Lec 2 :
Infections of the pharynx:
Acute Viral Pharyngitis
Etiology, symptoms: Acute viral pharyngitis, which
is often caused by influenza or parainfluenza
viruses, typically presents clinically with sudden
onset of fever, sore throat, and headache. There
may also be coughing and catarrhal symptoms (e.g.,
rhinitis, sinusitis).
Concomitant cervical adenopathy may also be
present.
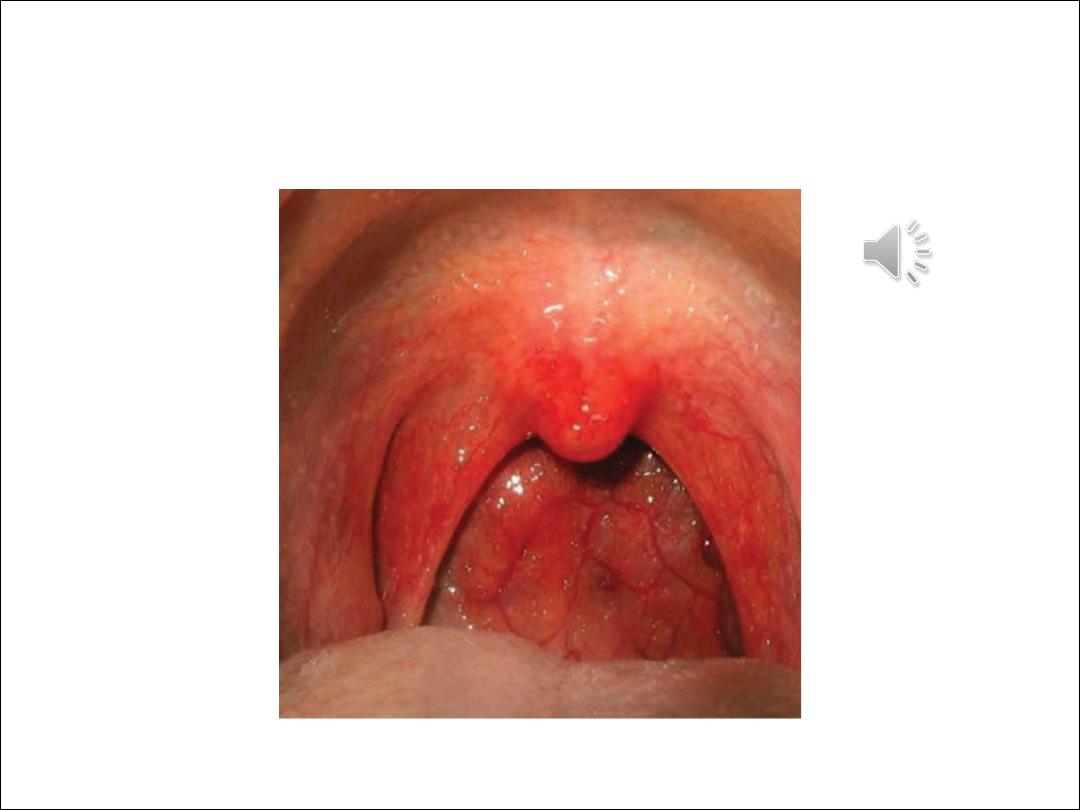
Diagnosis: The pharyngeal mucosa appears red and coated on
mirror examination. If a bacterial etiology is suspected, a rapid
streptococcal test can be performed
Treatment is supportive and consists mainly of analgesic agents.
Cold compresses to the neck can also help to relieve pain. The
patient should drink copious amounts of warm liquid to ease
complaints
Chronic Pharyngitis
Etiology: Chronic pharyngitis is often a result of long term
exposure to various noxious agents (nicotine, alcohol, chemicals,
gaseous irritants). It can also occur as a result of chronic mouth
breathing due to nasal airway obstruction (e.g., deviated
septum) or as an accompanying feature of chronic sinusitis.
