Preterm labor dr. alaa Hussein ali al- naser
Preterm birth (PTB) refers to a birth that occurs before 37 weeks of gestation. Sub classifications of PTB are variably and inconsistently defined as:Late preterm = 34 to 36 and 0/7ths weeks
Moderately preterm = 32 to 34 weeks
Very preterm = <32 weeks
Extremely preterm = <28 weeks
PTB can also be defined by birth weight (BW):
Low birth weight (LBW) — BW less than 2500
Very low birth weight (VLBW) — BW less than 1500 gExtremely low birth weight (ELBW) — BW less than 1000 g
By comparison, a term birth is defined as a birth occurring between 37 and 0/7ths and 42 weeks, and a post-term birth is defined as a birth occurring after 42 weeks.
SIGNIFICANCE
Taken together with its sequelae, PTB is by far the leading cause of infant mortality.PTB is also a major determinant of short- and long-term morbidity in infants and children.
INCIDENCE
8-12% and increased in developed country due increase assisted reproductive technique and multiple pregnancy.
PATHOGENESIS
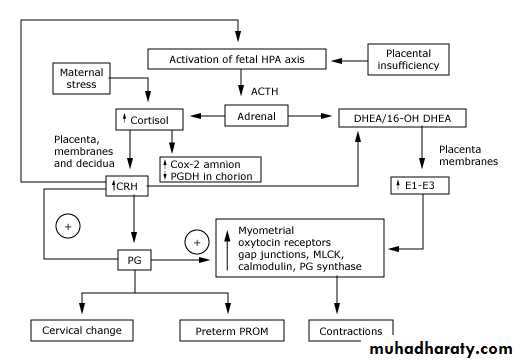
Approximately 70 to 80 percent of PTBs occur spontaneously: preterm labor (PTL) accounts for 40 to 50 percent of all PTBs and preterm premature rupture of membranes (PPROM) accounts for 20 to 30 percent. The remaining 20 to 30 percent of PTBs are due to intervention for maternal or fetal problems.Activation of the maternal or fetal hypothalamic-pituitary-adrenal axis
Infection
. Major maternal physical or psychological stressors, including depression.
Premature fetal HPA activation can result from the stress of uteroplacental vasculopathy. a four- to seven-fold increased risk of placental pathological evidence of vascular damage, bleeding, fetal vascular disruption, or lack of normal physiologic conversion of maternal spiral arteries , severe preeclampsia was associated with a threefold increase in the risk of spontaneous PTB
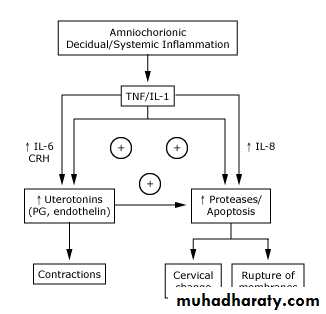
Infection
Inflammation a link between spontaneous PTB and the presence of both systemic and genitourinary tract pathogens.asymptomatic bacteriuria, which was independently associated with PTB
abnormal vaginal flora , lactobacilli and the presence of bacterial vaginosis (BV) were both associated with a two-fold increase in risk of PTB, while gram positive coccus-associated aerobic vaginitis was associated with a three-fold increase in risk of PTB.
Similarly, periodontal disease is associated with higher rates of PTB.
both clinical and subclinical chorioamnionitis are much more common in preterm than term deliveries, and may account for 50 percent of PTB before 30 weeks of gestation.
disorders of maternal innate or acquired immunity, rather than the presence of certain genital tract bacteria, are the primary causes of inflammation-associated PTB.
There is a significant racial disparity in inflammation-associated PTB, with African-Americans disproportionately affected.
Some organisms (eg, Pseudomonas, Staphylococcus, Streptococcus, Bacteroides, and Enterobacter) are capable of producing proteases, collagenases, and elastases that can degrade the fetal membranes. Bacteria also produce phospholipase A2 (which leads to prostaglandin synthesis) and endotoxin, substances that stimulate uterine contractions
Proinflammatory mediators unrelated to infection — Noninfectious etiologies, such as placental hypoperfusion, also appear to increase production of proinflammatory mediators. This may be another mechanism accounting for the slightly higher rate of spontaneous PTB among growth restricted infants.
