Staphylococcal Infections
DONE BY
DR MARWAN MAJEED IBRAHIM
CABM INTERNAL MEDICINE FICM PULMONARY MEDICINE

Staphylococcus aureus, the most virulent of the many
staphylococcal species. S. aureus is a pluripotent pathogen, causing
disease through both toxin- and non-toxin-mediated mechanisms. It
is responsible for numerous nosocomial and community- based
infections that range from relatively minor skin and soft tissue
infections (SSTIs) to life-threatening systemic infections. The “other”
staphylococci,
collectively
designated
coagulase-
negative
staphylococci (CoNS), are considerably less virulent than S. aureus
but remain important pathogens in select settings, such as
infections that involve prosthetic devices.
•
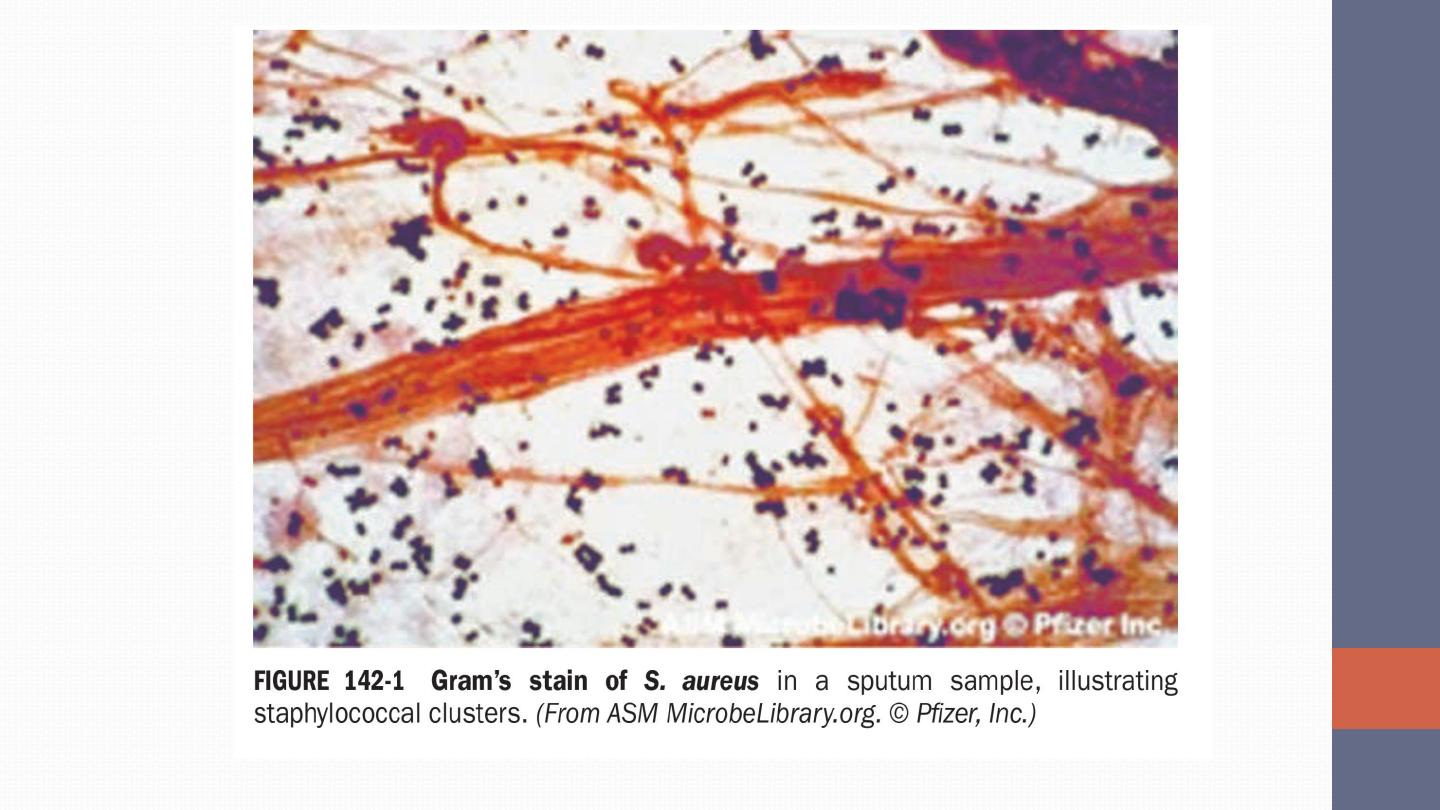
Staphylococci, gram-positive cocci, form grapelike clusters on
Gram’s stain . These organisms (~1 μm in diameter) are catalase-
positive (unlike streptococcal species), non-motile, aerobic, and
facultatively anaerobic.