Symptoms: The main clinical manifestations are a dry throat
sensation with frequent throat clearing and the drainage of a
viscous mucus. Some patients have a dry cough and a foreign-
body sensation in the pharynx.

Diagnosis: The history will often direct attention to possible
noxious agents. On mirror examination, the pharyngeal mucosa
appears red and “grainy” due to the hyperplasia of lymphatic
tissue on the posterior pharyngeal wall (hypertrophic form: The
pharyngeal mucosa may also have a smooth, shiny appearance
in some cases (atrophic form). A thorough nasal examination
should be performed to exclude nasal airway obstruction as the
cause of chronic pharyngitis, giving particular attention to
possible septal deviation or turbinate hyperplasia.
The middle meatus should also be examined endoscopically
Treatment: Any agents causing the pharyngitis should be
avoided. Also, an herbal product such as sage or chamomile can
be used in a steam inhalation to moisten the airways. In patients
with nasal airway obstruction due to septal deviation or
turbinate hyperplasia, a
surgical procedure can be performed to improve complaints

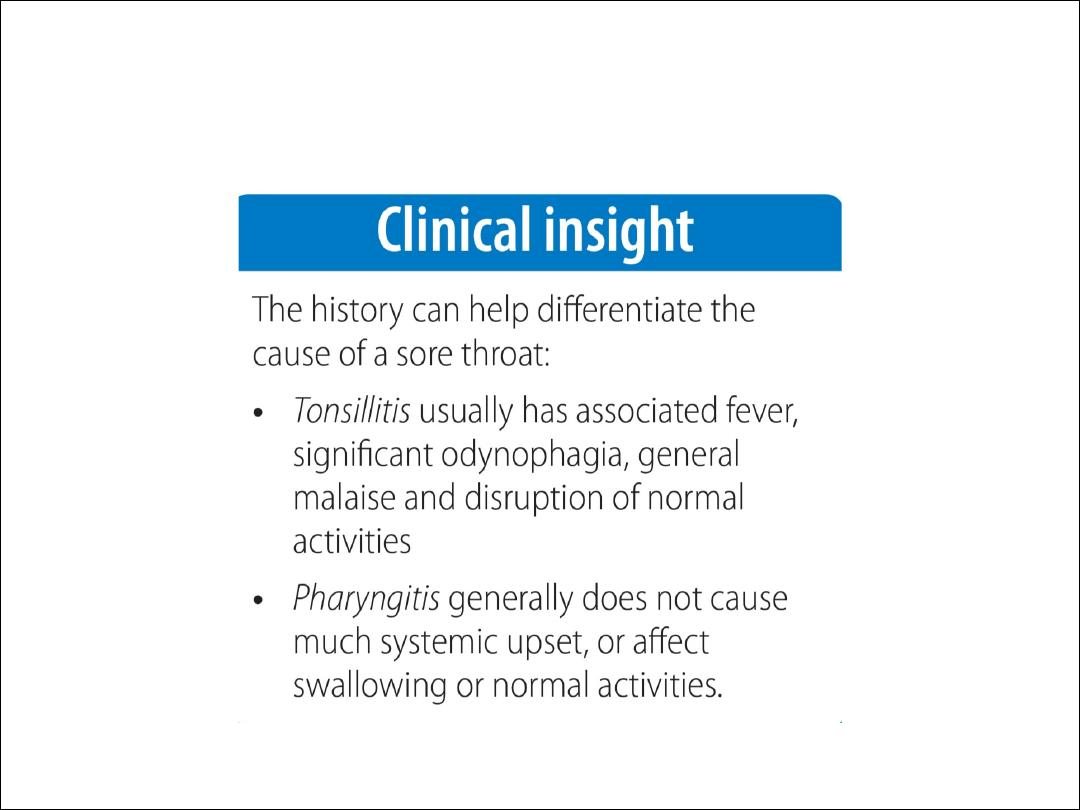
Tonsillitis
Tonsillitis, or infection of the tonsils is commonly seen
in ENT and in general practice. Common bacterial
pathogens are B haemolytic streptococcus,
pneumococcus and homophiles influenza. Sometimes
this occurs following an initial viral infection. Treatment
consists of appropriate antibiotics (e.g. penicillin),
regular simple analgesia, oral fluids and bed rest.
