Vulval lesions
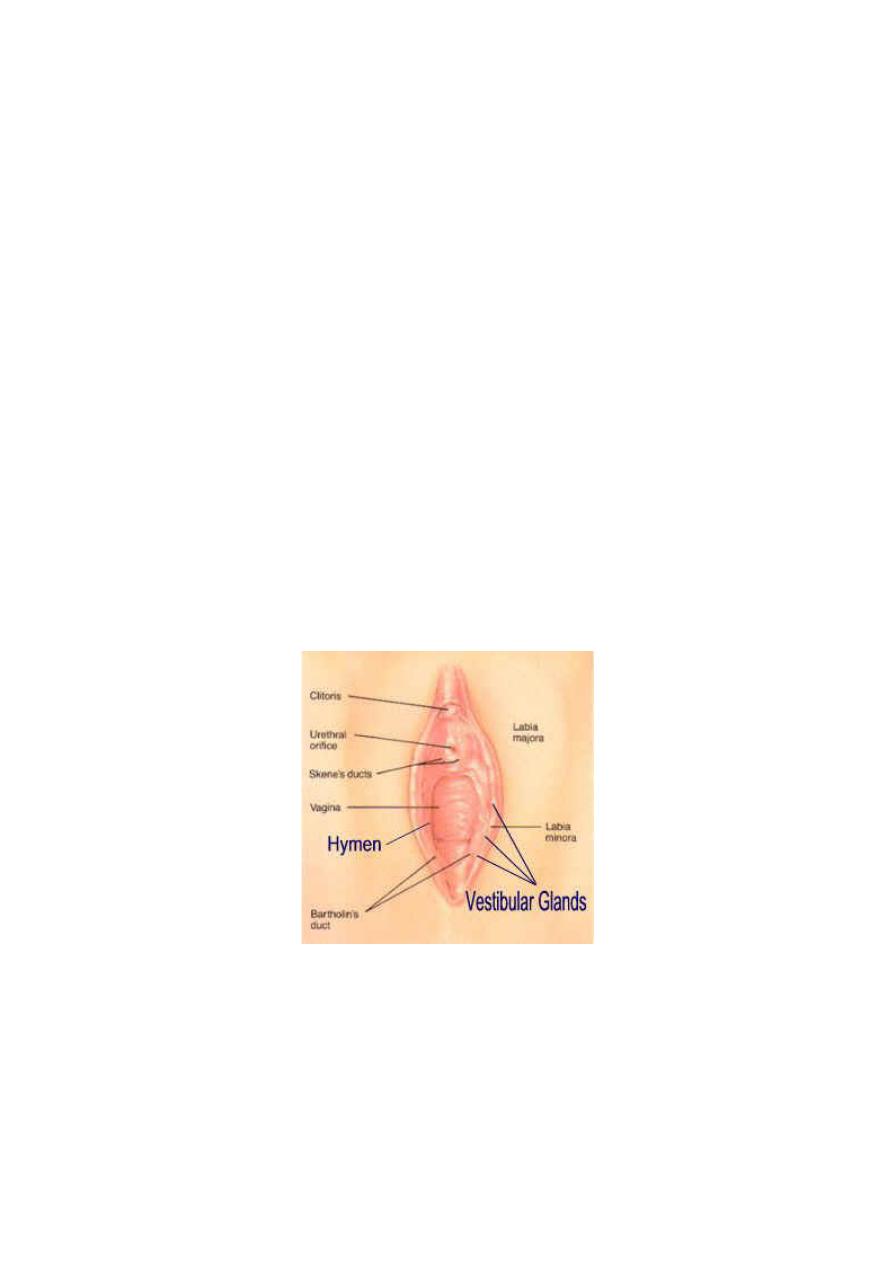
The vulva is the term used to describe the external female genitalia – the
sexual organs. It includes the labia majora and minor, clitoris and
fourchette. The vulval vestibule is defined anatomically as the area
between the lower end of the vaginal canal at the hymenal ring and the
labia minora. The different anatomical areas of the external genitalia have
different histological characteristics and embryological origins. Both the
labia minora and majora are covered with keratinized, pigmented,
squamous epithelium. The labia majora are two large folds of adipose
tissue covered by skin containing hair follicles, sebaceous and sweat
glands. In contrast, the labia minora are devoid of adipose tissue and hair
follicles, but contain sebaceous follicles. The normal vulval vestibule is
covered with non-keratinized, non-pigmented squamous epithelium and is
devoid of skin adnexa. Within the vulval vestibule are the ducts of the
minor vestibular glands, the periurethral glands of Skene, the urethral
meatus and the ducts of the Bartholin’s glands.