They are capable of prolonged survival on
environmental surfaces under varying conditions
.
•
With few exceptions, S. aureus is distinguished from other
staphylococcal species by its production of
coagulase +ve
, a
surface enzyme that converts fibrinogen to fibrin.
S. AUREUS INFECTIONS
S. aureus is both a commensal and an opportunistic pathogen.
Approximately 20–40% of healthy persons are colonized with S.
aureus, with a smaller percentage (~10%) persistently colonized with
the same strain.
The rate of colonization is elevated among insulin-
dependent diabetics, HIV-infected patients, patients undergoing
hemodialysis, injection drug users, and individuals with skin
damage.
The anterior nares and oropharynx are frequent sites of
human colonization, although the skin (especially when damaged),
vagina, axilla, and perineum are also often colonized
. These
colonization sites serve as potential reservoirs for future infections.

•
In the past three decades, there has been a dramatic change in the
epidemiology of infections due to
methicillin-resistant S. aureus
(MRSA). In addition to its major role as a nosocomial pathogen,
MRSA has become an established community-based pathogen.
•
The S. aureus toxin
Panton-Valentine leukocidin
is cytolytic to
PMNs, macrophages, and monocytes. Strains elaborating this
toxin have been epidemiologically linked with cutaneous and more
serious infections caused by strains of CA-MRSA.
•
S. aureus produces three types of toxin: cytotoxins, pyrogenic
toxin superantigens, and exfoliative toxins.

DIAGNOSIS
•
Elevated ESR, CRP & leukocytosis (band formation).
•
Peptide nucleic acid fluorescence in situ hybridization (PAN FISH) +ve.
•
Staphylococcal infections are readily diagnosed by Gram’s stain and
microscopic examination of abscess contents or of infected tissue.
Routine culture of infected material usually yields positive results,
and blood cultures are sometimes positive even when infections are