Signs of acute tonsillitis
•
Sore throat
•
Enlargement of the tonsils
•
Exudate on the tonsils
•
Difficulty in swallowing
•
Pyrexia
•
Malaise
•
Bad breath
•
Ear ache.

Complications of tonsillitis
Airway obstruction: This is very rare, but may occur in tonsillitis
due to glandular fever. The patient may experience severe
snoring and acute sleep apnoea. This may require rapid
intervention e.g. insertion of nasopharyngeal airway or
intubation.
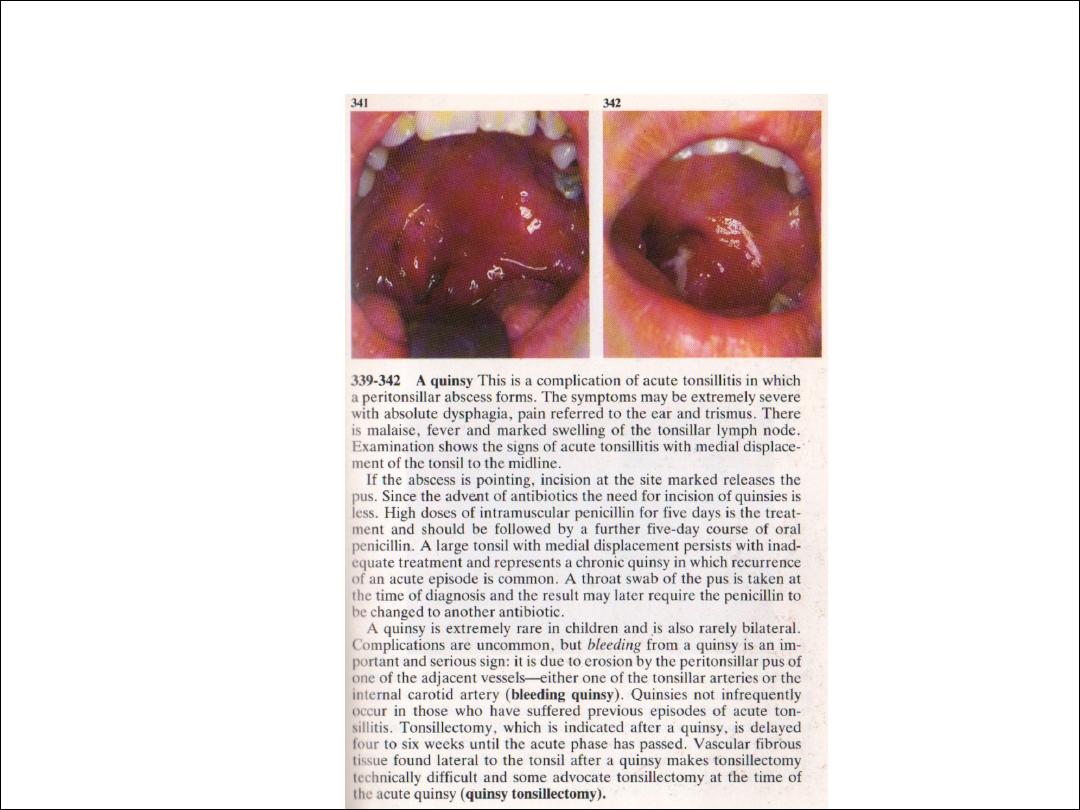
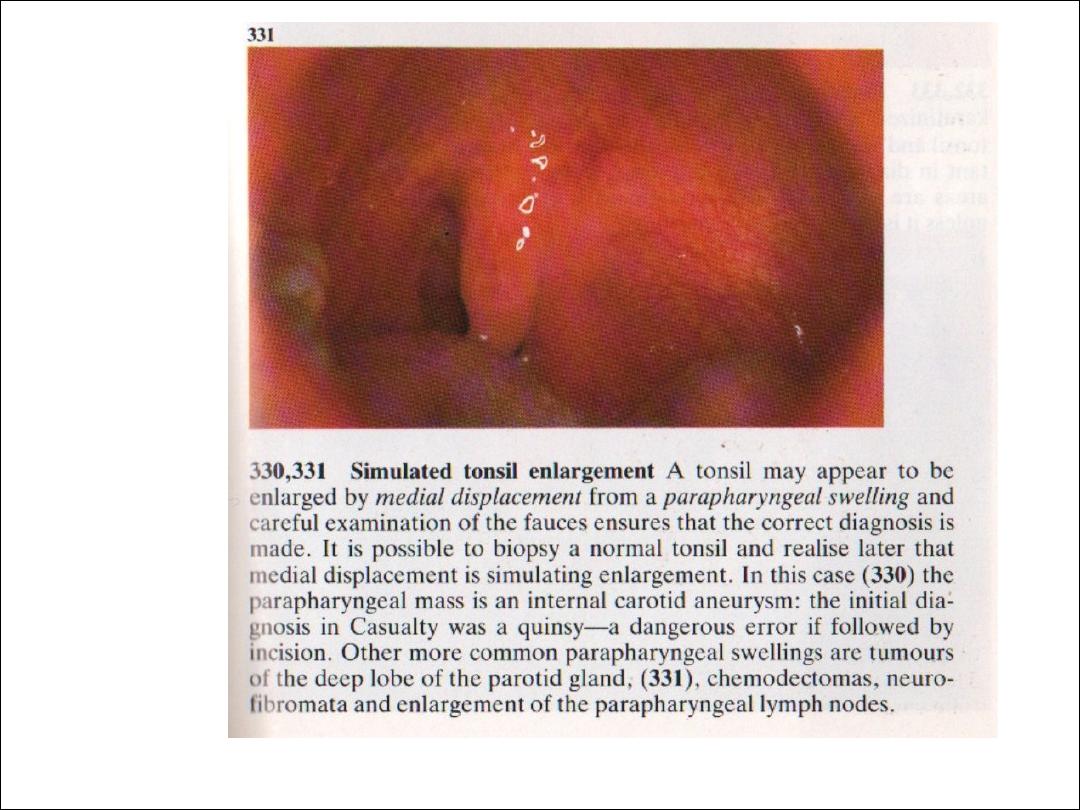
Quinsy (paratonsillar abscess): This appears as a swelling of the
soft palate and tissues lateral to the tonsil, with displacement
of the uvula towards the opposite side. The patient is usually
toxic with fetor, trismus and drooling. Needle aspiration or
incision and drainage is required, along with antibiotics which
are usually administered intravenously..
Parapharyngeal abscess: This is a serious complication of
tonsillitis and usually presents as a diffuse swelling in the neck.
Admission is required and surgical drainage is often necessary
via a neck incision. The patient will usually have an ultrasound
scan first, to confirm the site and position of the abscess.
Complications of acute Tonsillitis

Management
Patients with complicated tonsillitis, and those who
are unable to take enough fluid orally, will need to
be admitted to hospital for rehydration, analgesia,
and intravenous antibiotics. Ampicillin should be
avoided if there is any question of glandular fever,
because of the florid skin rash which will occur.