The vagina and vulva are commonly known as the lower genital tract
with the vagina leading to the upper genital tract (uterus, cervix, tubes
and ovaries).
Assessment
A full history and clinical examination (with optional vaginal swabs and
biopsies) are essential to make the diagnosis, history to ask about general
skin problems as this might point towards the diagnosis, for example
psoriasis or eczema, current methods of skin care, topical treatments,
The clinical examination should include all hair skin surfaces ,texture,
colour, and the vulval area should be examined systematically with a
good light source.
Sometimes it is necessary to carry out some swabs and a biopsy for
confirmation. Microbiological swabs may be indicated to exclude
infection, Biopsies should be carried out when there is a pigmented
lesion, a raised or indurated area and a persistent ulcer.

an itchy vulva (pruritus vulvae)?
An itchy vulva is a symptom, not a condition in itself. It can be caused by
many different conditions.
•
Infections. For example: thrush, threadworms, scabies, and some
sexually transmitted infections.
•
Skin conditions may affect vulval skin. For example: eczema,
psoriasis, lichen simplex, lichen planus and lichen sclerosus.
•
Sensitisation of the vulval skin to soaps, perfumes, deodorants,
excessive sweat, condoms, wet wipes, textile dyes, detergents,
fabric conditioners, sanitary wear, etc.
•
Urinary or faecal incontinence.
•
Menopause.
•
Pregnancy can cause itch due to vulval engorgement.
•
Breast-feeding can cause itch due to low oestrogen levels.
•
Any cause of a generalised body itch may also cause itching of
the vulva. For example, a generalised body itch may be a side-
effect of some medicines or due to some blood disorders, thyroid
problems or kidney or liver disease.
•
Diabetes
•
A cancer
•
Unknown causes.
•
It is therefore prudent to reduce
allergens
in all patients presenting
with symptoms of vulval pruritis. It is advisable to discourage women
from washing with any soaps or detergents (including feminine
washes), which disrupt the bacterial balance of the vagina and can
cause a vulval dermatitis. Water is preferable but some women find
olive (or other natural unperfumed) oils offer moisturization Women
should be encouraged to wear cotton underwear (with minimal dyes)
and wash clothing with an unperfumed non-biological washing
powder/fabric conditioner.
The vulval and vaginal condition of
candidal infection
or ‘thrush’ is
common and particularly affects women of reproductive age (or using
hormone replacement therapy, HRT) where oestrogen levels are high
(and there is an increased prevalence in pregnancy).
It is very important to consider diabetes as a cause of recurrent thrush.
Once excluded, a genuine case of candidal infection should be treated
with a course of 150 mg clotrimazole nightly over 3 consecutive nights.
In women with recurrent symptoms, it is important to exclude diabetes and assess for
underlying risk factors (e.g. immunodeficiency, corticosteroid use and frequent antibiotic use
.tratment include suppressive fluconazole prophylaxis (150 mg once a week six months), has
become the standard of care and will effectively prevent symptomatic episodes .
Benign conditions:
Lichen sclerosis
Lichen sclerosis is an autoimmune destructive inflammatory skin
condition which affects mainly the anogenital area of women.
The main symptoms on the vulva is itching and subsequent soreness of
the vulva, usually due to scratching. Splitting of the skin is common and
frequently occurs at the posterior fourchette which can lead to superficial
dyspareunia.
On examination of the skin, whitening, fissuring and loss of anatomy are
common , in long-standing cases treatment is a combination of good skin
care and strong steroid ointments, such as Dermovate., it is a
premalignant condition and incidence of malignancy aboute 3-5 %.
