1
THI QAR U. MEDICAL COLLEGE LECTURES 2017
DEPARTMENT OF INTERNAL MEDICINE Dr. FAEZ KHALAF, SUBSPACIALITY GIT
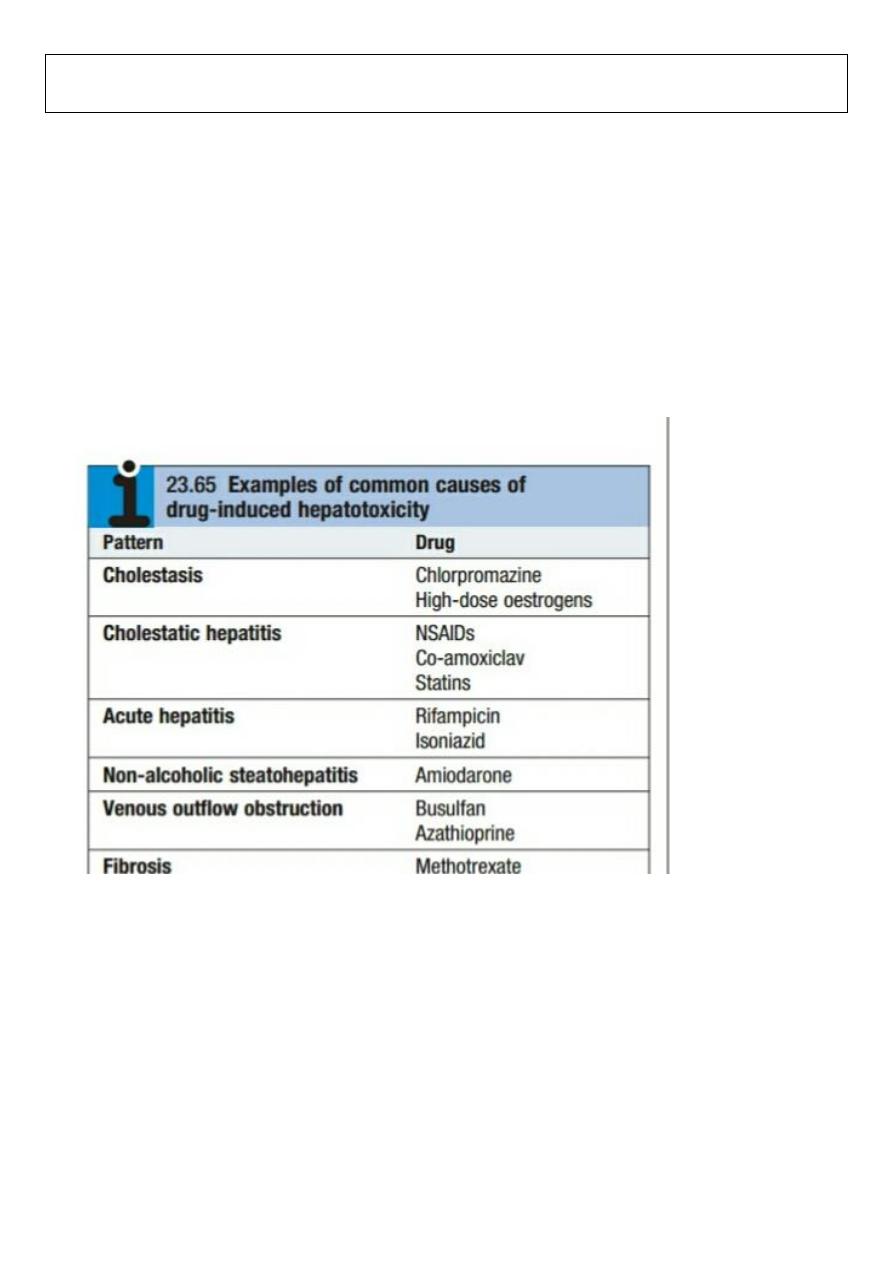
Drug & Toxin-Induced Hepatic Disease
• Mechanism of injury:
1.
Direct toxicity (Drugs are often divided into dose-dependent, or predictable, hematotoxins and dose-
independent, or unpredictable (idiosyncratic), hematotoxins)
2.
Hepatic conversion of a xenobiotic to an actual toxin
3.
Immune mechanisms
drug or metabolite acts as hapten
• Types of injury:
1.
Hepatocyte necrosis
2.
Cholestasis
3.
Insidious liver dysfunction
• Reye syndrome – children given ASA; extensive accumulation of fat droplets within hepatocytes
(micro vesicular steatosis)
Reye syndrome
•
Usually in children
< 4 years
of age
.
•
Often follows a chickenpox or influenza infection
•
Mitochondrial damage ( virus, salicylates)
1. Disruption of urea cycle increased serum ammonia
2. Defective beta-oxidation of fatty acids
•
Micro vesicular steatosis (Salicylate effect)
•
Clinical findings:
2
1. Encephalopathy
2. Hepatomegaly liver failure
•
Laboratory findings:
1. Transaminasemia
2. Normal to slight inc. total bilirubin
3. Increased serum ammonia
ACETAMINOPHEN
•
Acetaminophen (paracetamol) is a widely used analgesic available without prescription. It is safe when taken
in the recommended therapeutic dose of
1 to 4 g daily
, but hepatotoxicity produced by self-poisoning with
acetaminophen has been recognized since the 1960s. Despite the effectiveness of thiol-based antidotes,
acetaminophen remains the most common cause of drug-induced liver injury in most countries and an important
cause of acute liver failure. Para suicide and suicide are the usual reasons for overdose.
•
Single doses of acetaminophen that exceed
7 to 10 g (140 mg/kg body weight in children)
may cause liver
injury, but this outcome is not inevitable. Severe liver injury
(serum ALT level greater than 1000 U/L)
or fatal cases
usually involve doses of at least
15 to 25 g,
•
Among heavy drinkers and chronic liver diseases, daily acetaminophen doses of
2 to 6 g
have been
associated with fatal hepatotoxicity.
3
•
Self-poisoning with acetaminophen is most common in young women, but fatalities are most frequent in
men, possibly because of alcoholism and late presentation.
•
In the first two days after acetaminophen self-poisoning, features of liver injury are not present. Nausea,
vomiting, and drowsiness are often caused by concomitant ingestion of alcohol and other drugs.
After 48 to 72
hours,
serum ALT levels may be elevated, and symptoms such as anorexia, nausea and vomiting, fatigue, and malaise
may occur. Hepatic pain may be pronounced. In severe cases, the course is characterized by repeated vomiting,
jaundice, hypoglycemia, and other features of acute liver failure, particularly coagulopathy and hepatic
encephalopathy.
•
Indicators of a poor outcome include grade IV hepatic coma, acidosis, severe and sustained impairment of
coagulation factor synthesis, renal failure, and a pattern of falling serum ALT levels in conjunction with a worsening
prothrombin time.
Management:
•
In patients who present within
four hours
of ingesting an excessive amount of acetaminophen, the stomach
should be emptied with a wide-bore gastric tube. Osmotic cathartics or binding agents have little if any role in
management. Charcoal hemoperfusion has no established role. The focus of management is on identifying patients
who should receive thiol-based antidote therapy and, in those with established severe liver injury, assessing the
patient's candidacy for liver transplantation.
•
Cases of acetaminophen-induced severe liver injury are virtually abolished if N acetyl cysteine ( NAC ) is
administered within
12 hours
and possibly within
16 hours of
acetaminophen ingestion. After
16 hours,
thiol
donation is unlikely to affect the development of liver injury because oxidation of acetaminophen to NAPQI with
consequent oxidation of thiol groups is complete and mitochondrial injury and activation of cell death pathways are
likely to be established.