Treatment: The standard treatment for
streptococcal
tonsillitis is a 10–14-day course of penicillin V. This
regimen should be continued for at least 7 days to
avoid late complications . Macrolides or
oral cephalosporins can be used in patients allergic
to
penicillin. Analgesics are also administered for pain

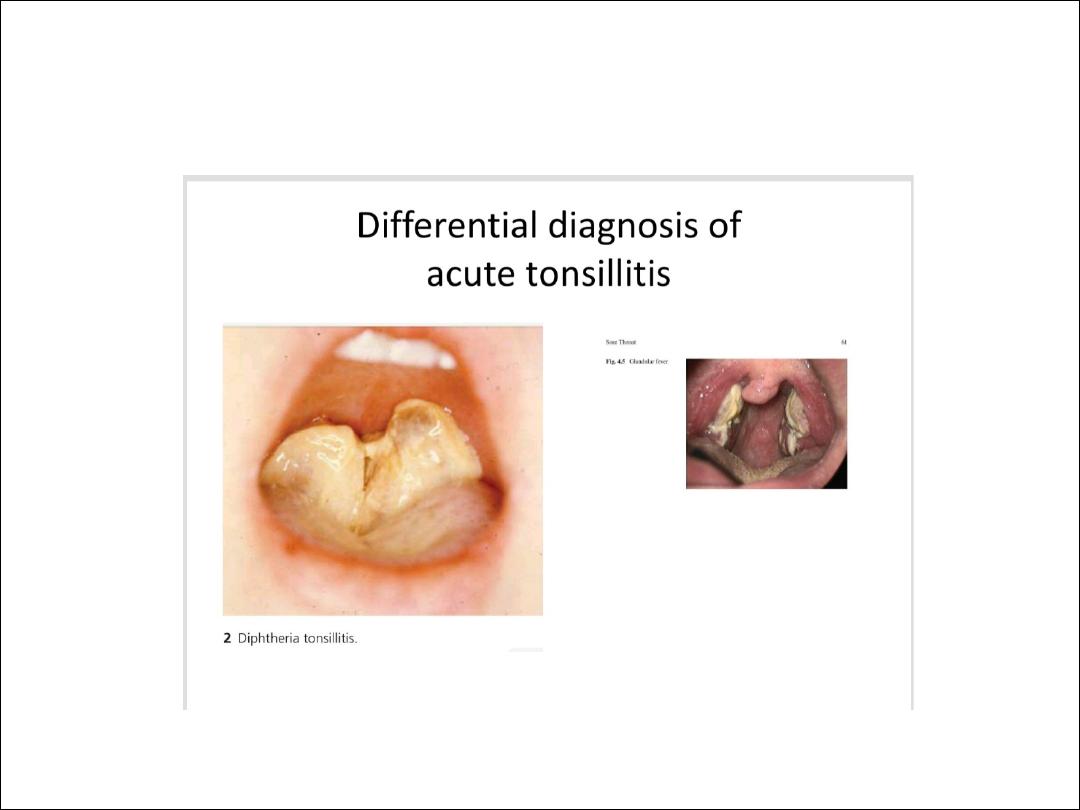
Diphtheria :
Epidemiology: Diphtheria was controlled for a time by active immunization,
but lately its incidence has been rising due to low vaccination numbers,
especially in immigrants from Eastern Europe, and secular fluctuations in the
virulence of the toxin .All instances of the disease must be reported to health
officials.
Causative organism: The causative organism is Corynebacterium diphtheriae,
which is transmitted by droplet inhalation or skin-to-skin contact. The
incubation period
is 1–5 days.
Pathogenesis: The bacterium produces a special endotoxin that causes
epithelial cell necrosis and ulcerations.
Clinical manifestations: Two main forms are distinguished based on their
clinical presentation:
• Local, benign pharyngeal diphtheria
• Primary toxic, malignant diphtheria
The disease begins with moderate fever and mild swallowing difficulties. The
clinical picture becomes fully developed in approximately 24 hours,
characterized by severe malaise, headache, and nausea.
