
Pre-malignant & Malignant
diseases of the Uterus
Dr. Bushra J. AL-Rubayae

Objectives:
• Definition.
• Predisposing factors.
• Types.
• Clinical presentation.
• Diagnosis.
• Treatment options.
• Prognosis.

Endometrial Hyperplasia:
Excessive proliferation of endometrial glands
and to less extent endometrial stroma.
Due to excessive oestrogen stimulation.
Its significance is the progression to carcinoma.
25% of endometrial cancer, had a history of
hyperplasia.

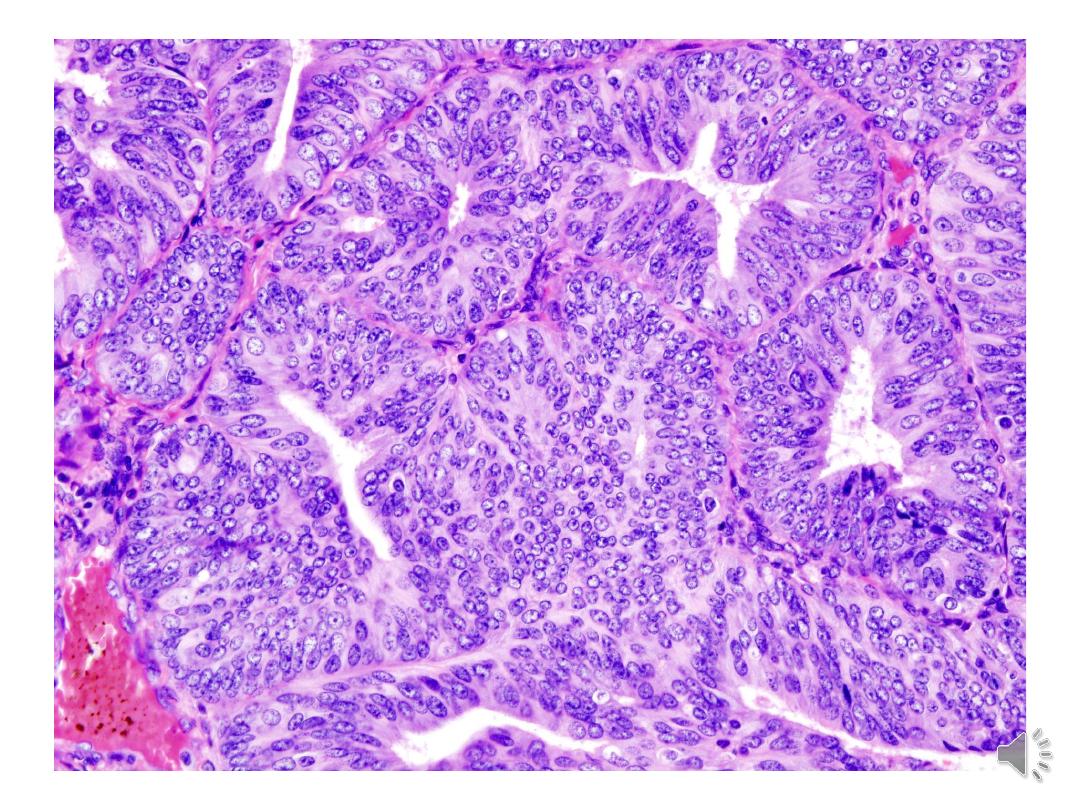
Classification of endometrial hyperplasia:
1- Simple H. Without atypia:
Increased no. Of glands & normal architecture.
90% regress , 1% progress to CA.
2 - Complex H. Without atypia:
Crowded irregular glands.
80% regress ,3% progress to CA.
3 - Simple H. With Atypia:
With cytological atypia (nuclei more
prominent & nuclear pleomorphism.
4 - Complex H. With atypia.

Patho-physiology:
Endogenous oestrogen unopposed by
progesterone
PCOD.
Obesity.
Tumours (granulosa cell tumour).
Medications: Tamoxifen(breast cancer ).
Late menopause.