NAC DOSE AND ADMINISTERATION :
•
Oral administration is preferred in the United States,with a loading dose of
140 mg/kg
followed by
administration of 70 mg/kg every 4 hours for 72 hours.
This regimen is highly effective, despite the theoretical
disadvantage that delayed gastric emptying and vomiting may reduce intestinal absorption of NAC. In Europe and
Australia, NAC is administered by slow bolus intravenous injection followed by infusion
(150 mg/kg over 15 minutes
in
200 mL of 5%
dextrose, with a second dose of
50 mg/kg 4 hours later,
if the blood acetaminophen levels indicate a
high risk of hepatoxicity, and
a total dose over 24 hours of 300 mg/kg
).The intravenous route may be associated with
a higher rate of hypersensitivity reactions because of the higher systemic blood levels achieved.
4
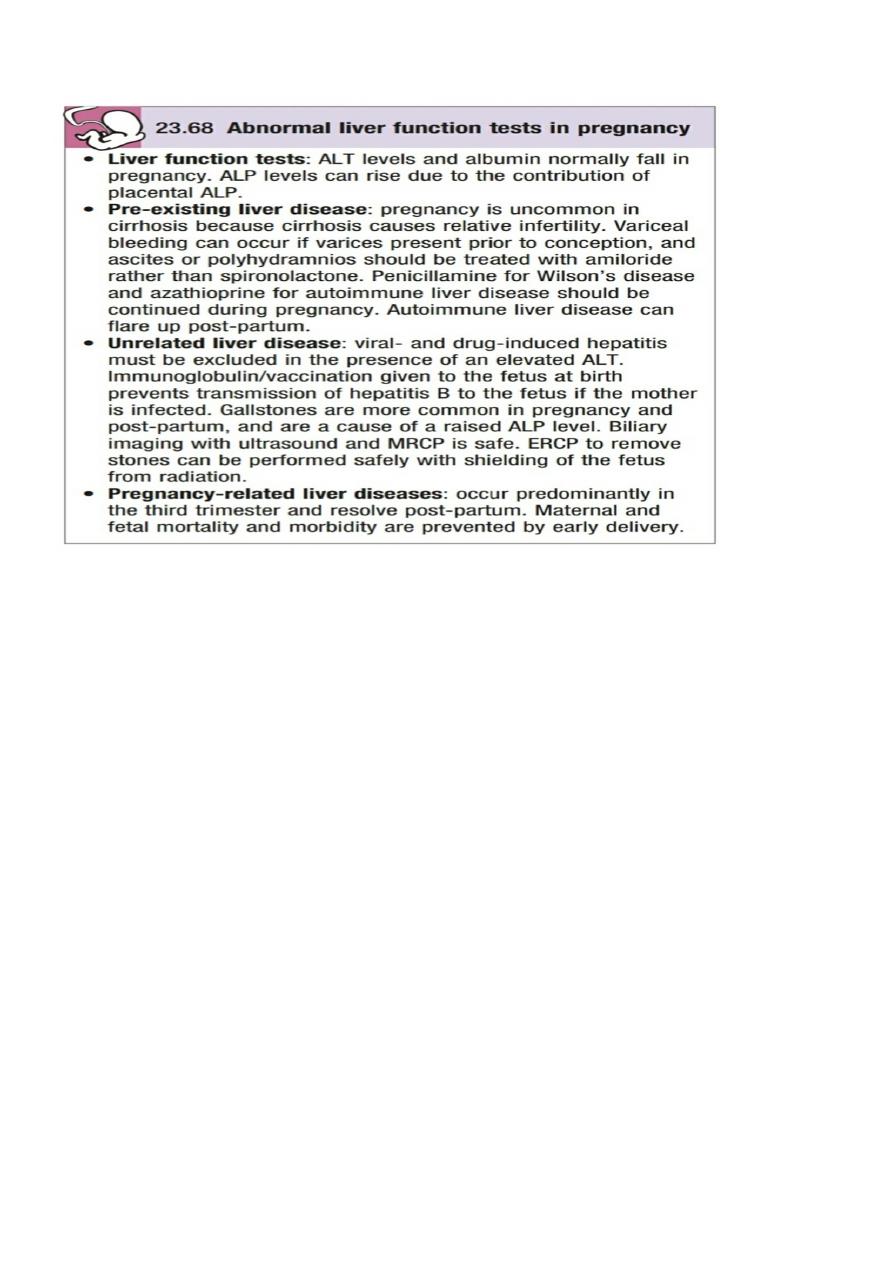
Hepatic Disease Associated with Pregnancy
Pre-eclampsia
•
Hypertension, proteinuria, dependent pitting edema in the third trimester
•
HELLP
syndrome
hemolytic anemia with schistocytes, elevated liver enzymes, low
platelet (due to DIC)
•
Morphology:
fibrin deposition in periportal sinusoids
hemorrhage into space of Disse
periportal hepatocellular coagulative necrosis
The HELLP syndrome (hemolysis, elevated liver enzymes and low platelets) is a variant of pre-eclampsia
that tends to affect multiparous women. It usually
presents at
27–36
weeks of pregnancy with hypertension,
proteinuria and fluid retention.
Jaundice only occurs in
5%
of cases. Blood tests may show low hemoglobin, with fragmented red cells,
markedly elevated serum transaminases and raised D-dimers.
The condition can be complicated by hepatic infarction and rupture.
Maternal complications also include disseminated intravascular coagulation and placental abruption.
Maternal mortality is
1%
and perinatal mortality can be up to
30%.
Delivery usually leads to prompt resolution,
and disease recurs in fewer than
5%
of subsequent pregnancies.
5
Acute fatty liver of pregnancy (AFLP)
•
sub-clinical hepatic dysfunction to hepatic failure, coma and death
•
Abnormality in beta-oxidation of fatty acids
•
3
rd
trimester; with multiple metabolic defects
•
diagnosis depends on:
a) high index of suspicion
b) characteristic micro vesicular steatosis demonstrated on frozen tissue
sections OR with stain (
oil red-O or Sudan black
)
•
Treatment: termination of pregnancy
This is more common in twin and first pregnancies, and may arise more frequently when the fetus is male .
It occurs in 1 in 14 000 pregnancies in the USA
.
It typically presents between 31 and 38 weeks of pregnancy
with vomiting and abdominal pain followed by jaundice. In severe cases, this may be followed by lactic acidosis,
coagulopathy, encephalopathy and renal
failure. Hypoglycaemia can also occur .
. Differentiation from toxaemia of pregnancy (which is more common) can be achieved by the finding of high serum
uric acid levels and the absence of haemolysis. Overlap between acute fatty liver of pregnancy, HELLP and toxaemia
of pregnancy can occur.
