Placenta accrete ,vasa previa
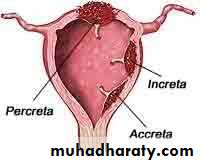
Placenta accreta refers to an abnormal placental implantation in which the anchoring placental villi attach to the myometrium, rather than being contained by decidual cells but not too deep in the uterine wall. This results in a placenta that is abnormally adherent to the uterus(75%).
Placenta increta in which the chorionic villi invade into the myometrium(17%).
Placenta percreta in which the chorionic villi penetrate to or through the uterine serosa and may invade surrounding organs(5-7%).
INCIDENCE
The incidence of placenta accreta approximately 1 in 2500 The marked increase in incidence has been attributed to the increased prevalence of cesarean delivery.
RISK FACTORS
The most important risk factor for placenta accreta is previous uterine surgery and the most common setting is placenta previa after a prior pregnancy delivered by cesarean. The mechanism for the abnormal implantation is thought to be thin, poorly formed, or absent decidua basalis in the scarred area of the lower uterine segment that does not resist deep penetration.The risk of placenta accreta in women with a placenta previa according to past obstetrical history is as follows:
Unscarred uterus, 1 to 5 percent
One previous cesarean birth, 11 to 25 percent
Two previous cesarean births, 35 to 47 percent
Three previous cesarean births, 40 percent
Four or more previous cesarean births, 50 to 67 percent
The risk of placenta accreta increases with an increasing number of cesarean deliveries even in the absence of placenta previa.
Other risk factors: include maternal age greater than 35 years, increasing parity, endometrial defects (Asherman syndrome), and sub mucous leiomyoma. The sex ratio favors females, previous uterine surgery, D&C, uterine radiation, endometrial ablation, uterine anomalies, hypertensive disorder of pregnancy, and smoking, ectopic implantation of placenta including cornual pregnancy.
CLINICAL MANIFESTATIONS
Abnormal placental implantation prevents normal, complete separation of the placenta following delivery. So, the first clinical manifestation of placenta accreta is usually profuse, life-threatening hemorrhage that occurs at the time of attempted manual placental separation. Part or all of the placenta remains strongly adherent to the uterine cavity, and no plane of separation can be developed.
Placenta percreta with bladder invasion can cause hematuria during pregnancy.
DIAGNOSIS
Prenatal diagnosis of placenta accreta is based upon the presence of characteristic findings on ultrasound examination in second and third trimester.
1. Loss of normal hypoechoic retro placental zone
2. Multiple vascular lacunae(irregular vascular spaces) within placenta, giving Swiss cheese appearance.
3. Blood vessels or placental tissues bridging uterine placental margin, myometrium –bladder interface, or cross uterine serosa.
4. Retro placental myometrial thickness of less than 1mm.
5. Numerous coherent vessels visualized with 3-dimensional power Doppler in basal view.
Magnetic resonance has been found by some investigators to be useful when the ultrasound findings are uncertain.
Careful sonographic (trans abdomenal, trans vaginal) evaluation beginning at the time of the second trimester fetal anatomy survey, or no later than 20 to 24 weeks of gestation. the woman and her family can be counseled about the suspected placental abnormality, and an appropriate delivery plan can be developed
Prenatal diagnosis and management appear to improve outcome.
Maternal serum alpha-fetoprotein — Several series and case reports have shown an association between placenta accreta and otherwise unexplained elevations in maternal serum alpha-fetoprotein (MSAFP) concentration.
Histology — Postpartum, the clinical diagnosis of placenta accreta is confirmed by pathological examination of the uterus. Histological findings show that the placental villi are anchored directly on myometrial cells, without an intervening decidual plate.
The diagnosis of focal accreta may be confirmed in the absence of hysterectomy by visualization of these findings in uterine curettings or in fragments of myometrium adherent to the placenta
COMPLICATIONS
1. Massive hemorrhage is the most common complication of placenta accreta. Potential sequelae of massive hemorrhage include disseminated intravascular coagulopathy(dilutional and consumption), adult respiratory distress syndrome, renal failure, acute transfusion reaction, transfusion related lung injury.2. Placenta accreta has become one of the most common indications for peripartum hysterectomy.
3. Placenta percreta with bladder invasion can cause hematuria, which may be severe. Cystoscopy, intentional cystotomy may be need, Partial cystectomy may also done. Ideally, a urogynecologist, urologist, or gynecologic oncologist should be consulted in cases where the bladder or uretric envolvement.
4. local organ damage(bowel, neurovascular structures in the retroperitoneum and lateral pelvic side walls from placental implantation and its removal)
5. Amniotic fluid embolism.
6. Post-operative repeated surgery.
7. Post operative thromboembolism, infection, multisystem organ failure, maternal death(6-7%).
MANAGEMENT
Preoperative management
A plan for managing women with a high likelihood of placenta accreta should be developed preoperatively. The goal is to provide information (informed consent) and plan interventions that will reduce the risk of massive hemorrhage, massive transfusion as well as the substantial morbidity and potential mortality associated with it. Cesarean hysterectomy is usually performed because the placenta cannot be removed any other way and, if left in situ, sub involution often results in postpartum hemorrhage.
Management by a multidisciplinary team, including expert obstetrical surgeons, anesthesiologists, neonatologists, and blood bank and nursing personnel, and delivery in a tertiary care facility result in improved outcomes and fewer complications than standard obstetrical care.
Planned delivery is associated with less intraoperative blood loss than emergency delivery.
