Dermatology / 2018-2019 Dr. Hussein A. Al-Sultany
Acne Vulgaris
Definition:
it is a self-limited disorder of the pilosebaceous unit, that is seen primarily
in adolescents, and appears on skin areas with numerous sebaceous glands.
Epidemiology:
Acne prevalence hits its peak during the teenage period (between 12 and 24 years), with
more than 85% of adolescents affected, and then steadily decreases. However, acne may
persist through the third decade or even later, particularly in women.
It affects both sexes equally, but the disease tends to be earlier and more persistent in
females, and more sever in males.
Genetic Factors: The number, size, and activity of sebaceous glands is inherited, and
acne severity seems to be familial.
Dietary Factors: Several studies have found that intake of milk, especially skim milk,
and a high glycemic-load diet are positively associated with acne prevalence and
severity
.
Etiology and Pathogenesis:
Development of acne involves the interplay of a variety of factors, including:
1- Poral occlusion: the epithelium of the upper hair follicle, the infundibulum, becomes
hyperkeratotic
with
increased
cohesion
of
the
keratinocytes
(follicular
Hyperkeratinization), result in a plug in the follicular ostium. This plug then causes
downstream concretions of keratin, sebum, and bacteria to accumulate in the follicle,
cause dilation of the upper hair follicle producing a microcomedone.
Some environmental factors (e.g. some cosmetics) can cause poral occlusion.
2- Excess sebum production:
patients with acne produce more sebum than those
without acne,
androgens control the sebaceous glands activity and the production of
sebum. These glands, react to maternal androgens for a short time after birth, and then lie
dormant until puberty, when the sebum output is increased.
Sebaceous glands are largest and most numerous on the face and upper trunk (acne prone
areas).
3- Bacterial: propionibacterium acne, a normal skin commensal of the pilosebaceous
unit, is a Gram-positive, anaerobic bacterium. Elevated production of sebum and
blockage of the follicle can cause P. acne bacteria to grow and multiply.
4- Inflammation: the microcomedone will continue to expand with densely packed
keratin, sebum, and bacteria, eventually this distension will cause follicular wall rupture,
causing extrusion of the keratin, sebum, and bacteria into the dermis results in a brisk
inflammatory response (represented clinically as papules, pustules, nodules or cysts).
1
Presentation:
● Sites: the predilection sites are the face, shoulders, upper chest and back.
● Lesions:
A-The non-inflammatory lesions (comedones): either open (black comedones) or closed
(white comedones). The black comedone appears as a flat or slightly raised lesion with a
central dark colored follicular impaction of keratin and lipid. The white comedone (the
most dangerous), may be difficult to visualize; they appear as pale or yellowish-white,
slightly elevated, small papule.
B-The inflammatory lesions: papules, pustules, nodules or cysts.