Early diagnosis, specialist care and delivery of the fetus have led to a fall in maternal and perinatal mortality to
1%
and
7%
respectively
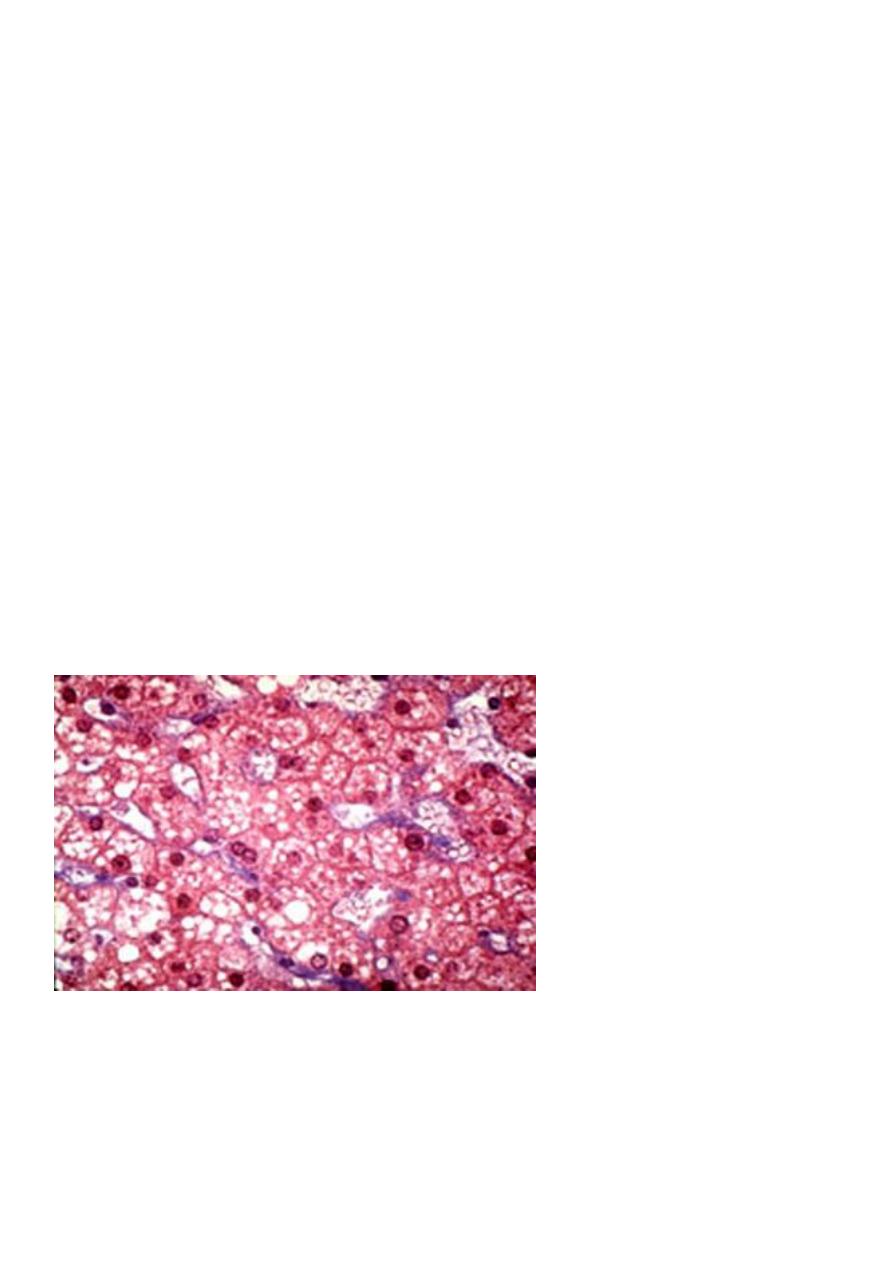
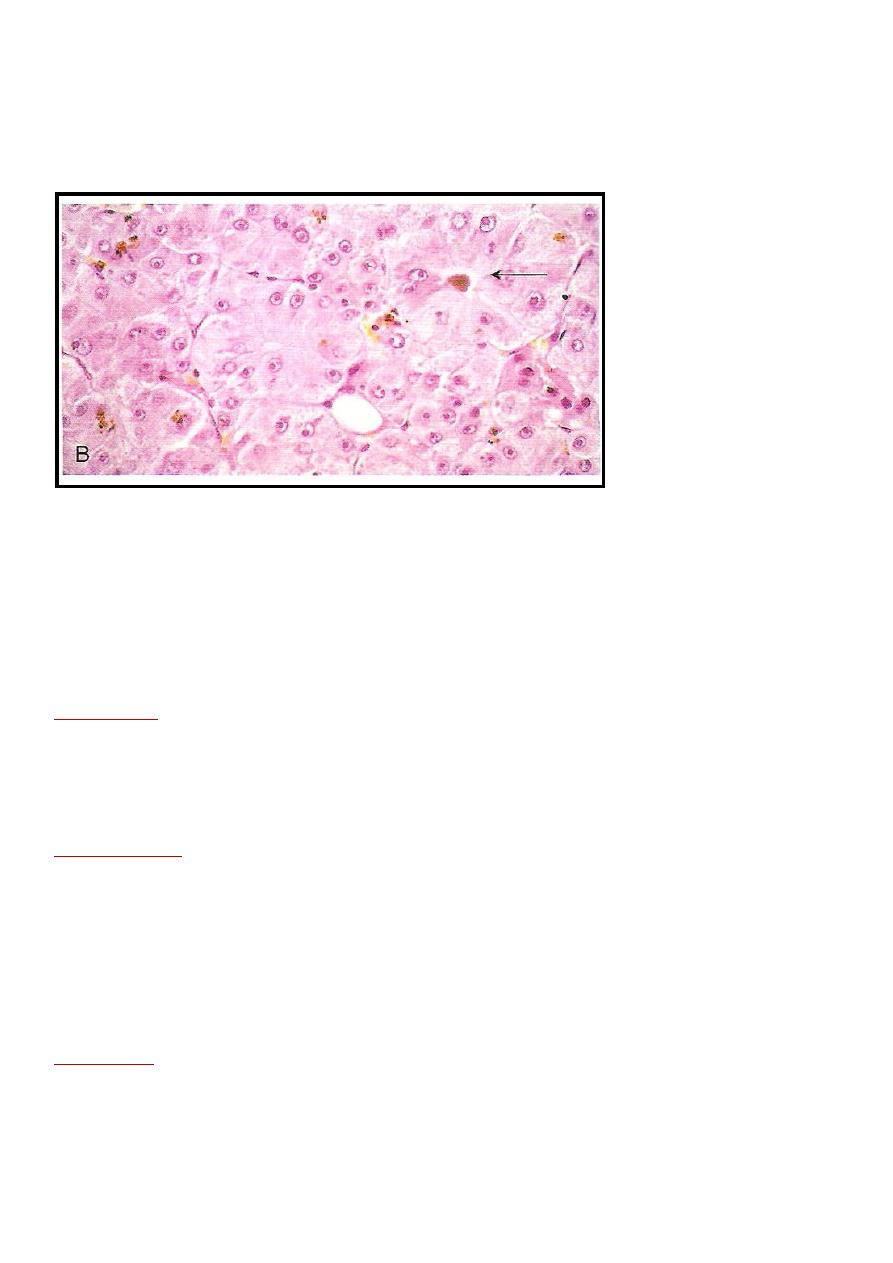
Acute fatty liver of pregnancy: lobular parenchyma characterized by microvesicular steatosis and a small number of
lymphocytes. (H&E)
6
Intrahepatic cholestasis of pregnancy
•
Characteristics:
a) onset of pruritus in
3
rd
trimester
b) darkening of urine with occ. light stools
c) jaundice – conjugated hyperbilirubinemia
•
Mechanism: altered hormonal state + biliary secretion defects
cholestasis
•
Increased incidence of fetal distress, stillbirth and prematurity
This accounts for
20%
of cases of jaundice in pregnancy
;
it usually occurs in the third trimester of pregnancy but can arise earlier. It may be linked with intrauterine growth
retardation and premature birth, but is most characteristically associated with intrauterine fetal death if the
pregnancy goes beyond
36 weeks
of gestation.
The condition characteristically presents with itching an cholestatic LFTs
.
Bile salts are elevated in the serum and this represents a useful clinical test. Delivery leads to resolution and should
be considered
from
36 weeks
onwards
Pregnancy should not be allowed to continue beyond term because of a steep rise in the risk of intrauterine death.
