
1
Skin reactions to light
The ultraviolet light is apart of electromagnetic spectrum. The spectrum is usually
divided into seven sections, from the longest to the shortest wavelengths: radio, microwave,
infrared, visible, ultraviolet, x-ray, and gamma-ray radiation.
Photobiology
Sunlight has profound effects on the skin and is associated with a variety of diseases.
Ultraviolet (UV) light causes most photobiologic skin reactions and diseases. The accepted
unit for measurement of the wavelength of light is the nanometer (nm). The solar radiation
that reaches the earth is a continuous spectrum consisting of wavelengths of electromagnetic
energy above 290 nm. UV light is divided into UVA (320 to 400 nm; long wave ), UVB
(290 to 320 nm; middle wave), and UVC (100 to 290 nm; short wave ) but UVC not reach
the earth because will absorb by ozone layer. UVA is further subdivided into two regions:
short-wave UVA, or UVA II (320 to 340 nm), and long-wave UVA, or UVA I (340 to 400
nm). The ratio of UVA to UVB is 20:1 but UVB more erythemogenic than UVA in 1000
times. Eighty percent of UVB and 70% of UVA radiation occur between the hours of 10 am
and 2 pm. More than 90% of UV may penetrate clouds.
UVA.
It is constant throughout the day and throughout the year. The longer wavelengths
of UVA can penetrate more deeply, reaching the dermis and subcutaneous fat. Chronic
exposure to UVA radiation causes the connective tissue degeneration seen in photoaging.
UVB.
UVB produces the most harmful effects and is greatest during the summer. UVB
delivers a high amount of energy to the stratum corneum and superficial layers of the dermis
and is primarily responsible for sunburn, pigmentary changes and photocarcinogenesis. It is
most intense when the sun is directly overhead between 10 am and 2 pm. UVB is absorbed
by window glass
UVC.
UVC is almost completely absorbed by the ozone layer .
Sunburn
Is the normal cutaneous reaction to sunlight. It occur when skin exposed to excess
amount of sun light. UVB penetrates the epidermis and superficial dermis, stimulating the
production and release of prostaglandins, leukotrienes, histamine, interleukin 1 (IL-1) and
tumour necrosis factor α (TNF-α), which cause erythema and pain, tenderness which occur
within 12 to 24 hours after exposure. In sever cases blister will occur. Oedema will occur in
the extremities, face. Fever , nausea , takycardia, hypotension may be present.
The redness is maximal after 1 day and then settles over the next 2 or 3 days, leaving
sheet like desquamation , diffuse pigmentation (a ‘tan’) and, sometimes, discrete lentigines.
د
.
و
ﺳ
ﺎ
م
ﻋ
ﻠ
ﻲ
ﻋ
ﻮ
ض
2
After UV exposure skin pigment undergo two changes.
Two types of pigmentation of the skin in humans occur in response to sun exposure .
The first is immediate pigment darkening (IPD), referred to as the Meirowsky phenomenon.
This is best observed in those with hyperpigmented skins and is most effectively induced by
long-wave UV light (UVA) with less extend to UVB and even visible light . It is transient
and, although rapidly induced, soon fades. Its due to release of already made melanin. The
second is the increased pigmentation that follows the erythemal response. This is the
delayed tanning reaction (DT) and can be seen 48-72h after the exposure of the skin to UV
light and last 10-14 day after sun exposure. Its due to new melanin formation. Its mainly due
to UVB exposure.
The inheritance tendency to tan depend on skin types as follow.