Presentation:
Post menopausal bleeding.
Heavy menstrual bleeding.
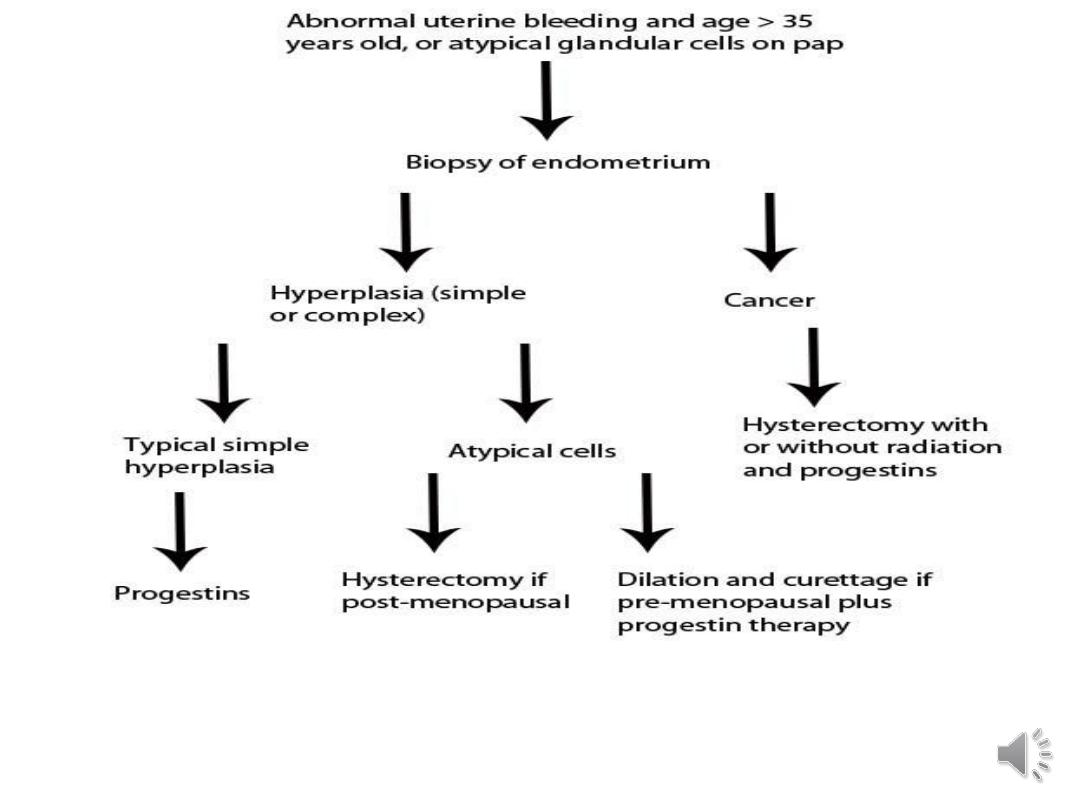
Diagnosis:
History & Physical exam.
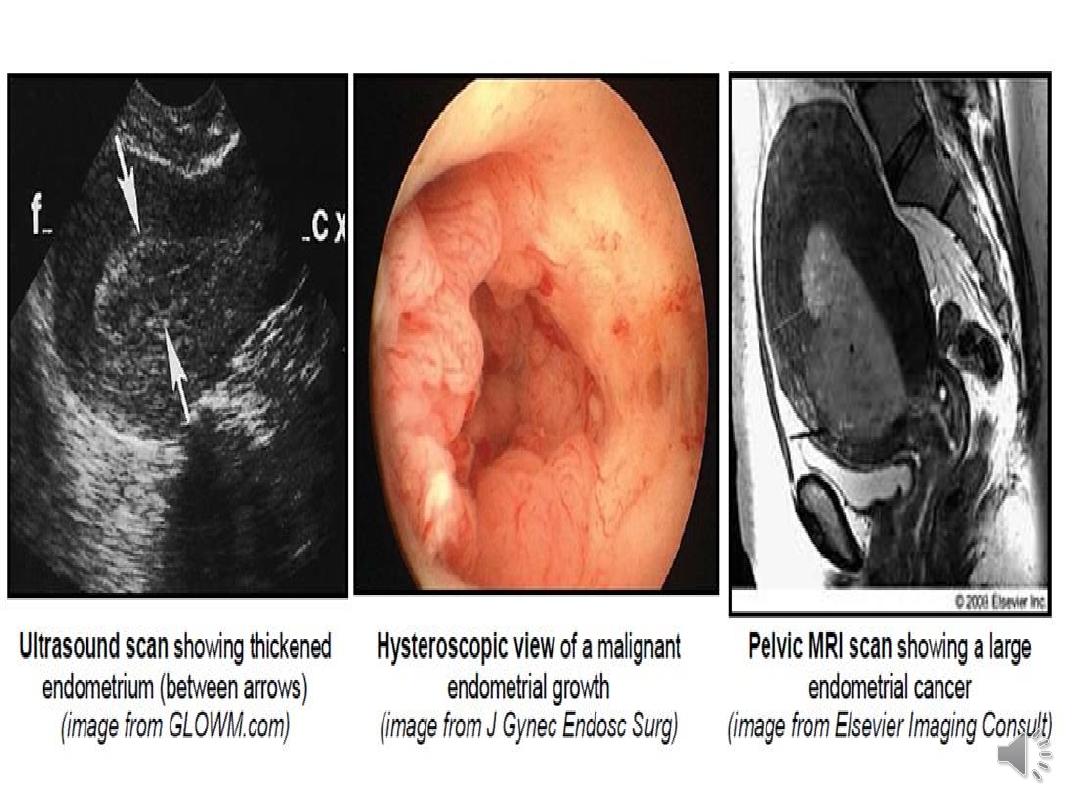