UDCA
(15 mg/kg daily)
effectively controls itching and probably prevents premature birth.
The major issue with UDCA in acute
cholestasis of pregnancy is the relatively long time required to achieve effective levels within the bile pool,
Cholestasis recurs in
60%
of future pregnancies.
Nodules & Tumors
Nodular Hyperplasia
•
non-cirrhotic liver nodules
•
types:
Focal nodular hyperplasia
spontaneous mass lesion; female preponderance
Morphology:
a) central stellate scar with large arterial vessels
exhibiting fibromuscular hyperplasia (+) narrowed
lumen
b) Intense alymphocytic infiltration
c) bile duct proliferation
7
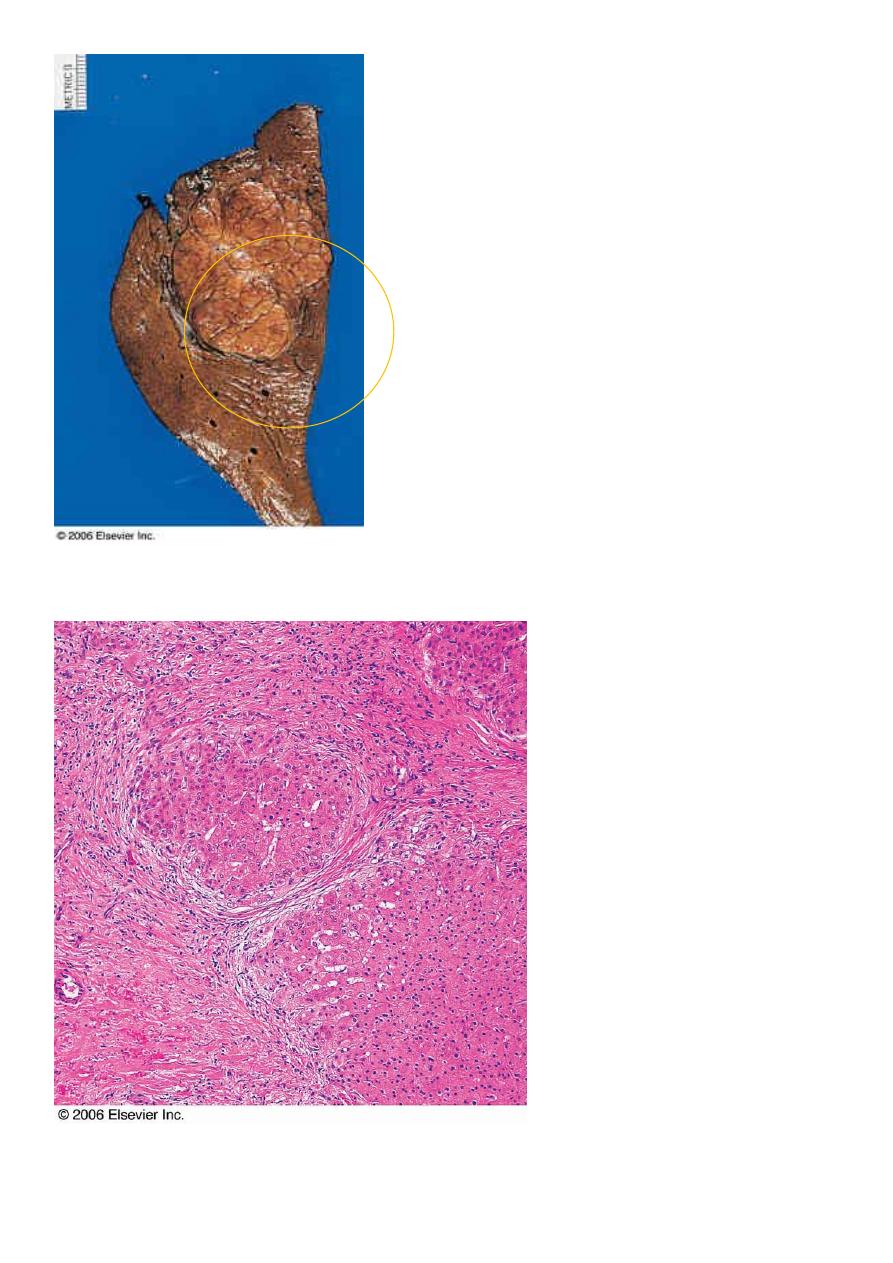
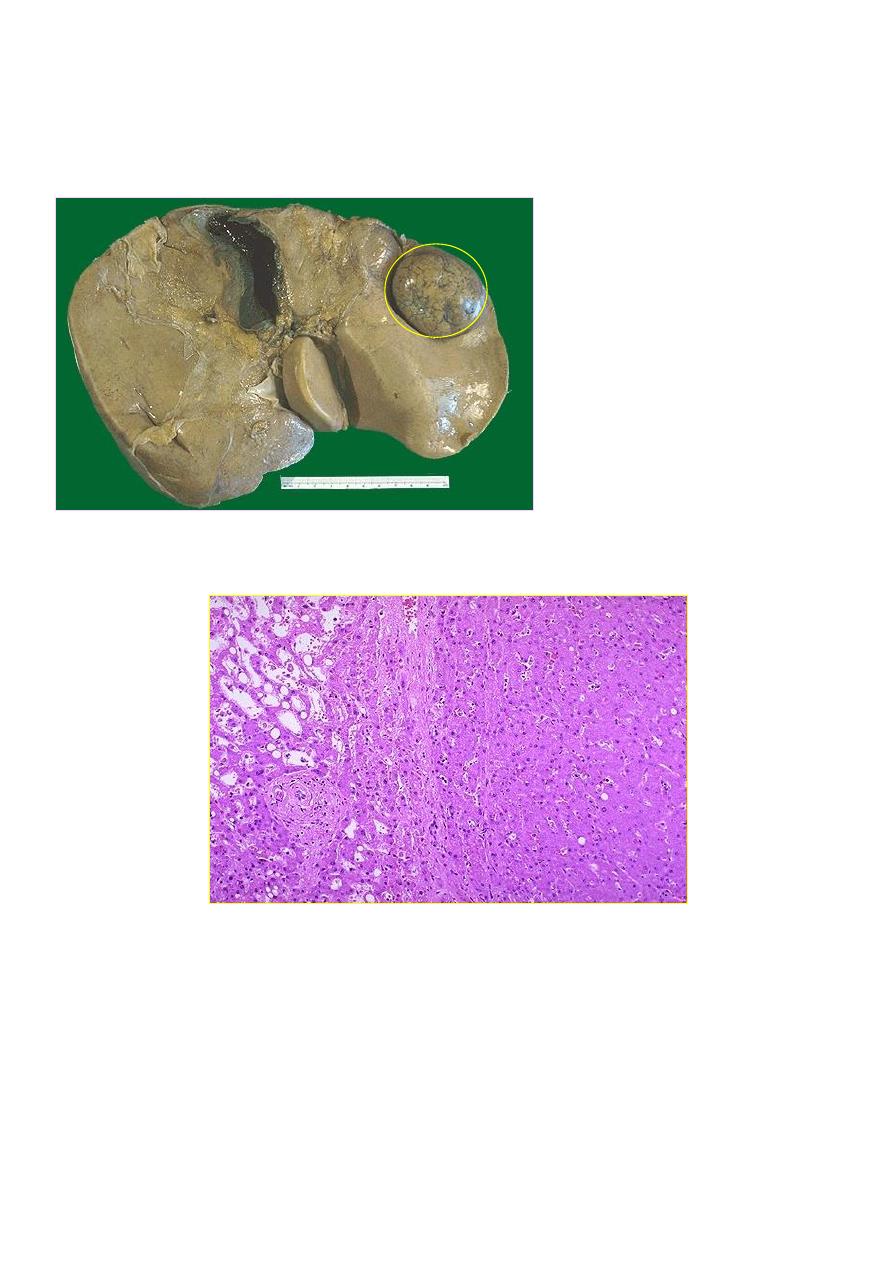
Focal Nodular Hyperplasia: Subcapsular
solid mass with central scar, composed of
the normal components of liver lobule
Central portion of nodular hyperplasia showing the interphase between the fibrous scar
and the hepatocytic nodules.