One approach is to assess fetal lung maturity at approximately 35 to 36 weeks of gestation followed by scheduled delivery if the test is mature. If immature indices are noted, we administer a course of antenatal glucocorticoids and deliver after 48 hours.
A preoperative anesthesia consultation should be obtained.
Adequate blood and clotting factors should be available at the time of delivery. Cell saver technology should be considered, if available. Directed donation and autologous donation are other options that can be considered.
The use of Factor VIIA for control of obstetric hemorrhage appears to be of value.
An intensive care unit should be available for postoperative care, as needed
Normovolemic hemodilution may be considered preoperatively. The procedure reduces the baseline hematocrit by removing red blood cells and replacing them with crystalloid or colloid. Thus, intraoperative bleeding results in less loss of red blood cell mass and less need for homologous blood transfusion.
Balloon catheterization — We frequently utilize balloon catheters for our patients with suspected accreta and believe that these catheters are helpful in controlling hemorrhage. Balloon occlusion of the aorta or internal iliac vessels is intended to prevent hemorrhage at the time of mobilization of the bladder flap and dissection of the lower uterine segment.
The procedure involves preoperative placement of balloon catheters retrograde through the femoral arteries under fluoroscopic guidance.
Intraoperative management — A vertical skin incision provides good exposure. The pelvis is inspected for evidence of percreta and the location of any collateral blood supply. A bladder flap is created if the area appears clear of adhesions and placenta. A vertical uterine incision is made above the placenta to avoid disrupting it and the infant is delivered.
A definitive decision regarding conservative management or cesarean hysterectomy should be made preoperatively.
The uterine incision is oversewn circumferentially to decrease blood loss. The hysterectomy is then performed with meticulous attention to securing hemostasis.
Hypo gastric artery ligation should not be performed because it is time consuming, ineffective in controlling pelvic hemorrhage in approximately 50 percent of cases, and precludes use of selective pelvic angiography and embolization if needed subsequently.
Uterine conservation
Focal accreta : This entity is typically not diagnosed antepartum, but detected intrapartum because of hemorrhage and/or a partially retained placenta at delivery. Treatment can involve medical (eg, carboprost tromethamine, topical hemostatic agents), radiological (eg, selective arterial occlusion of the internal iliac arteries: internal iliac artery ligation, bilateral uterine artery ligation), mechanical (Bakri balloon tamponade), and surgical attempts to control hemorrhage( curette any remaining placenta from the placental site and then oversew the placental bed, wedge resection of myometrium at the site of focal accreta is performed followed by a layered repair of the myometrial defect. Application of topical hemostatic agents can sometimes control ongoing bleeding .Sometime leaving placenta and curettage the uterus and methotrexate therapy.
women experienced severe morbidity, including sepsis, vesicouterine fistula, and/or uterine necrosis, severe intrauterine synechiae and amenorrheic.
PERINATAL OUTCOME
placenta accreta reported a significant increase in preterm birth, and small for gestational age infants.
Vasa previa
APT test differentiate maternal from fetal blood.The blood is mixed with a small amount of tap water to cause hemolysis. The sample is next centrifuged for several minutes. The pink hemoglobin-containing supernatant is then mixed with 1 mL of 1% NaOH for each 5 mL of supernatant. The color of the fluid is assessed after 2 minutes. Fetal hemoglobin will stay pink and adult hemoglobin will turn yellow-brown since adult hemoglobin will convert to hematin which has a hydroxide ligand.
Vasa previa
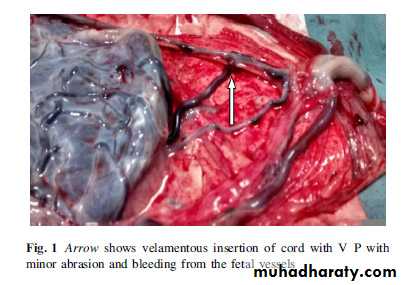
is an obstetric complication defined as "fetal vessels crossing or running in close proximity to the inner cervical os. These vessels course within the membranes (unsupported by the umbilical cord or placental tissue) and are at risk of rupture when the supporting membranes rupture
Vasa previa is present when fetal vessels traverse the fetal membranes over the internal cervical os. These vessels may be from either a velamentous insertion of the umbilical cord or may be joining an accessory (succenturiate) placental lobe to the main disk of the placenta. If these fetal vessels rupture the bleeding is from the fetoplacental circulation, and fetal exsanguination will rapidly occur, leading to fetal death.
Associated condition
Low-lying placenta.
Bilobed placenta.
Multi-lobed placenta.
Succenturiate-lobed placenta.
Multiple pregnancies.
Pregnancies resulting from IVF
Diagnosis:
The diagnosis of vasa previa is considered if vaginal bleeding occurs upon rupture of the membranes.
Concomitant fetal heart rate abnormalities, particularly a sinusoidal pattern.
Ideally, vasa previa is diagnosed antenatally by US with color flow DopplerDiagnosis
moderate vag bleeding + fetal distress
vessels may be palpable through dilated cervix
vessels may be visible on ultrasound
Management :
Consider hospitalization in the third trimester to provide proximity to facilities for emergency cesarean delivery.
Fetal surveillance to detect compression of vessels.
Antenatal corticosteroids to promote lung maturity.
Elective cesarean delivery at 35 to 36 weeks of gestation.
immediate C/S.
Avoid amniotomy as the risk of fetal mortality is 60-70% with rupture of the membranes.