localized to extravascular sites. S. aureus is rarely a blood culture
contaminant.
•
Polymerase chain reaction (PCR)–based assays are now often used for
the rapid diagnosis of S. aureus infection. A number of point-of-care
tests are now available to screen patients for colonization with
MRSA.
CLINICAL SYNDROMES
Skin and Soft Tissue Infections
•
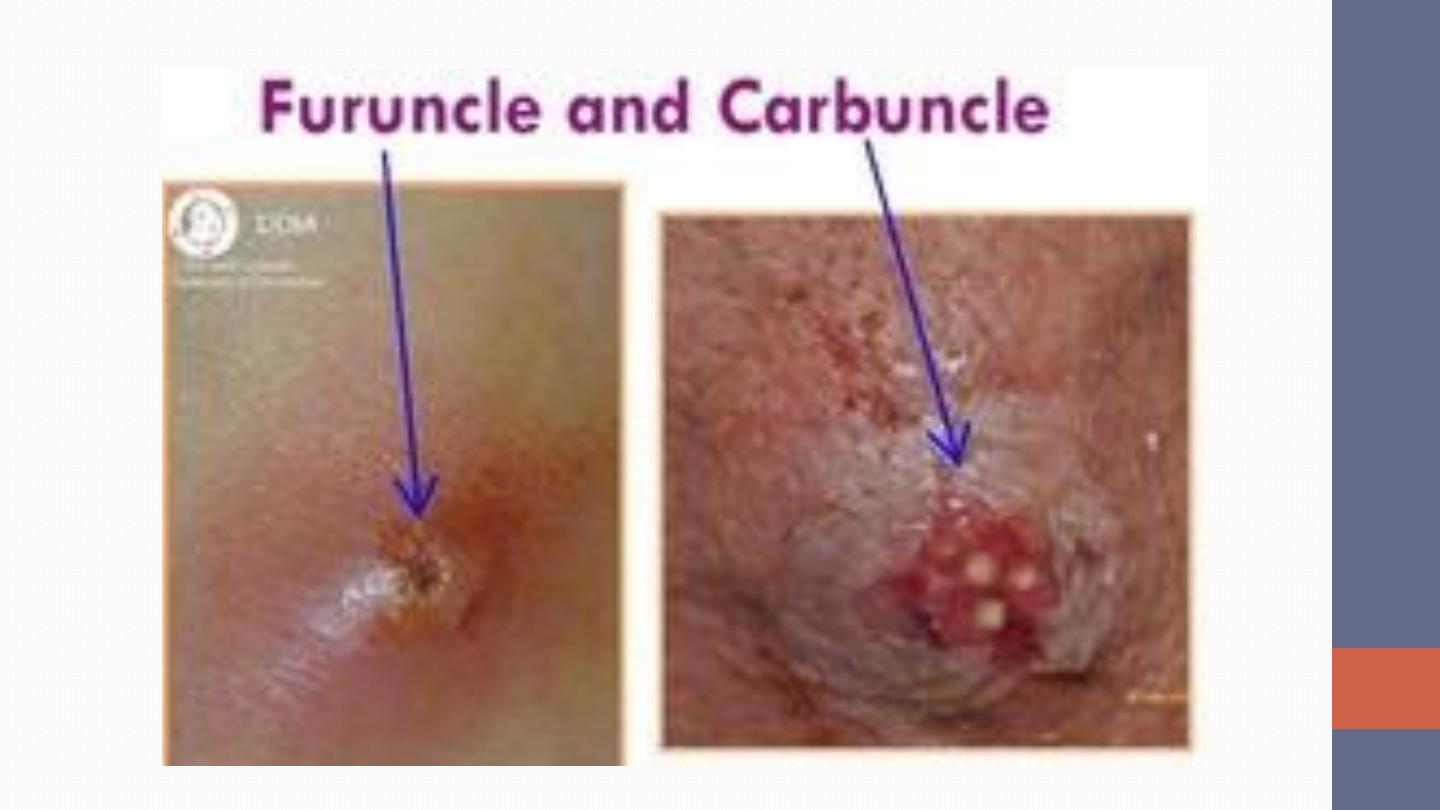
Folliculitis is a superficial infection that involves the hair follicle,
with a central area of purulence (pus) surrounded by induration
and erythema.
•
Furuncles (boils) are more extensive, painful lesions that tend to
occur in hairy, moist regions of the body and extend from the
hair follicle to become a true abscess with an area of central
purulence.
•
Carbuncles are most often located in the lower neck and are even
more severe and painful, resulting from the coalescence of other
lesions that extend to a deeper layer of the subcutaneous tissue.

SEPTIC EMBOLI
CELLULITIS
Musculoskeletal Infections
Hematogenous osteomyelitis in children most often involves the
long bones. Infections present with fever and bone pain or with
a child’s reluctance to bear weight. The white blood cell count and
erythrocyte sedimentation rate are often elevated. Blood
cultures are positive in ~50% of cases.

vertebral osteomyelitis & Discitis
is among the more common
clinical presentations. Often seen in patients with endocarditis,
those undergoing hemodialysis, diabetics, and injection drug
users. These infections may present as intense back pain with fever
but may also be clinically occult, presenting as chronic back pain
with low-grade fever. S. aureus is the most common cause of
epidural abscess, a complication that can result in neurologic
compromise. Patients report difficulty voiding or walking and
radicular pain in addition to the symptoms associated with their
osteomyelitis. Surgical intervention in this setting often constitutes
a medical emergency. MRI is USED to establish the diagnosis.