Investigations: TVUS: endometrial thickness.
Endometrial biopsy:
- Outpatient biopsy (pipelle biopsy)
- D&C.
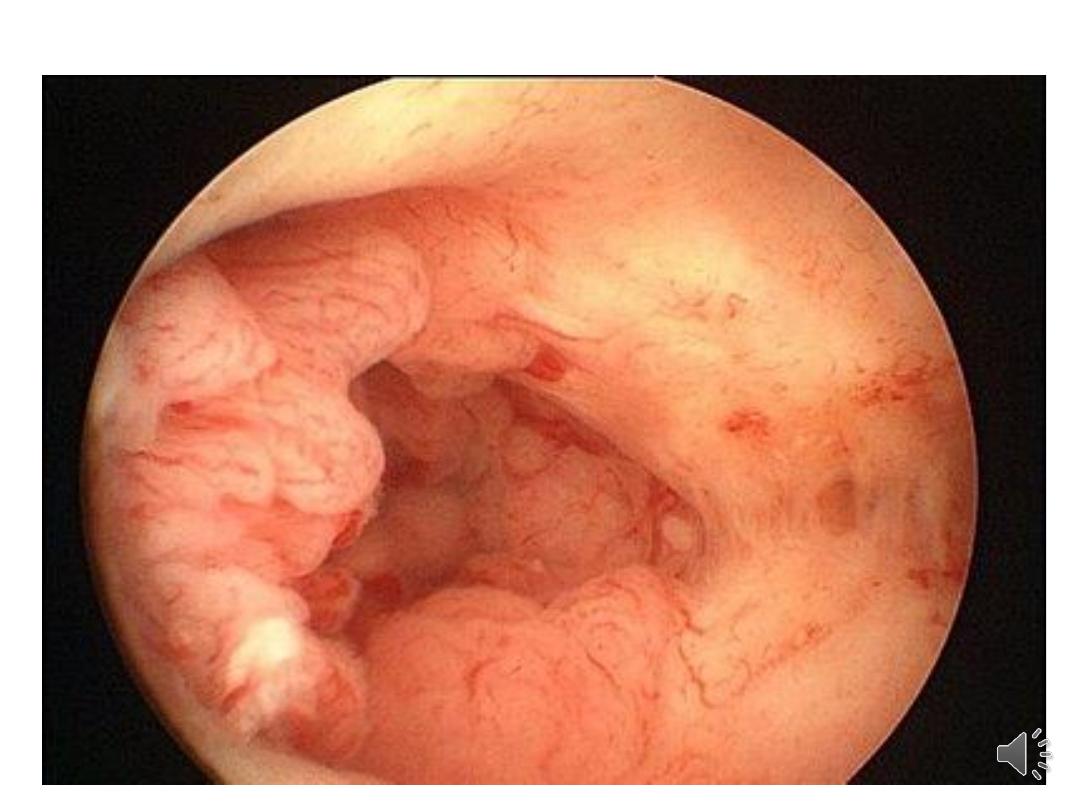
- Hysteroscopy.
MRI scan if TVUS not possible.