Differential diagnosis
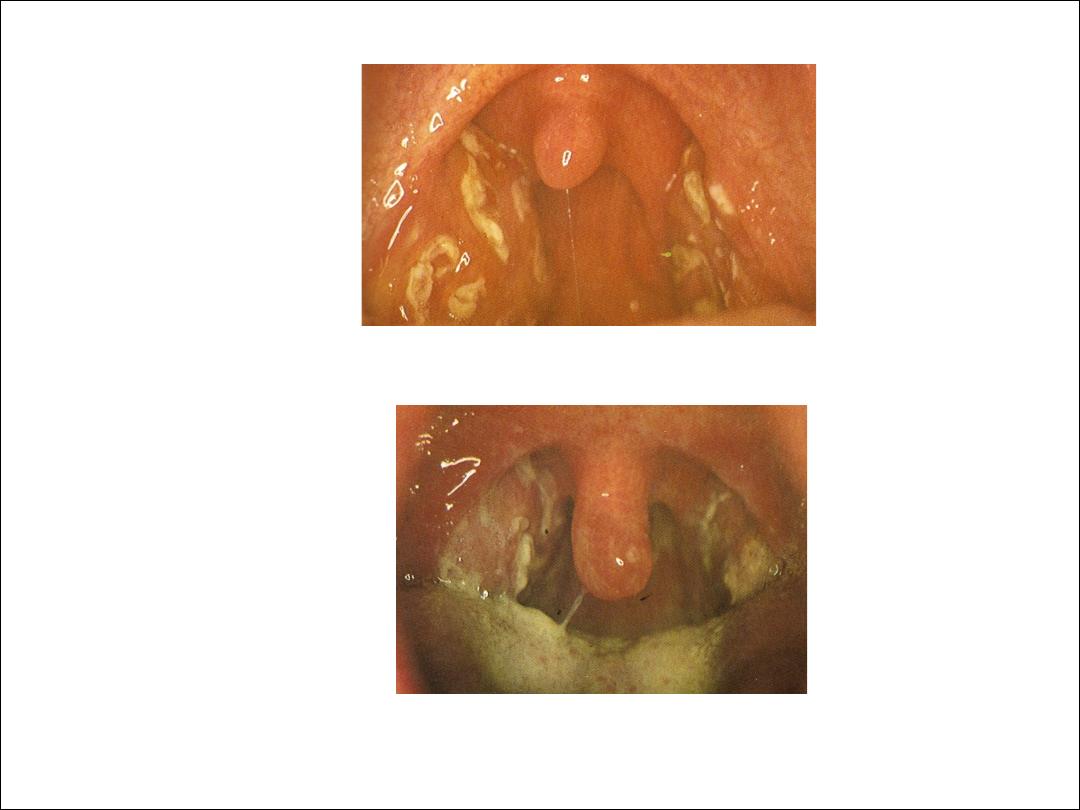
Diagnosis: Mirror examination of the pharynx reveals typical
grayish-yellow pseudo membranes that are firmly adherent to
the tonsils and may spread to the palate and pharynx. The
underlying tissue bleeds when the coatings are removed. A
slightly sweet breath smell is also characteristic. The diagnosis
is confirmed by the overall clinical impression, combined with
smear findings.
Treatment: First, the patient should be isolated. Whenever
diphtheria is suspected, even before it is confirmed by smear
results, diphtheria antitoxin (200–1000 IU/kg body weight)
should be administered by intravenous or intramuscular
injection. Allergy to the antitoxin should be excluded (with a
skin test) before it is administered .Penicillin G should also be
administered.
Discharge from the hospital is contingent upon test results :
three smears taken at 1-week intervals must all be negative.
Two percent of patients continue to carry the bacterium and
should undergo tonsillectomy.

Complications: Dangerous complications, which occur mainly in association
with the primary toxic malignant form, are toxic myocarditis (which may
terminate fatally in 10–14 days) and interstitial nephritis. The more severe
the diphtheria, the earlier these complications may arise. Electrocardiography
and urinalysis follow-ups should be continued for at least 6weeks after the
onset of the disease.