In both children and adults,
S. aureus is the most common cause
of septic arthritis in native joints
. This infection is rapidly
progressive and may be associated with extensive joint destruction
if left untreated.
It presents with intense pain on motion of the
affected joint, swelling, and fever
.
Aspiration of the joint
reveals turbid fluid, with >50,000 PMNs/ μL and gram-positive
cocci in clusters on Gram’s stain

In adults, septic arthritis may result from trauma, surgery, or
hematogenous dissemination
. The most commonly involved joints
include the knees, shoulders, hips, and phalanges. Infection
frequently develops in joints previously damaged by osteoarthritis
or rheumatoid arthritis. Iatrogenic infections resulting from
aspiration or injection of agents into the joint also occur.
Respiratory Tract Infections
•
In adults, nosocomial S. aureus pulmonary infections are common
among intubated patients in intensive care units. Nasally colonized
patients are at increased risk of these infections. Chest x-ray may
reveal pneumatoceles (shaggy, thin-walled cavities). Pneumothorax
and empyema are recognized complications.
•
Community-acquired respiratory tract infections due to S. aureus
often follow viral infections—most commonly influenza. Patients may
present with fever, bloody sputum production, and midlung-field
pneumatoceles or multiple, patchy pulmonary infiltrates. Diagnosis is
made by sputum Gram’s stain and culture. Blood cultures, although
useful, are usually negative
.
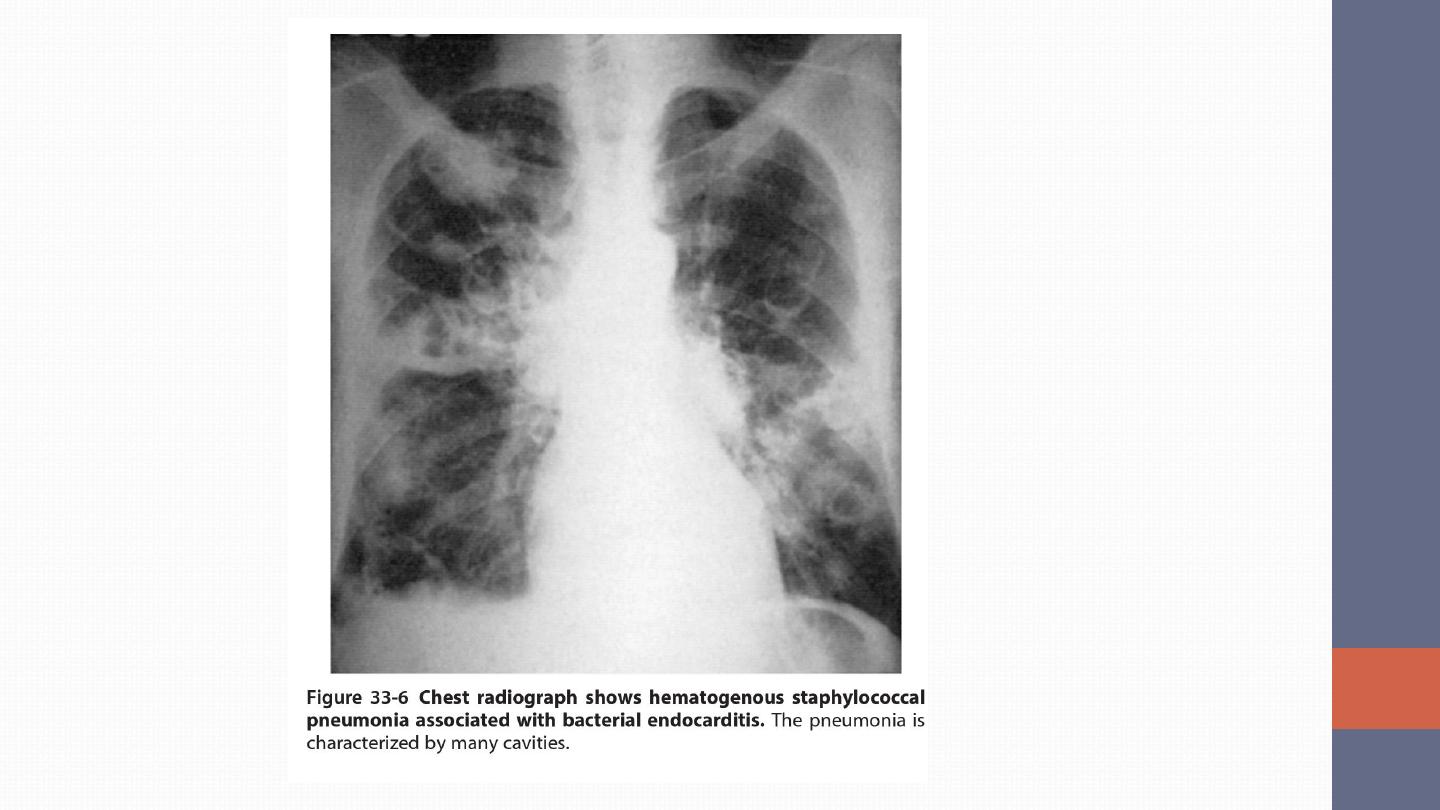

Bacteremia, Sepsis, and Infective Endocarditis S. aureus
bacteremia may be complicated by sepsis, endocarditis, vasculitis,
or metastatic seeding (establishment of suppurative collections at
other tissue sites). Among the more commonly seeded tissue sites
are bones, joints, kidneys, and lungs.
•
Acute right-sided tricuspid valvular S. aureus endocarditis is
most often seen in injection drug users
•
S. aureus is one of the more common causes of prosthetic-valve
endocarditis. This infection is especially fulminant in the early
postoperative period and is associated with a high mortality rate
Other infections:
•
Prosthetic Device–Related Infections
•
Urinary Tract Infections
•
Toxin-Mediated Diseases ; FOOD POISONING Even if the bacteria
are killed by warming, the heat-stable toxin is not destroyed. The
onset of illness is rapid, occurring within 1–6 h of ingestion. The
illness is characterized by nausea and vomiting, although diarrhea,