Treatment:
Depends on age, fertility wishes & risk factors
Medical: Progestins:
Control bleeding and prevent cancer
Medroxy -progesterone acetate
Micronized vaginal progesterone
Mirena(intrauterine system)
Which release progesterone daily for five years.

Surgical treatment:
Surgical options:Trans-cervical resection of
endometrium or Hysterectomy.
•If endometrial hyperplasia diagnosed in
postmenopausal women the treatment for
her is hysterectomy with bilateral salp;ngo-
oophrectomy.

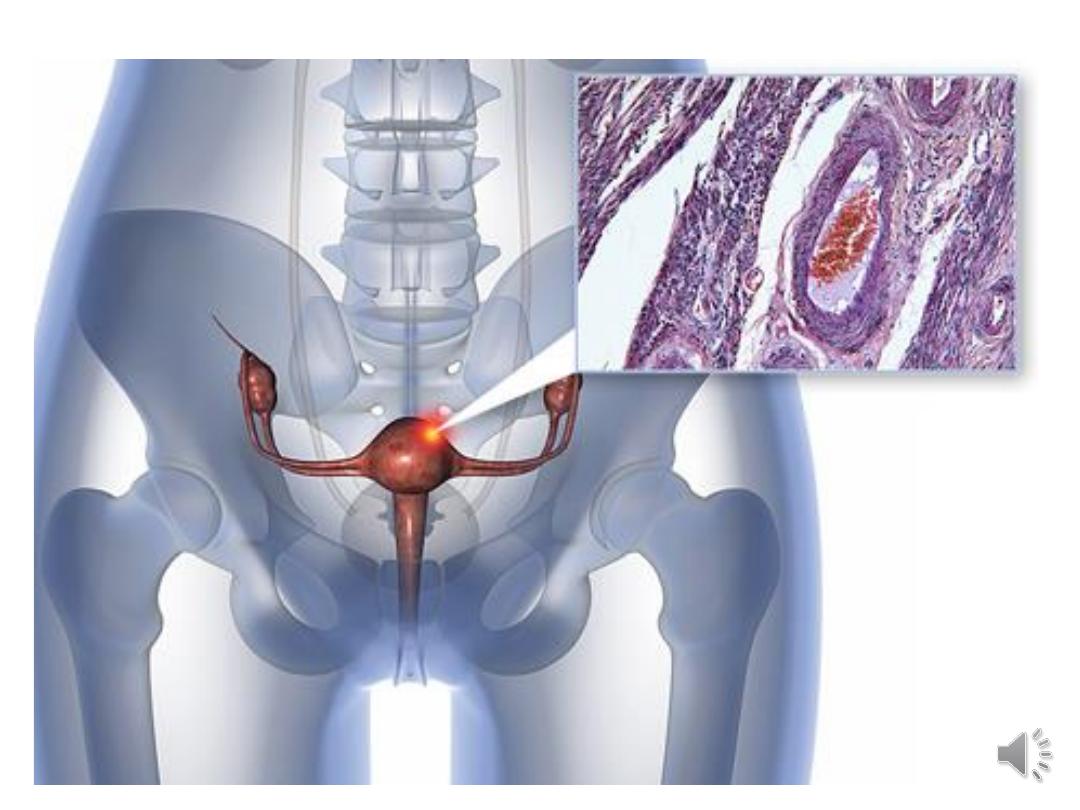
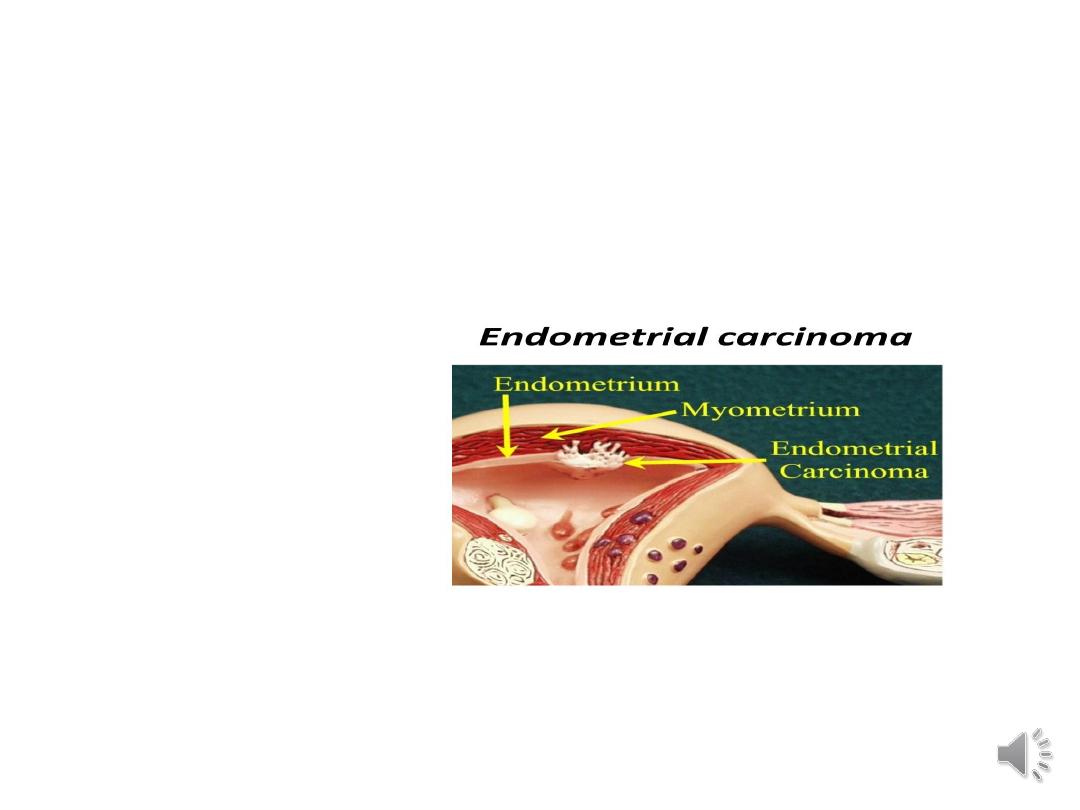
Endometrial Cancer:
•It’s growth out of control arise mostly from
endometrial lining of the uterus involving
the epithelial layer and invasion for the
basement membrane .It develop most
commonly in menopausal women.