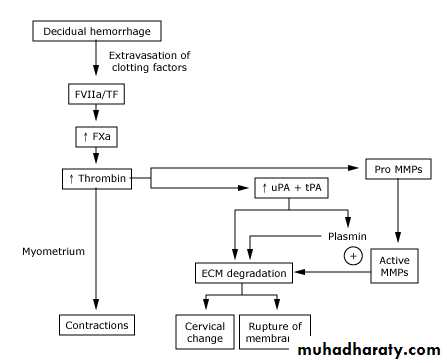
Decidual hemorrhage
Vaginal bleeding from decidual hemorrhage is associated with a high risk of PTL and PPROM, occult decidual hemorrhage (manifested by hemosiderin deposition and retro-chorionic hematoma formation)PTB is strongly linked to histological evidence of maternal spiral artery hemorrhage and damage and maternal genotypes, polymorphisms predisposing to decidual vasculopathy, thrombosis, and abruption also predispose to PTB. This finding helps account for the predominance of abruption-associated PTB in European populations.
Pathologic uterine distention
Multiple gestation, polyhydramnios, and other causes of excessive uterine distention are well described risk factors for PTB. Enhanced stretching of the myometrium induces the formation of gap junctions, upregulation of oxytocin receptors, and production of prostaglandin E2 and F2 and myosin light chain kinase, which are critical events preceding uterine contractions and cervical dilation.Distention of the fetal compartment also contributes to myometrial activation. Cytokines, prostaglandins, and collagenase are produced from excess stretch of the fetal membranes.
Pathologic cervical change
Cervical insufficiency refers to pathological dilatation and/or effacement of the uterine cervix unrelated to labor and leading to previable pregnancy loss. It may occur with or without coexisting distention of the corpus.Cervical insufficiency due to intrinsic cervical factors is probably a rare event. It is more likely that progressive cervical shortening prior to viability results from activation of the inflammatory of hemorrhagic pathways at a point in gestation when both myometrial quiescence, as well as amniotic fluid, fetal membrane, and decidual antiprotease activity are maximal. Thus, cervical change occurs without apparent antecedent PTL and PPROM.
Genetic factor link with cervical insufficiency.
loop electrosurgical excision procedure (LEEP), the risk of PTB was increased two-fold and the risk was even higher following repeated procedures or larger biopsies.
Risk factors for preterm birth
1. StressSingle women
Low socioeconomic status
Anxiety
Depression
Life events (divorce, separation, death))
Abdominal surgery during pregnancy
Occupational fatigue 2.
Upright posture
Use of industrial machines
Physical exertion
Mental or environmental stress
Excessive or impaired uterine distention 3.
Multiple gestation
Polyhydramnios
Uterine anomaly
Uterine leiomyoma
Diethylstilbestrol
Cervical factors 4.
History of second trimester abortion
History of cervical surgery
Premature cervical dilatation or effacement
Infection 5.
Sexually transmitted infections
Pyelonephritis, appendicitis, pneumonia
Systemic infection
Bacteriuria
Periodontal disease
Placental pathology 6.
Placenta previa
Abruption
Vaginal bleeding
Miscellaneous 6.
Previous preterm delivery
Substance abuse
Smoking
Maternal age (<18 or >40)
African-American race
Poor nutrition and low body mass index
Inadequate prenatal care
Inadequate prenatal care
Anemia (hemoglobin <10 g/dL)
Excessive uterine contractility
Low level of educational achievement
Genotype
Fetal factors 7.
Congenital anomaly
Growth restriction
CLINICAL MANIFESTATIONS AND DIAGNOSIS
PTL is one of the most common reasons for hospitalization of pregnant women, but identifying women with preterm contractions who will deliver preterm is an inexact process.
Signs and symptoms of early PTL include menstrual-like cramping, constant low back ache, mild uterine contractions at infrequent and/or irregular intervals, and vaginal discharge. Mucus that has accumulated in the cervix may be discharged as clear, pink, or slightly bloody secretions (ie, mucus plug, bloody show), sometimes several days before labor begins. However, these signs and symptoms are non-specific and often noted in women whose pregnancies go to term.
