Medical physics Dr. Entidhar. Altaee
1
Dr.Entidhar .J.Khamees
Chapter 9
Physics of diagnostic X-Rays
Objectives: after the end of this lecture, the student must know:
1- The main parts of X-ray unit
2- How X-rays are absorbed
3- Application of X-ray in medicine
X – rays:- electromagnetic radiation (EMR) of very short wavelength (λ 1-0.1 A°)
and very high penetrating power. It is very useful in diagnosis & radio therapy
The amount of energy carried by each photon depends on the frequency of radiation:
E = h υ = h c / λ
Where
h = Plan's constant = 6.6*
10
−34
(joule. sec)
c = velocity of light = 3*
10
8
m/sec
υ = frequency of radiation.
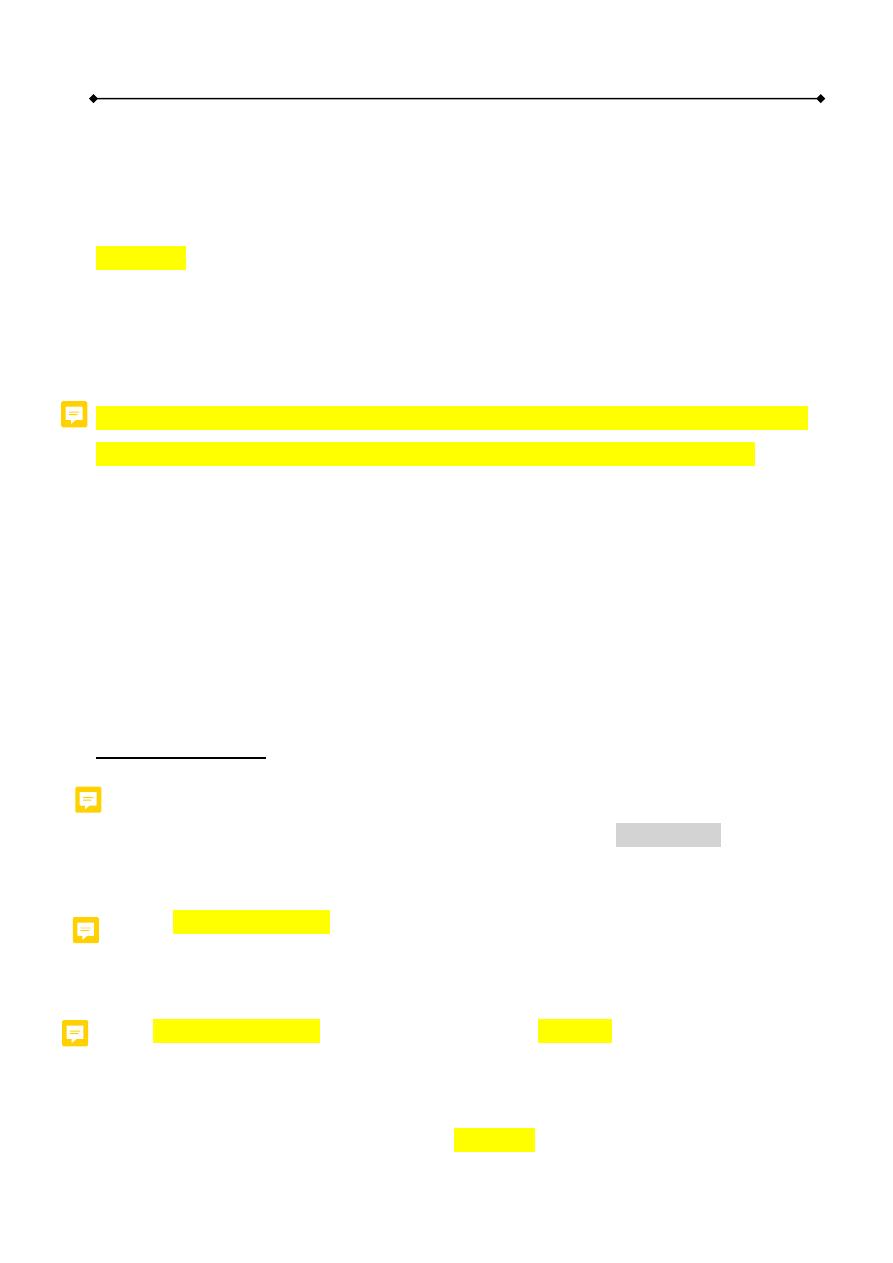
X- ray Production:
X-rays are produced when highly energetic electrons interact with matter, converting
some of their kinetic energy into electromagnetic radiation. Accordingly, the main
components of the X-ray tube are:
1.