Incidence:
Approximately 36 thousand new cases of uterine
cancer each year in the Unites States
1 out of every 44 women in America will get uterine
cancer.
For a lifetime incidence of 2 to 3 %.

Life time risk:
• 1 out of every 44 women in America will get
uterine cancer.
• incidence 2 to 3 % in developed countries.
•
Compare to a lifetime risk of 1 of 70 for
ovarian cancer
•
Approximately 1 of 9 for breast cancer.
•The median age at diagnosis is 61 years,
• Risk factors:
• Atypical hyperplasia is a precursor lesion for EM CA .
• Obesity .
excess of adipose tissue increases conversion of androstenedione
into estrone. Higher levels of estrone in the blood exposes the
endometrium to continuously high levels of estrogens.
• Late menopause.
• PCOS.

•
Ovarian tumour secreting oestrogen.
•
Medications: Tamoxifen ,HRT(oestrogen).
•
Null parity , subfertility.
•
Genetic :HNPPC(Lynch Syndrome).
•
(a defect in MSH mismatch repair genes) 40X risk of EM CA (5X Ov)
patients as young as 16y/o
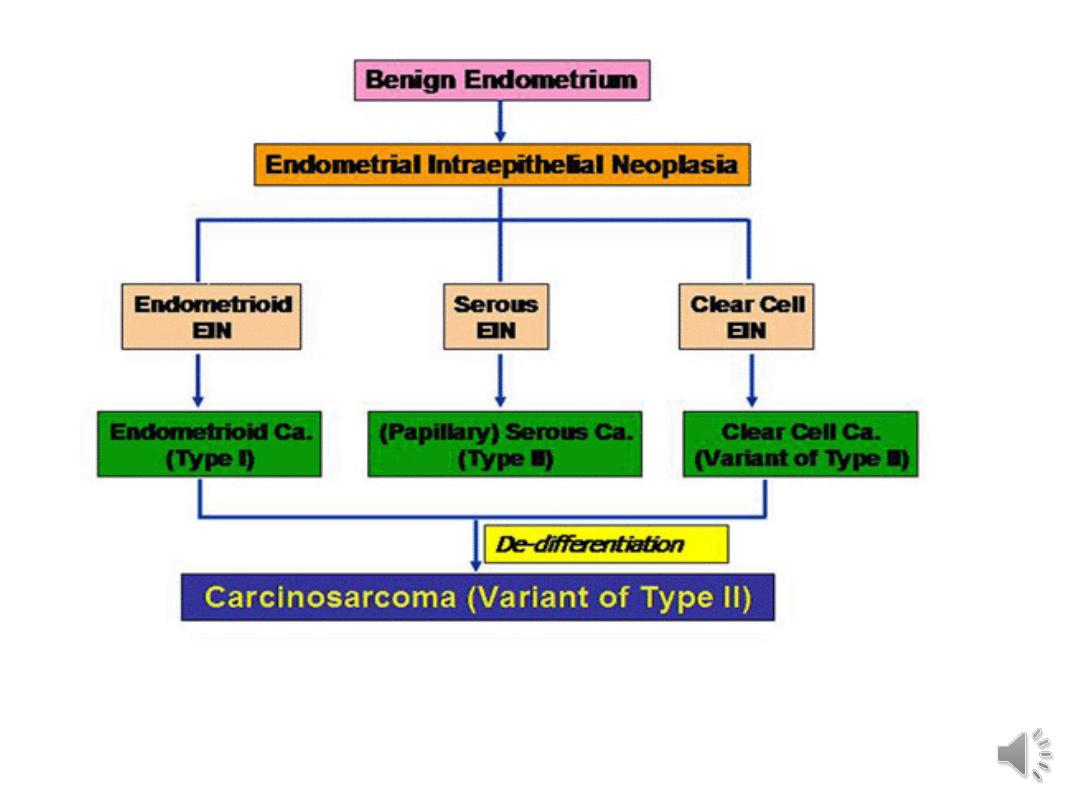

•The types of uterine cancers are:
--
carcinomas :
endometrioid or adeno-squamous histology
found in 85% and carry good prognosis.
-- Uterine papillary Cancer.
-- clear cell carcinomas
about 5% of the carcinoma, will have
poor prognosis &spread aggressively.

The sarcomas:
It’s less common but more aggressive than
endometrial carcinoma, develop in women in
forties.
It carry a poor prognosis.
About 6% of uterine CA in the US, but are
Twice as common in black women as compared to
whites.


Spread :
Direct:
Lymphatic Spread:
Upper part ,Para aortic ly .N.
Int . &ext .iliac ly.N,obtorator ly.N.Mid
&lower part:
Fundal area: inguinal lymph N
Blood .
Trans-peritoneal
.

