adolescents and adults. EBV is not highly contagious and
isolation of cases is unnecessary.

Clinical features EBV infection has a prolonged but
undetermined incubation period, followed in some cases by a
prodrome of fever, headache and malaise. This is followed by
IM with severe pharyngitis, which may include tonsillar
exudates and non-tender anterior and posterior cervical
lymphadenopathy. Palatal petechiae, periorbital oedema,
splenomegaly, inguinal or axillary lymphadenopathy, and
macular, petechial or erythema multiforme rashes may
occur. In most cases, fever resolves over 2 weeks, and fatigue
and other abnormalities settle over a further few weeks. Death
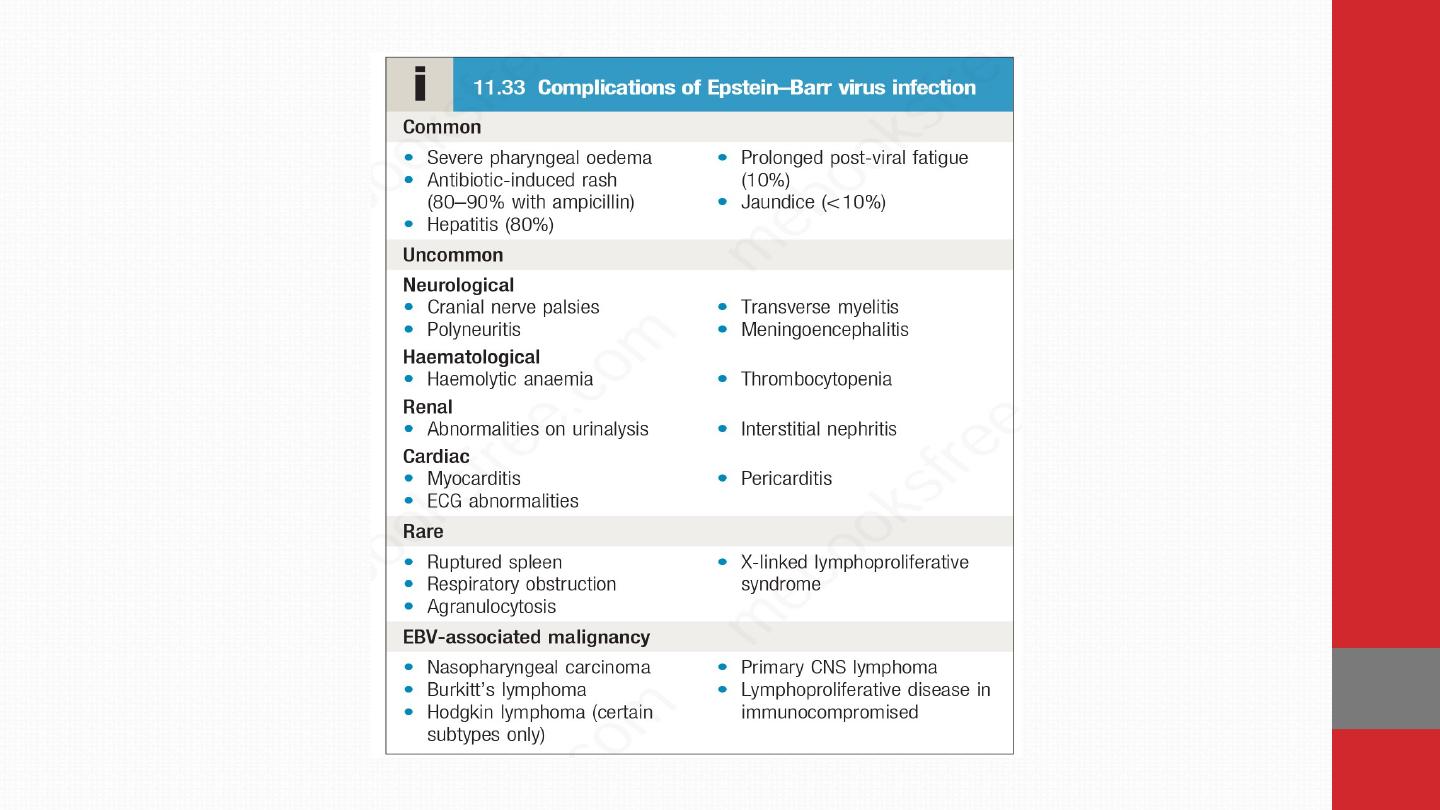
is rare but can occur due to respiratory obstruction,
haemorrhage from splenic rupture, thrombocytopenia or
encephalitis.
The diagnosis of EBV infection outside the usual age in
adolescence and young adulthood is more challenging. In
children under 10 years the illness is mild and short-lived, but
in adults over 30 years of age it can be severe and prolonged.
In both groups, pharyngeal symptoms are often absent. EBV may
present with jaundice, as a PUO or with a complication.
Long-term complications of EBV infection Lymphoma complicates
EBV infection in immunocompromised hosts, and some forms of
Hodgkin lymphoma are EBV-associated . The endemic form of
Burkitt’s lymphoma complicates EBV infection in areas of sub-
Saharan Africa where falciparum malaria is endemic.
Nasopharyngeal carcinoma is a geographically restricted
tumour seen in China and Alaska that is associated with EBV
infection.
Investigations
Atypical lymphocytes are common in EBV
infection
but also occur in other causes of IM, acute retroviral
syndrome with HIV infection, viral hepatitis, mumps and rubella. They
are also a feature of dengue, malaria and other geographically
restricted infections. A ‘heterophile’ antibody is present during
the acute illness and convalescence, which is detected by the
Paul–Bunnell or ‘Monospot’ test.
Specific EBV serology confirms the diagnosis. Acute infection is
characterised by IgM antibodies against the viral capsid, antibodies to
EBV early antigen and the initial absence of antibodies to EBV nuclear
antigen (anti-EBNA). Seroconversion of anti-EBNA at approximately 1
month after the initial illness may confirm the diagnosis in retrospect.
CNS infections may be diagnosed by detection of viral DNA in CSF.

Management
Treatment is largely symptomatic.
If a throat
culture yields a β-haemolytic streptococcus, penicillin should be
given.
Administration of ampicillin or amoxicillin in this
condition commonly causes an itchy macular rash and should
be avoided.
When pharyngeal oedema is severe, a short
course of glucocorticoids, e.g. prednisolone 30 mg daily for 5
days, may help. Current antiviral drugs are not active against
EBV.Return to work or school is governed by physical fitness rather
than laboratory tests;
contact sports should be avoided until
splenomegaly has resolved because of the danger of splenic
rupture
.