8
Nodular regenerative hyperplasia
•
(+) development of portal HPN
•
Associated with conditions affecting intrahepatic blood flow
renal transplant, BM
transplant, vasculitis conditions
•
Morphology: plump hepatocytes surrounded by atrophic cells; no fibrosis
Benign Neoplasms
Cavernous hemangioma
•
Most common; blood vessel tumor
•
Soft nodules
< 2 cm diameter
immediately beneath the capsule
•
Clinical significance: mistaken for metastatic tumors
blind percutaneous biopsies
not done
Liver cell adenomas
•
Cell of origin: hepatocytes
•
Young women on oral contraceptives
regress on discontinuance of use
•
Clinical significance:
1. Present as intrahepatic mass mistaken for HCC
2. If subcapsular (+) rupture intraperitoneal hemorrhage
3. May harbor HCC – rare
Normal liver
Hemangioma
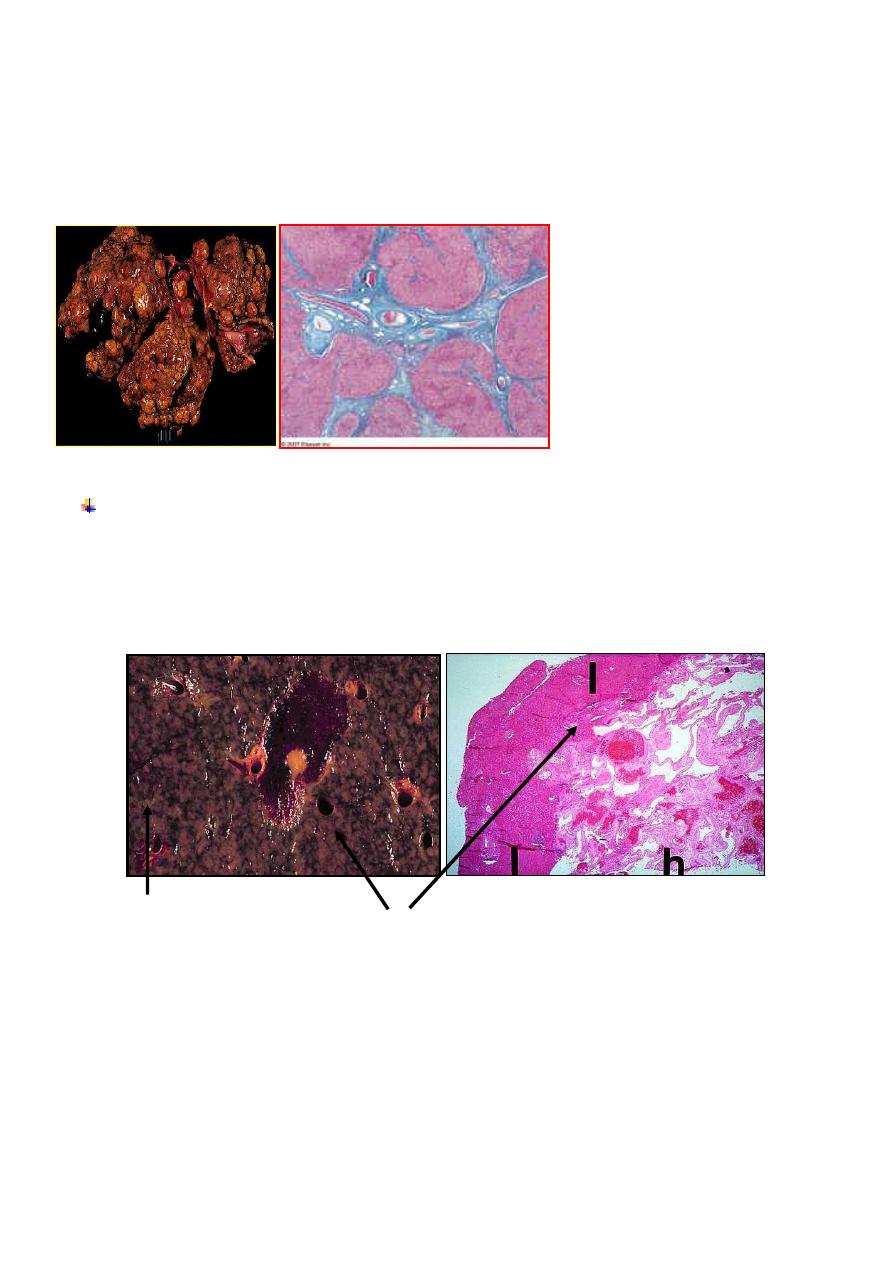
Nodular Regenerative Hyperplasia: non-cirrhotic non-neoplastic nodular transformation of the liver parenchyma.
9
•
Morphology: cords of hepatocytes with clear cytoplasm (w/ glycogen), absent portal tracts &
prominent arterial vessels and draining veins
At the upper right is a well-circumscribed neoplasm that is arising in liver. This
is an hepatic adenoma.
The hepatic adenoma is composed of cells that
closely
resemble
normal
hepatocytes
with
disorganized hepatocyte cords and does not contain
a normal lobular architecture.