•Staging of Endometrial Cancer:
•Stage I: Confined to the uterus.
•Stage II : Uterus & cervix.
•Stage III: Uterus ,adnexia ,vagina,pelvic ,aortic
lymph nodes involvement.
•Stage IV : Bladder ,rectum, inguinal lymph
nodes
Distant metastesis: liver , lung.
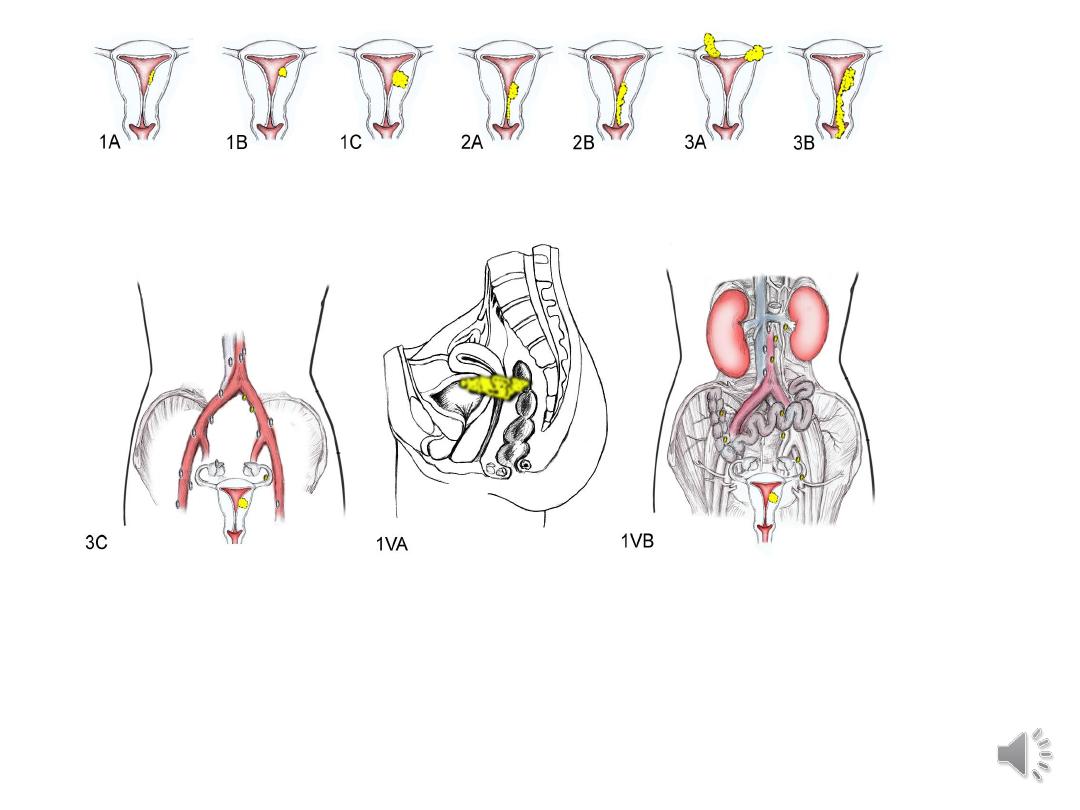

- It’s Surgical staging .
- Prognosis for endometrial cancer is generally
good, due to the early stage at presentation of
most patients
• - The overall 5 yr survival for all grades, stages
and histology's is 84%
- Stage of disease is the predictor of
survival, followed by it’s grade
surgical staging more accurately defines the
extent of a patient’s disease with respect to
metastases, depth of invasion, cervical
involvement..
Diagnosis:
History;
*Clinical presentation:
•
Postmenopausal bleeding
•
Peri-menopausal bleeding
•
inter-menstrual bleeding
•
Abnormal bleeding with history of anovulation

Clinical presentation continue
•
Postmenopausal women with endometrial cells on Pap
•
Thickened endometrial stripe via sonography
•
It is atypia that is the defining feature of
the premalignant endometrial lesion.
• * Risk factors: PCO, D.M,H.T,Nulliparty,

•Physical exam.
•General , abd.exam., pelvic exam.
•Investigations:
•U/S: Trans-vaginal U/S:
•Endometrial thickness more than 4mm in
menopausal woman.
•Endometrial biopsy:
• with or without hysteroscopy should be
performed
•
CXR to rule out pulmonary metastasis.
Mammogram.
Colon evaluation.
•
Both breast and colon cancer are more common in
women with EndometrialCA, therefore should be
screened for these diseases prior to surgical
treatment .