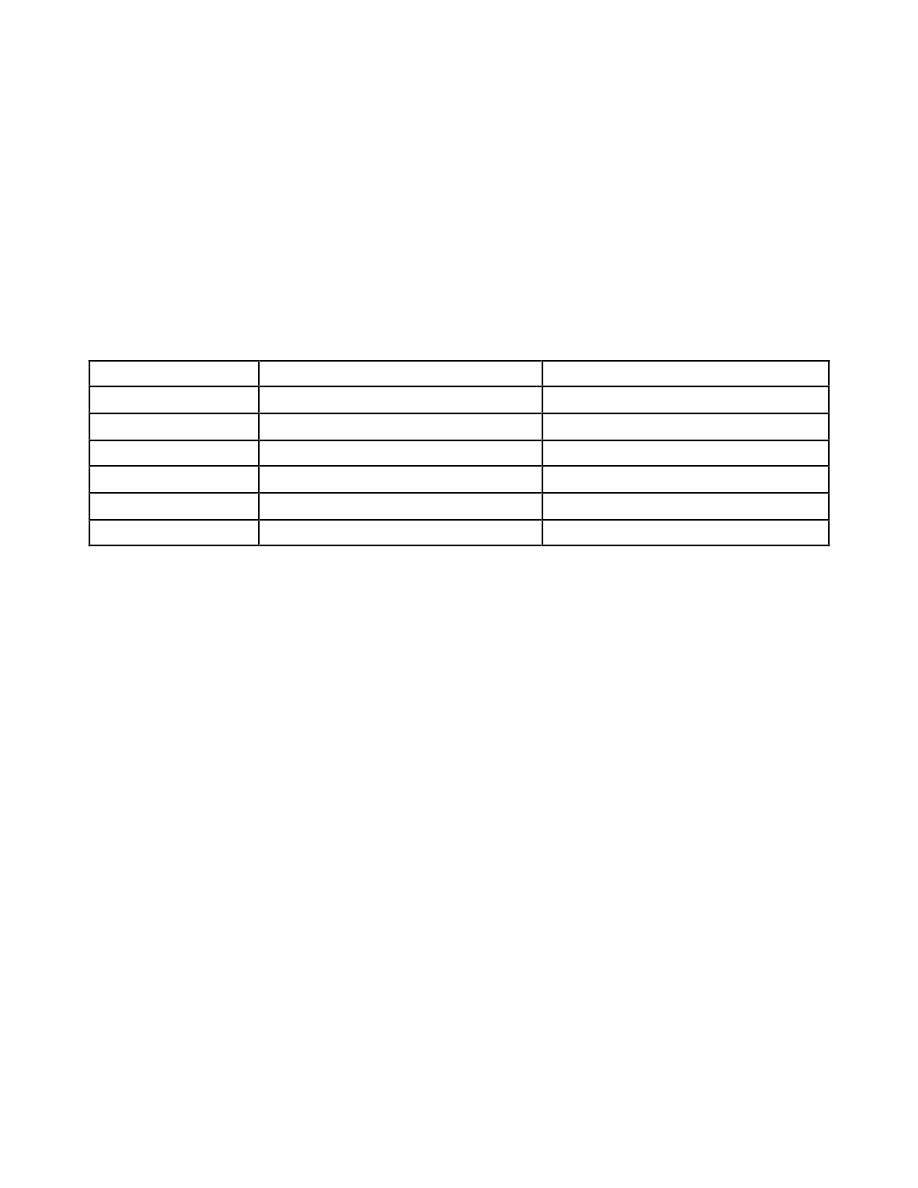
Skin type
Baseline skin colour
Sunburn and tanning history
I
Pale skin, red hair, freckles
Always burns but never tans
II
Fair skin
Always burns, tans minimally
III
white
Burn moderately, tan gradually
IV
Light brown(olive)
Minimal burn, tan well
V
Brown
Rarely burn, tan darkly
VI
Dark brown
Never burn, tan darkly black
Treatment
The treatment is symptomatic. Baths may be cooling and oily shake lotions (e.g. oily
calamine lotion), emollient or creams comforting. Potent topical corticosteroids help if used
early and briefly. Oral aspirin (a prostaglandin synthesis inhibitor) relieves the pain.. aspirin
given 2 tab every two hours for ten tab. Prevention of the sun burn by using sun screams.
Miliaria
Is the retention of sweat as a result of occlusion of eccrine sweat ducts and pores,
produces an eruption that is common in hot, humid climates such as the tropics and during
the hot summer months in temperate climates. The study showed that Staphylococcus
epidermidis, which produces an extracellular polysaccharide substance. They hypothesized
that it is this polysaccharide substance that obstructs the delivery of sweat to the skin surface
in miliaria. The occlusion prevents normal secretion from the sweat glands, and eventually
the backed-up pressure causes rupture of the sweat gland or duct at different levels. The
escape of sweat into the adjacent tissue produces miliaria. Depending on the level of the
injury to the sweat gland or duct, several different forms of miliaria are recoanized.