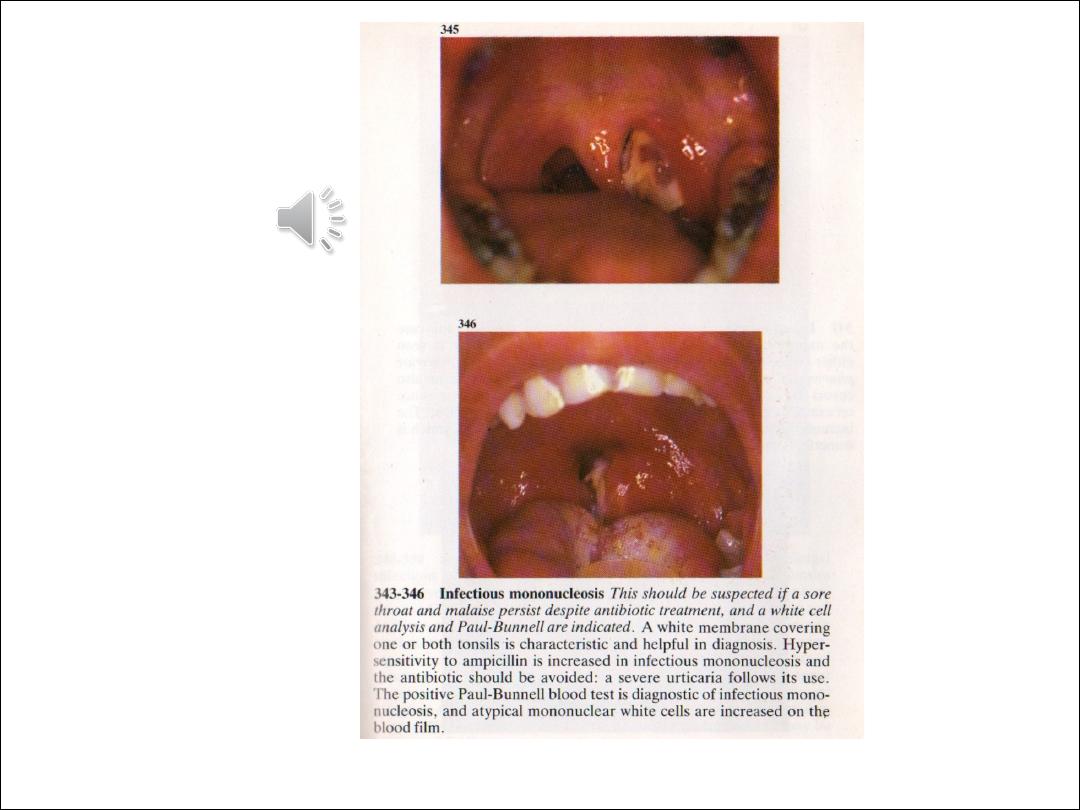
Glandular fever
Glandular Fever is also known as infectious mononucleosis or Epstein-Barr
virus infection. It is common in teenagers and young adults. Patients with
glandular fever may present a similar picture to patients with acute bacterial
tonsillitis, but with a slightly longer history of symptoms. Diagnosis relies
upon a positive monospot or Paul-Bunnell blood test, but early in the course
of the disease this test can still show up negative.
Signs and symptoms
•
Sore throat
•
Pyrexia
•
Cervical lymphadenopathy
•
White slough on tonsils
•
Petechial haemorrhages on the palate
•
Marked widespread lymphadenopathy
•
Hepatosplenomegaly.

Treatment
This is a self limiting condition for which there
is no cure as such. Treatment is largely
supportive with painkillers, although patients
may appreciate a short course of
corticosteroids to decrease swelling. IV fluids
may be necessary if they cannot drink enough.
Complications
Patients should be advised to refrain from
contact sports for six weeks because of the
risk of a ruptured spleen. This can lead to life
threatening internal bleeding.