A source of electrons (the cathode , filament) ; the number of electrons (as well
as the number of produced X-ray photons) is controlled by the product of the
tube current and time (mAs).
2.
An evacuated space in which the electron are speed up (glass envelope).
3.
A high positive potential to accelerate the negative electrons which control the
energy of the electrons (as well as the energy of the X-ray photons) (kV).
4.
A target which the electrons strike (the anode).
Medical physics Dr. Entidhar. Altaee
2
Dr.Entidhar .J.Khamees
NOTE: In the X-ray tube, up to 99% of accelerated electrons energy is converted
to heat and approximately 1% is converted to X-ray photons.
In general, the higher the atomic number (Z) of the anode , the more intensity X-
ray beam is produced (Z tungsten = 74) .
Increase the current in the cathode circuit = increase electrons.
Increase kv = increase speed of electron = increase energy of photons = high
resolution.
Fig. The basic components of an x-ray unit
The following techniques are used to overcome overheating problem in the anode
of the X -ray tube:
1. The anode material should has a high melting point (for tungsten 3400 C°)
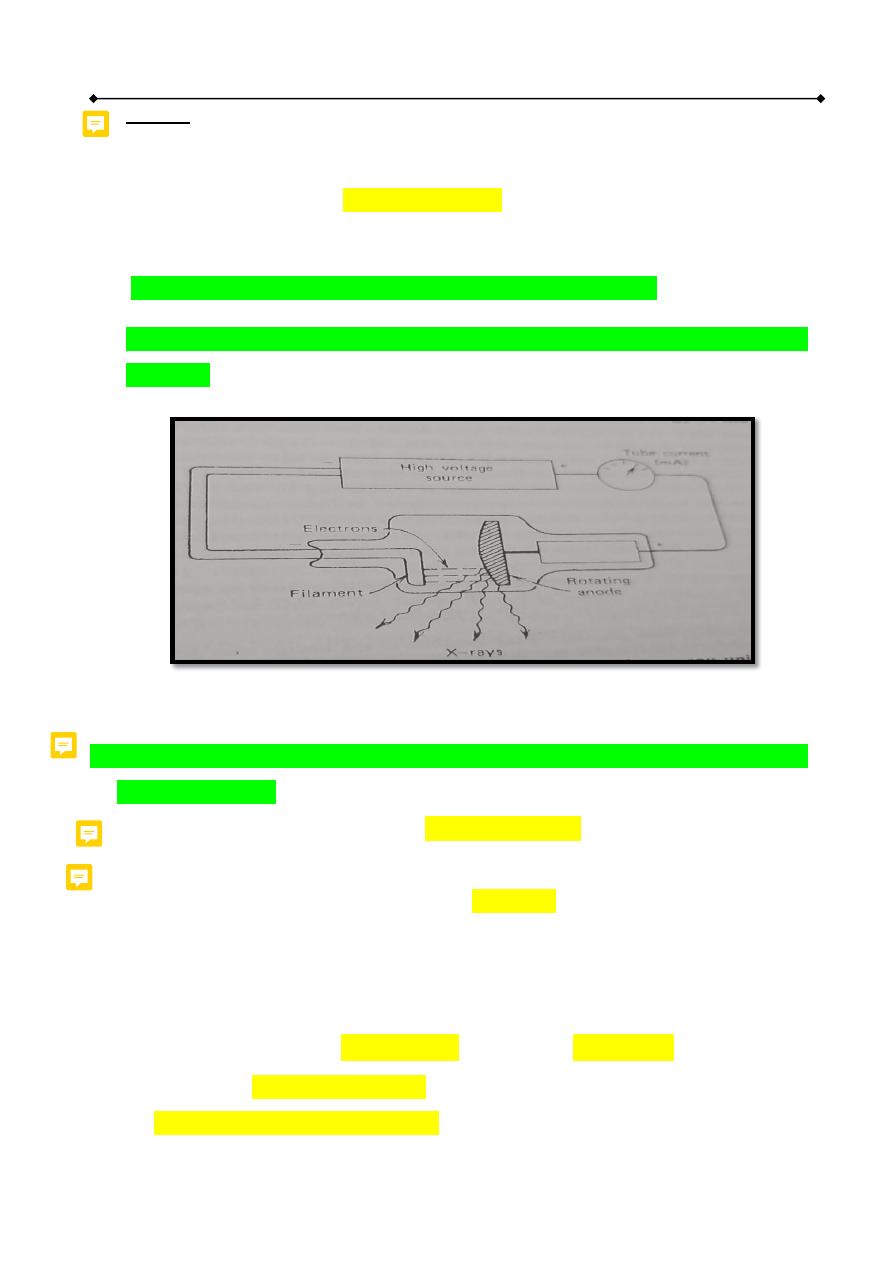
2.
Equipped the X-ray tube with two filaments which are used interchangeably
to produce large or small focal spots, focal spot is an area on the target struck
by electrons. The small focal spot produces less image blurring than the large
focal spot but it concentrates the heat on small area.
3.
Increasing the area struck by electrons (focal spot area) without increasing the
image blurring by the angulations’ of the anode 10 ° to 20 ° . This technique
is called as line- focus principle
4.
Using rotating anode X-ray tube (3600 rotation per minute) .
Medical physics Dr. Entidhar. Altaee
3
Dr.Entidhar .J.Khamees
Figure 14-1: line focus principle to avoid overheating
Types of X- ray