hypotension, and dehydration also may occur

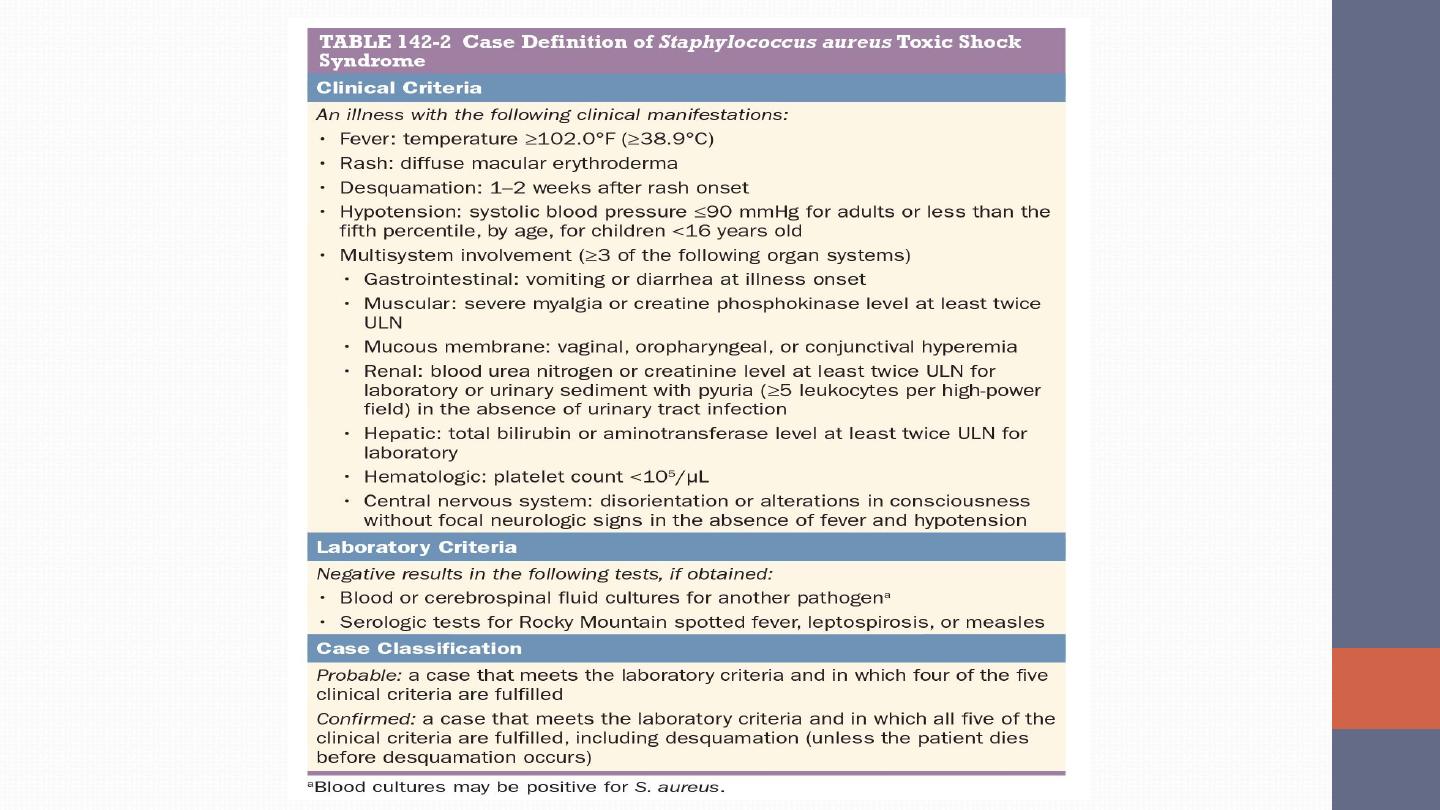
TOXIC SHOCK SYNDROME The clinical presentation is similar in
menstrual and nonmenstrual TSS. Evidence of clinical S. aureus
infection is not a necessary . TSS results from the elaboration of an
enterotoxin or the structurally related enterotoxin-like TSST-1

COAGULASE-NEGATIVE
STAPHYLOCOCCAL INFECTIONS
S. epidermidis is the CoNS species most often associated with
prosthetic device infections
. Infection is a two-step process, with
initial adhesion to the device followed by colonization. S.
epidermidis is uniquely adapted to colonize these devices because
of its capacity to elaborate the extracellular polysaccharide
(glycocalyx or slime) that facilitates formation of a protective biofilm
on the device surface.
CLINICAL SYNDROMES CoNS cause a diverse array of prosthetic
device–related infections, including those that involve prosthetic
cardiac valves and joints, vascular grafts, intravascular devices,
and CNS shunts. In all of these settings, the clinical presentation is
similar. The signs of localized infection are often subtle, the rate of
disease progression is slow, and clinical presentation is slow.