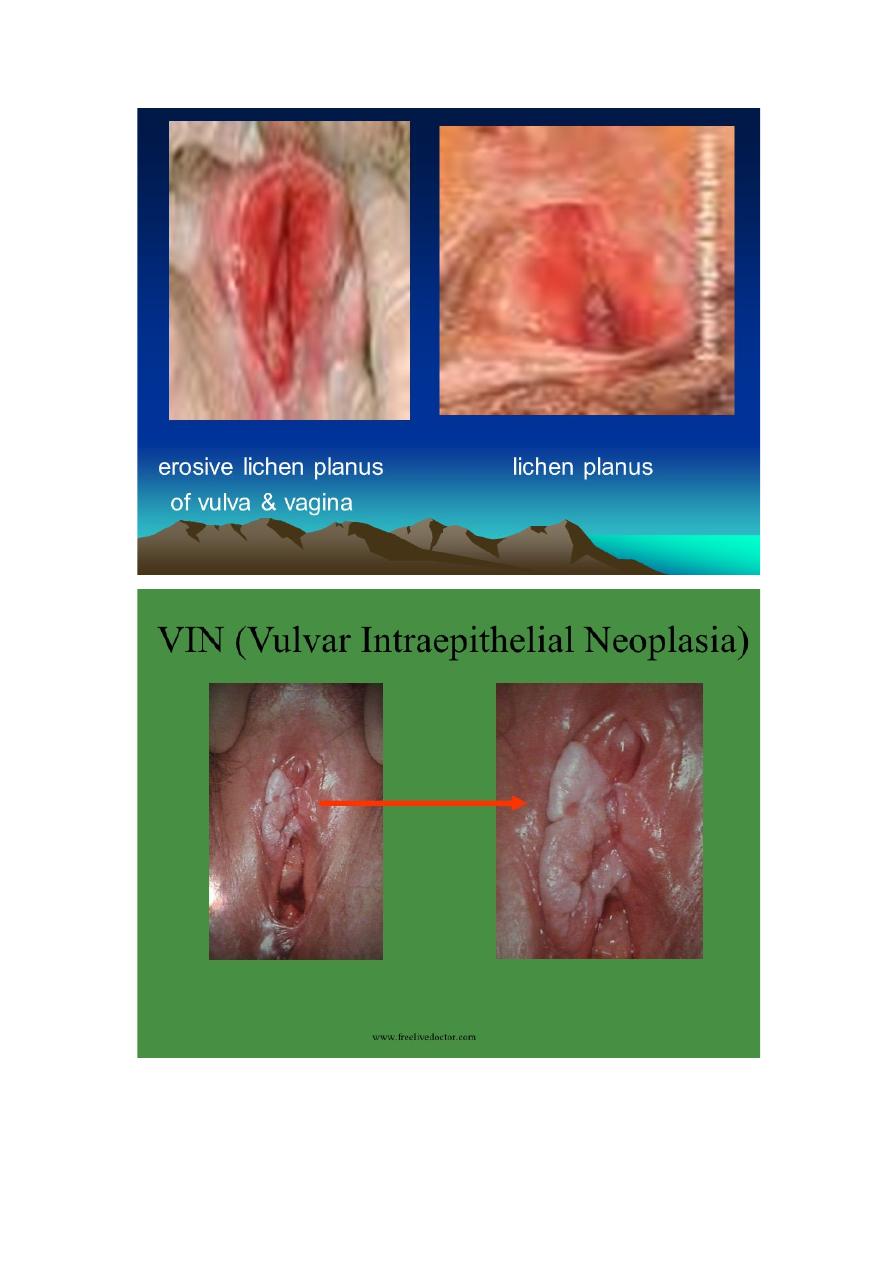
Vulval lichen planus
Lichen planus is an inflammatory disorder which can affect both the skin
and mucosal surfaces. The characteristic cutaneous lesions are small
purplish papules. These can also be seen on mucosal lesions. The papules
commonly occur on flexor surfaces and can koebnerize at sites of trauma.
There is often pigmentary incontinence, which is responsible for the
marked hyperpigmentation sometimes seen clinically
Management
The major treatment used is a super - potent topical steroid ointment
clobetasol propionate 0.05% is used daily for the first month and then
reduced to be used as needed.
Behcet ’ s s yndrome
The diagnosis is made when a patient has recurrent oral ulceration with at
least two of the following – recurrent genital ulceration, eye lesions,
cutaneous lesions and a positive pathergy test (where postulation occurs
at the site of minor skin trauma, such as venepuncture).
The treatment is with several drugs , including steroids, colchicines,
dapsone and thalidomide. Topical steroids may be used for the genital
ulcers.
Genital herpes simplex
Two serotypes
(types 1 and 2) are responsible for both oral and genital ulceration
The clinical presentation is variable with either a primary or secondary
infection. The typical history of herpetic illness is irritation or
paraesthesia at the site of the lesion before the appearance of painful
papules. These form vesicles that erode to give superficial erosions that
either heal or form ulcers.
In the acute phase, antiviral agents (acyclovir 200 mg orally five times
per day for 5 days) will reduce the length of viral shedding and shorten
the healing time in the primary attack. In recurrent herpes, suppression
therapy should be considered with long term acyclovir.
Benign cysts of the vulva
A Bartholin’s cyst is the most common type of cyst and develops in the
region of the Bartholin’s gland .
It is not uncommon for these cysts to get infected and cause a Bartholin’s
abscess which usually presents acutely and may require incision and
drainage. Marsupialization of the cyst is the term used when the internal
aspect of the cyst is sutured to the outside of the cyst to create a window
so that the cyst does not reform
Other Cystic lesions include: Congenital mucous cysts Skene’s duct
cyst Cyst of the canal of Nuck Sebaceous cysts hidradenoma.