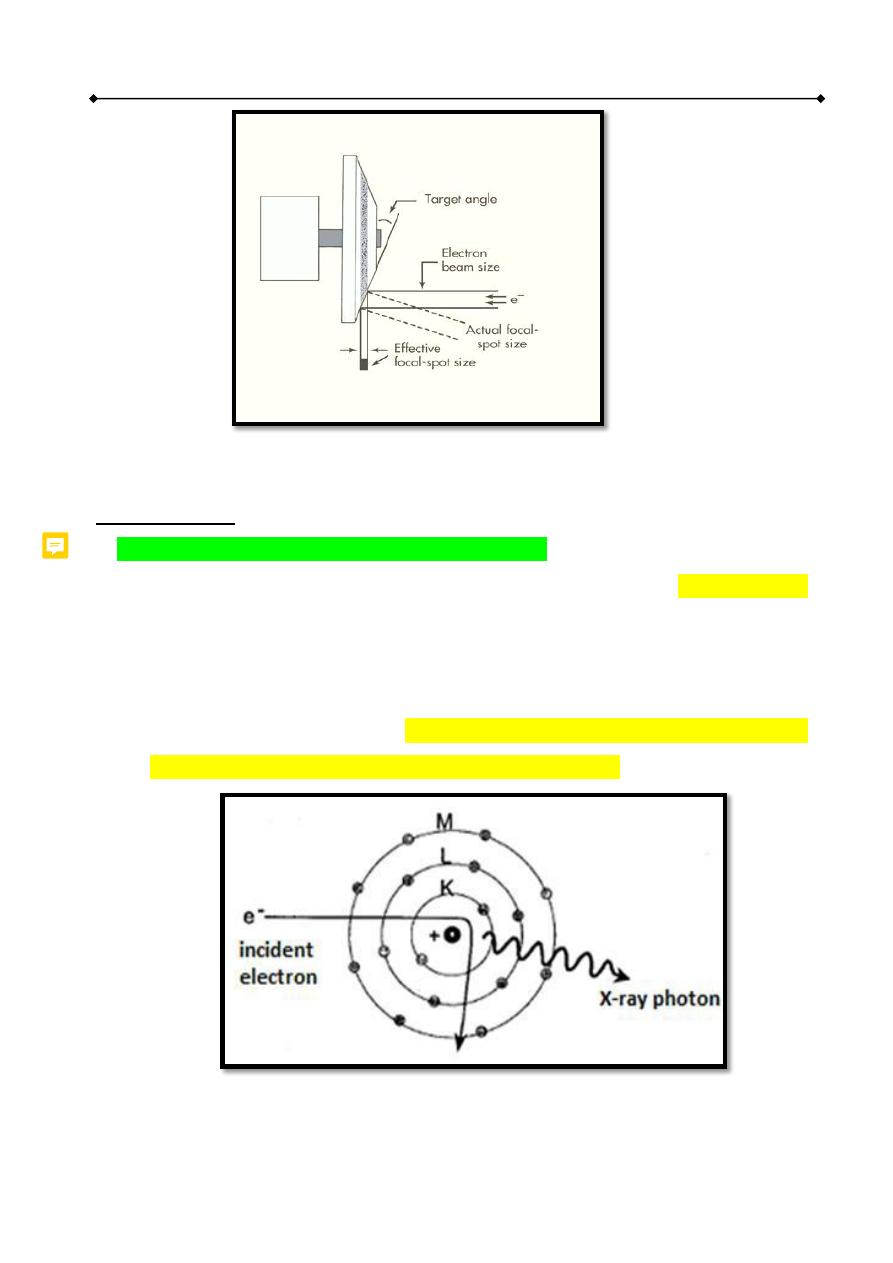
1. Bremsstrahlung Spectrum (Continuous X- ray):
A small fraction of the accelerated electrons come near an atomic nucleus
within the target and are influenced by its positive electric field. The electrons
are decelerated and change its direction, causing a loss of kinetic energy, which
is emitted as an X-ray photon of equal energy (bremsstrahlung radiation). For
a given number of electrons the amount of bremsstrahlung depends on (Z)
number of the target (protons number) and the kV peak.
Fig. Bremsstrahlung Spectrum (Continuous X- ray)
Medical physics Dr. Entidhar. Altaee
4
Dr.Entidhar .J.Khamees
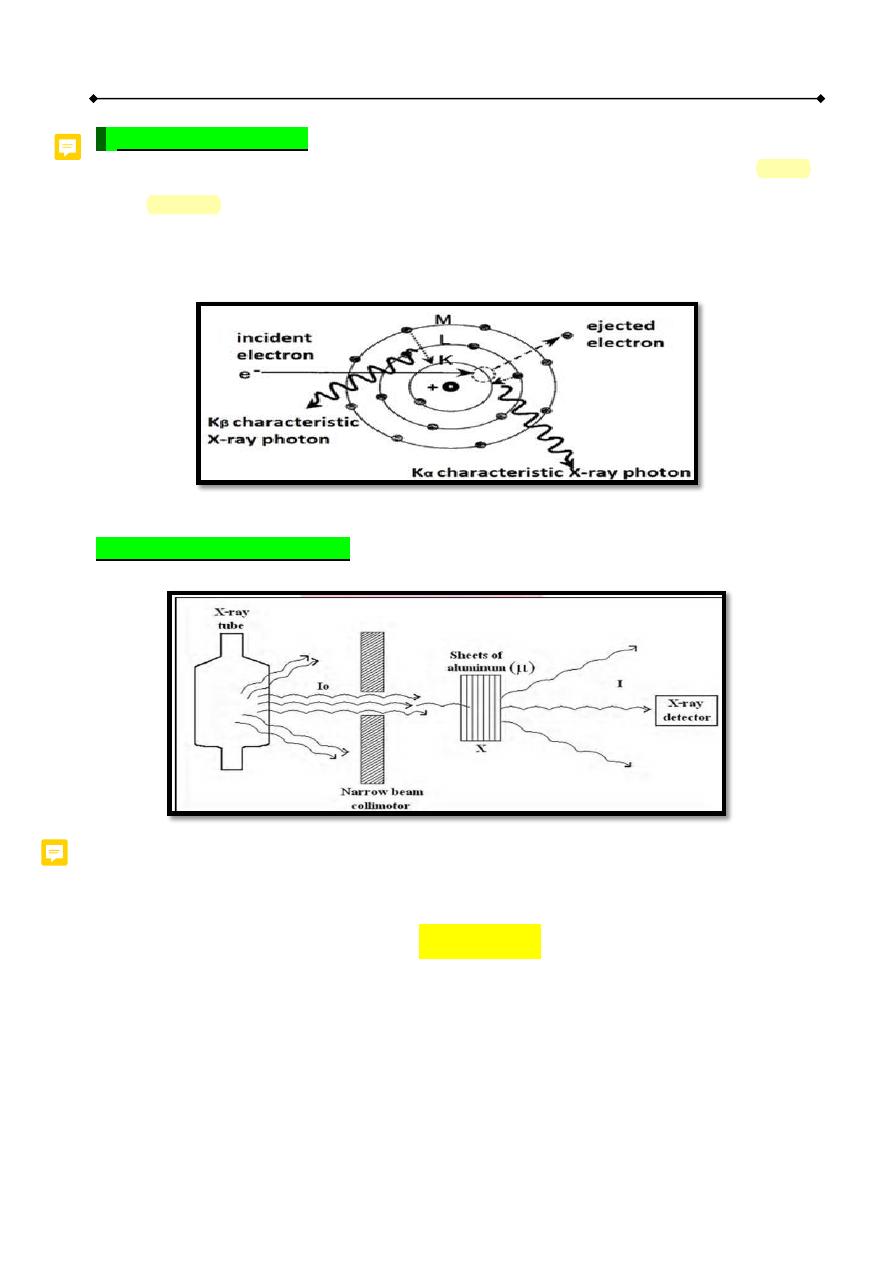
2. Characteristic X- ray
Characteristic radiation is emitted when an electron interacts with an atomic
electron within the anode and ejects it from its shell. Then the ejected electron
vacancy is filled by an outer shell electron emitting X-ray photon whose energy
is equal to the binding energy difference between the two shells.
Fig.
Characteristic X- ray
X- ray Absorption by Tissue
X -ray attenuation
is the reduction of the X-ray beam due to absorption and
scattering. The attenuation of an X-ray beam can be measured using the following
equation:
I = I˳ e
–μx
where
I
o
= initial beam intensity.
I = un attenuated (transmitted) beam intensity.
μ = linear attenuation Coefficient. e = 2.718
x = Thickness of the attenuator such as (brain tumor, bone, aluminum).
Medical physics Dr. Entidhar. Altaee
5
Dr.Entidhar .J.Khamees
Linear attenuation Coefficient (μ): measure the probability that photon interact
(absorbed or scattered) per unit length it travel in specified material.
It depends on:
1. energy of x-rays
2. atomic number (Z)
3. density (ρ) of material
Half value thickness HVT (X1/2) : is the thickness of material which reduce
the intensity of the beam of radiation one – half of its value (50%).