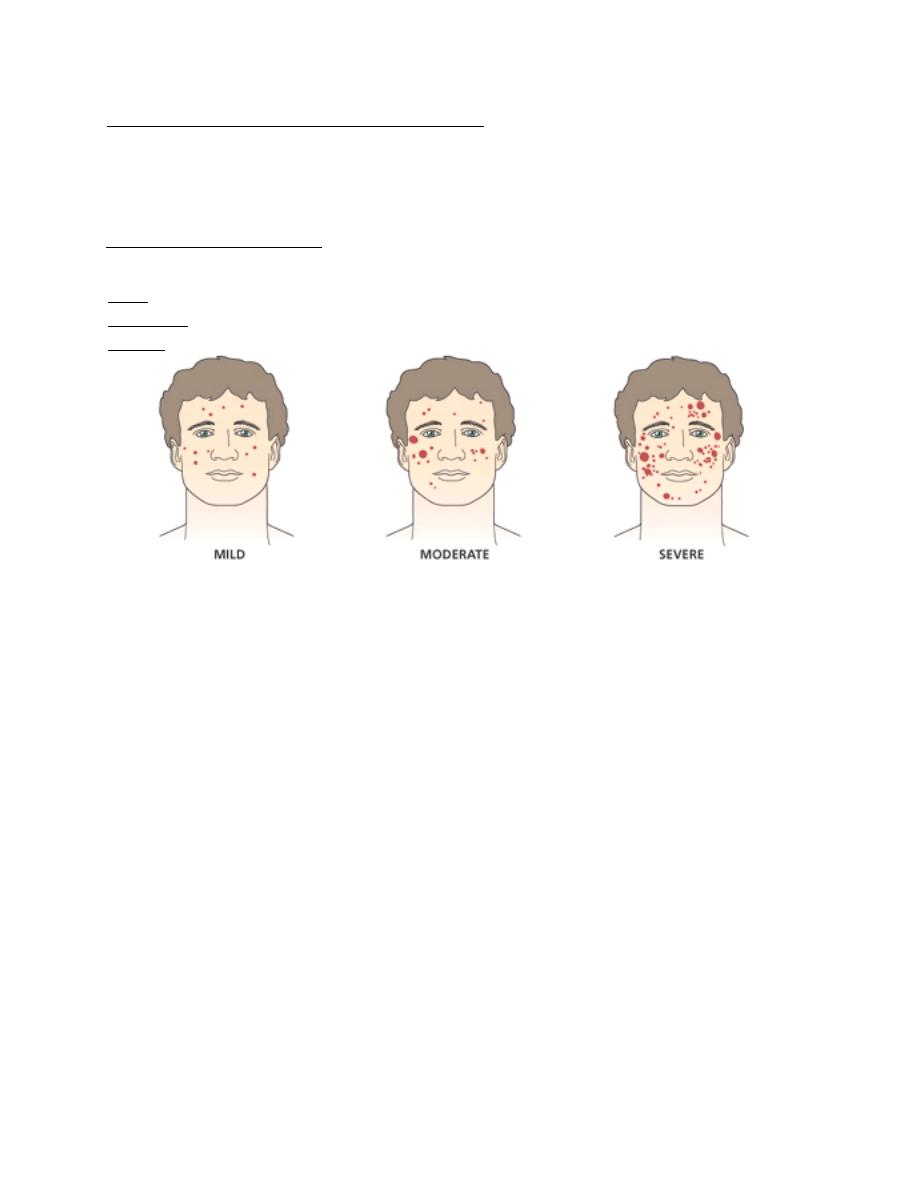
● Severity: acne vulgaris classified according to its severity into:
1- Mild (few papules & pustules (or comedones) with no nodules).
2- Moderate (many papules & pustules with few nodules).
3- Severe (many papules & pustules with many nodules).
Acne Variants:
1- Conglobate: a severe form with abscesses or cysts and communicating sinuses.
2- Fulminans: is a conglobate acne accompanied by fever, joint pains and a high ESR.
3- Infantile: rare type of acne presents at, or appears soon after birth. It is more common
in males and may last up to 3 years.
4- Excoriated: mostly seen in young girls. Obsessional picking or rubbing leaves
discrete denuded areas.
5- Late onset: occurs mainly in women and is often limited to the chin. Nodular and
cystic lesions predominate. It is stubborn and persistent.
6- Post epilation acne: followed hair epilation, mostly in women, inflammatory in
origin, papulopustular with absence of comedones.
7- Drug-induced (acne medicamentosa): suspicion should be raised when a
papulo-pustular acne, appears suddenly in a non teenager and coincides with taking of a
drug known to cause acneiform eruption {steroids (systemic or topical), androgens and
oral contraceptives, isoniazid, phenytoin, lithium, vit B12, bromides and iodides}.
Complications:
1- Psychological disturbances and depression.
2- Transient macular erythema.
3- Post inflammatory hyperpigmentation: may persist for months after resolution of acne.
4- Permanent scarring: There are five types of acne scars, ice pick (narrow, deep and
widest at the surface), rolling (shallow, wide) boxcar (the width is similar at the surface
and base), hypertrophic and keloidal scars.