Miliaria Crystalline . characterized by small, clear, and very superficial vesicles in
bedridden, ferial patient ,the lesions are asymptomatic and their duration is short lived
because they tend to rupture at the slightest trauma. The lesions are self-limited; no
treatment is required.

3
Miliaria Rubra . The lesions of miliaria rubra appear as discrete, extremely pruritic,
erythematous papulovesicles accompanied by a sensation of prickling, burning, or tingling.
They later may become confluent on a bed of erythema. The sites most frequently affected
are the antecubital and popliteal fossae, the trunk.
Miliaria Pustulosa. Miliaria pustulosa is always preceded by some other dermatitis
that has produced injury, destruction, or blocking of the sweat duct. The pustules are
pruritic, superficial, and independent of the hair follicle . Contact dermatitis, lichen simplex
chronicus, and intertrigo are some of the associated diseases, although pustular miliaria may
occur several weeks after the disease has subsided.
Miliaria Profunda. Nonpruritic, flesh-colored, deep-seated, whitish papules
characterize this form of miliaria. It is asymptomatic, usually lasts only 1 hour after
overheating has ended, and is concentrated on the trunk and extremities.
Treatment
Place patient on cold environment.
Topical emollient.
Erythema ab igne
Erythema ab igne is a persistent erythema or the coarsely reticulated residual
pigmentation resulting from that is usually produced by long exposure to excessive heat
without the production of a burn.
Erythema ab igne occurs on the legs as a result of habitually warming them in front of open
fireplaces, space heaters, or car heaters. Similar changes may be produced at sites of an
electric heating pad application such as the low back, or the upper thighs with laptop
computers.
Epithelial atypia, which may lead to Bowen’s disease and squamous cell carcinoma, has
rarely been reported to occur overlying erythema ab igne. Treatment with 5-fluorouracil
(5-FU) or imiquimod cream may be effective in reversing this epidermal alteration.
Photosensitivity
Photosensitivity includes cutaneous reactions that are
• Chemically induced (from an exogenous source).
• Metabolic (inborn errors such as the porphyrias, resulting in the production of
endogenous photosensitizers)
• Light-exacerbated disorders (genetic and acquired).
• Idiopathic.
Chemical induce was discussed in previous lectures.
Most important example about idiopathic Photosensitivity is polymorphic light eruption
(PLE).
Polymorphic light eruption
4
Is the most common form of photosensitivity. History of PLE can be elicited in
between 5% and 20% of the adult population.
All races and skin types can be affected. The
onset is typically in the first three decades of life, and females outnumber male by 2 or 3 to
1. The pathogenesis is unknown, but a family history may be elicited in between 10% and
50% of patients.
Clinically, the eruption may have several different morphologies, although in the
individual patient the morphology is usually constant.
• Papular (erythematopapular) variant is the most common.
• Papulovesecular.
• Eczematous.
• Erythematous .
• Plaque like lesions also occur. Plaque like lesions are more common in elderly
patients and may closely simulate discoid lupus erythematosus
• Prurirus only without an eruption may be reported later in life.
The lesions of PLE appear most typically 1 to 4 days after exposure to sunlight. Patients
may report itching and erythema during sun exposure, and development of lesions within
the first 24 hours. A change in the amount of sun radiation exposure appears to be more
critical than the absolute amount of radiation. Areas of involvement include the face, the V
area of the chest, the neck, and the arms. In general, for each individual certain areas are
predisposed. However, typically areas protected during the winter, such as the extensor
forearms, are particularly affected, whereas areas exposed all year (face and dorsa of hands)
may be relatively spared. The eruption appears most commonly in the springtime. Often the
eruption improves with continued sun exposure so that patients may be clear of the
condition in the summer or autumn.
PLE is induced by ultraviolet light, but the wavelengths responsible are variable UVA or
UVB. Visible light does not induce PLE.
Two, unusual variants of PLE are (both caused by UVA).
Juvenile spring eruption and solar purpura.
Juvenile spring eruption occurs most commonly in boys age 5 to 12 years. It
presents in the spring with grouped small papules or papulovesicles on the helices. It is self-
limited and does not scar.