Other lumps can be seen in the vulva are, Fibroma Dermatofibroma
Lipoma Condylomata, hernias, varicosities.,
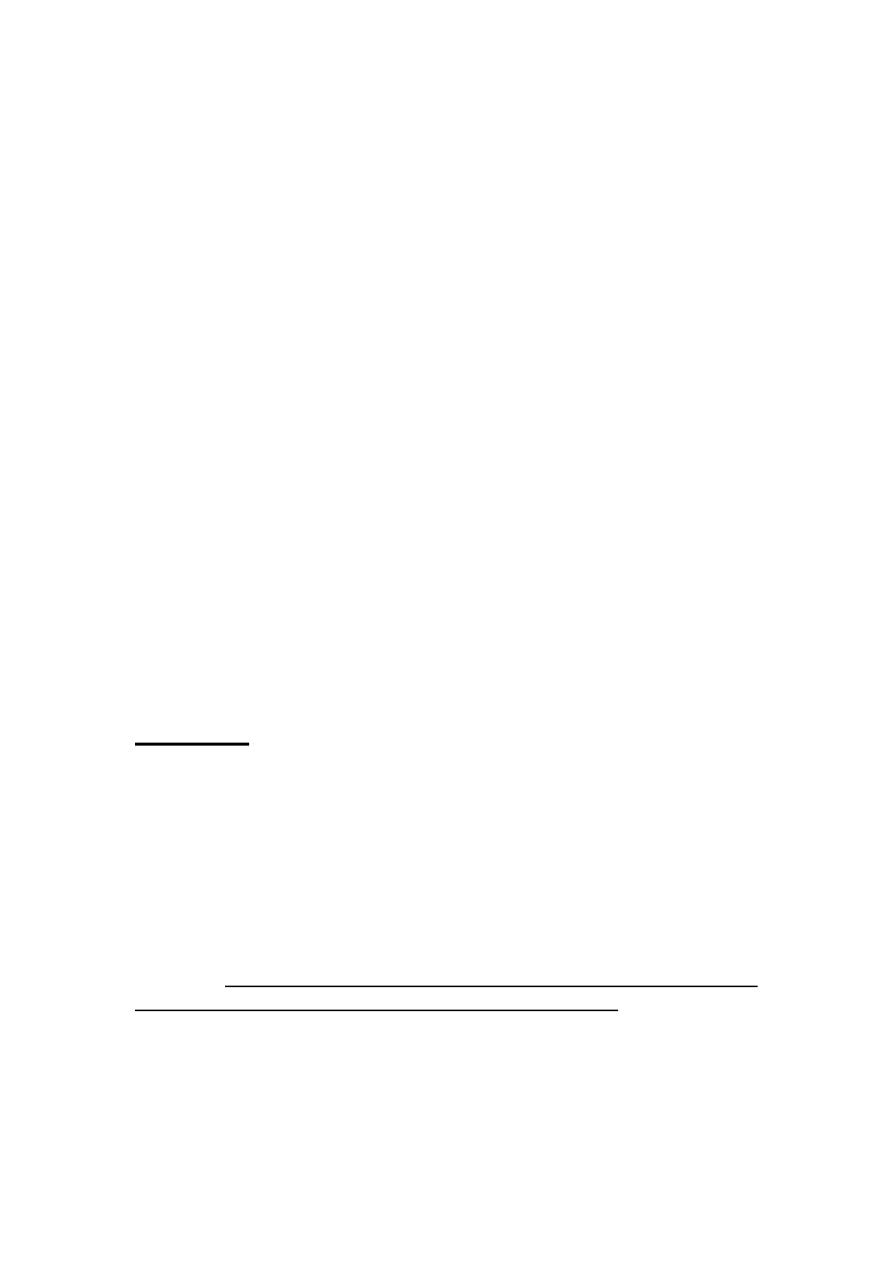
Vulval intraepithelial neoplasia
It is a premalignant condition, VIN can be either associated with human
papilloma viruses (HPV16 and 33
)
or with lichen sclerosis. Vulval intraepithelial
neoplasia affects mainly the labia minora and the perineum.
The lesions may extend to the perianal and anal mucosa. affected
women may complain of itching, soreness and burning, but many are asymptomatic. On
clinical examination, patients may have a variety of findings from
indurated, pigmented lesions to eroded red areas on the labia. Diagnosis is
made by examining the vulva with a good light source, such as the colposcope at low
magnification, and by taking representative biopsies. Like CIN, VIN is graded 1–3 in increasing
severity of abnormal cell maturation and stratification.
Current treatments for VIN :
Low-grade VIN should be observed. VIN3 lesions can be treated by local excision or laser
vaporization.
A topical immunomodulator called ‘imiquimod’ may be beneficial in treatment.

Lichen scleroses