Uterine contractions, the sine qua non of labor, are a normal finding at all stages of pregnancy, thereby adding to the challenge of distinguishing true from false labor. The frequency of contractions increases with gestational age, the number of fetuses, and at night. .
The diagnosis of PTL is generally based upon clinical criteria of regular painful uterine contractions accompanied by cervical dilation and/or effacement. include persistent uterine contractions (four every 20 minutes or eight every 60 minutes) with documented cervical change or cervical effacement of at least 80 percent, or cervical dilatation greater than 2 cm.
Digital cervical examination has limited reproducibility between examiners, especially when changes are not pronounced; therefore, some centers evaluate the cervix via transvaginal ultrasound to confirm the diagnosis. Sonographic measurement of cervical length is a more sensitive indicator of a patient's risk for PTB than cervical dilatation. Cervical length is predictive of PTB , including asymptomatic women with prior cone biopsy, mullerian anomalies, or multiple dilation and evacuations . A short cervix has been variously defined as a cervical length less than 2.0 cm, 2.5 cm, or 3.0 cm.
INITIAL EVALUATION — In addition to reviewing the patient's obstetrical and medical history, the initial evaluation of women with suspected PTL should determine:
1. The presence and frequency of uterine contractions.
Whether there is uterine bleeding 2.
3.Whether the fetal membranes have ruptured
Gestational age 4.
Fetal well-being 5.
Uterine contractions and fetal well-being are evaluated continuously using an electronic fetal heart rate and contraction monitor.
Physical examination — The uterus is examined to assess firmness, tenderness, fetal size, and fetal position. A sterile speculum examination is performed to rule out ruptured membranes, to visually examine the vagina and cervix, and to obtain specimens for laboratory testing . A digital examination to assess cervical dilatation and effacement is performed after placenta previa and PPROM have been excluded (by history and physical, laboratory, and ultrasound examinations, as indicated)
Laboratory tests
1.Urine culture, since bacteriuria and pyelonephritis are associated with PTB.
2.Rectovaginal group B streptococcal culture, to determine need for antibiotic prophylaxis
3.Tests for gonorrhea and chlamydia. Testing for gonorrhea and chlamydia may be omitted if previously performed, the results were negative, and the patient is not at high risk of acquiring sexually transmitted infections.
4.Fetal fibronectin (fFN). We obtain a swab for fFN on all symptomatic patients considered at high risk for PTB, and then perform transvaginal sonographic measurement of cervical length. We only send the swab to the laboratory for FFN determination if the cervical length is 20 to 30 mm
5.Given the link between cocaine use and placental abruption, we perform drug testing in patients with risk factors for drug abuse.
Imaging
we perform an ultrasound examination to measure cervical length.During this examination, we also confirm the fetal presentation and estimate fetal weight to counsel about mode of delivery and anticipated neonatal outcome.
Cervical length >30 mm — These women are at low risk of PTB, regardless of fFN result, so we do not send their swabs for fFN testing to the laboratory. We discharge the patients home after an observational period of four to six hours during which we confirm fetal well-being (eg, reactive nonstress test), exclude the presence of an acute precipitating event (eg, an abruption or overt infection), and assure ourselves that the cervix is not dilating or effacing.
Follow-up in one to two weeks is arranged and the patient is given instructions to call if she experiences additional signs or symptoms of PTL, or has other pregnancy concerns (eg, bleeding, PROM, decreased fetal activity).
Cervical length 20 to 30 mm — PTB is more likely in women with cervices 20 to 30 mm than in women with longer cervices, but most women in this group do not deliver preterm. Therefore, we send the swab for fFN testing in this subgroup of women. If the test is positive (level greater than 50 ng/mL), we actively manage the pregnancy to prevent morbidity associated with PTB.
Cervical length <20 mm — These women are at high risk of PTB regardless of fFN result. Therefore, we do not send their swabs for fFN testing to the laboratory and actively manage them to prevent morbidity associated with PTB.
MANAGEMENT OF WOMEN WITH PRETERM LABOR
We hospitalize women diagnosed with PTL at less than 34 weeks of gestation and initiate the following treatments:Antenatal glucocorticoids to reduce neonatal morbidity and mortality associated with PTB.
Appropriate antibiotics for GBS chemoprophylaxis
Tocolytic drugs for up to 48 hours to delay delivery so that glucocorticoids given to the mother can achieve their maximum effect.