Diff. Diagnosis for abnormal bleeding:
1.Endometrial CA:
Endometrial biopsy is the main diagnostic tool ,
15% of the post-menaposal women with
abnormal bleeding will be diagnosed as
malignancy.
2. hormone replacement induced bleeding.
3.vaginal or uterine bleeding from atrophy

4. benign condition of endometrial hyperplasia,
or polyps or fibroid induced bleeding.
5. other genital tract lesions and malignancies
(cervical, vaginal, vulvar)

•
Regarding screening for endometrial Cancer
-Cervical cytology screening is not satisfactory
-Trans-vaginal sonograph,
-Hysteroscopy and Uterine biopsy would not been
used as screening tools, though they are useful for
diagnostic purposes
.
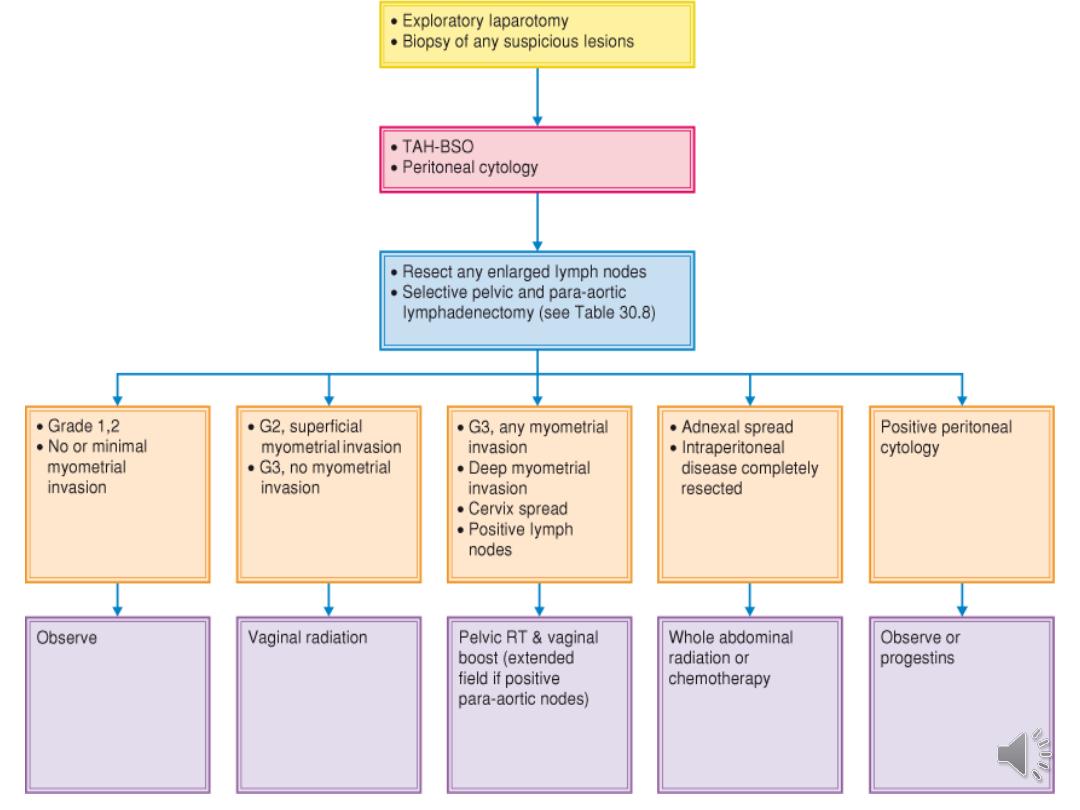
Treatment :
Stage I low risk: TAH+BSO
Stage I High risk: TAH+BSO –Post op. Radiation
Stage II : TAH+BSO –Post op. Radiation
Stage III: TAH +BSO +Post. op. Radiation
Stage IV: Radiation
For uterine sarcoma TAH +BSO +Radiation.

•The mainstay of adjuvant therapy for Endo.CA is
Radiation
Radiation may be delivered as either vaginal
brachy-therapy or whole pelvic tele-therapy or
both.
Hormonal therapy, with progestins, and cytotoxic
chemotherapy are generally reserved for
advanced disease or recurrent disease.

•Carcinosarcoma or MMMT is the most
common type of uterine sarcoma
•Both Carcinosarcomas and adenosarcomas
belong to a group of mixed tumors in which
epithelial and stromal components of the tumor.
•Carcinosarcomas contain histologically malignant
epithelial and non-epithelial components

•
while adenosarcomas contain benign epithelial
component with malignant stroma .
•
Both MMMT and LMS are twice as common in
blacks as compared to whites

THANK YOU