Adenoma
Normal liver
11
Malignant Tumors
•
Primary tumors uncommon
often involved in metastatic spread
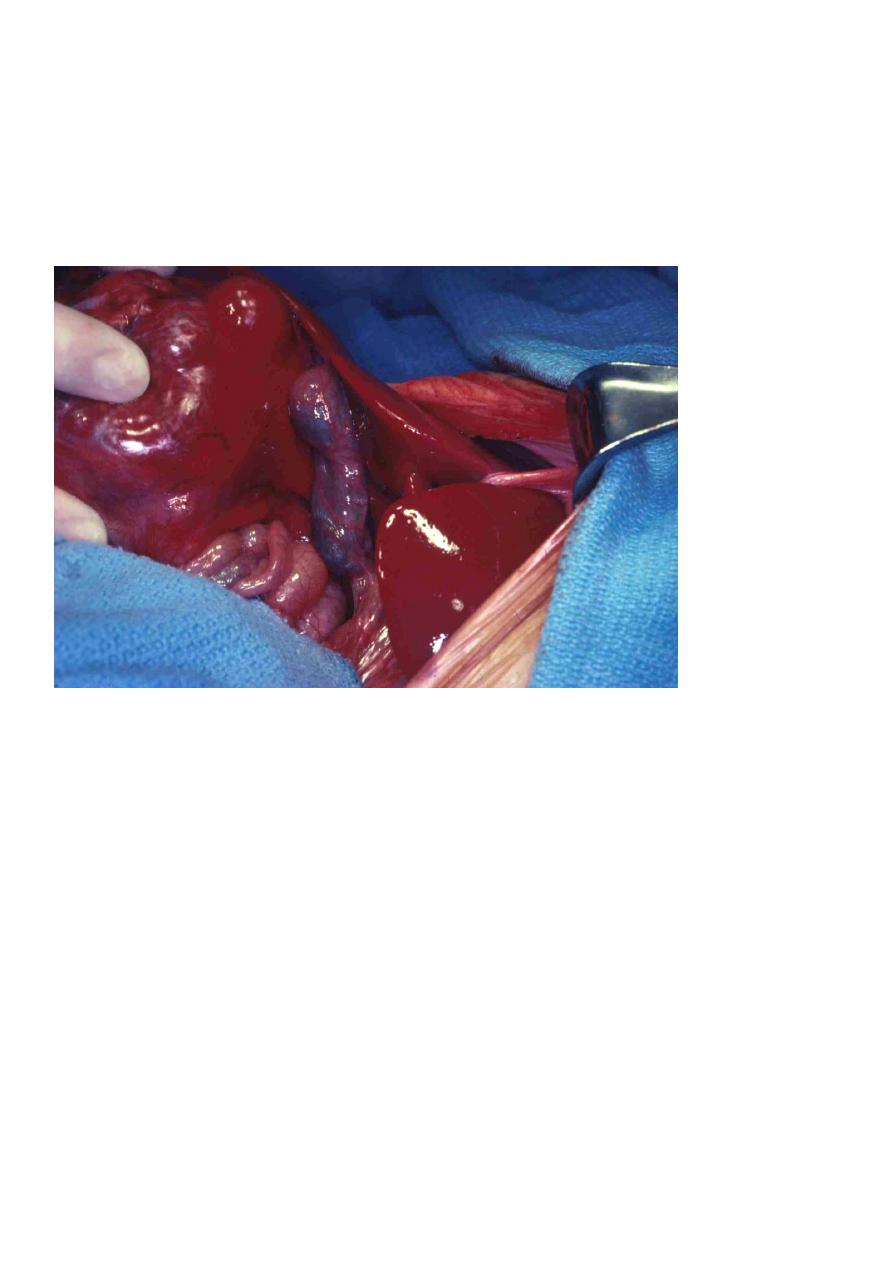
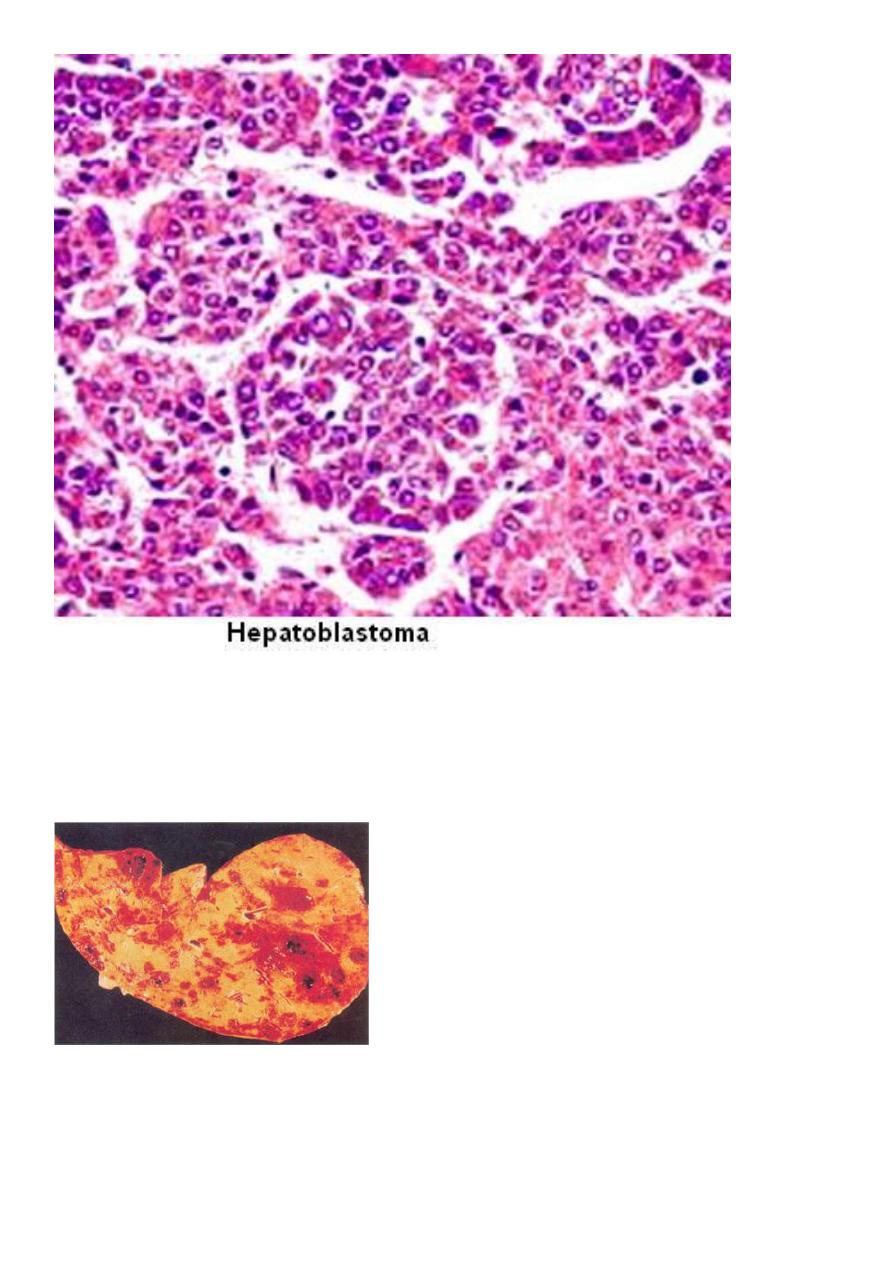
Hepatoblastoma
•
rare; most common liver tumor of young children
•
fatal if not resected
•
(+) activation of
Wnt/β-catenin
signaling pathway
stabilize mutations of
β-catenin
Hepatoblastoma found to be invading the inferior vena cava at the time of surgical exploration.
11
Angiosarcoma
•
rare; malignant endothelial neoplasm
•
associated with exposure to vinyl chloride, arsenic or Thorotrast
•
highly aggressive, metastatic, fatal
Angiosarcoma: Section of liver, showing multiple hemorrhagic tumor deposits.