Appropriate antibiotics to women with positive urine culture results or positive tests for gonorrhea or chlamydia
MANAGEMENT OF ASYMPTOMATIC WOMEN AT HIGH RISK OF PTB
Women with risk factors for PTB are sometimes followed with serial ultrasound measurement of cervical length. A cervical length ≥35 mm is generally considered normal and reassuring; as cervical length decreases below 35 mm, the risk of PTB increases.We manage asymptomatic patients at high risk of PTB similar to the way we manage symptomatic patients, but with a higher cervical length threshold for intervention. This minimizes overtreatment of high risk asymptomatic patients and undertreatment of symptomatic patients. Surveillance with serial cervical length measurements is begun at 22 weeks.
Cervical length ≥35 mm - The risk of PTB is low. We see these patients in routine follow-up in one to two weeks.
Cervical length 25 to 34 mm - We obtain a fFN concentration. If the test is positive (level greater than 50 ng/mL), we actively manage the pregnancy to prevent morbidity associated with PTB, we consider administering a course of glucocorticoids, we suggest that the patient stop physically demanding work, and we give appropriate antibiotics to women with positive urine culture results or positive tests for gonorrhea, chlamydia, or bacterial vaginosis. Early aggressive treatment of bacterial vaginosis in high risk patients may reduce PTB/PPROM . '
Cervical length <25 mm - The risk of PTB is increased. We actively manage the pregnancy to prevent morbidity associated with PTB..
Delay delivery by at least 48 hours so that glucocorticoids given to the mother can achieve their maximum effect. Predelivery administration of glucocorticoids reduces the risk of neonatal death, respiratory distress syndrome, intraventricular hemorrhage, and necrotizing enterocolitis in premature neonates. (See "Antenatal use of corticosteroids in women at risk for preterm delivery".)
Provide time for safe transport of the mother, if indicated, to a facility that can provide an appropriate level of neonatal care if the patient delivers preterm.
There is greater consensus regarding the upper gestational age limit. Thirty-four weeks of gestation typically defines the threshold at which perinatal morbidity and mortality are felt to be too low to justify the potential maternal and fetal complications and costs associated with the inhibition of labor. One decision analysis of PTL strategies by gestational age concluded that: at ≤32 weeks tocolysis was preferable to no tocolysis or decisions based on fetal lung maturity assessment, at ≥36 weeks no tocolysis was the preferred approach, but neither strategy was clearly preferable at 34 weeks. They also recommended not performing amniocentesis for determination of fetal lung maturity.
Contraindications
Tocolysis is contraindicated when the maternal/fetal risks of prolonging pregnancy or the risks associated with these drugs are greater than the risks associated with PTB. Contraindications to labor inhibition include:
Intrauterine fetal demise
Lethal fetal anomaly
Nonreassuring fetal status
Severe fetal growth restriction.
Severe preeclampsia or eclampsia
Maternal hemorrhage with hemodynamic instability
Chorioamnionitis
Known or suspected fetal pulmonary maturity is not an absolute contraindication to tocolysis as there are nonpulmonary morbidities associated with PTB. As an example, a 30-week fetus with a mature amniotic fluid test is still at risk for intraventricular hemorrhage, sepsis, hyperbilirubinemia, and other morbidities unrelated to respiratory distress syndrome. These fetuses could potentially benefit from prolongation of pregnancy and the nonpulmonary benefits of glucocorticoid therapy.
Inhibition of PTL is less likely to be successful when cervical dilation is greater than 3 cm. Tocolysis can still be considered in these cases, especially when the goal is to administer antenatal glucocorticoids or safely transport the mother to a tertiary care center.
BEDREST, HYDRATION, AND SEDATION — There is no high quality evidence of the efficacy of bedrest for prevention or treatment of PTL in singleton pregnancy.
tocolytics
BETA-ADRENERGIC RECEPTOR AGONISTS —
MAGNESIUM SULFATE
CALCIUM CHANNEL BLOCKERS
CYCLOOXYGENASE INHIBITOR
OXYTOCIN RECEPTOR ANTAGONISTS
NITRIC OXIDE DONORS
PROGESTERONE SUPPLEMENTATION
.