Solar purpura is a rare variant of PLE, presenting as macular or palpable purpura on
the legs.
Treatment:
Most patients with mild disease can be managed by avoiding the sun and using
sunscreens. These measures are critical for all patients. Topical steroid in several day to
weekly pulses is successful in controlling the pruritus and clearing the eruption.
Antihistamines may be used for pruritus. Systemic corticosteroids may be
necessary, especially in the springtime. In patients whose condition is not controlled by the
measures just mentioned, antimalarial (hydroxychloroquine sulfate 200 to 400 mg daily,

5
may be used. It has a delayed onset and is best instituted in the late winter to prevent
springtime outbreaks .PUVA therapy are extremely beneficial .Thalidomide is an
alternative in patients failing the above regimens. For patients with the most severe disease,
azathioprine is often effective.
The porphyrias
There are at least seven enzymes in the metabolic pathway that leads to the synthesis
of haem. There are also seven different types of porphyria, each being caused by adeficiency
of one of these enzymes, and each having its own characteristic pattern of accumulation of
porphyrin and porphyrin precursors. The most important one is Cutaneous hepatic porphyria
(porphyria cutanea tarda) which are two types: a sporadic type (accounting for 80% of
cases) and a type inherited as an autosomal dominant trait (20%).
patient presented with blisters, erosions form on the exposed parts of the face, and on
the backs of the hands in response to sunlight or to minor trauma. These areas become
scarred and hairy. The urine is pink and fluoresces a bright coral-pink under Wood’s light as
a result of excessive uroporphyrins, the same thing occur in the teeth . Treatment is based on
avoiding alcohol and oestrogens, but other including regular venesection or very low-dose
hydroxychloroquine therapy (e.g. 100 mg twice weekly) under specialist supervision.
Cold injury
Local cold injury are divided to chiliblain and frostbite. The mechanism of this condition as
followed:
Intense vasoconstriction resulting from the local action of cold.
Reflex vasoconstriction stimulation is reinforced by the passage of cold blood
through the vasomotor center.
Chilblains (Pernio)
Chilblains is a recurrent, localized erythema and swelling caused by exposure to cold.
Blistering and ulcerations may develop in severe cases. In people predisposed by poor
peripheral circulation, even moderate exposure to cold may produce chilblains. Acute
chilblains is the mildest form of cold injury. This occurs chiefly on the hands, feet, ears, and
face, especially in children. Patients are usually unaware of the injury at first, but later
burning, itching, and redness call it to their attention. The areas are bluish red. the color
partially or totally disappearing on pressure, and are cool to the touch . .
Chronic chilblains occurs repeatedly during cold weather and disappears during warm
weather. The affected extremities are cold, cyanotic , hyperhidrotic.
Treatment
General measures
The parts should be cleansed with water and massaged gently with warm oil each day and
should be protected against further injury and exposure to cold or dampness. If the feet are

6
affected, woolen socks should be worn at night during the cold months. Smoking is strongly
discouraged.
Medical measures
Topical and systemic steroid with systemic antihistamine
nifedipine. 20 mg three times daily, has been shown to be effective.
Vasodilators such as nicotinamide, 100 mg three times a day. or dipyridamole, 25 mg three
times a day, are used to improve circulation.
Frostbite (congelation)
When soft tissue is frozen and locally deprived of blood supply, the damage is called
frostbite.The ear , nose, cheeks, fingers, and toes are most often involved. The frozen part
painlessly become pale and waxy. The is various degrees of tissue destruction similar to
those caused by burns are encountered. These are erythema and edema, vesicles and bullae,
superficial gangrene . deep gangrene, and injury to muscles, tendons, periosteum, and
nerves .
Treatment.
Early treatment of frostbite before swelling develops should consist of covering the
part with clothing or with a warm hand to maintain a slightly warm temperirure so that
adequate blood circulation can be maintained. Rapid rewarming in a worm water bath is the
treatment of choice for all forms of frostbite.
Analgesics, unless contraindicated, should be given.
Bed rest elevation of limb.
Antibiotics with anticoagulant to prevent thrombosis and gangrene.
Full recovery may take several months.