12
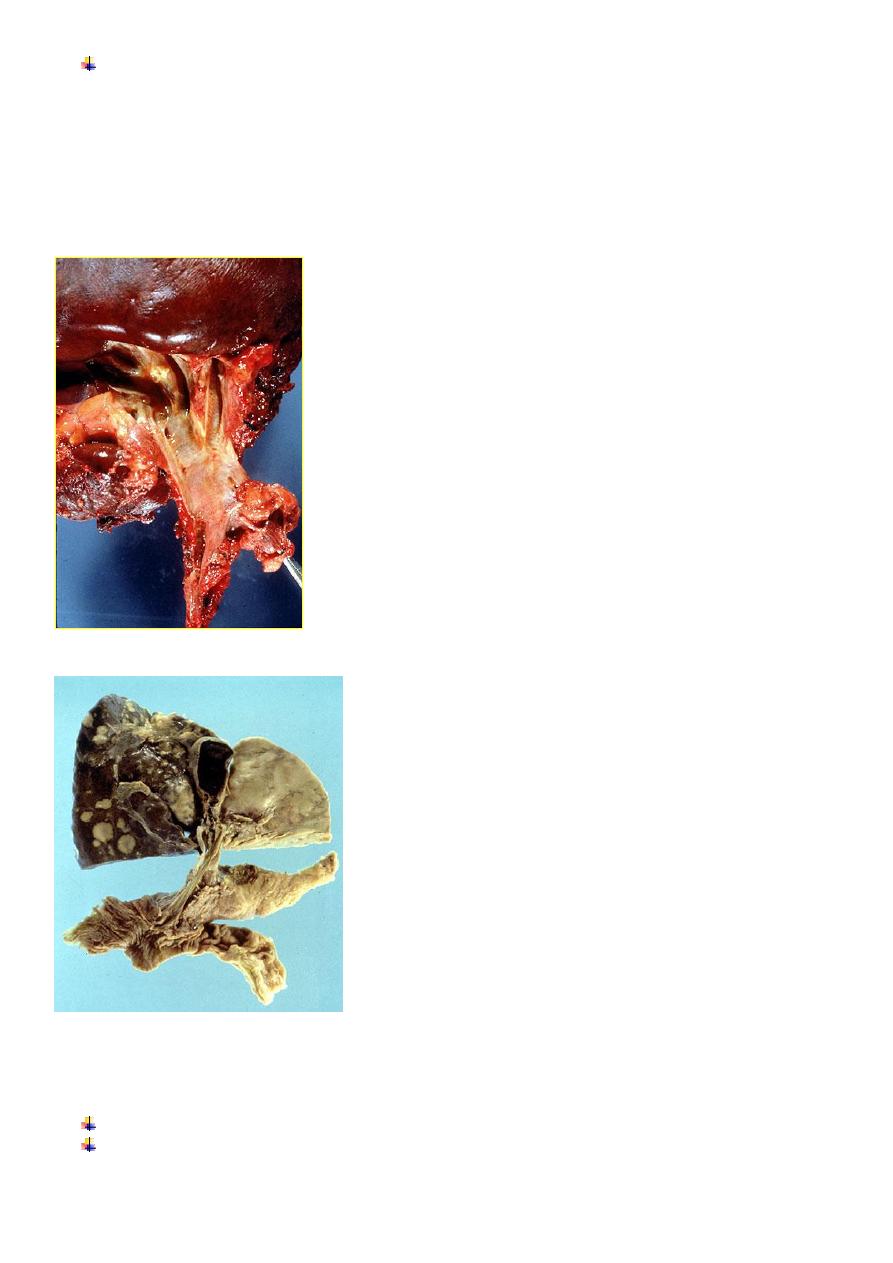
Cholangiocarcinoma
•
malignancy of intrahepatic biliary tract
•
risk factors:
1. Primary sclerosing cholangitis
2. Congenital fibropolycystic diseases of biliary system
3. Previous exposure to Thorotrast
4. Chronic liver fluke infection (O. sinensis)
•
Morphology: resemble sclerosing adenocarcinoma
well-defined glandular & tubular structures
separated by dense collagenous stroma
•
Intrahepatic
cholangiocarcinomas are
classified as either peripheral
or hilar. The hilar variety are
located in the hepatic hilum
region and appear as discrete
masses.
Peripheral cholangiocarcinoma is
the most common and develops in
the interlobular ducts of the liver,
where the interlobular bile duct
branches within the portal triads.
They may be a single or multiple
masses.
13
Hepatocellular Carcinoma
• male
preponderance;
20 – 40 y/o
•
Risk factors:
1. Viral infection – chronic HBV & HCV infection no cirrhosis
2. Chronic alcoholism – (+) cirrhosis
3. Food contaminants – aflatoxin from Aspergillus flavus bind covalently with cellular
DNA (+) p53 mutation
•
>85%
occur in countries with high rates of chronic HBV and HCV infections
Hepatocellular carcinoma (HCC) is the most common primary liver tumour,
the sixth most common cause of cancer worldwide
.
Cirrhosis is present in
75– 90%
of individuals with HCC and is an important risk factor for the disease
The risk is between
1% and 5%
in cirrhosis caused by hepatitis B and C.
There is also an increased risk in cirrhosis due to
haemochromatosis,
alcohol, NASH and α1-antitrypsin deficiency
Chronic hepatitis B infection increases the risk of HCC
100-fold
and is the major risk factor worldwide.
The risk of HCC is 0.4% per year in the absence of cirrhosis and 2–6% in cirrhosis.
The risk is four times higher in HBeAg-positive individuals than in those who are HBeAg-negative.
Hepatitis B
vaccination has led to a
fall in HCC in countries with a high prevalence of
hepatitis B.
The incidence in Europe and North America
has risen recently, probably related to the increased
prevalence of hepatitis C and NASH cirrhosis.
The risk is higher in men and rises with age
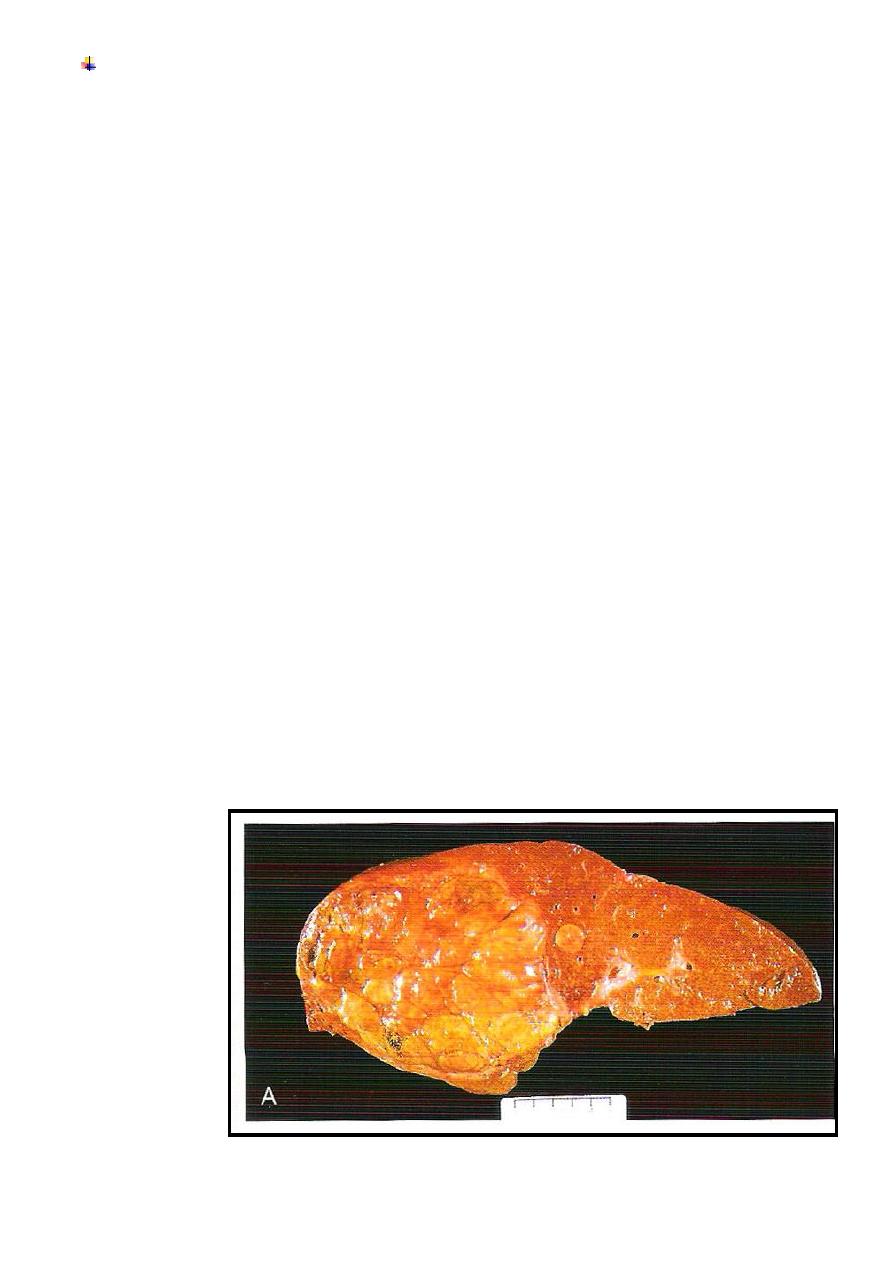
Morphology:
Gross
1. Unifocal large mass
2. Multifocal
3. Diffusely infiltrative
14
Morphology:
Microscopic:
Well differentiated trabecular pattern or acinar, pseudo glandular
pattern
Poorly differentiated pleiomorphic with anaplastic giant cells
Clinical features:
•
upper abdominal pain or fullness
•
malaise, fatigue, weight loss
•
hepatomegaly with irregularity or nodularity
Laboratory:
•
increased tumor markers – serum AFP and
serum CEA
not conclusive
false (+)
in non-neoplastic conditions (e.g.