(HVT) X
1/2
= 0.693 / μ
Methods o f X- ray interaction with matter
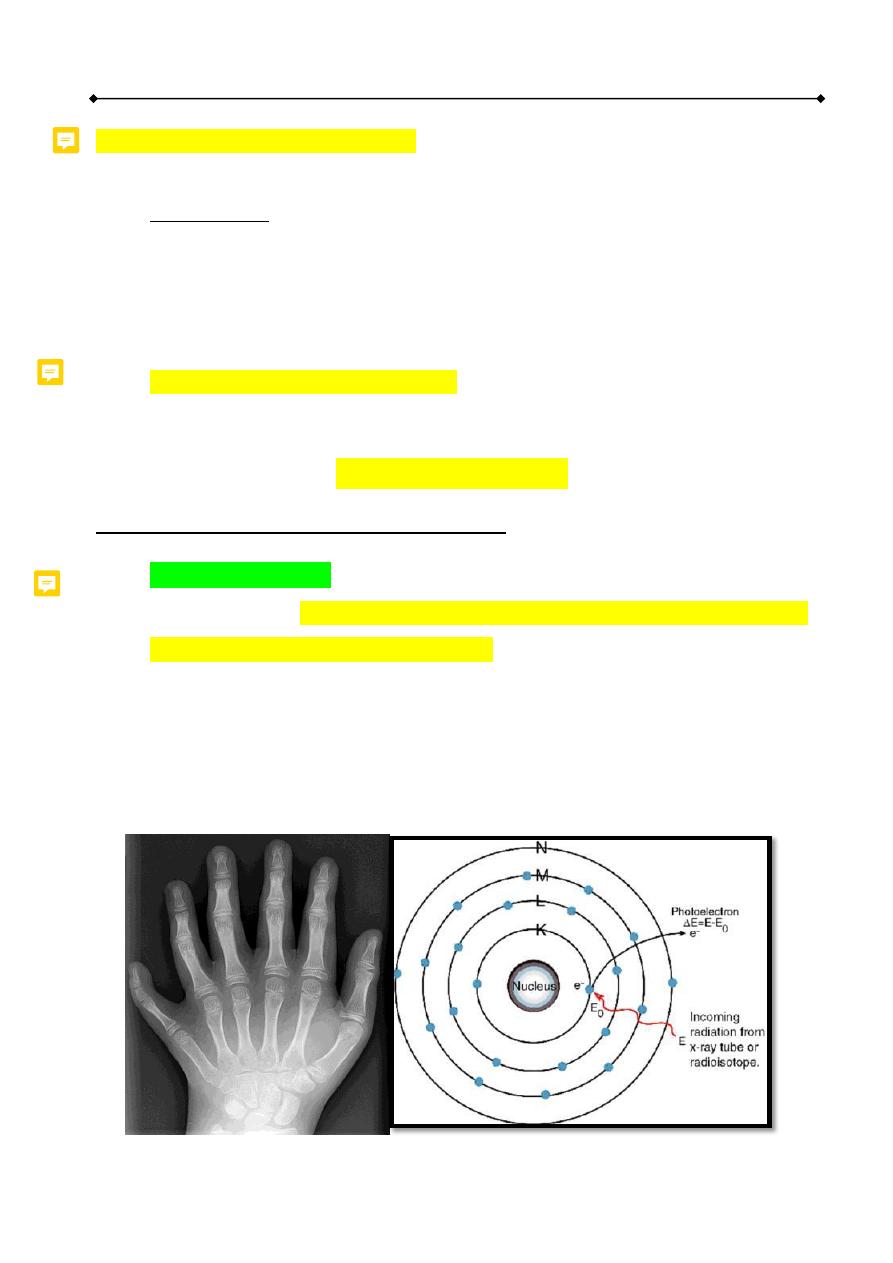
1. Photoelectric effect
is the most common way at diagnostic X-ray range . It
occurs when low energy X-ray photon transfers all of its energy to an atomic
electron more likely inner shell electron. It is more common in materials with
high (Z) number than those with low (Z) number.