2
Treatment:
I- General measures:
1- Psychological support: acne frequently has marked psychological effects.
2- Treatment of the underlying cause if found.
3- Determine the predominant type of acne lesions (comedonal or inflammatory).
4- Determine the severity of acne; mild acne may need topical treatments only,
Moderate or severe type, need to add systemic treatments.
II- Topical treatment:
1- Regular gentle cleansing:
2- Benzoyl peroxide (BPO): it is antibacterial and anti-inflammatory.
3- Topical antibiotics: as clindamycin or erythromycin.
4- Retinoids: vitamin A (retinol) analogues, (including: tretinoin, isotretinoin,
adapalene, and tazarotene) are especially effective against comedones. They may cause
skin irritation and photosensitivity.
5- Azelaic acid: is bacteriocidal for P. acne, it is also anti-inflammatory and inhibits the
formation of comedones by reducing the proliferation of keratinocytes.
6- Others: as sulphur, zinc sulphate, and peeling agents as alpha hydroxy acids (AHA).
7- Combinations.
III- Systemic treatment:
1- Antibiotics: (should be used for at least than 3 months).
a) Tetracyclines: (not given for pregnant or lactating patients).
Doxycycline: 100 mg tablets or capsules, once or twice daily. It is safe and effective.
The capsule should be taken after meal with a lot of water (because of gastric upset).
Minocycline: 50-100 mg once or twice daily. It is more effective than doxycycline, but
it is much more expensive and can cause blue grey pigmentation, especially on the faces
and over the shins.
b) Macrolides: azithromycin 500 mg three times weekly or erythromycin 500 mg four
times daily. It is the next antibiotic of choice, it is preferable for pregnant women and
those who might become pregnant. Its major drawback is the development of resistant P.
acne.
c) Trimethoprim: as a third-line antibiotic for acne, used in patients who do not respond
to other antibiotics.
2- Isotretinoin: it is a vitamin A (retinol) analogues, inhibits sebum excretion, growth of
P. acnes and the inflammatory processes. The drug is reserved for severe nodulocystic
acne. It is given for 4–6 months, in a dosage of 0.5–1 mg/kg/day.
The most important side-effect is teratogenicity, effective contraception must be taken
for 1 month before starting, throughout treatment, and for 1 month after treatment. Tests
for pregnancy should be carried out twice before starting treatment and at each follow-
up visits. Other side-effects are dry lips, mouth, vagina and eyes, peeling of skin,
pruritus, paronychia, hair thinning or loss, and hyperlipidaemia (mainly TG).
3
3- Hormonal: oral contraceptives (as Diane-35), spironolactone, or cyproterone acetate
used when there is hormonal disturbances and overproduction of androgen (as in PCOS).
Glucocorticoid hormones can be used in very severe acne.