cirrhosis, chronic hepatitis, massive liver
necrosis, fetal neural defects such as
anencephaly)
Investigations
Serum markers (AFP
)
Imaging( US, CT, MRI
)
Role of screening
Screening for HCC, by ultrasound scanning and AFP measurements at 6-month intervals, is indicated in high-risk
patients, such as those with
cirrhosis due to hepatitis B and C, haemochromatosis, alcohol, NASH and α1-antitrypsin
deficiency
.
It may also be indicated in individuals with chronic hepatitis B (who carry an increased risk of HCC, even in the
absence of cirrhosis).
Management
THE PRESENCE OF CIRRHOSIS
,
TUMOUR SIZE
,
MULTICENTRICITY
,
EXTENT OF LIVER DISEASE
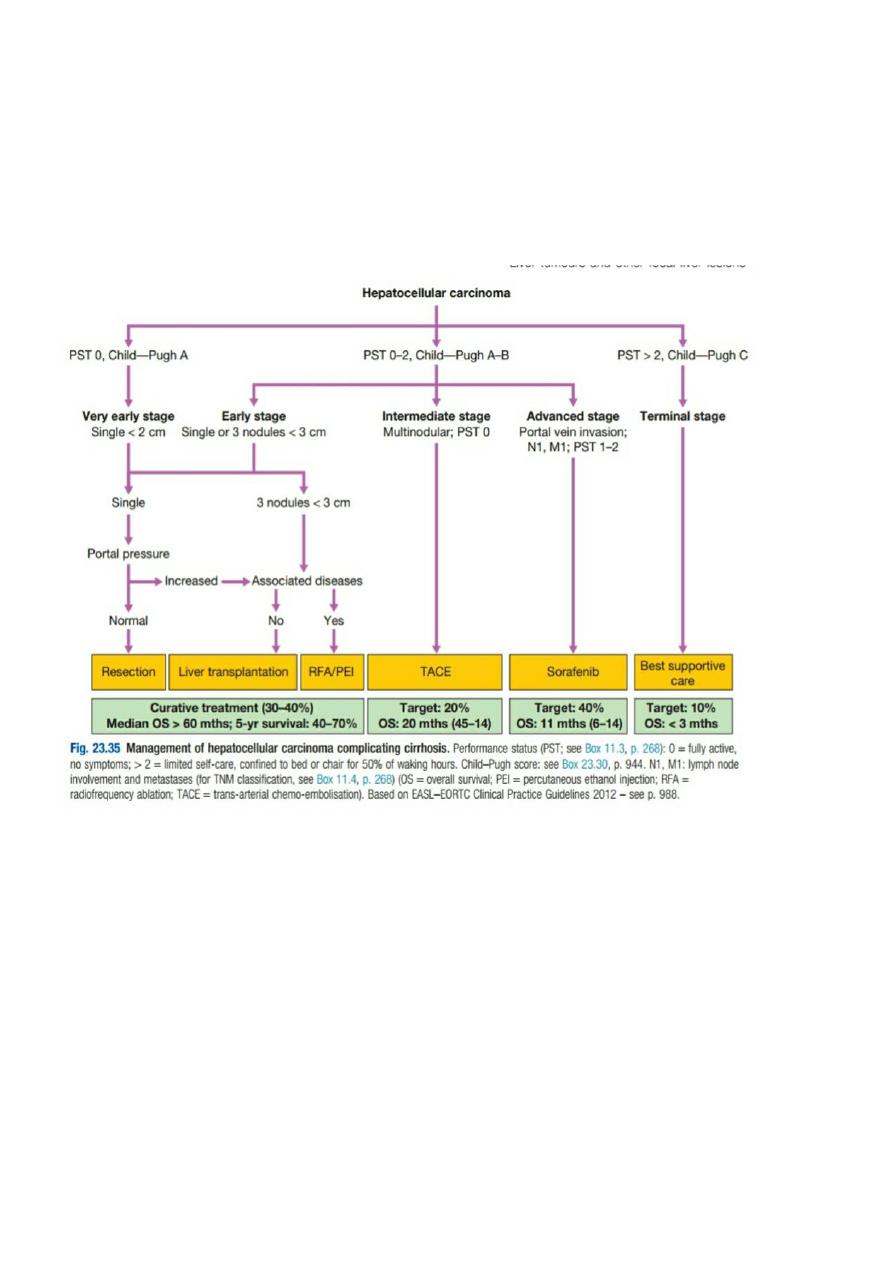
15
(C
HILD
–P
UGH SCORE
)
AND PERFORMANCE STATUS DICTATE
APPROPRIATE THERAPY
.
Hepatic resection
Liver transplantation
Percutaneous therapy
Trans-arterial chemo-embolisation
Chemotherapy
Fibrolamellar hepatocellular carcinoma
This rare variant differs from HCC in that it occurs in young adults, equally in males and females, in the
absence of hepatitis B infection and cirrhosis. The
tumours are often large at presentation and the AFP is usually normal. Histology of the tumour reveals malignant
hepatocytes surrounded by a dense fibrous stroma.
The treatment of choice is surgical resection.
This variant of HCC has a better prognosis following surgery than an equivalent-sized HCC, two-thirds of patients
surviving beyond 5 years
16
Take a home message
In the setting of a cirrhotic patient with a hepatic mass lesion larger than 2 cm in diameter and
suggestive features of hepatocellular carcinoma, an AFP level higher than 200 ng/mL is considered
diagnostic for hepatocellular carcinoma.
Hepatocellular carcinoma can be diagnosed with confidence in patients with a serum AFP level
higher than 200 ng/mL and a mass in the liver.
Secondary malignant tumours
These are common and usually originate from carcinomas in the lung, breast, abdomen or pelvis.
They may be single or multiple. Peritoneal dissemination frequently results in ascites
Clinical features
The primary neoplasm is asymptomatic in 50% of patients, being detected on either radiological, endoscopic
or blood biochemistry screening. There is liver enlargement and weight loss; jaundice may be present.
Investigations
A raised ALP activity is the most common biochemical abnormality but LFTs may be normal.
Ascitic fluid, if present, has a high protein content and may be bloodstained;
cytology sometimes reveals malignant cells. Imaging shows filling defects
(laparoscopy
may reveal the tumour and facilitates liver biopsy)
Management
Hepatic resection can improve survival for slow-growing tumours such as colonic carcinomas, and is
an approach that should be actively explored in patients who are fit for liver resection, have had the
primary tumour resected and in whom extrahepatic disease has been excluded.
Patients with neuro-endocrine tumours, such as
gastrinomas, insulinomas and glucagonomas
, and
those with lymphomas may benefit from surgery, hormonal treatment or chemotherapy.
Unfortunately, palliative treatment to relieve pain is all that is available for most patients; this may
include arterial embolisation of the tumour masses.