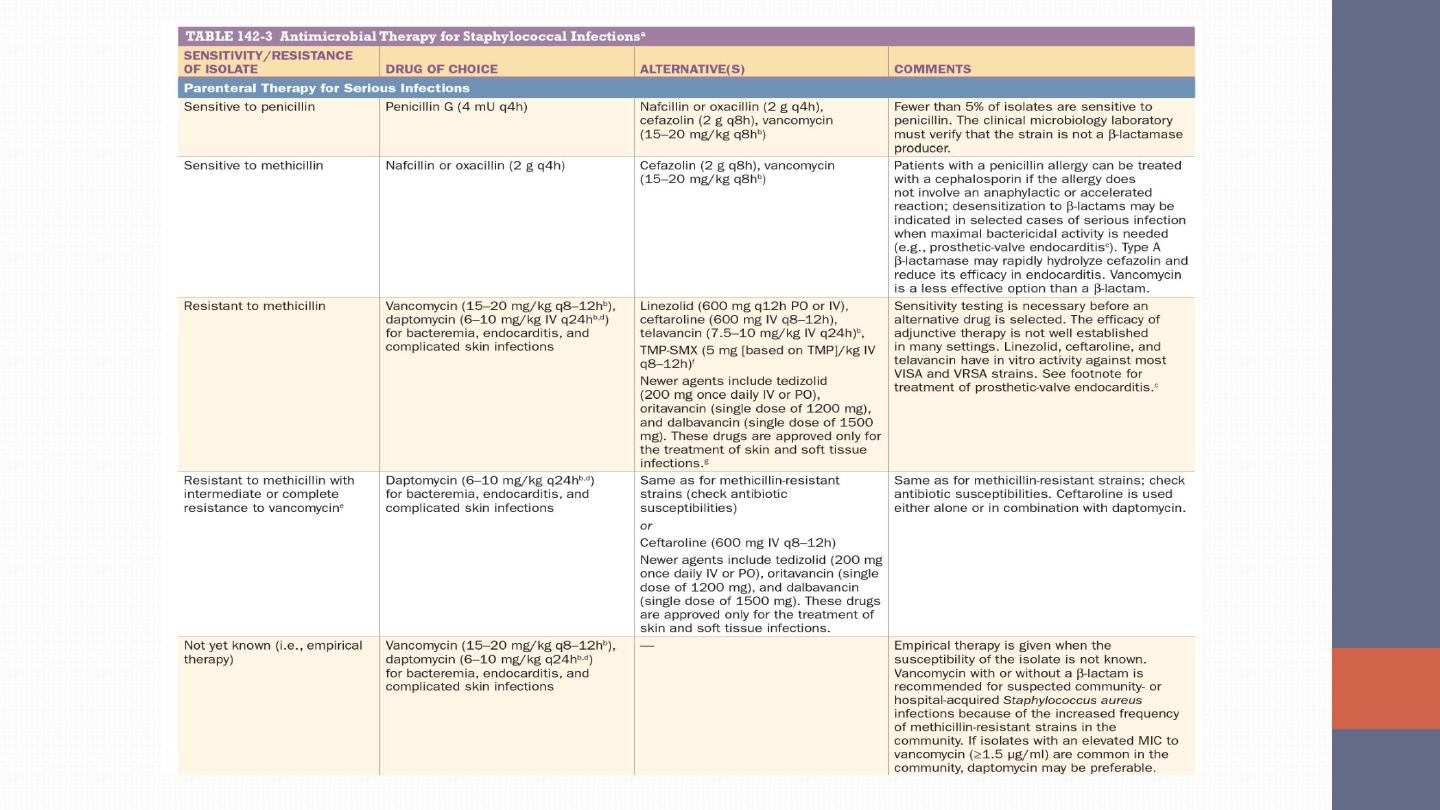
TREATMENT
•
Source control (e.g.,), coupled with rapid institution of appropriate
antimicrobial therapy.
•
Few strains of staphylococci (≤5%) remain susceptible to penicillin.
•
Penicillin-resistant isolates are treated with semisynthetic penicillinase-
resistant penicillins (SPRPs), such as oxacillin or nafcillin.
•
The isolation of MRSA was reported within 1 year of the introduction
of methicillin. Since then, the prevalence of MRSA has steadily
increased
•
Vancomycin or daptomycin is recommended as the drug of choice for
the treatment of invasive MRSA infections.

•
In 2002, the first clinical isolate of fully vancomycin-resistant S.
aureus (VRSA) was reported treated with daptomycin or
Linezolid—the first oxazolidinone—is bacteriostatic against
staphylococci; it offers the advantage of comparable bioavailability
after oral or parenteral administration.
•
Ceftaroline is a fifth-generation cephalosporin with bactericidal
activity against MRSA (including strains with reduced
susceptibility to vancomycin and daptomycin).
Combinations of antistaphylococcal agents have been used to
enhance bactericidal activity in the treatment of deep-seated
infections, to shorten the duration of therapy (e.g., for right-sided
endocarditis), or to optimize empirical therapy when the
susceptibility of the isolate to methicillin is not yet known (e.g.,
using a β-lactam plus vancomycin). Among the additional
antimicrobial agents often used are rifampin, gentamicin, fusidic
acid, doxycycline and clindamycin.