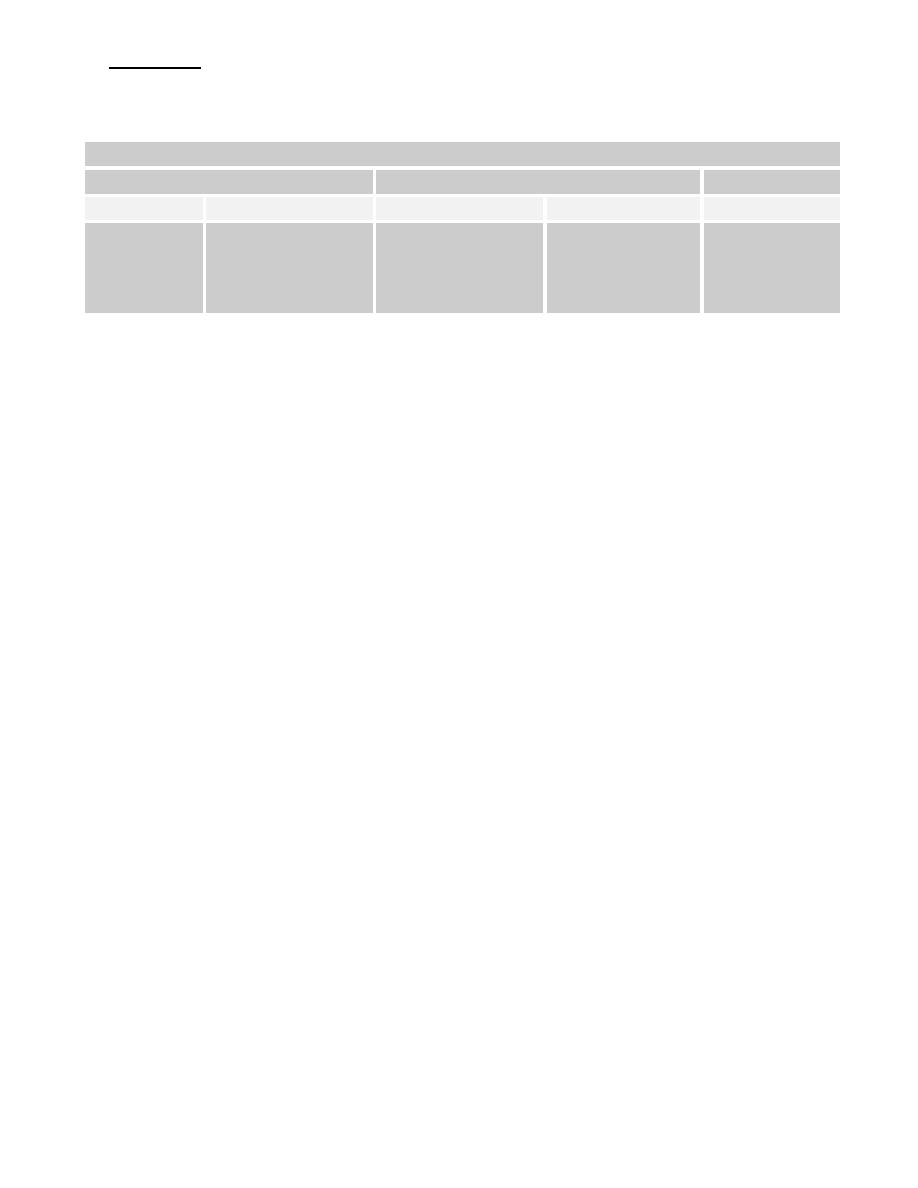
Treatment Algorithm of Acne Vulgaris
Mild
Moderate
Sever
Comedonal
Papular/pustular
Papular/pustular
Nodular
Nodulocystic
Topical
retinoid
Topical antibiotic
+Topical retinoid
or BPO
Oral antibiotic
+ topical retinoid
± BPO
Oral antibiotic
+ topical retinoid
± BPO
Oral
isotretinoin
IV- Physical treatment:
1-
Comedone removal
: by a comedon extractor.
2- Intralesional injections: of 0.1 mL of triamcinolone acetonide (2.5–10 mg/mL)
hasten the resolution of nodulocystic lesions, but can leave atrophy.
3- Phototherapy: lasers (pulse dye & KTP), intensive pulse light (IPL), UV radiation,
blue light therapy, and
photodynamic therapy (PDT)
.
V- Treatment of acne scars:
1- Atrophic scars:
(ice pick, rolling, or boxcar scars)
a) Laser therapy (fractional CO2), chemical peels, or dermabrasion: resurfacing the
skin by exfoliate the epidermis in a controlled manner, leading to regeneration of new
smooth skin .
c) Filler injections: hyaluronic acid can be used to raise atrophic scars to the level of
surrounding skin.
d) Collagen induction therapy: repeatedly puncturing the skin with a special tiny,
sterile needles results in induction of collagen growth (as dermal roller, dermal pen, and
fractional microneedle radiofrequency (secret)) .