Probability of photoelectric occur at material. e.g.:
Muscles ≤ 30 KeV
Bone ≤ 50 KeV
Medical physics Dr. Entidhar. Altaee
6
Dr.Entidhar .J.Khamees
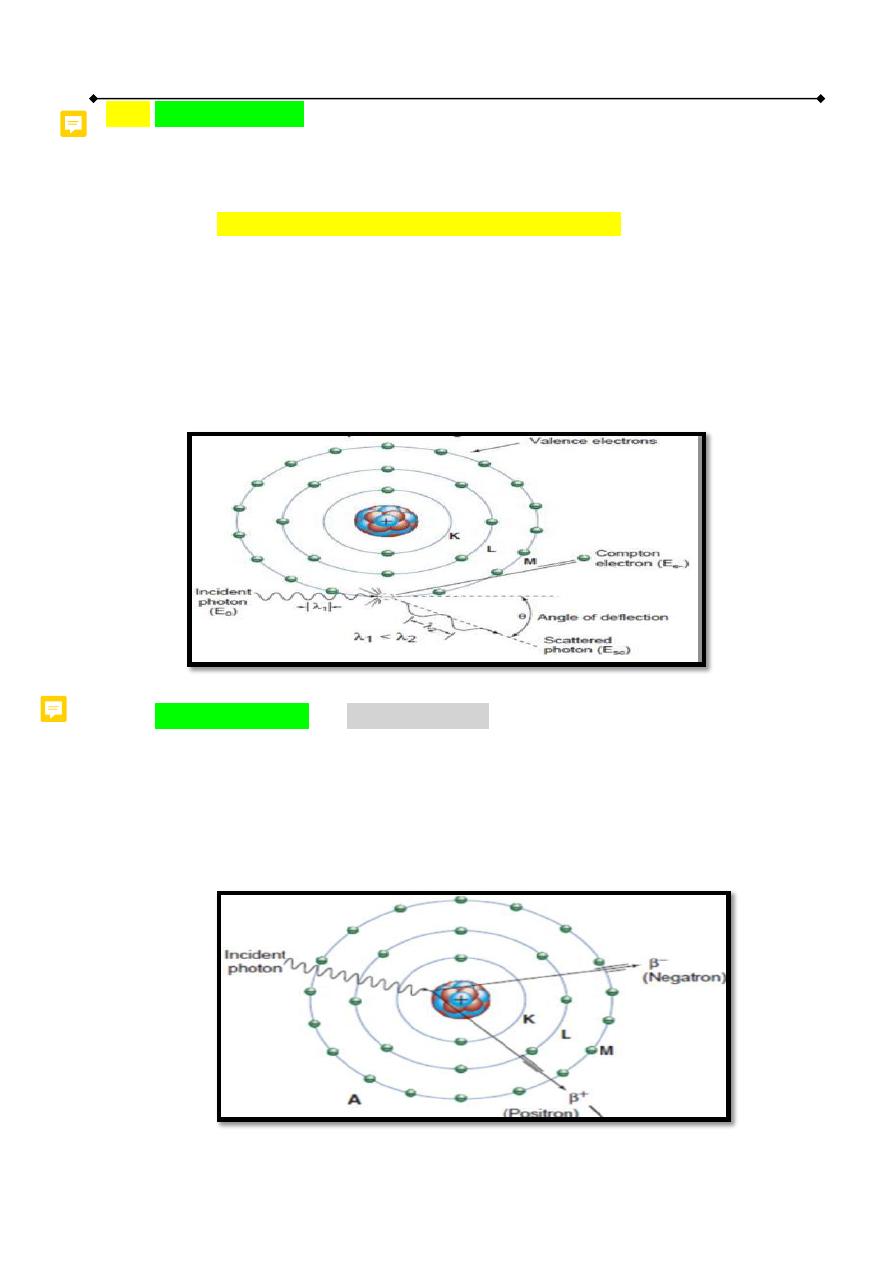
2. Compton Effect(C.E)
occurs when the X-ray photon collide with loosely
outer shell electron. In this case, the electron will receives part of the photon
energy and the remainder energy is given to Compton photon. Compton Effect
is more likely to occur in material with low (Z) number.
C.E. occur greatest at low Z material. e.g.:
In water or soft tissue C.E. is more probable occur than P.E effect at energy
≥ 30 KeV.
In bone C.E. is more probable occur than the P.E. effect at energy ≥ 100
KeV.
3. Pair production
is rarely occurring at diagnostic energy range as the
minimum energy required for pair production is 1.02 Mev. In pair production
the high energy photon enters the electric field of the nucleus and converted
into two particles (electron and positron) which are vanished and their mass
energy appears as two photons called
annihilation radiation
.

Medical physics Dr. Entidhar. Altaee
7
Dr.Entidhar .J.Khamees
X -ray contrast media
: are high Z materials introduced inside the patient
body (by injection or oral consumption) in order to increase the photoelectric
effect occurrence. Barium compounds and iodine compounds are the most
commonly used contrast agents. (
Z
barium
=56, Z
iodine
=53, Z
soft tissue
=7.42)