2- Hypertrophic scars: (hypertrophic and keloidal scar )
a) Semiocclusive ointments (silicone).
b) Intralesional steroid injections: full strength triamcinolone acetonide injections into
the scar may help flatten and soften the appearance of hypertrophic scars.
c) Surgery and laser therapy: not widely used, because of high risk of recurrence.
d)
Radiotherapy.
4

Rosacea
Definition:
it is a chronic inflammatory disorder involving the skin of the nose,
forehead, and cheeks (center of the face), that is characterized by congestion, flushing,
and telangiectasia.
Epidemiology:
the vast majority of cases occur in fair-skinned individuals.
It predominantly affects middle age women (30-50 years).
Etiology and Pathogenesis:
The exact cause and pathogenesis of rosacea is still unknown, but there are many
etiological and triggering factors, included:
1- Etiological factors:
● Abnormal vascular reactivity.
● Sun damage.
● Abnormalities of dermal connective tissue structure or composition.
● Abnormalities of the pilosebaceous structure.
● Microbial colonization: commensal organisms as P.acne and Demodex folliculorum.
2- Triggering factors:
Hot or cold temperature, sunlight, wind, hot drinks, spicy foods, alcohol, exercise,
emotions, cosmetics, topical irritants, and medications that may promote flushing
(as vasodilators and steroids).
Types and Clinical Features:
1- Papulopustular rosacea: it is the most common type, manifests as persistent, central-
face erythema with papules and pustules that predominate in convex areas of face.
(center of the face).
2- Erythematotelangiectatic rosacea: is characterized by persistent facial erythema and
flushing along with telangiectases, central face edema, burning and stinging, roughness
or scaling, or any combination of these signs and symptoms.
3- Phymatous rosacea: is characterized by patulous follicular orifices, thickened skin,
nodularities, and irregular surface contours in convex areas.
"Phyma" is the Greek word for swelling, or mass. Phyma most often occurs on the nose
of men (rhinophyma), women with rosacea usually do not develop phyma, perhaps for
hormonal reasons.
4- Ocular rosacea: may manifested as blepharitis, conjunctivitis, iritis, scleritis,
hypopyon, and keratitis. In half of ocular rosacea patients, ocular symptoms develop
after skin symptoms.
Complications:
1- Rhinophyma.
2- Ocular complications.
3- Lymphodema.
5

Differential Diagnosis:
A- Acne vulgaris: it differs from rosacea by:
1- More common.
2- Usually appears in adolescence (rosacea usually affect middle age).
3- Male and female are affected equally (rosacea affect women predominantly).
4- Affects fair and dark individuals (the vast majority of rosacea occur in fair-skinned).
5- All the face can be affected (rosacea usually affect the center of the face).
6- Extrafascial involvement are common, as chest and shoulders (very rare in rosacea).
7- Presence of comedones and scars (absent in rosacea).
B- Seborrhoeic dermatitis.
C- Systemic lupus erythematosus.
D- Photodermatitis.
E- Other causes of flushing: as carcinoid syndrome, or menopause.
Treatment:
Papulopustular:
Topical:
Metronidazole, ivermectin, azeleic acid, erythromycin, clindamycin, benzoyl peroxide,
permethrin, pimecrolimus or tacrolimus.
Systemic: for two months.
1- Tetracyclines: doxycycline, minocycline or tetracycline (same doses of acne).
2- Macrolides: azithromycin or erythromycin (same doses of acne).
3- Metronidazole: 200 mg once or twice daily.
4- Isotretinoin:
0.3 mg / kg / day.
Erythematotelangiectatic:
1- Photoprotection.
2- Topical agents: e.g. azelaic acid, or metronidazole.
3- Topical brimonidine gel:
Selective α2-adrenergic agonist that improves erythema.
4- Topical oxymetazoline cream:
Selective α1A-adrenergic agonist, improves erythema.
5- Laser therapy:
vascular lasers (pulsed dye, or KTP), and intense pulsed light (IPL).
Best Regards
6
